Abstract
Background
The relation of body fat distribution to left ventricular (LV) structure and function is poorly defined.
Methods and Results
2710 participants without heart failure or LV dysfunction in the Dallas Heart Study underwent dual energy x-ray absorptiometry and magnetic resonance imaging assessment of fat distribution, LV morphology, and hemodynamics. Cross-sectional associations of fat distribution with LV structure and function were examined after adjustment for age, sex, race, comorbidities, and lean mass. Mean age was 44 years with 55% women; 48% African-Americans; and 44% obese. After multivariable adjustment, visceral fat (VAT) was associated with concentric remodeling characterized by lower LV end-diastolic volume (β= -0.21), higher concentricity (β= 0.20) and wall thickness (β=0.09, p<0.0001 for all). In contrast, lower body subcutaneous fat (LBF) was associated with higher LV end-diastolic volume (β= 0.48), reduced concentricity (β= -0.50) and wall thickness (β= -0.28, p<0.0001 for all). VAT was also associated with lower cardiac output (β= -0.10, p<0.05) and higher systemic vascular resistance (β= 0.08, p<0.05) whereas LBF associated with higher cardiac output (β= 0.20, p<0.0001) and lower systemic vascular resistance (β= -0.18, p<0.0001). Abdominal subcutaneous fat (SAT) showed weaker associations with concentric remodeling and was not associated with hemodynamics. Among the subset of obese participants, VAT, but not SAT, was significantly associated with concentric remodeling.
Conclusions
VAT, a marker of central adiposity, was independently associated with concentric LV remodeling and adverse hemodynamics. In contrast, LBF was associated with eccentric remodeling. The impact of body fat distribution on heart failure risk requires prospective study.
Keywords: obesity, body fat distribution, visceral fat, left ventricular hypertrophy, concentric remodeling
The relationship between obesity and left ventricular (LV) structure and function is complex. Historically, obesity was believed to result in increased LV mass and cavity size1, 2 as a compensatory response to chronic volume overload, leading to eccentric LV remodeling, systolic dysfunction, and heart failure.3 However, more recent data suggest that increased adiposity can also be associated with a concentric LV remodeling phenotype, characterized by increased mass-to-volume ratio, LV wall thickness, and diastolic dysfunction.4, 5 In fact, approximately 50% of the obese participants with heart failure who underwent echocardiography in a study by Kenchaiah et al. had a diagnosis of heart failure with preserved ejection fraction.3 The reasons for heterogeneity in LV remodeling phenotypes in obesity, however, remain unclear.
One explanation may relate to body fat distribution. It is plausible that fat distribution may influence LV remodeling given that the varying adipose depots have different structural composition, metabolic activity, and functional expression.6 For example, visceral adipose tissue (VAT) is associated with multiple cardiovascular disease (CVD) risk factors7 and the development of diabetes,8 whereas fat stored in the gluteal-femoral region (lower body subcutaneous fat, LBF) may be potentially protective against CVD risk factors.9 Nevertheless, the impact of adipose tissue distribution (VAT versus abdominal subcutaneous [SAT] versus LBF) on LV remodeling is largely unknown. Studies examining the relationship of VAT and other fat depots with LV morphology are limited,10-12 and have not comprehensively addressed the impact of body fat distribution on LV concentric remodeling, a robust determinant of diastolic heart failure.13
Therefore, we investigated the cross-sectional associations of body fat composition by dual energy x-ray absorptiometry (DEXA) and abdominal fat distribution by magnetic resonance imaging (MRI) with cardiac MRI measures of LV mass, end-diastolic volume, mass-to-volume ratio (concentricity index) and wall thickness in a large, multiethnic cohort of adults. We hypothesized that VAT, but not LBF, would be independently associated with a concentric remodeling phenotype. We also explored the association of fat distribution with baseline hemodynamics assessed by cardiac MRI measurement of stroke volume.
Methods
Study population
The Dallas Heart Study (DHS) is a multi-ethnic, probability-based, population cohort study of Dallas County adults with deliberate over-sampling of African-Americans. Detailed methods of the DHS have been described previously.14 Briefly, between 2000 and 2002, 3072 subjects completed the three DHS visits, including a detailed in-home survey, laboratory testing, and imaging studies. For the present study, participants with a LV ejection fraction <40%, those with prevalent clinical heart failure (defined by self-report of “congestive heart failure, an enlarged heart, a weak heart, or cardiomyopathy”), and those with missing cardiac MRI data were excluded, yielding a final sample size of 2710. Participants provided written informed consent, and the protocol was approved by the institutional review board of the University of Texas Southwestern Medical Center.
Race/ethnicity, history of cardiovascular diseases (CVD), and smoking status were self-reported. Detailed descriptions of variable definitions for hypertension, hypercholesterolemia, and low high-density lipoprotein cholesterol have been previously described using conventional clinical definitions.15 Presence of the metabolic syndrome was defined according to the National Cholesterol Education Program's (NCEP) Adult Treatment Panel III report.16 The homeostasis model assessment of insulin resistance index (HOMA-IR) was calculated by fasting insulin (μIU/ml) × fasting glucose (mmol/liter)/22.5.17 Adipocytokines including total adiponectin,18 leptin,19 and highly-sensitive C-reactive protein levels19 were measured as previously described. Interleukin-6 was measured from thawed frozen plasma at Alere Inc. (San Diego, CA) using a Luminex sandwich assay, with minimum and maximum detection limits of 10 and 15,000 pg/mL, respectively, and an intra-assay coefficient of variation of 16%.
