Abstract
OBJECTIVE
An integrated sensor-augmented pump system has been introduced that interrupts basal insulin infusion for 2 h if patients fail to respond to low-glucose alarms. It has been suggested that such interruptions of basal insulin due to falsely low glucose levels detected by sensor could lead to diabetic ketoacidosis. We hypothesized that random suspension of basal insulin for 2 h in the overnight period would not lead to clinically important increases in blood β-hydroxybutyrate levels despite widely varying glucose values prior to the suspension.
RESEARCH DESIGN AND METHODS
Subjects measured blood glucose and blood β-hydroxybutyrate levels using a meter each night at 9:00 p.m., then fasted until the next morning. On control nights, the usual basal rates were continued; on experimental nights, the basal insulin infusion was reprogrammed for a 2-h zero basal rate at random times after 11:30 p.m.
RESULTS
In 17 type 1 diabetic subjects (mean age 24 ± 9 years, diabetes duration 14 ± 11 years, A1C level 7.3 ± 0.5% [56 mmol/mol]), blood glucose and blood β-hydroxybutyrate levels were similar at 9:00 p.m. on suspend nights (144 ± 63 mg/dL and 0.09 ± 0.07 mmol/L) and nonsuspend nights (151 ± 65 mg/dL and 0.08 ± 0.06 mmol/L) (P = 0.39 and P = 0.47, respectively). Fasting morning blood glucose levels increased after suspend nights compared with nonsuspend nights (191 ± 68 vs. 141 ± 75 mg/dL, P < 0.0001), and the frequency of fasting hypoglycemia decreased the morning following suspend nights (P < 0.0001). Morning blood β-hydroxybutyrate levels were slightly higher after suspension (0.13 ± 0.14 vs. 0.09 ± 0.11 mmol/L, P = 0.053), but the difference was not clinically important.
CONCLUSIONS
Systems that suspend basal insulin for 2 h are safe and do not lead to clinically significant ketonemia even if the blood glucose level is elevated at the time of the suspension.
Introduction
The Diabetes Control and Complications Trial (DCCT) demonstrated a clear relationship between improved glycemic control and a decreased risk of diabetes complications, but the ability to attain normoglycemia has been elusive for many patients living with type 1 diabetes (1,2). The DCCT also showed that the price that was paid for improved glycemic control with intensive treatment was a threefold increase in the risk of severe hypoglycemia (3). Hypoglycemia can lead to significant morbidity and mortality, and fear of hypoglycemia is often a deterrent for patients and clinicians to achieve and maintain the strict target blood glucose levels used in the DCCT (4).
Patients with type 1 diabetes are particularly vulnerable to severe hypoglycemic events while asleep at night (5). Unlike nondiabetic individuals, patients receiving therapy with fixed basal insulin replacement regimens are unable to automatically reduce insulin delivery and plasma insulin concentrations in response to falling plasma glucose levels. Since most patients with long-standing type 1 diabetes also lose the ability to mount a glucagon response to hypoglycemia (6), stimulation of epinephrine secretion is often the last line of defense to counteract the effects of insulin and to alert patients to low glucose levels (7). However, the release of epinephrine in response to hypoglycemia is markedly blunted during sleep at night in children and adults with and without diabetes (8,9). The Diabetes Research in Children Network demonstrated that the frequency of nocturnal hypoglycemia is increased twofold on nights after antecedent exercise (10), and continuous glucose monitoring studies have shown that low sensor glucose events at night are often prolonged (11). Indeed, in a case series, Buckingham et al. (12) demonstrated that low sensor glucose levels were detected 2–4 h prior to seizures in the middle of the night.
The introduction of new and improved sensor-augmented insulin pump systems has allowed a higher proportion of patients with type 1 diabetes to achieve target glucose and A1C levels with lower rates of severe hypoglycemia than those found in the DCCT (13–19). Moreover, such integrated systems offer the potential to “close the loop” of insulin administration by using computer algorithms to automatically adjust the rate of insulin infusion based on minute-to-minute changes in sensor glucose levels. Several studies have demonstrated the feasibility of this approach in inpatient clinical research center settings (20–29).
