Abstract
The use of bedside ultrasound in the emergency department has been gaining favor among emergency medicine physicians and can be invaluable in the prompt diagnosis and treatment of acutely ill patients, especially when radiology evaluation is unavailable or delayed. Although pediatric ultrasound examinations are taught in some pediatric residency programs, they are not part of the required pediatric residency curriculum in the United States. This is the first case report of a pediatric resident diagnosing intussusception by bedside ultrasound in a 4-year-old boy under the guidance of a pediatric emergency attending with ultrasound training. This report illustrates the ease of using bedside ultrasound even among early learners and highlights its potential importance in medical education for fellows and residents.
Keywords: intussusception, ultrasound, emergency medicine, medical education, pediatrics, residents, radiology
Introduction
The use of bedside ultrasound in the emergency department (ED) has been increasing among adult emergency medicine physicians and more recently among pediatric emergency medicine physicians. Among pediatric emergency fellowship program directors, 94% have expressed interest in ultrasound skills training,1 with a few pediatric emergency medicine fellowship programs integrating a 2–4 week ultrasound rotation into training.2 There have been increasing reports of the use of bedside ultrasound in pediatric emergency medicine in cases involving pediatric trauma, adolescent pregnancy, and intussusception.3–5
Intussusception occurs when part of the gastrointestinal tract telescopes into an adjacent distal segment and is the most common cause of intestinal obstruction in children between three months and six years of age with an incidence of 38 per 100,000 cases in the first year of life and 31 per 100,000 cases in the second year of life.6 If not promptly diagnosed and treated with enema reduction, intussusception can lead to intestinal necrosis, sepsis, or death.7 The classical presentation of intussusception consists of the triad of colicky abdominal pain, bloody stool (commonly described as “currant jelly”), and vomiting. While the presence of this triad has a positive predictive value of 93% for intussusception, it unfortunately occurs in less than 25% of cases. Many patients instead present with varying combinations of non-specific symptoms including vomiting, abdominal pain, excessive crying, or lethargy and may initially be misdiagnosed with other abdominal and neurological conditions.8,9
While the gold standard for diagnosis of intussusception has been contrast enema, the use of ultrasound has been gaining favor as the initial study choice due to being non-invasive, radiation-free, painless, fast, and relatively low in cost compared to other radiological procedures. If evaluation by a radiologist is delayed or unavailable, a bedside ultrasound performed by a trained physician in the ED can be crucial in reducing the time to diagnosis and definitive treatment. Although the test characteristics of an ultrasound examination for intussusception greatly depend on user experience, multiple international studies have shown that the sensitivity and specificity of ultrasound are high and range between 96.6% to 100% and 88% to 100%, respectively.7,10–13 Studies of radiology residents and emergency medicine physicians have suggested that the technique is relatively easy and can be taught quickly.14 This is the first case report of a pediatric resident (KWR) with no prior radiology training successfully performing bedside ultrasound for intussusception.
Case Report
A previously healthy 4-year-old boy presented to an ED with a two day history of abdominal pain and non-bilious, non bloody vomiting. He was given a suppository for suspected constipation that resulted in a non-bloody bowel movement and relief of pain. However, he returned to the ED the following day due to worsening abdominal pain occurring every 5 to 20 minutes. An ultrasound was performed and read by the radiologist as positive for intussusception. The patient was transferred to a tertiary pediatric facility where he was seen by a third year pediatric resident (KWR). His examination revealed a soft and non-distended abdomen with audible bowel sounds. He had tenderness in the right lower quadrant but no palpable mass. The rest of the exam was unremarkable. Intravenous fluids were started and morphine was given for pain control. The transferred patient did not arrive with any radiographic images from the referring ED. Under guidance from a pediatric emergency medicine attending trained in pediatric ultrasound, the pediatric resident performed a bedside ultrasound for intussusception for her first time and was able to obtain images of the target sign and the hayfork sign typical of intussusception (Figures 1 and 2). An ultrasound read by the radiologist confirmed the diagnosis of ileocolic intussusception, which was successfully reduced with contrast enema with gastrografin. The patient was admitted for overnight observation per protocol and was discharged the following day without complications.
