Abstract
Asthma, diabetes, and high blood pressure are common maternal conditions that can impact birth outcomes. Data from hospital discharges in Hawai‘i were analyzed for 107,034 singleton births from 2003–2008. Categories were determined using the International Statistical Classification of Diseases, ninth revision (ICD-9) from linked delivery records of mother and infant. Prevalence estimates of asthma (ICD-9: 493), diabetes (ICD-9: 250,648.0, 648.8), high blood pressure (ICD-9: 401–405,642) as coded on the delivery record, low birth weight (<2500 grams), high birth weight (>4500 grams), Cesarean delivery, and median hospital charges were calculated. Median regression analysis assessed total hospital charges adjusting for maternal age, maternal race, insurance, and Cesarean delivery. Maternal asthma was present in 4.3% (95% confidence interval=4.1–4.4%), maternal diabetes was present in 7.7% (95% CI=7.6–7.9%), and maternal high blood pressure was present in 9.2% (95% CI=9.0–9.3%) of births. In the adjusted median regression analysis, mothers with asthma had $999 (95% CI: $886 to $1,112) higher hospital charges compared to those without; mothers with diabetes had $743 (95% CI: $636 to $850) higher charges compared to those without; and mothers with high blood pressure had $2,314 (95% CI: $2,194 to $2,434) higher charges compared to those without. Asthma, diabetes, and high blood pressure are associated with higher hospital delivery charges and low birth weight. Diabetes and high blood pressure were also associated with Cesarean delivery. An increased awareness of the impact of these conditions on both adverse birth outcomes and the development of chronic disease is needed.
Keywords: Chronic Conditions, Reproductive Health, Birth Outcomes, Hospital Charges
Introduction
Chronic disease is associated with morbidity and mortality, affects quality of life, and is associated with substantial health care expenditures. The Centers for Disease Control and Prevention (CDC) estimates that 70% of deaths among Americans each year are from chronic disease, as are 75% of the annual health care costs.1 The primary prevention of chronic disease through improvement in modifiable risk factors such as physical inactivity, smoking, poor nutrition, and excessive alcohol consumption has the potential to improve the long term health of the population.2 There have been significant increases in the prevalence of many chronic conditions and their risk factors among women of reproductive age (18–44 years) in the United States.3,4 Chronic conditions such as high blood pressure, diabetes, and asthma are also related to adverse reproductive health outcomes including the morbidity associated with Cesarean delivery, eclampsia, perinatal infections, preterm delivery, low birth weight, macrosomia, infant death, and increased health care utilization.5–16 The primary prevention of chronic disease in women before and between pregnancies can improve perinatal outcomes. Addressing the risk factors of chronic disease, as early as possible, including those identified during pregnancy has the potential to promote overall health throughout the life course for women and their families.
In most populations in the United States, women are delaying birth of their first child to an older age, with an average maternal age at first birth of 25.0 years in 2006 compared to 21.4 years in 1970.17 These women may experience an increase in chronic conditions and the risk factors associated with them just by being older as well as due to the increases seen in the general population for chronic conditions, which may have an impact on their reproductive health outcomes. In the United States, the proportion of births to women aged 35 years and older increased from 8.8% in 1990 to 14.2% in 2008.18 The longer a woman has risk factors for chronic disease, or has been diagnosed with one or more chronic diseases, the higher the likelihood she may be in poorer health entering pregnancy, be at greater risk for adverse maternal and infant morbidity and mortality, and develop complications of chronic disease.19–21 With the increasing rates of chronic conditions and their risk factors in women of reproductive age,3 it is important to document the associated burdens through surveillance of chronic disease during pregnancy and associated birth outcomes.
Estimates of high blood pressure, diabetes, and asthma during pregnancy are largely unknown among the diverse Asian, Native Hawaiian, and multiple race population that lives in Hawai‘i. National data on the leading causes of death among adult women in the aggregated Asian and Pacific Islander group show higher death rates for stroke, cancer, and diabetes than the estimate for all race and ethnic groups combined and above that of the non-Hispanic White group.22 Within the Pacific Islander group, data show Native Hawaiians and Other Pacific Islanders to be one of the highest risk populations for cardiometabolic diseases.23 These higher rates of chronic disease among Asian and Pacific Islander populations highlight the importance of conducting surveillance and promoting chronic disease prevention at early opportunities throughout the life course, including during and shortly after pregnancy.
The goals of this analysis are to provide prevalence estimates of maternal asthma, high blood pressure, and diabetes among women who had a birth and to explore their associations with adverse birth outcomes and hospital charges for the diverse population in the State of Hawai‘i. This surveillance can be used to establish baseline estimates of these maternal chronic conditions during pregnancy and provide data so that appropriate interventions can be developed to help improve reproductive health, reduce hospital charges, and decrease the overall burden of disease.
Methods
Hospital discharge data were obtained from the Hawai‘i Health Information Corporation (HHIC)—a private, non-profit corporation that maintains a database of health care encounters in the State that occur in an emergency department or result in an inpatient hospitalization. The data collected are primarily administrative in nature, but include clinical data such as the International Statistical Classification of Diseases, ninth revision (ICD-9) codes, discharge disposition, birth weight, age, race, gender, hospital charges, and other limited data. The Hawai‘i Department of Health requested a data set from HHIC that linked the mothers' and infants' birth records (>95% linkage rate). Analysis was limited to 107,034 linked mother-infant pairs for singleton births during 2003–2008.