The first, relatively small step in the direction of a closed-loop system for outpatient treatment of type 1 diabetes has been achieved with the introduction of the MiniMed Paradigm Veo system (Medtronic, Northridge, CA). The low-glucose suspend feature of this sensor-augmented pump system allows the basal rate of the patient’s pump to be automatically suspended for up to 2 h if the patient fails to respond to the sensor’s low-glucose alarms. Recent standardized inpatient protocols and unstructured outpatient clinical use studies showed that the “low-glucose suspend” feature reduces the duration and severity of hypoglycemia without causing rebound hyperglycemia (30–34). In the recently published ASPIRE (Automation to Simulate Pancreatic Insulin Response) in-home study, which was a 3-month randomized outpatient trial comparing the use of the low-glucose suspend feature to sensor-augmented pump therapy, threshold-based pump suspensions led to a 30% reduction in nocturnal hypoglycemia without concomitant deterioration in glycemic control (35). Similarly, in the study by Ly et al. (36) use of the low-glucose suspend feature compared with pump-only treatment in a 6-month outpatient randomized trial led to a reduction in episodes of severe and moderate hypoglycemia. A potential concern related to the low-glucose suspend capability of sensor-augmented pumps is that suspension of basal insulin delivery for 2 h due to a failing sensor when the blood glucose levels are not actually low might lead to hyperglycemia and ketoacidosis. To address this question, the current study was designed and implemented to evaluate the effects of random nighttime suspensions of basal insulin infusion rates for 2 h even when blood glucose levels were not low.
Research Design and Methods
Study Subjects and Enrollment
Subjects were recruited from the Yale Type 1 Diabetes Program. Inclusion criteria included the following: age 15–50 years; clinical diagnosis of type 1 diabetes with a duration of at least 1 year; current use of a Medtronic insulin pump to allow pump downloads to CareLink personal software or willingness to use a Medtronic pump for the study period; duration of pump use of at least 3 months; A1C level ≤9% (75 mmol/mol); BMI <95th percentile for age and sex; no other chronic medical condition (except treated hypothyroidism); not receiving medications (other than insulin) known to affect blood glucose levels; no episodes of severe hypoglycemia within 3 months of study participation; and female subjects could not be pregnant or lactating. Subjects using sensor-augmented pump therapy were permitted to take part in the study; however, during the study period they were advised to not use their usual continuous glucose monitor to prevent alterations in care due to real-time sensor readings. All adult and pediatric subjects were required to have a responsible adult living in the same household who would serve as an alternate contact in the event of problems on basal suspension nights; these individuals were required to sign a study partner consent form. After a complete explanation of the study protocol, written informed consent was obtained from subjects ≥18 years; in subjects <18 years, both an adolescent assent and parent permission were obtained. The study was approved by the Yale University Human Investigation Committee.
Study Procedures
Following enrollment, subjects had a CGMS iPro Recorder (Medtronic) inserted for blinded sensor glucose data collection. Subjects were provided with a OneTouch Ultra blood glucose meter (LifeScan, Milpitas, California), a Precision Xtra meter (Abbott Diabetes Care, Alameda, CA), and urine ketone strips. They were instructed to check blood glucose, blood β-hydroxybutyrate, and urine ketone levels at 9:00 p.m. on each study night and again the next morning prior to 8:00 a.m. while fasting before breakfast.
On each suspend night, one of the investigators called the subject to verify that prebed glucose and blood β-hydroxybutyrate levels were in acceptable ranges. Once verified, the investigator instructed the subject on which of the six randomized basal suspend patterns to use. All suspensions lasted for 2 h with 0 unit/h basal rates that started at six different times (11:30 p.m., 12 a.m., 12:30 a.m., 1 a.m., 1:30 a.m., or 2:00 a.m.). For convenience, two of these patterns were preprogrammed into the pump at one of the study visits. Verification that suspends occurred as instructed was possible with downloads to CareLink.
In order to test compliance with the study protocol, blood glucose and ketone levels at 9:00 p.m. and fasting levels the next morning were obtained on 3–7 nights during the first week of the study without any 2-h suspensions. These data were included in the analysis of nonsuspend nights. During the next 2 weeks of the study, the patients received either their usual basal insulin doses (additional nonsuspend nights) or one of the alternate basal rate profiles that included a basal rate of 0 for 2 h at random times starting between 11:30 p.m. and 2:00 a.m. (suspend night data). Subjects and study staff were therefore not blinded to the study condition. Throughout the study period, subjects wore a Medtronic CGMS iPro Recorder to gather blinded sensor glucose data.
On all study nights, subjects were instructed not to administer a bolus of insulin after 9:00 p.m. and to consume carbohydrate-containing snacks only if the 9:00 p.m. blood glucose level was <100 mg/dL. If the blood glucose level was >300 mg/dL and/or the blood β-hydroxybutyrate level was >0.5 mmol/L at 9:00 p.m., subjects were instructed to take a correction dose of insulin, and any planned suspension was not performed. These nights were excluded from all data analysis.
