Abstract
Background: Adrenal myelolipoma (AM) is a benign lesion for which adrenalectomy is infrequently indicated. We investigated operative indications and outcomes for AM in a large single-institution series.
Subjects and Methods: A retrospective cohort study of prospectively collected data was conducted. Patients (≥16 years of age) who underwent adrenalectomy in the Division of General Surgery at Barnes-Jewish Hospital (1993–2010) were grouped by operative indication (myelolipoma versus other pathology) and compared using nonparametric tests (α<0.05).
Results: Sixteen patients (4.0%) had myelolipomas resected out of 402 patients who underwent adrenalectomy. Fourteen patients with suspected AM underwent adrenalectomy, 13 (93%) of whom had AM confirmed on pathology. Indications for adrenalectomy were abdominal or flank pain, large tumor size (>8 cm), atypical radiologic appearance, and/or inferior vena cava compression. Three patients with suspected other adrenal lesions had AM confirmed on final pathology. Operative approach was laparoscopic in 15 cases and open in 1 case of a 21-cm lesion. Patients who underwent laparoscopic adrenalectomy for AM (n=15) or other adrenal pathology (n=343) were similar with respect to age, gender, American Society of Anesthesiologists classification, prior abdominal operation, tumor side, operative time, conversion rate, estimated blood loss, intraoperative complications, hospital length of stay, and 30-day morbidity. However, patients with resected AM had a higher body mass index (36.5±8.1 kg/m2 versus 30.1±7.5 kg/m2; P<.01) and a larger preoperative tumor size (8.4±3.0 cm versus 3.1±1.7 cm; P<.01).
Conclusions: Laparoscopic adrenalectomy may be appropriate for patients with a presumptive diagnosis of AM and abdominal or flank pain, large tumor size, and/or uncertain diagnosis after imaging. Outcomes and morbidity following LA for AM and other adrenal pathology appear comparable.
Background
Adrenal myelolipoma (AM) is a benign tumor of mature adipose and variable amounts of hematopoietic tissues. The majority of AM cases are found incidentally by imaging studies performed for other reasons or at autopsy and are recognizable by the detection of macroscopic fat within adrenal tissue.1 According to Olsson et al.,2 the incidence of myelolipoma at autopsy ranges from 0.08% to 0.4%. Males and females are affected equally, and the peak age range at diagnosis is between 50 and 70 years of age.3 Although most AMs are small and asymptomatic, larger tumors may present with symptoms ranging from nonspecific abdominal pain to spontaneous retroperitoneal hemorrhage. On imaging, myelolipomatous lesions tend to fall into one of three clinicopathologic patterns: (1) isolated AMs, (2) myelolipoma with hemorrhage (mean diameter, >10 cm), and (3) myelolipomatous foci within other adrenal pathologic conditions.3 Rarely, myelolipomas have also been reported in extra-adrenal sites. Computed tomography (CT) imaging studies show macroscopic fat and calcification with heterogeneous echogenicity due to a nonuniform architecture. Typically, asymptomatic nonhemorrhagic AMs do not require therapy, and surgical excision is only used for symptomatic lesions or those with atypical features or if the diagnosis is unclear.4
Few studies have looked specifically at the indications for surgery for AM. Moreover, this lesion is often underappreciated as a source of adrenal incidentaloma and may be misdiagnosed as a potentially malignant adrenal lesion. The purpose of this study was to review our series of patients with AM who required surgical intervention and to establish the indications for surgery, appropriateness of a laparoscopic approach, and operative outcomes relative to other indications for adrenalectomy.
Subjects and Methods
Subjects
A prospectively maintained registry of all patients who underwent adrenalectomy by the authors was reviewed. From 1993 to 2010, 422 adrenalectomies were performed on 402 patients by surgeons in the Sections of Minimally Invasive Surgery, Endocrine and Oncologic Surgery, and Hepatobiliary-Pancreatic and Gastrointestinal Surgery at Washington University School of Medicine/Barnes-Jewish Hospital (St. Louis, MO), the overall outcomes of which as a group have been previously reported.5 Of 402 cases, 16 patients (4%) underwent adrenalectomy for AM confirmed on final pathology. Data were prospectively collected and used for retrospective cohort analysis under Institutional Review Board approval. Patient characteristics, perioperative variables, and operative approach were recorded.