Body fat distribution measurements
BMI was calculated as weight (kilograms)/height (meters)2. Body surface area (BSA) was calculated using the method of Tikuisis.20 Waist circumference was measured 1 cm above the iliac crest and hip circumference at the widest circumference of the buttocks at the area of the greater trochanters. DEXA (Delphi W scanner, Hologic Inc., Bedford, MA and Discovery software [version 12.2]) was used to measure total body fat, lean mass, percent body fat, and LBF. LBF was delineated by two oblique lines crossing the femoral necks and converging below the pubic symphysis, and included gluteal-femoral fat.9 VAT (intraperitoneal + retroperitoneal fat) and SAT were measured by a 1.5-T MRI system (Intera, Philips Medical Systems, Best, The Netherlands) using a prospectively designed and validated method of fat mass prediction from a single MRI slice at the L2-L3 inter-vertebral level.21 Single slice measurement of SAT and VAT fat mass at this inter-vertebral level has been shown to be highly concordant with total abdominal fat mass measured at all inter-vertebral levels (R2=85-96%).21
Cardiac imaging and hemodynamic measurements
LV mass, end-systolic and diastolic volumes, and wall thickness were obtained from short-axis, breath-hold, electrocardiographic-gated cine cardiac MRI images using the same 1.5-T system as previously described.22 Heart rate and blood pressure were measured at the time of the MRI scan. Stroke volume, defined as end-diastolic volume minus end-systolic volume, was multiplied by heart rate to obtain cardiac output (L/min). Systemic vascular resistance (dynes*sec/cmˆ5) was calculated as 80 × (mean arterial pressure minus right atrial pressure) divided by cardiac output, assuming a right atrial pressure of 5 mmHg. LV concentricity index was defined as the ratio of LV mass to end-diastolic volume. LV hypertrophy (LVH) was defined as LV mass/BSA ≥89 g/m2 in women and ≥112 g/m2 in men, based on a phenotypically normal subpopulation of the DHS cohort.22
Statistical Analysis
Characteristics were compared between normal weight (BMI<25 kg/m2), overweight (25≤BMI<30 kg/m2), and obese (BMI≥30 kg/m2) participants using chi-square tests for dichotomous variables and Wilcoxon rank-sum tests for continuous variables. Linear regression modeling was used to assess associations of fat parameters with LV structure and hemodynamics, with the fat parameter as the independent variable and LV structure or hemodynamic parameter as the dependent variable. Standardized β coefficients were used to facilitate comparisons between fat and LV structure measurements. The standardized β coefficient represents the change in the LV structure variable (in standard deviation units) per a 1 standard deviation increase in the fat parameter. Models were adjusted for age, sex, African-American race, hypertension, diabetes, hyperlipidemia, exercise, alcohol use, cardiovascular disease, smoking, and lean mass, and sequentially adjusted for all fat parameters in order to assess the independent associations of each fat depot with LV structure and function independent of overall fat and lean mass. Due to potential collinearity by inclusion of both fat and lean mass in multivariable models, variance inflation factors were tested, which were consistently less than 4. Multivariable models were also tested stratified by sex and obesity-status, and with additional adjustment for HOMA-IR and adipocytokine levels; by replacement of hypertension status with systolic blood pressure and antihypertensive medication use; and by replacement of lean mass with BSA or height2.7. Sensitivity analyses were performed excluding participants with hypertension, diabetes, LVH, and CVD. Logistic regression analysis was used to assess the multivariable adjusted associations of visceral fat mass with the highest sex-specific quartile of concentricity index across subgroups of age, sex, race, and obesity status. For all statistical testing, a 2-sided p-value <0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.2 software (SAS Corporation, Cary, NC).
Results
Univariable Associations of Fat Distribution with LV Geometry
Among the 2710 participants meeting study criteria, mean age was 44, 55% were women and 48% African-American. 24% of the study cohort was normal weight (BMI<25 kg/m2), 32% overweight (25≤BMI<30 kg/m2), and 44% obese (BMI≥30 kg/m2). Baseline characteristics are presented in Table 1. Compared with normal weight individuals, those overweight or obese were older and more likely to be African-American with greater prevalence of hypertension, diabetes, metabolic syndrome, and LVH (p<0.05 for each). Overweight or obese individuals had both more fat and lean mass compared with their normal weight counterparts (p<0.05 for each).