Figure 1.
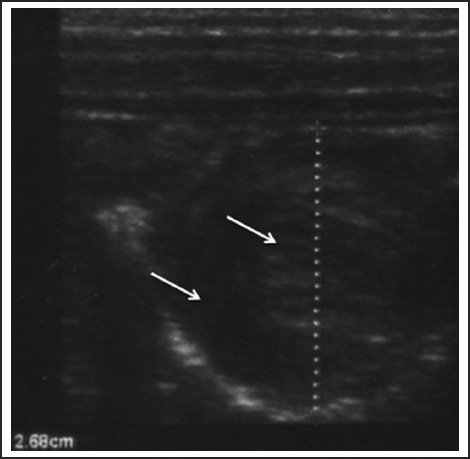
Transverse view through the right mid abdomen showing the target or bulls eye sign characteristic of intussusception, which is formed by a hypoechoic ring (between the two arrows) from the edematous walls of the intusscipiens around an echo-dense center of the intussuceptum.
Figure 2.
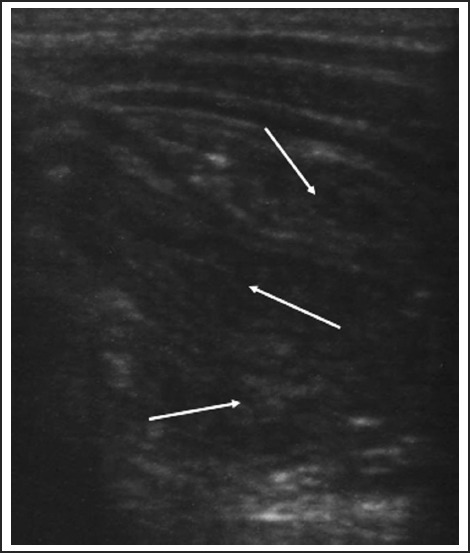
Longitudinal view showing the hayfork sign representing the apex of the intussusception. The hayfork sign is formed by three parallel hypoechoic areas (demonstrated by the three arrows) separated by hyperechoic zones, which represents the dilated intussucipiens containing the intussuceptum, and is considered pathognomonic for intussusception.
Discussion
Intussusception has a characteristic appearance on ultrasound. Using warm gel and a 10 MHz linear transducer, the examiner begins the ultrasound exam at the cecum in the right lower quadrant of the abdomen and gradually moves proximally toward the right upper quadrant while aligning the transducer in a transverse orientation to the colon until the area of intussusception is encountered; this area sometimes presents as a palpable mass.6,10 On longitudinal view, the characteristic hayfork or sandwich sign is formed by three parallel hypoechoic areas separated by hyperechoic zones. These zones represent the dilated intussucipiens containing the intussuceptum and is considered pathognomonic for intussusception.15 Alternatively, the appearance of a pseudokidney sign is formed if the intussusception is curved and when the mesentery is seen on only one side of the intussusceptum.16 The pseudokidney sign is most commonly seen on long-axis view.17 On axial view, there is a hypoechoic ring from the edematous walls of the intussuscipiens around an echo-dense center formed by the interfaces of the mucosal and serosal layers of the intussusceptum. This characteristic sign, which goes by several names including bulls eye sign, target sign, donut sign, or concentric ring sign, may also be seen in normal intestinal loops and with space-occupying lesions.16
With its characteristic appearance on ultrasound, the diagnosis of intussusception using ultrasound has been taught successfully to physicians and other healthcare providers after relatively brief teaching sessions. Since timely diagnosis and treatment is essential in preventing the complications of intussusception, such skills are invaluable to healthcare providers working on overnight hospital shifts, in remote community health centers, in third world countries, or in other situations where radiology services are not readily available. The value of teaching bedside ultrasound diagnosis of intussusception to local physicians and nurse practitioners in resource poor settings without access to radiology services has been recognized in several international case reports.18,19
There has also been growing interest in bedside ultrasound training for pediatric emergency physicians and fellows due to the reported ease of use and high sensitivity in early learners. One study showed that six pediatric emergency medicine physicians who completed a one hour long course in bedside ultrasound were able to perform the exam with a sensitivity of 85%, specificity of 97%, positive predictive value of 85%, and negative predictive value of 97% for diagnosing intussusception.6 Another study found that a month long training course in bedside ultrasound examination enabled five pediatric emergency medicine physicians to perform bedside