Variables
Preoperative variables included patient age, gender, body mass index (BMI), American Society of Anesthesiologists score, history of prior abdominal operations, side of the lesion, radiographic tumor size (maximum diameter), tumor functioning status as determined by biochemical evaluation, and indication for operation. Intraoperative variables were total operative time, estimated blood loss, transfusion requirement, ultrasound use, and complications. Postoperative variables were recorded for the period immediately following surgery and up to the 30-day follow-up; they included specimen size, gross and surgical pathology, need for transfusion, hospital length of stay, complication frequency and severity, and overall morbidity and mortality.
Analysis
Patients who underwent laparoscopic adrenalectomy (LA) for AM or other adrenal pathology were compared for differences in characteristics, operative indications, perioperative outcome, and morbidity using nonparametric tests (α=0.05).
Results
Over the study time period, 16 patients with AM underwent adrenalectomy. Indications for adrenalectomy included abdominal or flank pain (44%), tumor diameter >8 cm (50%), atypical radiographic appearance (31%), and inferior vena cava compression (7%) as shown in Table 1. Six cases had multiple indications (38%). Preoperatively, the diagnosis was suspected myelolipoma in all but 3 cases. On imaging, the AMs ranged in size from 2.8 cm to 30 cm, with a mean size of 9.6±6.2 cm. CT was used to identify 12 of the 16 lesions, and magnetic resonance imaging identified the remaining 4 cases. The typical radiologic and gross appearances of AM are shown in Figures 1 and 2. The presence of macroscopic fat, which is diagnostic of this lesion, is seen in Figure 1B (arrows).
Table 1.
Indications for Adrenalectomy
| Number of patients (total n=16) | |
|---|---|
| Abdominal or flank pain | 7 (44%) |
| Tumor diameter greater than 8 cm | 8 (50%) |
| Atypical radiologic appearance | 5 (31%) |
| IVC compression | 1 (7%) |
| Multiple indications | 6 (38%) |
IVC, inferior vena cava.
FIG. 1.
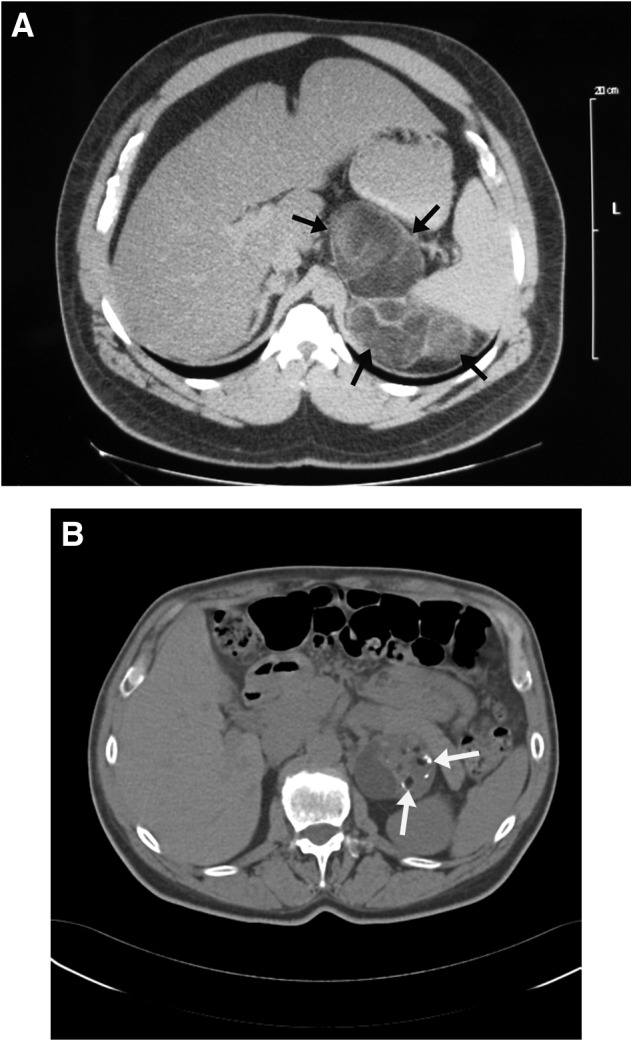
Radiographic computed tomography appearance of left adrenal myelolipomas: (A) a 15-cm myelolipoma with large areas of fat density material (arrows) and (B) a 5.5-cm myelolipoma with several areas of low attenuation (arrows), which represent macroscopic fat.