Table 1. Characteristics of the Study Population Stratified by Obesity Status (N=2710).
| Variable | Normal Weight (n=644) | Overweight (n=876) | Obese (n=1190) | P-trend |
|---|---|---|---|---|
| Age (yrs) | 41 (35, 50) | 44 (37, 51) | 44 (36, 52) | 0.01 |
| Male (%) | 48.1 | 53.5 | 37.5 | <0.0001 |
| Race (%) | ||||
| Caucasian | 40.7 | 34.9 | 26.1 | <0.0001 |
| African-American | 42.9 | 43.5 | 54.4 | <0.0001 |
| Hispanic | 12.9 | 18.9 | 18.6 | 0.006 |
| Hypertension (%) | 18.0 | 28.4 | 42.2 | <0.0001 |
| Systolic Blood Pressure (mmHg) | 115 (106, 127) | 119 (111, 130) | 125 (116, 137) | <0.0001 |
| Diabetes (%) | 4.5 | 5.8 | 17.2 | <0.0001 |
| HOMA-IR | 1.4 (0.9, 2.2) | 2.3 (1.5, 3.8) | 4.4 (2.9, 6.7) | <0.0001 |
| Hypercholesterolemia (%) | 8.7 | 13.0 | 14.7 | 0.0004 |
| Low HDL Cholesterol (%) | 22.4 | 36.9 | 51.3 | <0.0001 |
| Metabolic Syndrome (%) | 8.4 | 22.2 | 55.6 | <0.0001 |
| Current Smoking (%) | 37.7 | 26.7 | 22.8 | <0.0001 |
| Prior CVD (%) | 4.5 | 2.9 | 4.5 | 0.76 |
| Left Ventricular Hypertrophy (%) | 7.9 | 9.5 | 11.2 | 0.02 |
| Adiposity Measures | ||||
| Weight (kg) | 63.5 (57.2, 69.9) | 78.1 (71.0, 85.3) | 98.0 (87.3, 110.2) | <0.0001 |
| Body Surface Area (m2) | 1.7 (1.6, 1.8) | 1.9 (1.8, 2.0) | 2.1 (2.0, 2.3) | <0.0001 |
| Body Mass Index (kg/m2) | 22.7 (21.2, 23.9) | 27.5 (26.2, 28.7) | 34.8 (32.1, 38.8) | <0.0001 |
| Waist Circumference (cm) | 81.5 (75.5, 87.0) | 93.5 (88.0, 99.0) | 110.0 (102.0, 118.0) | <0.0001 |
| Waist/Hip ratio | 0.86 (0.80, 0.92) | 0.91 (0.85, 0.96) | 0.92 (0.86, 0.98) | <0.0001 |
| Total Fat Mass (kg) | 15.2 (11.0, 19.1) | 22.8 (18.8, 26.7) | 35.0 (28.9, 42.8) | <0.0001 |
| Total Lean Mass (kg) | 46.5 (39.7, 55.6) | 55.4 (44.7, 63.5) | 57.8 (50.6, 68.4) | <0.0001 |
| Visceral Fat (kg) | 1.2 (0.9, 1.7) | 2.0 (1.5, 2.5) | 2.6 (2.0, 3.2) | <0.0001 |
| Abdominal Subcutaneous Fat (kg) | 2.2 (1.6, 2.9) | 3.7 (2.9, 4.5) | 6.5 (5.0, 8.8) | <0.0001 |
| Lower Body Fat (kg) | 5.7 (3.9, 7.7) | 7.7 (5.9, 10.1) | 12.1 (9.2, 15.6) | <0.0001 |
| Cardiac MRI Measures | ||||
| LV Mass (g) | 138.8 (115.7, 167.4) | 155.0 (129.2, 186.3) | 167.4 (142.6, 197.9) | <0.0001 |
| LV Mass/BSA (g/m2) | 79.7 (69.6, 92.8) | 81.5 (70.5, 93.5) | 78.9 (69.8, 91.4) | 0.26 |
| LV End-Diastolic Volume (mL) | 93.3 (79.4, 108.6) | 98.0 (84.2, 113.7) | 102.3 (88.3, 119.4) | <0.0001 |
| LV End-Diastolic Volume/BSA (mL/m2) | 54.6 (47.9, 61.0) | 51.7 (45.9, 58.1) | 49.1 (42.8, 55.8) | <0.0001 |
| LV Wall Thickness (mm) | 10.6 (9.6, 11.9) | 11.4 (10.3, 12.5) | 11.9 (10.8, 13.2) | <0.0001 |
| Concentricity Index (g/mL) | 1.5 (1.3, 1.7) | 1.6 (1.4, 1.8) | 1.6 (1.4, 1.9) | <0.0001 |
| Heart Rate (bpm) | 64.5 (58.5, 71.5) | 65.5 (59.0, 73.3) | 69.5 (62.5, 77.0) | <0.0001 |
| Mean Arterial Pressure (mmHg) | 92.3 (85.5, 100.2) | 95.5 (88.7, 104.6) | 99.7 (92.3, 109.3) | <0.0001 |
| Cardiac Output (L/min) | 4.3 (3.7, 4.9) | 4.7 (4.0, 5.3) | 5.2 (4.4, 6.2) | <0.0001 |
| Cardiac Index (L/min/m2) | 2.5 (2.1, 2.8) | 2.4 (2.1, 2.8) | 2.5 (2.2, 2.9) | 0.13 |
| Systemic Vascular Resistance (dynes*sec/cmˆ5) | 1664 (1390, 1959) | 1563 (1359, 1865) | 1460 (1230, 1742) | <0.0001 |
Data are presented as median (25%, 75% percentile) or proportion (%) where indicated.