ultrasound with a similar positive predictive value for intussusception compared to ultrasound performed by trained gastroenterologists.20 These studies show that different approaches can be used to teach novice learners how to diagnose intussusception with ultrasound. These approaches provide physicians the benefit of a rapid diagnosis, resulting in timely treatment and reduced length of stay in the ED—benefits that were also emphasized in this study as well as in other case reports of bedside ultrasound by emergency medicine physicians.21
Our case report illustrates that ultrasound applications may also be quickly taught to general pediatric residents working in the ED. Although pediatric ultrasound examinations may be taught in some pediatric residency programs, they are not part of the required curriculum in United States general pediatrics residency programs.22 Since 2010, University of Hawai‘i pediatric residents have been taught bedside ultrasound skills during their residency while rotating in the pediatric ED. The focus during the second year of residency consists of didactic lectures, hands-on teaching with pediatric patients, understanding the layout of the ultrasound machine and the different transducers, and becoming familiar with the concepts of [ultrasound] frequency, depth, and gain effect. Simple bedside ultrasound exams such as bladder volume evaluation prior to urethral catheterization and abscesses and foreign body identification are taught by an RDMS certified pediatric emergency physician. During the third year of residency, pediatric residents are taught more advanced pediatric emergency bedside ultrasound applications such as evaluation of pneumothorax, hip effusion, hydronephrosis, abdominal pathology, and confirmation of successful intubation. Education in the use of bedside ultrasound may be a valuable experience for pediatric residents going into primary care, subspecialties, global health, or hospital medicine, as illustrated by our case report. There may be a growing role for ultrasound training within the medical education curriculum for all pediatric residents.
Conflict of Interest
None of the authors identify any conflict of interest.
References
- 1.Chen L, Santucci KA. Probing the availability of emergency ultrasound in pediatrics. Pediatric Emergency Care. 2006;22(9):688. [Google Scholar]
- 2.Ramirez-Schrempp D, Dorfman DH, Tien I, Liteplo AS. Bedside ultrasound in pediatric emergency medicine fellowship programs in the United States: little formal training. Pediatr Emerg Care. 2008 Oct;24(10):664–667. doi: 10.1097/PEC.0b013e3181884955. [DOI] [PubMed] [Google Scholar]
- 3.Chen L, Baker MD. Novel applications of ultrasound in pediatric emergency medicine. Pediatr Emerg Care. 2007 Feb;23(2):115–123. doi: 10.1097/PEC.0b013e3180302c59. [DOI] [PubMed] [Google Scholar]
- 4.Halm BM, Boychuk RB, Franke AA. Diagnosis of intussusception using point-of-care ultrasound in the pediatric ED: a case report. Am J Emerg Med. 2011 Mar;29(3):354 e351–354 e353. doi: 10.1016/j.ajem.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 5.Kairam N, Kaiafis C, Shih R. Diagnosis of pediatric intussusception by an emergency physician-performed bedside ultrasound: a case report. Pediatr Emerg Care. 2009 Mar;25(3):177–180. doi: 10.1097/PEC.0b013e31819a8a46. [DOI] [PubMed] [Google Scholar]