FIG. 2.
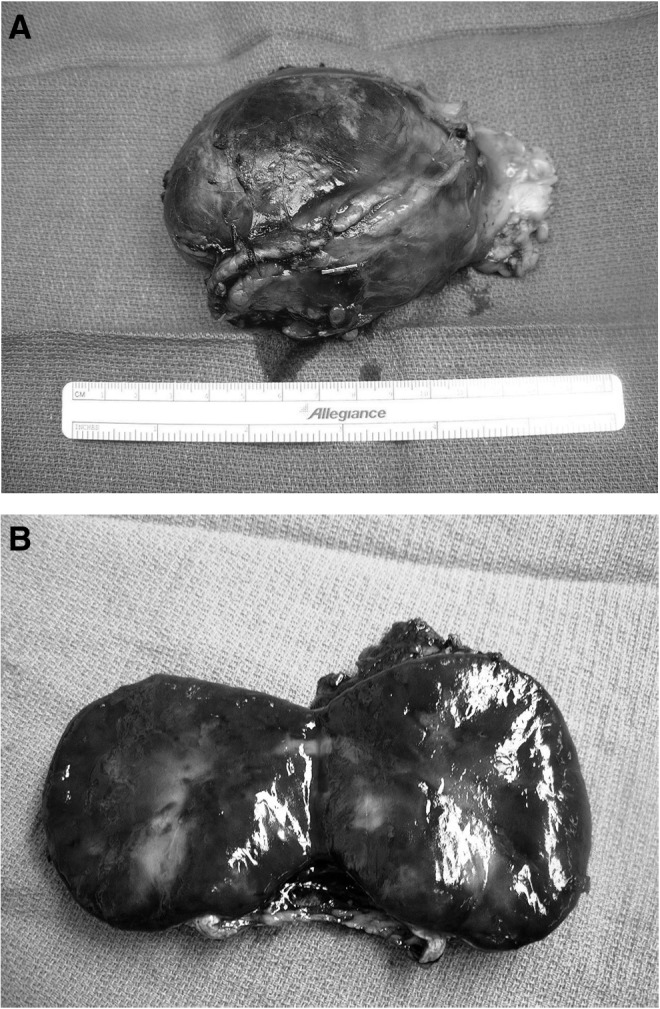
(A) Intact and (B) cut gross appearance of a large adrenal myelolipoma.
Of the 16 cases, 15 were operated on with a laparoscopic technique, including one 15-cm lesion that was removed in a laparoscopic hand-assist fashion. A large left retroperitoneal lesion that measured 30 cm on preoperative imaging and was suspected to be a liposarcoma was removed via an open procedure with en bloc resection of the mass with concomitant nephrectomy, splenectomy, and distal pancreatectomy. Final pathology revealed a 21-cm myelolipoma. The mean patient age was 54 years, with a range of 33 to 76 years. Mean BMI was 35.2±6.1 kg/m2, putting the majority of patients in the obese category, which corresponds to previous case reports. Nine were left-sided AM, and 7 were right-sided. Patients who underwent LA for AM (n=15) were statistically similar to those who underwent LA for other adrenal pathology (n=343) with respect to demographics and operative outcomes as shown in Table 2. There was no difference in gender between the two groups (62% versus 54% female), side of the lesion (54% versus 52% left), prior abdominal surgery (46% versus 46%), or American Society of Anesthesiologists classification (2.2±0.4 versus 2.5±0.6). Compared with patients with other adrenal pathology, patients with AM had a higher BMI (36.5±8.1 kg/m2 versus 30.1±7.5 kg/m2; P<.01) and a larger preoperative tumor size (8.4±3.0 cm versus 3.1±1.7 cm; P<.01). Six of the 13 patients (46%) in whom the BMI was recorded had BMI values ≥39 kg/m2.