Data Analysis and Statistical Considerations
Blood glucose and blood β-hydroxybutyrate levels were compared during suspend and nonsuspend conditions at 9:00 p.m. and while fasting the next morning before 8:00 a.m. Data are expressed as the mean ± SD. Blood glucose and blood β-hydroxybutyrate levels were verified by meter downloads; CareLink uploads verified that subjects performed the suspensions as instructed and that no extra bolus doses of insulin were given in the overnight period on each of the suspend nights (Fig. 1). Data collected from blinded continuous glucose monitors were used to assess changes in sensor glucose levels at the start of the suspend period (0 h), at the end of the suspend period (2 h), and 4 h after the initiation of the suspend period (4 h). Nonsuspend nights were chosen at random and were matched within each subject to have the same time points analyzed.
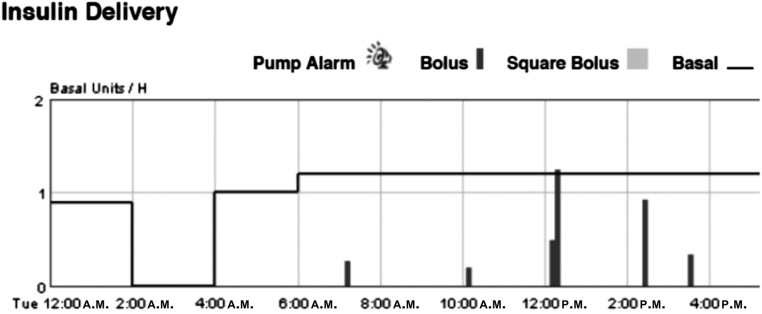
Figure 1.
Verification of suspension through download of insulin pump. Downloading subjects’ pump data onto CareLink personal software ensures that basal insulin suspension occurred as specified and that no surreptitious insulin delivery occurred in the overnight period. In this graph, basal insulin delivery in units per hour is listed on the left y-axis, as noted by the horizontal lines, whereas bolus insulin delivery is noted by the vertical lines. Here suspension occurred between 2:00 and 4:00 a.m.
Statistical comparisons between suspend and nonsuspend nights were accomplished with unpaired t tests. Post hoc analysis included determination of the frequency of hypoglycemia in the morning before breakfast (defined as a blood glucose level <70 mg/dL) with comparison of suspend vs. nonsuspend nights achieved using a χ2 test. Calculations were performed using Prism 6 (GraphPad Software, San Diego, CA).
Results
Nineteen subjects were enrolled into the study, but two subjects withdrew consent during the nonsuspend week of data collection. The 17 subjects who completed the study were aged 24 ± 9 years (range 15–44 years) and had a diabetes duration of 14 ± 11 years (range 4–34 years). Seven of the subjects (41%) were female. Subjects were generally well controlled with a mean A1C of 7.3 ± 0.5% (range 6.3–8.2% [56 mmol/mol; range 45–66 mmol/mol]).
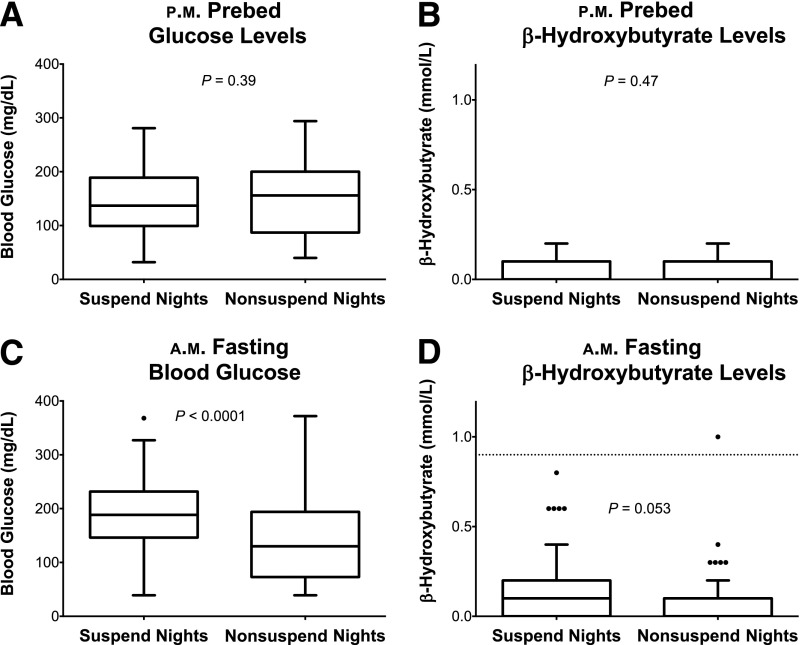
A total of 118 suspend nights (5–8 nights per subject) and 131 nonsuspend nights (5–10 nights per subject) were included in the analysis. As demonstrated in Fig. 2, mean 9:00 p.m. blood glucose levels were similar on suspend nights (144 ± 63 mg/dL) and nonsuspend nights (151 ± 65 mg/dL), and ranged between 32 and 281 mg/dL on suspend nights and 40 and 294 mg/dL on nonsuspend nights. The 9:00 p.m. blood β-hydroxybutyrate levels were also similar on suspend and nonsuspend nights (0.09 ± 0.07 vs. 0.08 ± 0.06 mmol/L, P = 0.47).