Hospital discharge data are tied to billing for reimbursement of services and thus provide an opportunity for surveillance of conditions among women with a live birth. These data may better characterize the presence of maternal conditions compared to other data sources such as birth certificate information, which are known to underestimate the presence of maternal conditions when compared to hospital discharge data,24,25 or compared to actual medical records.26 Maternal conditions were defined based on the presence of specific ICD-9 coding on any of the 20 available billing levels from the maternal record for each observation (Table 1). For high blood pressure, pregnancy associated (includes gestational hypertension, pre-eclampsia, and eclampsia) conditions were included due to their increasing recognition as risk factors for development of chronic disease.27–29 Women with either gestational diabetes or abnormal glucose tolerance identified during the pregnancy were considered to have diabetes due to the significantly increased risk of development of diabetes beyond the pregnancy for both of these diagnoses.29–32 Although there are specific codes for hypertension and diabetes complicating the pregnancy, the general ICD-9 codes for these chronic conditions (250 Diabetes, and 401–405 for Hypertension) were included to identify these conditions that were not recorded under a pregnancy related codes. This had little impact and identified only 10 additional cases for diabetes (0.1% of all diabetes diagnoses) and 10 additional cases for high blood pressure (0.1% of all high blood pressure diagnoses). For asthma, no specific code related to pregnancy exists so only the general ICD-9 code for the chronic condition was used. The focus of this analysis was to combine those with a pre-existing chronic condition and those with onset during pregnancy and see the impact on birth outcomes. Based on the diagnostic codes, 75% of those who were defined as having high blood pressure had onset with the pregnancy while 25% had chronic high blood pressure prior to or complicating the pregnancy. This was somewhat different from those who were defined as having diabetes where 88.3% had diabetes with an onset with the pregnancy and only 11.7% having had it prior to the pregnancy. These distributions were skewed towards those with an onset of the condition during pregnancy for both of these estimates and suggests the importance of providing appropriate anticipatory guidance related to the risks of developing chronic high blood pressure and diabetes post-partum.27–32
Table 1.
International Statistical Classification of Diseases, Ninth Revision (ICD-9) Codes Used to Define Maternal Conditions
| Maternal Condition | ICD-9 Coding |
| Asthma | 493 |
| Diabetes | 250, 648.0, 648.8 |
| High Blood Pressure | 401–405, 642 |
Outcomes
Birth Weight
Infant birth weight is related to the rate of fetal growth and gestational duration of the pregnancy. It is strongly related to both newborn morbidity and mortality and is a key population level indicator for maternal and child health.33 Birth weight was obtained from the newborn record and categorized as low birth weight (LBW: <2,500 grams) and high birth weight (HBW: >4,500 grams).
Delivery Type
A Cesarean delivery is a major surgery that is typically performed in the presence of pregnancy complications that could jeopardize the health of the mother and/or fetus. The rate of Cesarean delivery has steadily increased in the United States from 5.8% in 1970 to 32.3% in 2008 but has not been associated with significant improvement in neonatal morbidity or maternal health.34 For this analysis, delivery type was based on the newborn record with an ICD-9 code of ‘V3000’ signifying a vaginal delivery and a code of ‘V3001’ representing a Cesarean delivery; analyses were restricted to singleton births. The delivery type variable was also used to stratify results for hospital charges due to differences between vaginal and Cesarean deliveries for these outcomes.
Total Hospital Charges
Hospital charges were obtained from both the newborn's and the mother's records. Records with no information on hospital charges (14.4%, n=15,458) were excluded from this part of the analysis, and largely represented births from military hospitals (n=15,440) that do not report charge data to HHIC. Records with military insurance (n=1,367) that had charge information were included in the analysis. Total hospital charges were obtained by summing newborn and maternal charges.
Selected Maternal Characteristics
Age was based on mother's age on admission and categorized as <20, 20–24, 25–29, 30-–4, and 35 years and older. Self-identified race/ethnicity included White, Black, Hawaiian, Filipino, Japanese, and “Other.” The “Other” racial group included those who indicated more than one race, and those for whom race did not fall into one of the above categories. Those with race information listed as “unknown,” “not applicable,” or “not collected” accounted for 18.6% of records and are referred to as “unknown” in this report. Geographic variation was categorized into county of residency based on the mailing address reported at delivery. Insurance status was based on payer listed on maternal delivery record and was categorized as “None,” “Medicaid/QUEST,” “Military,” or “Private” insurance.
Analysis
Prevalence estimates and 95% confidence intervals (95% CI) based on exact binomial proportions35 were calculated for each chronic condition by selected maternal characteristics. For the continuous variable of hospital charges, the medians are presented and two-sided Wilcoxon-Mann-Whitney tests were used to compare median differences between those with and without the chronic condition. A small percentage of the population accounted for a large percentage of the hospital charges, reflecting a skewed distribution. The log-transformed total hospital charges were not normally distributed so the more robust median (50th quantile) regression analysis on the untransformed charges was performed to better account for the positively skewed distribution of this variable.36 A median regression analysis based on the SAS QUANTREG procedure was used to assess the effect of chronic conditions on total hospital charges while accounting for the potential confounding factors of maternal age, maternal race, maternal insurance, and delivery type. SAS v9.2 (SAS Institute Inc, Cary, North Carolina) statistical software was used for analysis.
Results
Overall in Hawai‘i, in this 6-year aggregate of singleton births, nearly three quarters of births occurred in women 20-34 years of age, with about 25% in each of the middle three age groups (20–24, 25–29, and 30–34 years) (Table 2). The most common race groups represented were Hawaiian (18.7% of births), Filipino (15.6%), and White (14.3%). Of particular note is that 20.7% of births had a race classified as “other” and 18.6% had no information related to race in the data—representing a combined 39.3% of births without a specific race group noted. Just over half the births were to those with private insurance, nearly one-third were to those on Medicaid/QUEST insurance, and 15.7% were to those with military insurance.
Table 2.