Table 2.
Laparoscopic Adrenalectomy Patient Characteristics
| Adrenal myelolipoma (n=15) | Other adrenal pathology (n=343) | |
|---|---|---|
| Demographics | ||
| Age (years) | 51±8.7 | 49.4±14.6 |
| Female | 62% | 54% |
| BMI (kg/m2) | 36.5±8.1a | 30.1±7.5a |
| ASA classification | 2.2±0.4 | 2.5±0.6a |
| Prior abdominal surgery | 46% | 46% |
| Side of lesion (left) | 54% | 52% |
| Preoperative tumor size (cm) (range) | 8.4±3 (2.5–21)a | 3.1±1.7 (0.2–17.5)a |
| Operative outcomes | ||
| Operative time | 160±64.6 | 159±69 |
| Conversion to open | 0% | 6% |
| Estimated blood loss (≤100 mL) | 92% | 81% |
| Intraoperative complications | 0% | 3.5% |
| Length of stay (days) | 1.7±0.9 | 2.6±2.2 |
| 30-day morbidity | 6.7% | 11% |
Data are mean±standard deviation values.
Indicates statistically significant difference (P<.01).
ASA, American Society of Anesthesiologists; BMI, body mass index.
No intraoperative complications occurred in these patients. In only 1 case was intraoperative ultrasound used. The average length of stay was 1.7 days. One patient experienced postoperative hypotension that required intensive care unit observation and transfusion of 1 unit of blood but no further intervention. Length of follow-up ranged from 14 to 213 days, and no complications occurred during follow-up.
Discussion
AM is an uncommon lesion that consists of macroscopic fat and hematopoietic precursor cells. It has been proposed that formation of AM may be precipitated by adrenocortical metaplasia of the reticuloendothelial cells of blood capillaries secondary to infection, stress, or necrosis.3,6,7 Most often, they present as “incidentalomas” on imaging obtained for other reasons. Typically, they are unilateral, but bilateral AMs are occasionally seen.8,9 Various imaging modalities are available for detection of AM, including ultrasound, CT, and magnetic resonance imaging. The appearance of AMs is variable because of their heterogeneous composition and presence of fat and myeloid precursors. The majority of AMs do not require treatment; however, large size, possible symptoms, or atypical radiologic appearance merits consideration for adrenalectomy.
The true incidence of myelolipomas of the adrenal has not been systematically analyzed, but recent series place the frequency as high as 10%–15% of incidentally discovered adrenal masses.10 In our own practice, we have seen increasing numbers of these lesions over the last several years, in part because of their relatively large size compared with other adrenal incidentalomas and because of uncertainty about the diagnosis. They are therefore more likely to be referred for surgical evaluation than smaller, benign-appearing cortical adenomas. Indeed, many of the patients referred to us who prove to have a myelolipoma have radiologic reports from outside our institution that describe a “large adrenal mass concerning for malignancy” or similar verbiage with no mention of myelolipoma in the differential diagnosis. Therefore, greater awareness and recognition of AM by primary physicians, radiologists, and surgeons are needed in order to reassure patients and avoid unnecessary adrenalectomy.
Few reports exist of surgical series of adrenalectomy for myelolipoma beyond small case series. In a study of pathologic cases from both surgical and postmortem files over a 30-year period, Lam and Lo11 identified 20 patients with adrenal lipomatous tumors, 11 of which were myelolipomas. Only one malignant tumor was present in this group, which was an 18-cm liposarcoma, which represented 2.6% of primary adrenal tumors in their series. Of the myelolipomas, mean tumor size was 4.3 cm, and the largest AM measured 14.5 cm. Daneshmand and Quek10 reviewed the published literature on AM and recommended removal of lesions >7 cm in diameter because of the risk of rupture, although this remains a rare event. The natural history was studied by Han et al.,4 who followed up 12 patients with serial imaging over 3.2 years; tumor size remained stable in 5 cases, decreased in 2 cases, and increased in 6 (from a mean size of 5.1 cm to 5.6 cm).