Figure 2.
Prebed and fasting blood glucose and β-hydroxybutyrate levels. A: Prebed glucose levels (in milligrams per deciliter) on suspend vs. nonsuspend nights were similar, with a wide range of prebed glucose levels. B: Likewise, prebed β-hydroxybutyrate levels were equivalent in the two study conditions. C: As expected, blood glucose levels in the fasting period tended to be higher after nights with basal insulin suspension (P < 0.0001). D: Fasting β-hydroxybutyrate levels tended to be higher in the fasting period after basal insulin suspension. Outliers are noted as closed circles. The dashed line at 0.9 mmol/L is the upper limit of blood β-hydroxybutyrate levels associated with trace urinary ketones.
Fasting blood glucose levels varied widely on suspend nights (range 39–368 mg/dL) and nonsuspend nights (39–372 mg/dL). However, the suspension of basal insulin for 2 h during the night resulted in mean fasting glucose levels that were 50 mg/dL higher than on nonsuspend nights (suspend nights 191 ± 68 vs. 141 ± 75 mg/dL, P < 0.0001). Blood β-hydroxybutyrate levels were slightly higher in the morning after the suspension of basal insulin (nonsuspend nights 0.13 ± 0.14 vs. 0.09 ± 0.11 mmol/L), but the difference did not reach statistical significance (P = 0.053). Moreover, as shown in Fig. 2, fasting blood β-hydroxybutyrate levels were >0.5 mmol/L on only five suspend nights and one nonsuspend night (P = 0.1); corresponding morning urinary ketone levels ranged between trace to small on suspend nights, and the urine ketone level was small on the one nonsuspend night with a blood β-hydroxybutyrate level of 1.0 mmol/L.
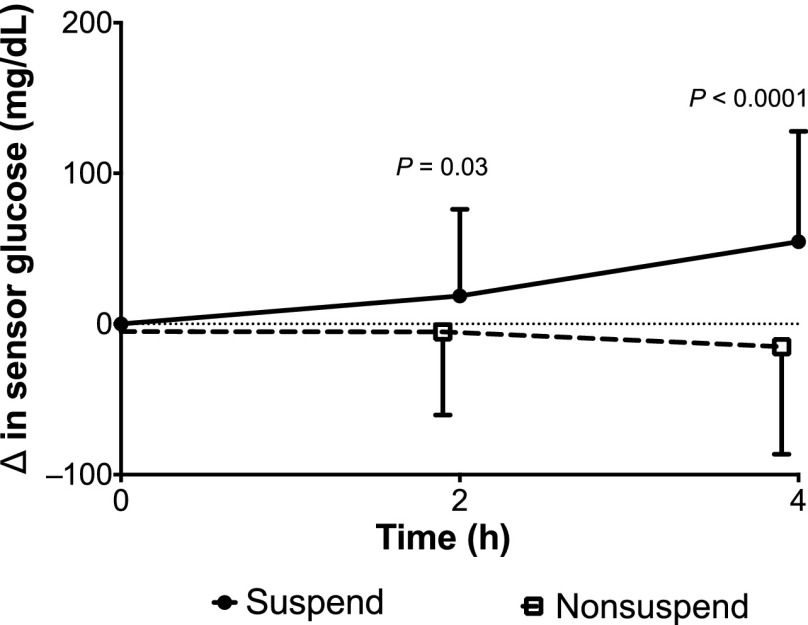
Sensor glucose data were collected during 99 suspend nights and 81 nonsuspend nights. At the start of the suspend period, the mean sensor glucose level was 135 ± 64 mg/dL and ranged between 40 and 331 mg/dL. As shown in Fig. 3, the sensor glucose level rose by 18 ± 58 mg/dL by the end of the 2-h suspension, and by 55 ± 73 mg/dL 4 h after the suspension. This differed significantly from the nonsuspend nights, where the baseline sensor glucose level was 152 ± 78 mg/dL (range 40–400 mg/dL); no change in sensor glucose level was seen at 2 and 4 h (P = 0.03 and <0.0001, respectively, vs. suspend nights).
Figure 3.