Normal weight: BMI<25 kg/m2; Overweight 25≤BMI<30 kg/m2; Obese BMI≥30 kg/m2
Abbreviations: BSA= body surface area; CVD= cardiovascular disease; HDL= high density lipoprotein; HOMA-IR= homeostasis model assessment of insulin resistance; LV= left ventricular; MRI= magnetic resonance imaging
Obesity was associated with higher LV mass, end-diastolic volumes, wall thickness, and concentricity (p<0.05 for each, Table 1). However, when LV mass was indexed by BSA (to account for overall body size), there were no significant differences in LV mass index between normal weight, overweight, or obese individuals. Additionally, after indexing by BSA, overweight and obesity were associated with a graded decrease in end-diastolic volumes compared with those of normal weight (p<0.0001). In analyses restricted to obese participants, those with larger (> median) versus smaller (≤ median) waist circumference or larger (> median) versus smaller (≤ median) waist-hip ratio had significantly higher LV concentricity (Online Supplemental Table 1).
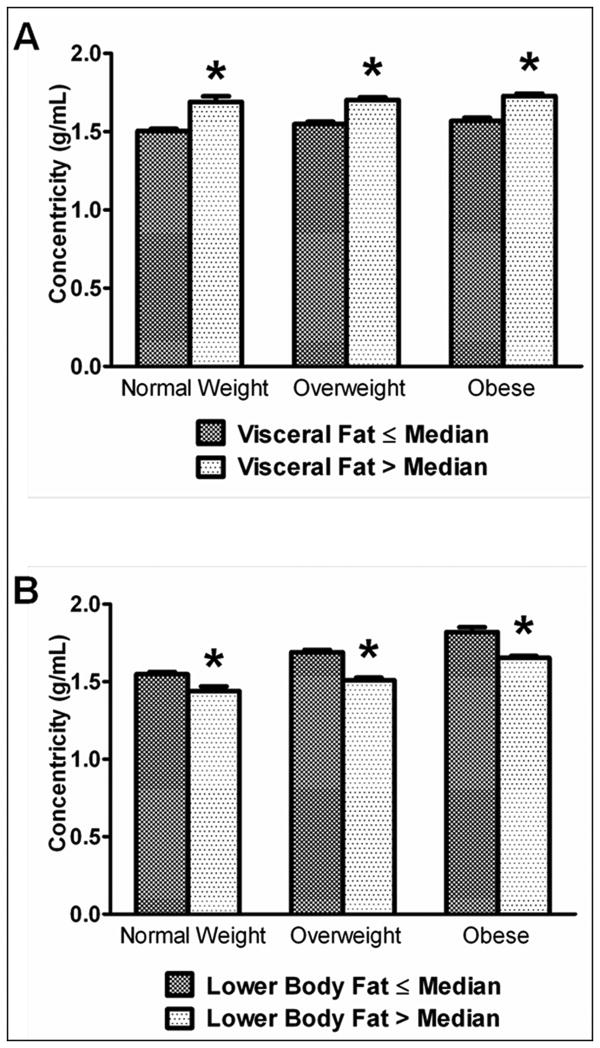
In unadjusted analyses, VAT and SAT were both positively associated with a concentric hypertrophy phenotype including greater LV mass (β = 0.41, and 0.13, respectively), concentricity (β = 0.31 and 0.06, respectively) and LV wall thickness (β = 0.43 and 0.14, respectively; p<0.05 for each). In contrast, LBF was inversely associated with these parameters (β = -0.07, -0.09, and -0.06, respectively; p<0.05 for each). Concentricity index remained positively associated with VAT and inversely associated with LBF across strata of normal weight, overweight, and obese individuals (Figure 1).
Figure 1. Concentricity index by visceral and lower body fat mass across BMI categories.
Mean and SE of concentricity for visceral fat (A) and lower body fat (B) stratified by median level are shown by BMI category as follows: normal weight, BMI <25 kg/m2 (n=642); overweight, 25≤BMI<30 kg/m2 (n=875); obese BMI≥30 kg/m2 (n=1133). Mean BMIs for fat mass ≤median and >median are 22 and 23, 27 and 27, and 35 and 36 kg/m2 respectively for normal weight, overweight, and obese categories. *p<0.05 vs. ≤ median group.