AM is principally a radiographic diagnosis, with the hallmark features being a heterogeneous density with the presence of macroscopic fat as shown in Figure 1. This feature is in contrast with cortical adenomas in which the fat is intracellular and which results in a homogeneous low attenuation appearance (<10 Hounsfield units) on noncontrast CT imaging. Because most myelolipomas are referred after CT scanning done for other reasons, magnetic resonance imaging may be useful in delineating the diagnosis for cases in which the imaging appearance is unclear. Adrenalectomy is indicated for patients with pain-related symptoms, large size, or an atypical appearance on imaging. In our series, the indications for adrenalectomy were most commonly ipsilateral abdominal or flank pain, large tumor size (defined as >8 cm), or an atypical radiographic appearance that made the diagnosis uncertain. Six patients had more than one of these indications. None of the patients had had an acute hemorrhagic event. Although such cases have been reported in the literature,12 we have not recommended surgery for asymptomatic patients unless the imaging diagnosis is unclear.
What should be the approach to the patient with myelolipoma once the radiographic diagnosis is clear? Our group would generally recommend at a minimum biochemical screening with fractionated plasma metanephrines to exclude a pheochromocytoma. This step insures that this diagnosis is not considered further; it also is performed because preanesthetic pheochromocytoma exclusion is obligatory for any future non–adrenal-related surgical procedure. Whether these patients should be screened for cortisol dysfunction is debatable. Isolated reports of associated hypersecretion of adrenal hormones has been observed,14–16 but such secretion may be due to the coexistence of a cortical adenoma or pheochromocytoma in addition to the AM.10 Our approach has been to screen with an overnight dexamethasone test only in cases in which there may be clinical suspicion of clinical or subclinical Cushing's syndrome.13 For small myelolipomas no further imaging or testing should be indicated. For AMs 5 cm or larger, one follow-up scan (usually non-contrast adrenal CT) is done at 6–12 months, and if the lesion is stable, no further testing is recommended.
Our series is the first series of this size to report outcomes of LA for AM and the first to compare outcomes with other adrenal tumors. Despite their large size, myelolipomas can usually be removed laparoscopically because they are well encapsulated, are easily mobilized from the surrounding retroperitoneum, and have virtually no risk of recurrence. If a primary adrenal cortical malignancy is suspected, then the same criteria for open versus laparoscopic should be used (i.e., size <7 cm, lack of invasiveness and high level of surgeon experience). The largest AM removed in our series was 21 cm and was approached with an open procedure with en bloc resection of surrounding organs because of the suspicion of a liposarcoma. A 15-cm myelolipoma in a patient with bilateral AMs was removed in a laparoscopic hand-assisted approach. None of the cases was converted to an open procedure, and no patient experienced an intraoperative complication.
Recently, Shen et al.16 reported 8 patients with AM who were treated by retroperitoneal laparoscopic liposuction. Mean tumor size was 10.5 cm and ranged from 8 to 14 cm. Their technique involved making a 1-cm incision on the membrane surface of the AM, suctioning out the lesion under routine suction pressure, and then closing the membrane with a clip. Although no recurrence was observed over 8–77 months of follow-up, no mention was made of whether any residual AM tissue could be seen on follow-up imaging. Whether this technique will have a future role in the surgical approach to AM should await studies in larger numbers of patients with longer follow-up.
A potentially interesting observation in our AM patients is the incidence of obesity. Mean BMI was 36 kg/m2, and most patients were obese; 6 of 13 patients for whom BMI data were available had BMI values >39 kg/m2. These BMI values were also significantly higher than for the rest of our adrenalectomy population. Because fat is a major component of AM, this raises the question of whether AM may be seen more commonly in the era of the obesity epidemic.