Selected Characteristics of Women Who Had Singleton Births, HHIC*, 2003–2008
| n | Proportion (%) | ||
| Age Group (years) | |||
| <20 | 9,166 | 8.6% | |
| 20–24 | 26,624 | 24.9% | |
| 25–29 | 28,291 | 26.4% | |
| 30–34 | 24,688 | 23.1% | |
| >=35 | 18,264 | 17.1% | |
| Subtotal | 107,033 | ||
| Race | |||
| White | 15,357 | 14.3% | |
| Black | 500 | 0.5% | |
| Hawaiian | 20,063 | 18.7% | |
| Filipino | 16,671 | 15.6% | |
| Japanese | 9,668 | 9.0% | |
| Chinese | 2,699 | 2.5% | |
| Other | 22,175 | 20.7% | |
| Unknown | 19,901 | 18.6% | |
| Subtotal | 107,034 | ||
| Insurance | |||
| None | 1,622 | 1.5% | |
| Medicaid/QUEST | 32,825 | 30.7% | |
| Military | 16,807 | 15.7% | |
| Private | 55,624 | 52.0% | |
| Subtotal | 106,878 | ||
| County of Residence | |||
| Hawai‘i | 13,364 | 12.6% | |
| Honolulu | 76,641 | 72.3% | |
| Kaua‘i | 4,754 | 4.5% | |
| Maui | 11,285 | 10.6% | |
| Subtotal | 106,044 | ||
| Total | 107,034 | ||
Note: HHIC represents data from the Hawai‘i Health Information Corporation
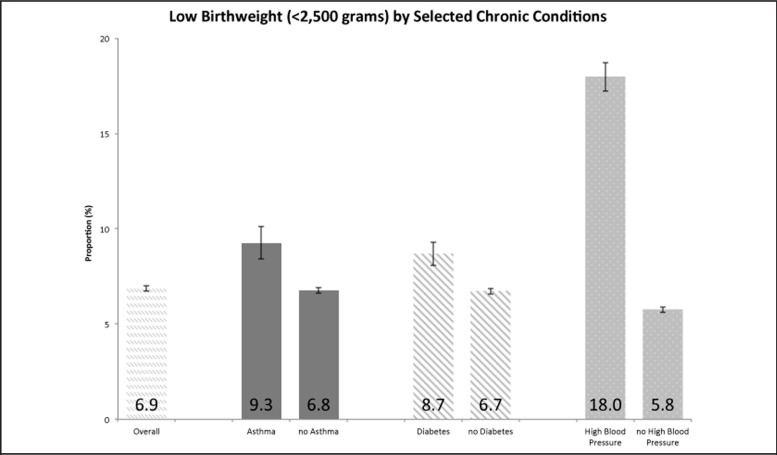
The occurrence of an asthma diagnosis decreased with increasing maternal age, and was highest among those of Hawaiian race and lowest among those of White and Chinese race (Table 3). The prevalence of a diagnosis of asthma was higher among those on Medicaid/QUEST insurance and those living in Honolulu County. Those with an asthma diagnosis had higher proportions of low birth weight infants, but no difference in high birth weight or cesarean sections compared to mothers without asthma (Figures 1–3). Total median hospital charges were higher among those with an asthma diagnosis compared to those without (Table 4). Those with an asthma diagnosis also had higher total median hospital charges in both cesarean and vaginal deliveries compared to those without an asthma diagnosis.
Table 3.
Prevalence Estimates of Asthma, Diabetes, and High Blood Pressure Among Women Who Had Singleton Births, by Selected Maternal Characteristics, HHIC*, 2003–2008
| Asthma | Diabetes | High Blood Pressure | |||||||
| Count | Prevalence (%) | 95% CI | Count | Prevalence (%) | 95% CI | Count | Prevalence (%) | 95% CI | |
| Age Group (years) | |||||||||
| <20 | 492 | 5.4 | (4.9–5.8) | 219 | 2.4 | (2.1–2.7) | 847 | 9.2 | (8.7–9.8) |
| 20–24 | 1,216 | 4.6 | (4.3–4.8) | 1,041 | 3.9 | (3.7–4.1) | 2,503 | 9.4 | (9.1–9.8) |
| 25–29 | 1,152 | 4.1 | (3.8–4.3) | 1,944 | 6.9 | (6.6–7.2) | 2,194 | 7.8 | (7.4–8.1) |
| 30–34 | 1,019 | 4.1 | (3.9–4.4) | 2,519 | 10.2 | (9.8–10.6) | 2,171 | 8.8 | (8.4–9.2) |
| >=35 | 682 | 3.7 | (3.5–4.0) | 2,524 | 13.8 | (13.3–14.3) | 2,080 | 11.4 | (10.9–11.9) |
| Race | |||||||||
| White | 453 | 3.0 | (2.7–3.2) | 665 | 4.3 | (4–4.7) | 1,002 | 6.5 | (6.1–6.9) |
| Black | 32 | 6.4 | (4.3–8.6) | 32 | 6.4 | (4.3–8.6) | 46 | 9.2 | (6.7–11.7) |
| Hawaiian | 1,343 | 6.7 | (6.4–7.0) | 1,411 | 7.0 | (6.7–7.4) | 2,014 | 10.0 | (9.6–10.5) |
| Filipino | 712 | 4.3 | (4.0–4.6) | 1,884 | 11.3 | (10.8–11.8) | 1,728 | 10.4 | (9.9–10.8) |
| Japanese | 375 | 3.9 | (3.5–4.3) | 852 | 8.8 | (8.3–9.4) | 670 | 6.9 | (6.4–7.4) |
| Chinese | 74 | 2.7 | (2.1–3.4) | 312 | 11.6 | (10.4–12.8) | 148 | 5.5 | (4.6–6.3) |
| Other | 942 | 4.3 | (4.0–4.5) | 1,665 | 7.5 | (7.2–7.9) | 1,712 | 7.7 | (7.4–8.1) |
| Unknown | 630 | 3.2 | (2.9–3.4) | 1,426 | 7.2 | (6.8–7.5) | 2,475 | 12.4 | (12–12.9) |
| Insurance | |||||||||
| None | 30 | 1.9 | (1.1–2.5) | 72 | 4.4 | (3.4–5.4) | 77 | 4.8 | (3.7–5.8) |
| Medicaid/QUEST | 1,875 | 5.7 | (5.5–6.0) | 2,033 | 6.2 | (5.9–6.5) | 2,882 | 8.8 | (8.5–9.1) |
| Military | 551 | 3.3 | (3.0–3.6) | 1,203 | 7.2 | (6.8–7.6) | 2,178 | 13.0 | (12.5–13.5) |
| Private | 2,088 | 3.8 | (3.6–3.9) | 4,916 | 8.8 | (8.6–9.1) | 4,637 | 8.3 | (8.1–8.6) |
| County of Residence | |||||||||
| Hawai‘i | 202 | 1.5 | (1.3–1.7) | 728 | 5.5 | (5.1–5.8) | 1,197 | 9.0 | (8.5–9.4) |
| Honolulu | 4,188 | 5.5 | (5.3–5.6) | 6,469 | 8.4 | (8.2–8.6) | 7,689 | 10.0 | (9.8–10.3) |
| Kaua‘i | 54 | 1.1 | (0.8–1.4) | 370 | 7.8 | (7.0–8.5) | 325 | 6.8 | (6.1–7.6) |
| Maui | 76 | 0.7 | (0.5–0.8) | 618 | 5.5 | (5.1–5.9) | 487 | 4.3 | (3.9–4.7) |
| Overall | 4,561 | 4.3 | (4.1–4.4) | 8,247 | 7.7 | (7.6–7.9) | 9,795 | 9.2 | (9.0–9.3) |
Note: HHIC represents data from the Hawai‘i Health Information Corporation
Figure 1.