Multivariable Adjustment
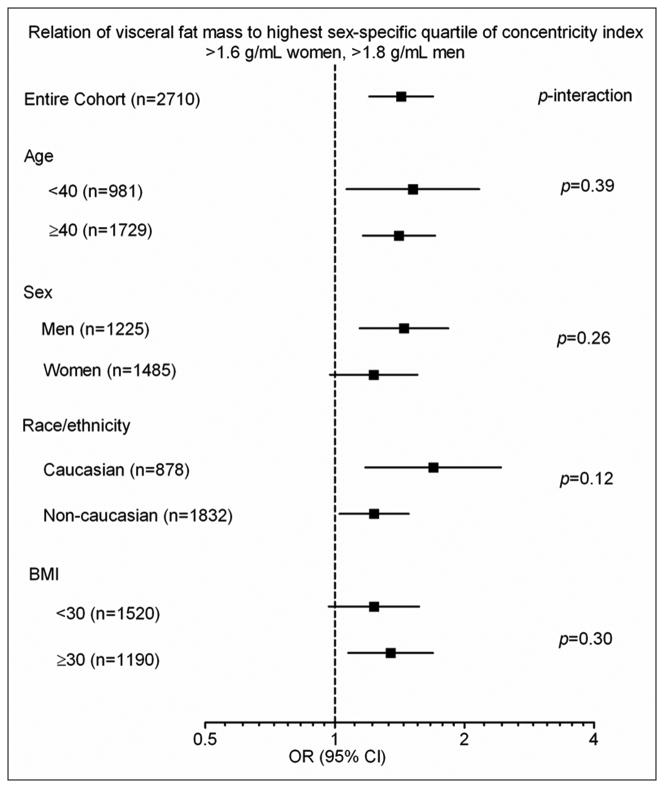
After multivariable adjustment for age, sex, African-American race, hypertension, diabetes, hyperlipidemia, exercise, alcohol use, cardiovascular disease, smoking, and lean mass, VAT was inversely associated with LV end-diastolic volume (β= -0.21, p<0.0001) and remained positively associated with LV concentricity and wall thickness (β= 0.20 and 0.09, p<0.0001 for both) (Table 2). In contrast, LBF was associated with significantly higher LV end-diastolic volume (β= 0.48, p<0.0001) and reduced concentricity and wall thickness (β= -0.50 and -0.28, p<0.0001 for both). Results were unchanged after additional adjustment for all fat mass depots and HOMA-IR (Table 2) and were consistent in sex-stratified models (Online Supplemental Table 2). Associations of SAT with LV phenotypes were generally similar, although weaker, to those of VAT. All findings were insensitive to exclusion of participants with hypertension, diabetes, LVH, and CVD; and were unchanged after replacement of hypertension status with systolic blood pressure and antihypertensive medication use or by additional adjustment for adipocytokine levels in the models (Online Supplemental Table 3). Findings were also generally similar using adjustment for BSA or height2.7 instead of lean mass (data not shown). The multivariable adjusted association between higher VAT and increased concentricity index was consistent across subgroups defined by age, sex, race, and obesity-status, with no interactions observed (Figure 2). In multivariable models stratified by obesity-status, VAT, but not SAT, was independently associated with LV concentricity and wall thickness among obese participants (β= 0.21 and 0.11, p<0.01 for both); in contrast, both VAT and SAT were associated with LV concentricity and wall thickness among the non-obese. LBF remained associated with an eccentric phenotype in both obese and non-obese individuals. In general, associations between VAT and LBF and LV structure were stronger among obese participants compared with those non-obese (Table 3).
Table 2. Multivariable-Adjusted Linear Regression Models of Relation of Adiposity Phenotypes to Cardiac Structure and Function.
| LV Mass | LV EDV | Concentricity | LV Wall Thickness | |||||
|---|---|---|---|---|---|---|---|---|
| β | P-value | β | P-value | β | P-value | β | P-value | |
|
| ||||||||
| Visceral Fat | ||||||||
|
| ||||||||
| Model 1 | 0.41 | <0.0001 | 0.19 | <0.0001 | 0.31 | <0.0001 | 0.43 | <0.0001 |
| Model 2 | -0.01 | 0.77 | -0.21 | <0.0001 | 0.20 | <0.0001 | 0.09 | <0.0001 |
| Model 3 | 0.01 | 0.76 | -0.17 | <0.0001 | 0.19 | <0.0001 | 0.09 | <0.0001 |
| Model 4 | -0.003 | 0.89 | -0.17 | <0.0001 | 0.18 | <0.0001 | 0.08 | 0.0005 |
| Abdominal Subcutaneous Fat | ||||||||
|
| ||||||||
| Model 1 | 0.13 | <0.0001 | 0.11 | <0.0001 | 0.06 | 0.004 | 0.14 | <0.0001 |
| Model 2 | 0.01 | 0.76 | -0.08 | 0.07 | 0.11 | 0.02 | 0.10 | 0.01 |
| Model 3 | 0.02 | 0.36 | -0.11 | 0.001 | 0.17 | <0.0001 | 0.13 | <0.0001 |
| Model 4 | 0.02 | 0.41 | -0.11 | 0.001 | 0.17 | <0.0001 | 0.13 | <0.0001 |
| Lower Body Fat | ||||||||
|
| ||||||||
| Model 1 | -0.07 | 0.001 | 0.02 | 0.30 | -0.09 | <0.0001 | -0.06 | 0.002 |
| Model 2 | 0.01 | 0.70 | 0.48 | <0.0001 | -0.50 | <0.0001 | -0.28 | <0.0001 |
| Model 3 | -0.06 | 0.03 | 0.17 | <0.0001 | -0.26 | <0.0001 | -0.16 | <0.0001 |
| Model 4 | -0.07 | 0.02 | 0.18 | <0.0001 | -0.26 | <0.0001 | -0.17 | <0.0001 |
Models constructed with cardiac measures as dependent variables and fat parameters as independent variables; β coefficient is per 1-SD of the fat parameter.
Model 1 is unadjusted.
Model 2 is adjusted for age, sex, African-American race, hypertension, diabetes, hyperlipidemia, exercise, alcohol use, cardiovascular disease, smoking, and lean mass.