Change in sensor glucose levels. Change in sensor glucose value (in milligrams per deciliter) is compared on suspend night (solid circles with solid line) vs. nonsuspend nights (open boxes with dashed line). Sensor glucose levels at the start of a suspend period (0 h), the end of the suspend period (2 h), and 4 h after the initiation of a suspend period (4 h) are noted. On nonsuspend nights, sensor glucose levels were assessed at time periods that would coincide with suspend nights (i.e., 11:30 p.m.–1:30 a.m. or 2:00–4:00 a.m.).
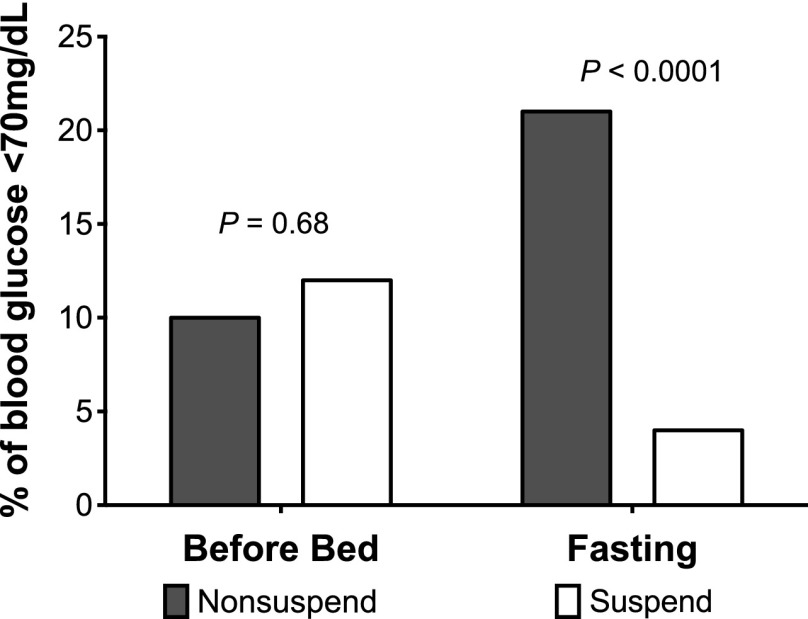
As shown in Fig. 4, the 9:00 p.m. blood glucose level was <70 mg/dL on 12% of suspend nights and on 10% of nonsuspend nights (P = 0.69). Notably, basal insulin suspension was associated with a reduced frequency of fasting hypoglycemia regardless of evening blood glucose levels with only 4% of pre-breakfast values <70 mg/dL vs. 21% on nonsuspend nights (P < 0.0001). Additionally, sensor data documented 12 nights with a sensor glucose level <70 mg/dL (mean level 52 ± 10 mg/dL) at the start of the suspend period. Sensor glucose levels rose by 16 ± 34 mg/dL (0.9 ± 1.9 mmol/L) at 2 h, and by 63 ± 57 mg/dL at 4 h; on 83% of suspend nights, the sensor glucose level was ≥60 mg/dL 4 h after basal insulin interruption. This differed from the 12 documented nonsuspend nights with baseline sensor glucose levels <70 mg/dL (mean level 58 ± 11 mg/dL), during which sensor glucose levels at 2 h and 4 h were relatively unchanged (65 ± 23 and 69 ± 27 mg/dL, respectively, P = NS).
Figure 4.
Frequency of hypoglycemia. Prebed and fasting blood glucose levels were classified based on whether or not hypoglycemia was present (blood glucose <70 mg/dL). The nonsuspend study condition is noted by gray bars. The percentage of blood glucose levels <70 mg/dL is represented on the y-axis.
Conclusions
This study was undertaken to evaluate whether 2-h suspensions of basal insulin due to artifactually low sensor glucose values during the overnight period are safe, in the absence of concurrent insulin pump or infusion site problems. We developed a study protocol that allowed us to evaluate this issue in a real-life outpatient setting over a range of blood glucose levels and a large number of study nights. Even though we purposely did not wake subjects to measure blood glucose levels just prior to suspension of the basal infusion, the wide range of 9:00 p.m. and fasting a.m. blood glucose values, as well as blinded sensor glucose levels, that were observed during the study serve to validate this approach. To eliminate the possibility of concurrent pump or infusion site problems, basal insulin suspensions were not carried out when the 9:00 p.m. blood glucose level was >300 mg/dL or blood β-hydroxybutyrate level was >0.5 mmol/L. Food intake was unrestricted until 9:00 p.m. However, the subjects were asked not to eat or to administer a bolus of insulin after 9:00 p.m. in order to avoid masking the effects of the basal insulin suspend by taking extra insulin boluses during the night.