Proportion of Low Birth Weight (<2,500 grams), Overall and by Selected Chronic Conditions, Hawai‘i Health Information Corporation, 2003–2008 Singleton Births.
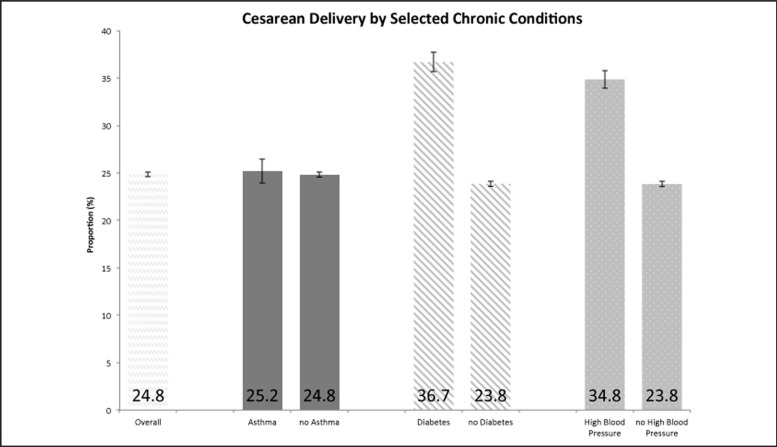
Figure 3.
Proportion of Cesarean Delivery, Overall and by Selected Chronic Conditions, Hawai‘i Health Information Corporation, 2003–2008 Singleton Births.
Table 4.
Median Hospital Charges Among Singleton Births for Presence or Absence of Chronic Conditions, Overall and by Delivery Type, HHIC*, 2003–2008
| Median Charge | Median Charge (Cesarean) | Median Charge (Vaginal) | |
| Asthma | $9,988.00 | $14,926.00 | $9,025.00 |
| no Asthma | $8,918.00 | $12,926.00 | $7,997.00 |
| P-value ** | < .001 | < .001 | < .001 |
| Diabetes | $10,701.00 | $13,807.00 | $9,002.00 |
| no Diabetes | $8,848.00 | $12,908.50 | $7,984.00 |
| P-value | < .001 | < .001 | < .001 |
| High Blood Pressure | $11,785.00 | $16,240.00 | $9,971.50 |
| no High Blood Pressure | $8,775.00 | $12,764.00 | $7,928.00 |
| P-value | < .001 | < .001 | < .001 |
| Overall | $8,968.00 | $13,000.00 | $8,041.00 |
Note: HHIC represents data from the Hawai‘i Health Information Corporation. Charges not available for births occurring at military facilities (n= 15,440 births) and for 5 births with Quest and 13 with Private Insurance. There were 1,367 births with military insurance had charges—occurred at non-military facilities.
P-value denotes difference by a two-sided Wilcoxon-Mann-Whitney test among those with the conditions vs not having the condition.
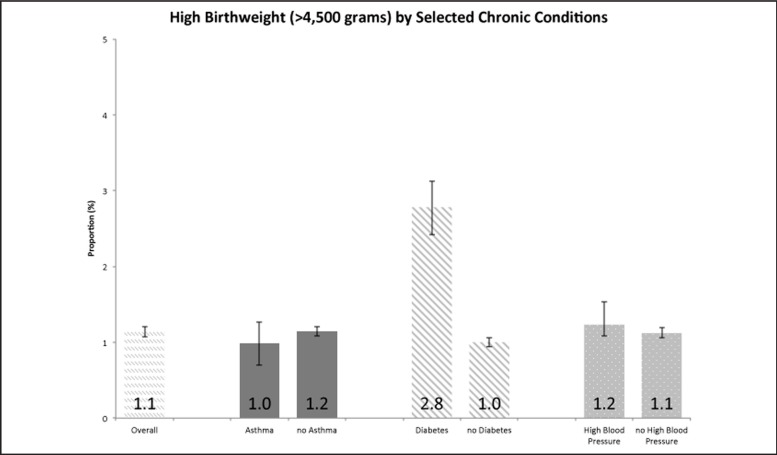
The occurrence of diabetes increased with increasing age and was higher among those of Filipino and Chinese race (Table 3). A diagnosis of diabetes was more common among those with private and military insurance and those living in Honolulu and Kaua'i Counties. Women with a diagnosis of diabetes had a higher percentage of low birth weight, high birth weight, and Cesarean section deliveries than women without a diagnosis of diabetes (Figures 1–3). Total median hospital charges were higher among those with a diagnosis of diabetes compared to those without (Table 4). Those with a diagnosis of diabetes also had higher total median hospital charges in both Cesarean and vaginal deliveries compared to those without a diagnosis of diabetes.
The occurrence of high blood pressure was higher in both the younger and the older age groups with those aged 25–29 years having the lowest estimates (Table 3). A diagnosis for high blood pressure was higher among those of Filipino, Hawaiian, and “unknown” race (Table 3). It was also more common among those with military insurance and those living in Honolulu and Hawai‘i Counties. Those with a diagnosis of high blood pressure had higher proportions of low birth weight and Cesarean sections, but no difference for high birth weight as compared with mothers without high blood pressure (Figures 13). Total median hospital charges were higher among those with a diagnosis of high blood pressure compared to those without (Table 4). Those with a diagnosis of high blood pressure also had higher total median hospital charges in both Cesarean and vaginal deliveries compared to those without the diagnosis.