In summary, we report one of the largest series of AMs treated surgically to date. Indications for surgery most often include large size, local symptoms of pain, or atypical imaging appearance and uncertainty of the diagnosis. LA results in good outcomes and should be the preferred approach for the select group of AM patients in whom surgical resection is indicated.
Acknowledgments
V.M.G. was supported by training grant T35 NIDDK from the National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
References
- 1.Butori N, Guy F, Collin F, Benet C, Causeret S, Isambert N. Retroperitoneal extra-adrenal myelolipoma: Appearance in CT and MRI. Diagn Interv Imaging 2012;93:e204–e207 [DOI] [PubMed] [Google Scholar]
- 2.Olsson CA, Krane RJ, Klugo RC, Selikowitz SM. Adrenal myelolipoma. Surgery 1973;73:665–670 [PubMed] [Google Scholar]
- 3.Kenney PJ, Wagner BJ, Rao P, Heffess CS. Myelolipoma: CT and pathologic features. Radiology 1998;208:87–95 [DOI] [PubMed] [Google Scholar]
- 4.Han M, Burnett AL, Fishman EK, Marshall FF. The natural history and treatment of adrenal myelolipoma. J Urol 1997;157:1213–1216 [PubMed] [Google Scholar]
- 5.Bittner JB, Gershuni V, Matthews BD, Moley JF, Brunt LM. Risk factors affecting operative approach, conversion, and morbidity: A single institution experience of 4032 cases. Surg Endosc 2013;27:2342–2350 [DOI] [PubMed] [Google Scholar]
- 6.Plaut A. Myelolipoma in the adrenal cortex; myeloadipose structures. Am J Pathol 1958;34:487–515 [PMC free article] [PubMed] [Google Scholar]
- 7.Meaglia JP, Schmidt JD. Natural history of an adrenal myelolipoma. J Urol 1992;147:189–1090 [DOI] [PubMed] [Google Scholar]
- 8.Bishoff JT, Waguespack RL, Lynch SC, May DA, Poremba JA, Hall CR. Bilateral symptomatic adrenal myelolipoma. J Urol 1997;158:1517–1518 [PubMed] [Google Scholar]
- 9.Wrightson WR, Hahm TX, Hutchinson JR, Cheadle W. Bilateral giant adrenal myelolipomas: A case report. Am Surg 2002;68:588–589 [PubMed] [Google Scholar]
- 10.Daneshmand S, Quek ML. Adrenal myelolipoma: Diagnosis and management. Urol J 2006;3:71–74 [PubMed] [Google Scholar]
- 11.Lam KY, Lo CY. Adrenal lipomatous tumours: A 30 year clinico-pathological experience at a single institution. J Clin Pathol 2001;54:707–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bradbury R, Lambrianides AL, OLoughlin B, Manawwar S. Image of the month. Arch Surg 2011;146:1445–1446 [DOI] [PubMed] [Google Scholar]
- 13.Kanj HA, Noronha J, D'Aguillo AF, Amorosa JK, Amorosa LF. Bilateral adrenal myelolipomas with Cushing's syndrome. JAMA 1988;259:3034–3036 [PubMed] [Google Scholar]
- 14.Umpierrez MB, Fackler S, Umpierrez GE, Rubin J. Adrenal myelolipoma associated with endocrine dysfunction: Review of the literature. Am J Med Sci 1997;314:338–341 [DOI] [PubMed] [Google Scholar]
- 15.Wagnerova H, Lazurova I, Bober J, Sokol L, Zachar M. Adrenal myelolipoma. 6 cases and a review of the literature. Neoplasma 2004;51:300–305 [PubMed] [Google Scholar]
- 16.Shen X, Qui Y, Zheng Y, Zhang S. Retroperitoneal laparoscopic liposuction for large adrenal myelolipomas: A report of nine cases. J Laparoendosc Adv Surg Tech A 2012;22:578–580 [DOI] [PubMed] [Google Scholar]