The major findings of the study support our hypothesis regarding the safety of 2-h basal insulin suspensions during the overnight period. Even though there was a trend to slightly higher morning blood β-hydroxybutyrate levels after basal suspends, the 0.04 mmol/L difference compared with nonsuspend nights was not statistically significant or clinically meaningful. Moreover, in 113 of the 118 suspend nights, fasting blood β-hydroxybutyrate levels were within the normal range at <0.5 mmol/L, and the others were between 0.6 and 0.8 mmol/L. To put this finding into a more common clinical context, these blood levels resulted only in trace to small urinary ketone levels on the mornings after the suspension.
Our results are similar to those that were observed during a study by Attia et al. (37). That study was performed to describe the time course of metabolic deterioration in insulin pump patients after prolonged interruptions of basal insulin during the overnight period. In that study, mean blood β-hydroxybutyrate levels rose from 0.1 to 1.0 mmol/L after a 6-h suspension of the basal infusion of lispro insulin, and, as in the current study, the rise in mean blood β-hydroxybutyrate levels was <0.1 mmol/L during the first 2 h of basal insulin suspension. However, the study by Attia et al. (37) involved only nine subjects who were receiving lispro insulin during only one overnight stay in the clinical research center. Additionally, prior to basal insulin suspension, subjects in that study needed to be within a target blood glucose range of 60–150 mg/dL. Thus, the results were far less convincing than our findings of minimal increases in blood β-hydroxybutyrate levels in 17 subjects over 118 nights, with suspensions occurring at widely varying glucose levels. On the other hand, the number of subjects who were studied was relatively small. Thus, we cannot rule out the possibility that some patients may have exaggerated increases in blood ketone levels under the same conditions.
The ∼50 mg/dL increase in mean fasting glucose levels on suspend nights is consistent with the 30–45 mg/dL increase in plasma glucose levels during the first 2 h of basal insulin suspension in the study by Attia et al. (37). Our findings are also similar to the 30–65 mg/dL increase in blood glucose levels reported in clinical research center and clinical use studies of the Medtronic Paradigm Veo system after a 2-h basal insulin suspend (31–34). Although not a primary outcome of the study, it is noteworthy that the random 2-h basal insulin suspensions markedly decreased the frequency of fasting hypoglycemia the next morning.
Conducting a clinical trial in the outpatient setting like this poses a number of substantial challenges. Subjects may not follow the study protocol and may give bolus doses of insulin in the middle of the night, which, in turn, might minimize glycemic deterioration from the basal suspension. However, our use of the CareLink personal software program allowed for examination of every overnight period to ensure that basal suspension was programmed as instructed and that extra insulin was not delivered surreptitiously. It should also be noted that our cohort of subjects was relatively well controlled, making the subjects less susceptible to rapid deterioration when basal insulin infusion was interrupted. On the other hand, well-controlled, intensively treated patients with type 1 diabetes are precisely the individuals who are likely to receive the greatest benefit of sensor-augmented pumps with low-glucose suspend capability.
The main obstacle that must be overcome before closed-loop systems become a practical reality for the treatment of type 1 diabetes at home is to have redundant safeguards in place that will prevent the overdelivery of insulin due to a system malfunction. Although automatically turning up insulin delivery to prevent hyperglycemia presents a potentially devastating safety risk, turning off a pump for a relatively short period of time to limit the extent and duration of hypoglycemia presents an attractive first step along the pathway to an artificial pancreas. Our demonstration of the safety of a 2-h suspension of basal insulin supports this approach and also sets the stage for the next step toward automatic control of glucose in patients with type 1 diabetes; namely, automatically suspending basal insulin delivery based on a projected low glucose level without sounding alarms.
Article Information
Acknowledgments. The authors thank the participants and their families, and the nurses and staff of the Yale Children’s Diabetes Clinic and the Yale Center for Clinical Investigation, whose support and participation made this project possible.
Funding. This work was supported by grants from the National Institutes of Health (K12-DK-094714, UL1-RR-024139, and P30-DK-045735).
Duality of Interest. Medtronic Diabetes provided infusion sets, reservoirs, and loaner pumps to allow subjects not using Medtronic pumps to be recruited into the study. W.V.T. serves as a consultant to Medtronic MiniMed and Animas Corporation. S.A.W. serves as a consultant to Animas Corporation and received in-kind research support from Medtronic. No other potential conflicts of interest relevant to this article were reported.