In the median regression analysis, an asthma diagnosis was associated with a $999 (95% CI: $886 to $1,112) higher median charge compared to those without after controlling for the two other conditions and maternal age, maternal race, insurance, and cesarean delivery (Table 5). A diagnosis of diabetes was associated with a $743 (95% CI: $636 to $850) higher median charge compared to not having a diagnosis of diabetes after controlling for other conditions and characteristics. A high blood pressure diagnosis was associated with a $2,314 (95% CI: $2,194 to $2,434) higher median charge compared to those without a high blood pressure diagnosis after controlling for other conditions and characteristics.
Table 5.
Univariate (Crude) and Multivariable (Adjusted*) Analyses of Total Hospital Charges Among Those with and Without Selected Chronic Diseases, HHIC*, 2003–2008
| Univariate Analysis | Multivariable Analysis** | |||
| Parameter | β† | 95% CI*** | β† | 95% CI |
| Intercept | - | - | 7,552 | (7,379 – 7,726) |
| Asthma | ||||
| Yes | 1,070 | (903 – 1,237) | 999 | (886 – 1,112) |
| No | Reference | Reference | ||
| Diabetes | ||||
| Yes | 1,853 | (1,727 – 1,979) | 743 | (636 – 850) |
| No | Reference | Reference | ||
| High Blood Pressure | ||||
| Yes | 3,010 | (2,836 – 3,184) | 2,314 | (2,194 – 2,434) |
| No | Reference | Reference | ||
Note: HHIC represents data from the Hawai‘i Health Information Corporation.
Regression coefficients are derived from median regression analysis.
Adjusted for Age group, Race group, Maternal Insurance, and Cesarean Section.
95% CI refers to the 95% Confidence Interval
Discussion
This study highlighted that nearly 1 in 10 women who delivered a baby in Hawai‘i have a diagnosis of high blood pressure, about 1 in 12 have a diagnosis of diabetes, and about 1 in 25 have a diagnosis of asthma as reflected in hospital discharge delivery record. Further, these women had more adverse birth outcomes and higher hospital charges compared to those without one of these conditions. The burden of chronic disease among women of reproductive age is expected to increase, particularly with the rise in chronic disease in younger populations. Efforts to promote healthy lifestyle choices can prevent or delay the development of disease throughout the life course. Efforts focused among women of reproductive age have the potential to also improve reproductive health outcomes.
There is a growing awareness of asthma and potential links to health and quality of life in the general population. The prevalence of ever being diagnosed with asthma in the general population of US women of reproductive age (18–44 years) in 2009 was estimated to be 16.2%, an increase of 20% since 2001.3 Estimates for current asthma in women of reproductive age in Hawai‘i from 2010 Behavioral Risk Factor Surveillance System (BRFSS) data was 13.3% compared to 21.3% for ever being diagnosed with asthma, which are both significantly higher than national estimates.37 The estimates from hospital discharge delivery records are much lower when compared to estimates of both current and having ever been diagnosed with asthma and may be related to under-reporting of the condition in this administrative record. Women with an asthma diagnosis in the hospital discharge delivery records may represent those with more severe disease than other mothers who had milder forms of asthma. Additionally, unlike chronic high blood pressure and chronic diabetes, there is no specific pregnancy related diagnostic code for asthma, which may also contribute to under-reporting of this disease. Estimates from Hawai‘i BRFSS data show the highest levels of asthma among women of reproductive age in Hawai‘i County,37 whereas this study revealed the highest level in Honolulu County, so there may also be some differential reporting of asthma in hospital discharge delivery records related to geography. The relationship between maternal asthma and low birth weight represents a possible explanation for the higher hospital charges compared to those without asthma. This is consistent with some of the general literature showing associations between asthma and low birth weight.10,38 Of the three birth outcomes examined comparing those with to those without Asthma, there was only a significant difference in low birth weight. Thus, the finding of higher hospital charges for those with asthma compared to those with diabetes, which is associated with all three adverse birth outcomes, was unexpected and highlights that charges are likely not just related to increased adverse birth outcomes.
A diagnosis of diabetes was listed in 7.7% of the hospital discharge delivery records in our study, which is consistent with the general literature and highlights that diabetes diagnoses may be well captured by the data. Estimates in the general population of women of reproductive age, using BRFSS data, highlighted that 5.8% reported having had either chronic or gestational diabetes in 2008 and that 2.9% had chronic diabetes in 2009.3,39 A population limited to those who are pregnant would explain the higher estimates of diabetes when compared to all women of reproductive age. Of the three adverse birth outcomes examined, there were significant differences between mothers with compared to those without diabetes among all of them (high birth weight, low birth weight, and cesarean delivery). Thus, the increased costs found in this study were expected as these outcomes are likely associated with higher hospital charges. Women diagnosed with gestational diabetes have a seven-fold greater risk of developing chronic diabetes later in life, compared to those who did not have gestational diabetes.30 Even those with just an abnormal glucose screen in pregnancy (but normal follow up testing for gestational diabetes) are at increased risk for development of diabetes later in life.31 Although nearly all the diagnoses in our study (88.%) were related to the pregnancy specific billing codes,the increase risk of developing chronic diabetes among those with pregnancy related diabetes highlights the importance of ensuring that these women have appropriate treatment during pregnancy and follow up after delivery. Diabetes identified during pregnancy appears to be an early clinical marker of risk, and appropriate follow up in the postpartum period may help decrease the burden of disease. The American Diabetes Association recommends that mothers who had gestational diabetes be screened six to twelve weeks postpartum and then every three years to identify as early as possible those who develop chronic diabetes.40