Model 3 is adjusted for all covariates from Model 2 plus visceral fat, abdominal subcutaneous fat, and lower body fat mass.
Model 4 is adjusted for all covariates from Model 3 plus HOMA-IR.
Figure 2. Multivariable adjusted associations of visceral fat with the highest sex-specific quartile of concentricity index (>1.6 g/mL for women and >1.8 g/mL for men) by age, sex, race, and obesity subgroups.
Odds ratios per 1-standard deviation increment in visceral fat mass. Adjusted for age, sex, African-American race, hypertension, diabetes, hyperlipidemia, exercise, alcohol use, cardiovascular disease, smoking, lean mass, abdominal subcutaneous fat, liver fat, and lower body fat mass. p-value for subgroup interaction.
Table 3. Multivariable-Adjusted Linear Regression Models of Relation of Adiposity Phenotypes to Cardiac Structure and Function Stratified by Obesity-Status (Obese N=1190, Non-Obese N=1520).
| LV Mass | LV EDV | Concentricity | LV Wall Thickness | |||||
|---|---|---|---|---|---|---|---|---|
| β | P-value | β | P-value | β | P-value | β | P-value | |
|
| ||||||||
| Visceral Fat | ||||||||
|
| ||||||||
| Obese | 0.01 | 0.75 | -0.19 | <0.0001 | 0.21 | <0.0001 | 0.11 | 0.001 |
| Non-Obese | -0.07 | 0.002 | -0.17 | <0.0001 | 0.10 | 0.002 | 0.02 | 0.48 |
| Abdominal Subcutaneous Fat | ||||||||
|
| ||||||||
| Obese | 0.02 | 0.68 | -0.08 | 0.13 | 0.11 | 0.05 | 0.09 | 0.05 |
| Non-Obese | 0.01 | 0.65 | -0.05 | 0.14 | 0.07 | 0.04 | 0.06 | 0.02 |
| Lower Body Fat | ||||||||
|
| ||||||||
| Obese | 0.001 | 0.98 | 0.44 | <0.0001 | -0.46 | <0.0001 | -0.27 | <0.0001 |
| Non-Obese | -0.002 | 0.95 | 0.10 | 0.002 | -0.11 | 0.002 | -0.07 | 0.01 |
Models constructed with cardiac measures as dependent variables and fat parameters as independent variables; β coefficient is per 1-SD of the fat parameter.
Model is adjusted for age, sex, African-American race, hypertension, diabetes, hyperlipidemia, exercise, alcohol use, cardiovascular disease, smoking, lean mass, visceral fat, abdominal subcutaneous fat, and lower body fat mass.
Associations of Fat Distribution with Hemodynamics
Overweight and obese individuals had significantly higher heart rate, mean arterial pressure, and cardiac output and lower systemic vascular resistance compared with normal weight individuals; however, after accounting for body surface area, cardiac index did not differ between groups (Table 1). In multivariable analysis, overall body fat remained significantly associated with higher cardiac output and lower systemic vascular resistance (β= 0.12 and -0.06, p<0.05 for both); however, this association was not uniform across fat depots. LBF was positively associated with cardiac output and inversely associated with systemic vascular resistance (β= 0.20 and -0.18, respectively, p<0.0001 for both) (Table 4). In contrast, VAT was associated with lower cardiac output and higher systemic vascular resistance in fully adjusted models (β= -0.10 and 0.08, respectively, p<0.05 for both). Findings were unchanged when the assumed right atrial pressure was changed to 10 or 15 mmHg (data not shown) and were insensitive to exclusion of all participants with hypertension and those treated with antihypertensive medication (Table 4). SAT was not independently associated with hemodynamic parameters.
Table 4. Multivariable-Adjusted Linear Regression Models of Relation of Adiposity Phenotypes to Hemodynamics.
| Cardiac Output | Systemic Vascular Resistance | |||
|---|---|---|---|---|
|
| ||||
| β | P-value | β | P-value | |
|
| ||||
| Visceral Fat | ||||
|
| ||||
| Model 1 | -0.10 | 0.0006 | 0.08 | 0.01 |
| Model 2 | -0.09 | 0.003 | 0.07 | 0.03 |
| Abdominal Subcutaneous Fat | ||||
|
| ||||
| Model 1 | 0.01 | 0.80 | 0.04 | 0.25 |
| Model 2 | 0.01 | 0.82 | 0.05 | 0.21 |
| Lower Body Fat | ||||
|
| ||||
| Model 1 | 0.20 | <0.0001 | -0.18 | <0.0001 |
| Model 2 | 0.19 | <0.0001 | -0.17 | <0.0001 |
Models constructed with hemodynamic measure as dependent variable and fat parameter as independent variable; β coefficient is per 1-SD of the fat parameter.
Model 1 is adjusted for age, sex, African-American race, systolic blood pressure, antihypertensive medication use, diabetes, hyperlipidemia, exercise, alcohol use, cardiovascular disease, smoking, lean mass, visceral fat, abdominal subcutaneous fat, and lower body fat mass.
Model 2 is identical to Model 1 but excludes all participants with hypertension or treated with antihypertensive medication.