No sponsor had any role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Author Contributions. J.L.S. researched data and wrote the manuscript. M.P.C., E.C., C.M., L.C., A.T.S., K.W., M.Z, and E.T. researched data and contributed to the discussion. W.V.T. and S.A.W. researched data, contributed to the discussion, and reviewed and edited the manuscript. J.L.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 72nd Scientific Sessions of the American Diabetes Association, Philadelphia, PA, 8–12 June 2012; the 6th International Conference on Advanced Technologies and Treatments for Diabetes, Paris, France, 27 February–3 March 2013; Translational Science 2013, Washington, DC, 17–19 April 2013; the American Society for Clinical Investigation and the Association of American Physicians Joint Meeting, Chicago, IL, 26–28 April 2013; and the 73rd Scientific Sessions of the American Diabetes Association, Chicago, IL, 21–25 June 2013.
References
- 1.Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 2.Diabetes Control and Complications Trial Research Group Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr 1994;125:177–188 [DOI] [PubMed] [Google Scholar]
- 3.Diabetes Control and Complications Trial Research Group Effect of intensive therapy on residual beta-cell function in patients with type 1 diabetes in the Diabetes Control and Complications Trial. A randomized, controlled trial. Ann Intern Med 1998;128:517–523 [DOI] [PubMed] [Google Scholar]
- 4.Nixon R, Pickup JC. Fear of hypoglycemia in type 1 diabetes managed by continuous subcutaneous insulin infusion: is it associated with poor glycemic control? Diabetes Technol Ther 2011;13:93–98 [DOI] [PubMed] [Google Scholar]
- 5.DCCT Research Group Epidemiology of severe hypoglycemia in the Diabetes Control and Complications Trial. Am J Med 1991;90:450–459 [PubMed] [Google Scholar]
- 6.Bolli G, de Feo P, Compagnucci P, et al. Abnormal glucose counterregulation in insulin-dependent diabetes mellitus. Interaction of anti-insulin antibodies and impaired glucagon and epinephrine secretion. Diabetes 1983;32:134–141 [DOI] [PubMed] [Google Scholar]
- 7.Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003;26:1902–1912 [DOI] [PubMed] [Google Scholar]
- 8.Jones TW, Porter P, Sherwin RS, et al. Decreased epinephrine responses to hypoglycemia during sleep. N Engl J Med 1998;338:1657–1662 [DOI] [PubMed] [Google Scholar]
- 9.Banarer S, Cryer PE. Sleep-related hypoglycemia-associated autonomic failure in type 1 diabetes: reduced awakening from sleep during hypoglycemia. Diabetes 2003;52:1195–1203 [DOI] [PubMed] [Google Scholar]
- 10.Tsalikian E, Mauras N, Beck RW, et al. Diabetes Research In Children Network Direcnet Study Group Impact of exercise on overnight glycemic control in children with type 1 diabetes mellitus. J Pediatr 2005;147:528–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group Prolonged nocturnal hypoglycemia is common during 12 months of continuous glucose monitoring in children and adults with type 1 diabetes. Diabetes Care 2010;33:1004–1008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buckingham B, Wilson DM, Lecher T, Hanas R, Kaiserman K, Cameron F. Duration of nocturnal hypoglycemia before seizures. Diabetes Care 2008;31:2110–2112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahern JA, Boland EA, Doane R, et al. Insulin pump therapy in pediatrics: a therapeutic alternative to safely lower HbA1c levels across all age groups. Pediatr Diabetes 2002;3:10–15 [DOI] [PubMed] [Google Scholar]
- 14.Boland EA, Grey M, Oesterle A, Fredrickson L, Tamborlane WV. Continuous subcutaneous insulin infusion. A new way to lower risk of severe hypoglycemia, improve metabolic control, and enhance coping in adolescents with type 1 diabetes. Diabetes Care 1999;22:1779–1784 [DOI] [PubMed] [Google Scholar]
- 15.Maniatis AK, Klingensmith GJ, Slover RH, Mowry CJ, Chase HP. Continuous subcutaneous insulin infusion therapy for children and adolescents: an option for routine diabetes care. Pediatrics 2001;107:351–356 [DOI] [PubMed] [Google Scholar]
- 16.Plotnick LP, Clark LM, Brancati FL, Erlinger T. Safety and effectiveness of insulin pump therapy in children and adolescents with type 1 diabetes. Diabetes Care 2003;26:1142–1146 [DOI] [PubMed] [Google Scholar]
- 17.Sulli N, Shashaj B. Continuous subcutaneous insulin infusion in children and adolescents with diabetes mellitus: decreased HbA1c with low risk of hypoglycemia. J Pediatr Endocrinol Metab 2003;16:393–399 [DOI] [PubMed] [Google Scholar]
- 18.Willi SM, Planton J, Egede L, Schwarz S. Benefits of continuous subcutaneous insulin infusion in children with type 1 diabetes. J Pediatr 2003;143:796–801 [DOI] [PubMed] [Google Scholar]