High blood pressure was diagnosed in 9.2% of all hospital deliveries, which is also consistent with the general literature. A recent clinical review highlighted that 5–10% of all pregnancies are affected by hypertensive disorders (all subtypes) and that these hypertensive disorders in pregnancy were associated with severe morbidity as well as increased maternal, fetal, and infant mortality.41 The variation by race group shown in our study is consistent with that seen in the general adult population for Hawai‘i with Hawaiian and Filipino race groups having the highest rates of diagnosed high blood pressure.42 Those with high blood pressure diagnoses accounted for the highest charges of the three chronic conditions evaluated in this paper and were consistent across delivery type with the highest median charges in both cesarean and vaginal delivery. Associations among high blood pressure, low birth weight, and cesarean delivery provide a likely explanation for the increased overall charges found among affected women. High blood pressure during pregnancy is increasingly being recognized to have long-term adverse consequences to mothers and children.28,29 A recent review showed a nearly 4-fold greater risk of hypertensive disease at a mean of 14 years after pregnancy among those with preeclampsia compared to those who had normal blood pressure during pregnancy.29 Although nearly all the diagnoses in our study (75%) were related to the pregnancy billing codes, the increase risk of developing chronic hypertension among those with pregnancy related high blood pressure highlights the importance of ensuring that these women have appropriate treatment during pregnancy and follow up after delivery. High blood pressure identified during pregnancy appears to be an early clinical marker of cardiovascular risk, and appropriate follow up in the postpartum period may help decrease the burden of heart disease. The American Heart Association Effectiveness Based Guidelines for the Prevention of Cardiovascular Disease in Women identifies women with a history of pre-eclampsia, gestational diabetes, or pregnancy related hypertension to have a major risk factor for cardiovascular disease and supports the importance of appropriate follow up in these women postpartum.43
Clinical visits such as those related to preconception and interconception services provide opportunities to help address chronic conditions among women who have had or are planning a pregnancy. The vast majority of those with high blood pressure and diabetes did not have a diagnosis prior to pregnancy. This finding reinforces the importance of providing appropriate education in the interconception period related to the increase risks of developing chronic disease. With the appropriate training, clinicians can use these opportunities to promote healthy lifestyles which could lead to reductions in adverse reproductive outcomes,44–46 as well as reductions in the development and morbidity associated with chronic disease.47 Additionally, population level efforts, such as the CDC Healthy Communities Program, could help reduce the burden of chronic disease and achieve health equity in 52 state and territorial health departments and 331 communities nationwide through sustainable change where people live, learn, work and play.48 The Healthy Communities Program focuses on healthy choices related to tobacco, physical inactivity, and unhealthy eating which are also likely to improve reproductive outcomes by promoting these same health behaviors in women of reproductive age.
The findings in this report are subject to at least six limitations. First, hospital discharge data is an administrative data set and may under-estimate the prevalence of maternal chronic conditions compared to clinical records if the data are not in the hospital record used to generate the billing codes as shown for diabetes and other chronic conditions.25,49,50 Thus actual medical records, including outpatient records, may be more appropriate for a true surveillance of chronic disease in pregnancy. Secondly, each maternal condition was treated independently in the base analysis and does not account for the potential of clustering of these conditions which could potentially explain some of the differences seen between the conditions, but the sample sizes to investigate this clustering were not sufficient in this data set. However, the inclusion of all three conditions in the median regression analysis did partly account for this possibility by the inclusion of all three conditions in the model simultaneously. Third, the associations seen with diabetes and high blood pressure represents those for the aggregated measures including those with the chronic condition prior to the pregnancy compared to those who developed the condition associated with the pregnancy. Despite the increased risk for long term chronic disease in those with pregnancy associated conditions, there could be differential outcomes if the conditions are disaggregated which may lead to an under or over estimation of the actual hospital charges and other birth outcomes evaluated in this study. The focus of this study was to evaluate the impact of these aggregated measures so this differential was not assessed within the framework of this analysis, but highlights some potential areas for future work. Fourth, we could not examine the actual level, treatment, or control of these conditions (eg, changes in diabetes, high blood pressure, or asthma over time due to behavioral and pharmacological means) that could influence the impact on the pregnancy and contribute to birth outcomes. Additionally, the available demographic data are limited in detail, particularly as related to racial identification and other measures that are often associated with adverse birth outcomes. For example, one hospital, whose births comprise approximately 15% of state births, does not report information about race; hence, the race for mothers giving birth there was classified “Other.” Some other measures that could not be addressed in the analysis include the social determinants of health, such as education, employment, social support, and living environments that may result from long-term health inequalities.51 Lastly, the true burden of the impact of these conditions should include assessment for any longitudinal outcomes such as increased morbidity and mortality that may result after the hospital admission for birth, which are not available within the data used for this analysis.
Additional analysis could evaluate the increased costs associated with asthma and the inter-relations between these chronic conditions and their associations with both adverse birth outcomes, but also longitudinally evaluate the increased utilization of health services in those identified initially with chronic conditions or their strong risk factors during pregnancy. The collection of more information related to specific subpopulations could allow a better assessment of variation and disparities among groups such as within the Asian and Pacific Islander subgroups. Addressing risk factors by encouraging healthy lifestyle choices throughout the lifespan and in multiple settings will likely lead to reductions in the severity of chronic diseases, improve the quality of life for individuals, and also promote healthy pregnancy outcomes. Ensuring that women who are diagnosed with pregnancy related diabetes and high blood pressure receive appropriate postpartum care as recommended by the American Heart Association and the American Diabetes Association are important foci, and can contribute to other multi-disciplinary approaches emphasizing chronic disease prevention at every age. However, it will be important to monitor the effectiveness of these initiatives to reduce chronic disease and improve birth outcomes through appropriate evaluation to assess the impact of these interventions. An increased awareness of the impact of these conditions on both adverse birth outcomes and the development of chronic disease is needed.
Figure 2.
Proportion of High Birth Weight (>4,500 grams), Overall and by Chronic Condition Conditions. Hawai‘i Health Information Corporation, 2003–2008 Singleton Births.
Acknowledgment
The authors would like to acknowledge the Hawai‘i Health Information Corporation, particularly Jill Miyamura, for making the data available to researchers. The authors also appreciate the assistance from Cheryl Prince, Dave Goodman, and Charlan Kroelinger from the Maternal and Child Health Epidemiology Program, Applied Sciences Branch, Division of Reproductive Health, National Center for Chronic Disease Prevention and Public Health Promotion, Centers for Disease Control and Prevention, for scientific guidance on this analysis and manuscript.
Conflict of Interest
None of the authors identify a conflict of interest.