Discussion
Principal Findings
In a large, population-based cohort of community-dwelling adults, we observed a complex relationship between obesity and LV morphology that is dependent upon adipose tissue distribution with distinct structural cardiac phenotypes seen across different fat depots. Increased central adiposity was independently associated with concentric LV remodeling (increased LV wall thickness, increased LV mass/volume ratio, and smaller LV end-diastolic volume) and a significantly lower cardiac output and higher systemic vascular resistance. In contrast, lower body (gluteal-femoral) adiposity was associated with eccentric remodeling (increased LV end-diastolic volume with reduced LV mass, concentricity, and wall thickness) and a higher cardiac output and lower systemic vascular resistance. Accounting for blood pressure, HOMA-IR, and circulating adipocytokines did not attenuate these associations, suggesting that the link between adiposity and LV structure and function may be at least partially independent of intermediary risk factors. Novel findings in our study include the association of multiple direct measures of central adiposity (VAT and SAT) with LV concentricity and adverse hemodynamics and the relation of LBF with more eccentric LV morphology.
In Context of the Current Literature
Prior studies examining the relationship between adiposity and LV morphology have primarily focused on generalized measures of obesity such as BMI or total fat mass. In general, these studies have reported that obesity is positively associated with LV mass and end-diastolic volume (or dimension). For example, in a sub-study of the Swedish Obese Subjects (SOS) Study, total fat mass was correlated with higher LV mass and end-diastolic diameter (R=0.23, p<0.05 for both) independent of age, sex, lean mass, systolic blood pressure, and circulating insulin.23 A larger study from the Multi-Ethnic Study of Atherosclerosis (MESA) using cardiac MRI demonstrated similar findings, including the novel finding that obesity was associated with an increased mass-volume ratio (concentricity index), suggesting a relationship between obesity and concentric LV remodeling.4 However, because lean body mass is a well-recognized determinant of LV mass and obesity is associated with parallel increases in both fat and lean mass, the relationship between adiposity and LV mass may be confounded.24 Additionally, these studies are limited to derived measures of fat and lean mass and are unable to further differentiate between different adipose tissue depots. More recent studies using direct imaging based measures of VAT have shown no or minimal independent association between central adiposity and LV mass but a robust inverse association with LV end-diastolic volume.10, 11 The discordant LV mass findings between studies may relate to the use of height and weight based models of body composition (which may lack sensitivity and specificity compared with imaging-based measures) limiting the ability of these prior studies to resolve independent effects of fat and lean mass on LV mass.
Using direct, imaging based assessments of fat and lean mass, in addition to body fat distribution, the current findings suggest that the relationship between adiposity and LV structure and function is highly dependent on body fat distribution, with abdominal adiposity, but not LBF, independently related to a concentric LV morphologic phenotype. Importantly, although the relation of VAT and LBF with LV structure and function was consistent among both obese and non-obese individuals, we noted a difference in the relationship between abdominal SAT and LV morphology, as the current findings demonstrate that abdominal SAT was not independently associated with LV structure or function among the subset of individuals with obesity (BMI ≥30 kg/m2). These findings are similar to those from a recent study in which we observed no independent relationship of abdominal SAT with markers of insulin resistance, dyslipidemia, or atherosclerosis in an obese population sample.25 Taken together, these observations are consistent with the theory that inadequate expansion of the subcutaneous adipose depot (the preferred site of fat storage) in the setting of obesity results in excess fatty acid accumulation in visceral and ectopic tissues, leading to adverse metabolic and cardiovascular consequences such as diabetes, dyslipidemia, and concentric LV remodeling.
Potential Mechanisms
There are several possible explanations for our findings. VAT has been consistently linked to an adverse cardiovascular risk profile, including higher prevalence of traditional risk factors,7 circulating inflammatory cytokines,26 dyslipidemia, and atherosclerosis.25 The relationship between central adiposity and LV structure and function may therefore be partially mediated through effects on risk factors and systemic inflammation. Additionally, VAT is a risk factor for insulin resistance and diabetes,8 which in turn may impact concentric LV remodeling.27 However, the current findings were independent of measured adipocytokines and insulin resistance, as measured by HOMA-IR, suggesting that the link between abdominal adiposity and LV structure and function may be mediated at least in part by alternative pathways. However, from available data, we cannot exclude the possibility that other, more physiologic, indexes of insulin resistance, such as decreased translocation of the GLUT-4 receptor,28 mediate the association of abdominal adiposity and concentric remodeling. Another putative mechanism of the associations reported herein is the potential for increased cardiac lipotoxicity in individuals with excess abdominal adiposity, given that visceral adipose tissue has been recently identified to have increased susceptibility to lipolysis.29 As postulated in the metabolic syndrome of chronic heart failure,30 cardiac lipotoxicity caused by excess free fatty acids associated with the more metabolically active VAT could have important consequences on cardiac structure and function. Conversely, LBF may act as a metabolic sink, buffering the influx of dietary lipids and protecting other tissues, including the heart, from lipotoxicity caused by lipid overflow and ectopic fat deposition. Indeed, LBF has been independently associated with a favorable lipid and glycemic profile, as well as decreases in cardiovascular and metabolic risk.31 The divergent hemodynamic findings between abdominal and lower body fat may also relate to differences in arterial compliance associated with regional body fat distribution since abdominal obesity is associated with higher arterial stiffness, whereas LBF is associated with lower arterial stiffness, independent of age, sex, body mass, and blood pressure.32 Finally, impaired cardiorespiratory fitness, which is associated with higher VAT at any given BMI, may contribute to more concentric remodeling of the LV over time.