- 6.Riera A, Hsiao AL, Langhan ML, Goodman TR, Chen L. Diagnosis of intussusception by physician novice sonographers in the emergency department. Ann Emerg Med. 2012 Sep;60(3):264–268. doi: 10.1016/j.annemergmed.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiFiore JW. Intussusception. Seminars in Pediaric Surgery. 1999 Nov;8(4):214–220. doi: 10.1016/s1055-8586(99)70029-6. [DOI] [PubMed] [Google Scholar]
- 8.Lai AH, Phua KB, Teo EL, Jacobsen AS. Intussusception: a three-year review. Ann Acad Med Singapore. 2002;31(1):81–85. [PubMed] [Google Scholar]
- 9.Harrington L, Connolly B, Hu X, Wesson DE, Babyn P, Schuh S. Ultrasonographic and clinical predictors of intussusception. The Journal of Pediatrics. 1998;132(5):836–839. doi: 10.1016/s0022-3476(98)70314-2. [DOI] [PubMed] [Google Scholar]
- 10.Hofman V, Deeg KH, Hoyer PF. Ultraschaldiagnostik in Paediatrie und Kinderheikunde Lehrbuch und Atlas. Stuttgart, Germany: Thieme; 2005. [Google Scholar]
- 11.Hryhorczuk AL, Strouse PJ. Validation of US as a first-line diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol. 2009 Oct;39(10):1075–1079. doi: 10.1007/s00247-009-1353-z. [DOI] [PubMed] [Google Scholar]
- 12.Justice FA, de Campo M, Liem NT, Son TN, Ninh TP, Bines JE. Accuracy of ultrasonography for the diagnosis of intussusception in infants in Vietnam. Pediatr Radiol. 2007 Feb;37(2):195–199. doi: 10.1007/s00247-006-0381-1. [DOI] [PubMed] [Google Scholar]
- 13.Mandeville K, Chien M, Willyerd FA, Mandell G, Hostetler MA, Bulloch B. Intussusception: clinical presentations and imaging characteristics. Pediatr Emerg Care. 2012 Sep;28(9):842–844. doi: 10.1097/PEC.0b013e318267a75e. [DOI] [PubMed] [Google Scholar]
- 14.Eshed I, Gorenstein A, Serour F, Witzling M. Intussusception in children: can we rely on screening sonography performed by junior residents? Pediatric Radiology. 2004 Feb;34(2):134–137. doi: 10.1007/s00247-003-1089-0. [DOI] [PubMed] [Google Scholar]
- 15.Alessi V, Salerno G. The “hay-fork” sign in the ultrasonographic diagnosis of intussusception. Gastrointest Radiol. 1985;10(2):177–179. doi: 10.1007/BF01893097. [DOI] [PubMed] [Google Scholar]
- 16.del-Pozo G, Albillos JC, Tejedor D, et al. Intussusception in children: current concepts in diagnosis and enema reduction. Radiographics. 1999 Mar-Apr;19(2):299–319. doi: 10.1148/radiographics.19.2.g99mr14299. [DOI] [PubMed] [Google Scholar]
- 17.Halm B, Foster J. Chapter 26. Paroxysmal abdominal pain and vomiting in a 7-month-old boy. Cambridge University Press; 2013. Case studies in pediatric emergency and critical care ultrasound. [Google Scholar]
- 18.Gingrich AS, Saul T, Lewiss RE. Point-of-care ultrasound in a resource-limited setting: diagnosing intussusception. J Emerg Med. 2013 Sep;45(3):e67–e70. doi: 10.1016/j.jemermed.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 19.Stolz LA, Kizza H, Little K, Kasekende J. Intussusception detected with ultrasound in a resource-limited setting. Lancet. 2013 Jun 8;381(9882):2054. doi: 10.1016/S0140-6736(13)60690-X. [DOI] [PubMed] [Google Scholar]
- 20.Chang YJ, Hsia SH, Chao HC. Emergency medicine physicians performed ultrasound for pediatric intussusceptions. Biomed J. 2013 Jul-Aug;36(4):175–178. doi: 10.4103/2319-4170.112739. [DOI] [PubMed] [Google Scholar]
- 21.Halm BM. Reducing the time in making the diagnosis and improving workflow with point-of-care ultrasound. Pediatr Emerg Care. 2013 Feb;29(2):218–221. doi: 10.1097/PEC.0b013e318280d698. [DOI] [PubMed] [Google Scholar]
- 22.Accreditation Council for Graduate Medical Education, author. ACGME Program Requirements for Graduate Medical Education in Pediatrics. [July 1, 2013]. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf.