- 19.Tamborlane WV, Beck RW, Bode BW, et al. Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–1476 [DOI] [PubMed] [Google Scholar]
- 20.Hovorka R, Allen JM, Elleri D, et al. Manual closed-loop insulin delivery in children and adolescents with type 1 diabetes: a phase 2 randomised crossover trial. Lancet 2010;375:743–751 [DOI] [PubMed] [Google Scholar]
- 21.Weinzimer SA, Steil GM, Swan KL, Dziura J, Kurtz N, Tamborlane WV. Fully automated closed-loop insulin delivery versus semiautomated hybrid control in pediatric patients with type 1 diabetes using an artificial pancreas. Diabetes Care 2008;31:934–939 [DOI] [PubMed] [Google Scholar]
- 22.Weinzimer SA, Sherr JL, Cengiz E, et al. Effect of pramlintide on prandial glycemic excursions during closed-loop control in adolescents and young adults with type 1 diabetes. Diabetes Care 2012;35:1994–1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El-Khatib FH, Russell SJ, Nathan DM, Sutherlin RG, Damiano ER. A bihormonal closed-loop artificial pancreas for type 1 diabetes. Sci Transl Med 2010;2:27ra27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russell SJ, El-Khatib FH, Nathan DM, Magyar KL, Jiang J, Damiano ER. Blood glucose control in type 1 diabetes with a bihormonal bionic endocrine pancreas. Diabetes Care 2012;35:2148–2155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Renard E, Place J, Cantwell M, Chevassus H, Palerm CC. Closed-loop insulin delivery using a subcutaneous glucose sensor and intraperitoneal insulin delivery: feasibility study testing a new model for the artificial pancreas. Diabetes Care 2010;33:121–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kovatchev B, Cobelli C, Renard E, et al. Multinational study of subcutaneous model-predictive closed-loop control in type 1 diabetes mellitus: summary of the results. J Diabetes Sci Tech 2010;4:1374–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Castle JR, Engle JM, El Youssef J, et al. Novel use of glucagon in a closed-loop system for prevention of hypoglycemia in type 1 diabetes. Diabetes Care 2010;33:1282–1287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nimri R, Atlas E, Ajzensztejn M, Miller S, Oron T, Phillip M. Feasibility study of automated overnight closed-loop glucose control under MD-logic artificial pancreas in patients with type 1 diabetes: the DREAM Project. Diabetes Technol Ther 2012;14:728–735 [DOI] [PubMed] [Google Scholar]
- 29.Ward WK, Castle JR, El Youssef J. Safe glycemic management during closed-loop treatment of type 1 diabetes: the role of glucagon, use of multiple sensors, and compensation for stress hyperglycemia. J Diabetes Sci Tech 2011;5:1373–1380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garg S, Brazg RL, Bailey TS, et al. Reduction in duration of hypoglycemia by automatic suspension of insulin delivery: the in-clinic ASPIRE study. Diabetes Technol Ther 2012;14:205–209 [DOI] [PubMed] [Google Scholar]
- 31.Agrawal P, Welsh JB, Kannard B, Askari S, Yang Q, Kaufman FR. Usage and effectiveness of the low glucose suspend feature of the Medtronic Paradigm Veo insulin pump. J Diabetes Sci Tech 2011;5:1137–1141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Danne T, Kordonouri O, Holder M, et al. Prevention of hypoglycemia by using low glucose suspend function in sensor-augmented pump therapy. Diabetes Technol Ther 2011;13:1129–1134 [DOI] [PubMed] [Google Scholar]
- 33.Choudhary P, Shin J, Wang Y, et al. Insulin pump therapy with automated insulin suspension in response to hypoglycemia: reduction in nocturnal hypoglycemia in those at greatest risk. Diabetes Care 2011;34:2023–2025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ly TT, Nicholas JA, Retterath A, Davis EA, Jones TW. Analysis of glucose responses to automated insulin suspension with sensor-augmented pump therapy. Diabetes Care 2012;35:1462–1465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bergenstal RM, Klonoff DC, Garg SK, et al. ASPIRE In-Home Study Group Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med 2013;369:224–232 [DOI] [PubMed] [Google Scholar]
- 36.Ly TT, Nicholas JA, Retterath A, Lim EM, Davis EA, Jones TW. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs. standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial. JAMA 2013;310:1240–1247 [DOI] [PubMed] [Google Scholar]
- 37.Attia N, Jones TW, Holcombe J, Tamborlane WV. Comparison of human regular and lispro insulins after interruption of continuous subcutaneous insulin infusion and in the treatment of acutely decompensated IDDM. Diabetes Care 1998;21:817–821 [DOI] [PubMed] [Google Scholar]