Disclaimer
The findings and conclusions in this article are those of the authors and do not represent the official position of the Centers for Disease Control and Prevention or the Hawaii Department of Health.
References
- 1.Hardy GE. The burden of chronic disease: the future is prevention. Introduction to Dr. James Marks' presentation, “The Burden of Chronic Disease and the Future of Public Health”. Prev Chronic Dis. 2004 Apr;1(2):A04. [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention, author. Chronic Disease Prevention and Health Promotion. 2012. [January 18 2013]. http://www.cdc.gov/chronicdisease/overview/index.htm.
- 3.Hayes DK, Fan AZ, Smith RA, Bombard JM. Trends in selected chronic conditions and behavioral risk factors among women of reproductive age, behavioral risk factor surveillance system, 2001–2009. Prev Chronic Dis. 2011 Nov;8(6):A120. [PMC free article] [PubMed] [Google Scholar]
- 4.Ahluwalia IB, Mack KA, Mokdad A. Report from the CDC. Changes in selected chronic disease-related risks and health conditions for nonpregnant women 18–44 years old BRFSS. J Womens Health (Larchmt) 2005 Jun;14(5):382–386. [Google Scholar]
- 5.Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001 Mar;91(3):436–440. doi: 10.2105/ajph.91.3.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Catov JM, Nohr EA, Olsen J, Ness RB. Chronic hypertension related to risk for preterm and term small for gestational age births. Obstet Gynecol. 2008 Aug;112(2 Pt 1):290–296. doi: 10.1097/AOG.0b013e31817f589b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004 Feb;103(2):219–224. doi: 10.1097/01.AOG.0000107291.46159.00. [DOI] [PubMed] [Google Scholar]
- 8.Chappell LC, Enye S, Seed P, Briley AL, Poston L, Shennan AH. Adverse perinatal outcomes and risk factors for preeclampsia in women with chronic hypertension: a prospective study. Hypertension. 2008 Apr;51(4):1002–1009. doi: 10.1161/HYPERTENSIONAHA.107.107565. [DOI] [PubMed] [Google Scholar]
- 9.Chu SY, Bachman DJ, Callaghan WM, et al. Association between obesity during pregnancy and increased use of health care. N Engl J Med. 2008 Apr 3;358(14):1444–1453. doi: 10.1056/NEJMoa0706786. [DOI] [PubMed] [Google Scholar]
- 10.Clifton V. Maternal asthma during pregnancy and fetal outcomes: potential mechanisms and possible solutions. Curr Opin Allergy Clin Immunol. 2006 Oct;6(5):307–311. doi: 10.1097/01.all.0000244788.28789.dd. [DOI] [PubMed] [Google Scholar]
- 11.Ehrenberg HM, Durnwald CP, Catalano P, Mercer BM. The influence of obesity and diabetes on the risk of cesarean delivery. Am J Obstet Gynecol. 2004 Sep;191(3):969–974. doi: 10.1016/j.ajog.2004.06.057. [DOI] [PubMed] [Google Scholar]
- 12.Enriquez R, Griffin MR, Carroll KN, et al. Effect of maternal asthma and asthma control on pregnancy and perinatal outcomes. J Allergy Clin Immunol. 2007 Sep;120(3):625–630. doi: 10.1016/j.jaci.2007.05.044. [DOI] [PubMed] [Google Scholar]
- 13.Gessner BD, Chimonas MA. Asthma is associated with preterm birth but not with small for gestational age status among a population-based cohort of Medicaid-enrolled children <10 years of age. Thorax. 2007 Mar;62(3):231–236. doi: 10.1136/thx.2005.053363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacMullen NJ, Tymkow C, Shen JJ. Adverse maternal outcomes in women with asthma: differences by race. MCN Am J Matern Child Nurs. 2006 Jul-Aug;31(4):263–268. doi: 10.1097/00005721-200607000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Lu GC, Rouse DJ, DuBard M, Cliver S, Kimberlin D, Hauth JC. The effect of the increasing prevalence of maternal obesity on perinatal morbidity. Am J Obstet Gynecol. 2001 Oct;185(4):845–849. doi: 10.1067/mob.2001.117351. [DOI] [PubMed] [Google Scholar]
- 16.Graham J, Zhang L, Schwalberg R. Association of maternal chronic disease and negative birth outcomes in a non-Hispanic Black-White Mississippi birth cohort. Public Health Nurs. 2007 Jul-Aug;24(4):311–317. doi: 10.1111/j.1525-1446.2007.00639.x. [DOI] [PubMed] [Google Scholar]
- 17.Matthews TJ, Hamilton BE. Delayed childbearing: more women are having their first child later in life. NCHS Data Brief. 2009 Aug;(21):1–8. [PubMed] [Google Scholar]
- 18.Ventura SJ, Curtin SC, Abma JC, Henshaw SK. Estimated pregnancy rates and rates of pregnancy outcomes for the United States, 1990–2008. Natl Vital Stat Rep. 2012 Jun;60(7):1–22. [PubMed] [Google Scholar]
- 19.Peipert JF, Bracken MB. Maternal age: an independent risk factor for cesarean delivery. Obstet Gynecol. 1993 Feb;81(2):200–205. [PubMed] [Google Scholar]
- 20.Chang J, Elam-Evans LD, Berg CJ, et al. Pregnancy-related mortality surveillance--United States 1991–1999. MMWR Surveill Summ. 2003 Feb;52(2):1–8. [PubMed] [Google Scholar]
- 21.Naeye RL. Maternal age, obstetric complications, and the outcome of pregnancy. Obstet Gynecol. 1983 Feb;61(2):210–216. [PubMed] [Google Scholar]
- 22.Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008 Apr;19(3):227–256. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mau MK, Sinclair K, Saito EP, Baumhofer KN, Kaholokula JK. Cardiometabolic health disparities in native Hawaiians and other Pacific Islanders. Epidemiol Rev. 2009;31:113–129. doi: 10.1093/ajerev/mxp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Northam S, Knapp TR. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs. 2006 Jan-Feb;35(1):3–12. doi: 10.1111/j.1552-6909.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- 25.Devlin HM, Desai J, Walaszek A. Reviewing performance of birth certificate and hospital discharge data to identify births complicated by maternal diabetes. Matern Child Health J. 2009 Sep;13(5):660–666. doi: 10.1007/s10995-008-0390-9. [DOI] [PubMed] [Google Scholar]
- 26.Zollinger TW, Przybylski MJ, Gamache RE. Reliability of Indiana birth certificate data compared to medical records. Ann Epidemiol. 2006 Jan;16(1):1–10. doi: 10.1016/j.annepidem.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 27.Robbins CL, Dietz PM, Bombard J, Valderrama AL. Gestational hypertension: a neglected cardiovascular disease risk marker. Am J Obstet Gynecol. 2011 Apr;204(4):336.e331–339. doi: 10.1016/j.ajog.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 28.Smith GN, Walker MC, Liu A, et al. A history of preeclampsia identifies women who have underlying cardiovascular risk factors. Am J Obstet Gynecol. 2009 Jan;200(1):58.e51–58. doi: 10.1016/j.ajog.2008.06.035. [DOI] [PubMed] [Google Scholar]
- 29.Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007 Nov;335(7627):974. doi: 10.1136/bmj.39335.385301.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009 May;373(9677):1773–1779. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 31.Retnakaran R. Glucose tolerance status in pregnancy: a window to the future risk of diabetes and cardiovascular disease in young women. Curr Diabetes Rev. 2009 Nov;5(4):239–244. doi: 10.2174/157339909789804378. [DOI] [PubMed] [Google Scholar]
- 32.Retnakaran R, Qi Y, Connelly PW, Sermer M, Hanley AJ, Zinman B. Risk of early progression to prediabetes or diabetes in women with recent gestational dysglycaemia but normal glucose tolerance at 3-month postpartum. Clin Endocrinol (Oxf) 2010 Oct;73(4):476–483. doi: 10.1111/j.1365-2265.2010.03834.x. [DOI] [PubMed] [Google Scholar]
- 33.Fund UNCs, Organization WH, author. Low Birthweight: County, Regional, and Global Estimates. New York: UNICEF; 2004. [Google Scholar]
- 34.Blanchette H. The rising cesarean delivery rate in America: what are the consequences. Obstet Gynecol. 2011 Sep;118(3):687–690. doi: 10.1097/AOG.0b013e318227b8d9. [DOI] [PubMed] [Google Scholar]
- 35.Clopper C, Pearson E S. The use of confidence intervals or fi ducial limits illustrated in the case of binomial. Biometrika. 1934;26(4):10. [Google Scholar]
- 36.Koenker R, Bassett G. Regression Quantiles. Econometrica. 1978;46(1):18. [Google Scholar]
- 37.(CDC) CfDCaP, author. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: US: Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 38.Almeida ML, Santana PA, Guimarães AM, Gurgel RQ, Vianna EO. Asthma and pregnancy: repercussions for neonates. J Bras Pneumol. 2010 May-Jun;36(3):293–300. doi: 10.1590/s1806-37132010000300005. [DOI] [PubMed] [Google Scholar]
- 39.Denny CH, Floyd RL, Green PP, Hayes DK. Racial and ethnic disparities in preconception risk factors and preconception care. J Womens Health (Larchmt) 2012 Jul;21(7):720–729. doi: 10.1089/jwh.2011.3259. [DOI] [PubMed] [Google Scholar]
- 40.Tovar A, Chasan-Taber L, Eggleston E, Oken E. Postpartum screening for diabetes among women with a history of gestational diabetes mellitus. Prev Chronic Dis. 2011 Nov;8(6):A124. [PMC free article] [PubMed] [Google Scholar]
- 41.Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 2011 Aug;25(4):391–403. doi: 10.1016/j.bpobgyn.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 42.Hawaii Health Data Warehouse. http://hhdw.org.
- 43.Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women--2011 update: a guideline from the american heart association. Circulation. 2011 Mar;123(11):1243–1262. doi: 10.1161/CIR.0b013e31820faaf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moos MK, Dunlop AL, Jack BW, et al. Healthier women, healthier reproductive outcomes: recommendations for the routine care of all women of reproductive age. Am J Obstet Gynecol. 2008 Dec;199(6 Suppl 2):S280–289. doi: 10.1016/j.ajog.2008.08.060. [DOI] [PubMed] [Google Scholar]
- 45.Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care--United States A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006 Apr;55(RR-6):1–23. [PubMed] [Google Scholar]
- 46.Elsinga J, de Jong-Potjer LC, van der Pal-de Bruin KM, le Cessie S, Assendelft WJ, Buitendijk SE. The effect of preconception counselling on lifestyle and other behaviour before and during pregnancy. Womens Health Issues. 2008 Nov-Dec;18(6 Suppl):S117–125. doi: 10.1016/j.whi.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 47.Ehrenthal DB, Núñez AE, O'Neill E, Robertson-James C, Addo SF, Stewart A. The role of the obstetrician/gynecologist in the prevention of cardiovascular disease in women. Womens Health Issues. 2011 Sep-Oct;21(5):338–344M. doi: 10.1016/j.whi.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention, author. Healthy Communities Program. 2012. [Jan 15, 2013]. http://www. cdc.gov/healthycommunitiesprogram/
- 49.Hadfield RM, Lain SJ, Cameron CA, Bell JC, Morris JM, Roberts CL. The prevalence of maternal medical conditions during pregnancy and a validation of their reporting in hospital discharge data. Aust N Z J Obstet Gynaecol. 2008 Feb;48(1):78–82. doi: 10.1111/j.1479-828X.2007.00818.x. [DOI] [PubMed] [Google Scholar]
- 50.Lain SJ, Hadfield RM, Raynes-Greenow CH, et al. Quality of data in perinatal population health databases: a systematic review. Med Care. 2012 Apr;50(4):e7–20. doi: 10.1097/MLR.0b013e31821d2b1d. [DOI] [PubMed] [Google Scholar]
- 51.WHO Commission on Social Determinants of Health., World Health Organization, author. Closing the gap in a generation : health equity through action on the social determinants of health : Commission on Social Determinants of Health final report. Geneva, Switzerland: World Health Organization, Commission on Social Determinants of Health; 2008. [Google Scholar]