Strengths and Limitations
Strengths of the current study include detailed phenotyping using multiple novel adipose tissue imaging techniques and a racially diverse sample of adults applicable to the general population. Several limitations also merit comment. Since the analysis was cross-sectional, we cannot determine a causal relationship between body fat distribution and LV structure and function; therefore, further confirmation in prospective studies with serial assessment of body fat distribution and LV morphology are required. Second, we are unable to examine the role that adipocytokines other than those measured play in the relationship between adiposity and LV structure. Third, calculation of systemic vascular resistance may have been overestimated in some participants since right atrial pressure was assumed to be 5 mmHg. However, findings were consistent using higher estimates of right atrial pressure. Finally, the present findings are not necessarily generalizable to individuals older than age 65 or with symptomatic heart failure in which both body fat distribution and LV morphology may be different compared with our study population.
Clinical Implications
Although obesity is associated with an increased risk for heart failure,3 the lack of association between obesity and reduced LV ejection fraction in most studies4 suggests that risk for diastolic heart failure may be more significant than for systolic dysfunction. Our findings suggest that the diastolic heart failure risk associated with obesity may be heterogeneous and dependent on distribution of excess body fat. These observations may also have important implications for differentiating risk among individuals with normal body weight but increased visceral adiposity (normal weight obese) who may be prone to LV concentricity, but who are difficult to identify because they are lean. Similarly, our results suggest that elevated BMI per se may not accurately identify all patients at higher risk for diastolic heart failure as some obese individuals with more lower body fat (so-called healthy obese) may be less likely to develop concentric LV remodeling.
The current observations may have important therapeutic implications as well, since obese individuals with a prominent lower body adiposity phenotype may not achieve significant cardiovascular benefit from intensive weight reduction therapies, whereas patients with greater visceral adiposity may gain significant risk reduction from intensive exercise, pharmacologic intervention, or bariatric surgery even at lower body weights. If our findings are confirmed, adiposity reduction aimed at selectively decreasing abdominal fat (e.g. with exercise or bariatric surgery), may be a therapeutic target in the prevention and treatment of diastolic heart failure. Newer strategies addressing abdominal adiposity may be especially relevant given the paucity of effective diastolic heart failure therapies in clinical practice, beyond more aggressive control of blood pressure and other traditional risk factors. Alternatively, future pharmacologic therapies aimed at redistributing fat from visceral and ectopic sites to more favorable lower body subcutaneous depots may potentially lead to reverse LV remodeling and impact cardiac function.
Conclusions
In a multiethnic cohort of adults without heart failure, we observed that central abdominal and lower body subcutaneous adiposity were associated with divergent cardiovascular structural and hemodynamic phenotypes. Abdominal adiposity, but not lower body fat, was associated with adverse concentric LV remodeling and a reduced cardiac output and higher systemic vascular resistance. Further investigation of these distinct adipose tissue depots is essential to better define the mechanisms by which obesity leads to heart failure.
Supplementary Material
Acknowledgments
Sources of Funding: This work was supported by award number T32HL007360 from the National Heart, Lung, and Blood Institute to Dr. Neeland, by grants UL1DE019584 and PL1DK081182 from the National Institutes of Health, and by grant number UL1TR000451 from the National Center for Advancing Translational Sciences. Dr. Drazner was supported by the James M. Wooten Chair in Cardiology.
Abbreviations
- BSA
body surface area
- CVD
cardiovascular disease
- DEXA
dual energy x-ray absorptiometry
- LV
left ventricle
- LVH
left ventricular hypertrophy
Footnotes
Disclosures: None.
References
- 1.Heckbert SR, Post W, Pearson GD, Arnett DK, Gomes AS, Jerosch-Herold M, Hundley WG, Lima JA, Bluemke DA. Traditional cardiovascular risk factors in relation to left ventricular mass, volume, and systolic function by cardiac magnetic resonance imaging: the Multiethnic Study of Atherosclerosis. J Am Coll Cardiol. 2006;48:2285–92. doi: 10.1016/j.jacc.2006.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lauer MS, Anderson KM, Kannel WB, Levy D. The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA. 1991;266:231–6. [PubMed] [Google Scholar]
- 3.Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, Kannel WB, Vasan RS. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–13. doi: 10.1056/NEJMoa020245. [DOI] [PubMed] [Google Scholar]
- 4.Turkbey EB, McClelland RL, Kronmal RA, Burke GL, Bild DE, Tracy RP, Arai AE, Lima JA, Bluemke DA. The impact of obesity on the left ventricle: the Multi-Ethnic Study of Atherosclerosis (MESA) JACC Cardiovasc Imaging. 2010;3:266–74. doi: 10.1016/j.jcmg.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pascual M, Pascual DA, Soria F, Vicente T, Hernandez AM, Tebar FJ, Valdes M. Effects of isolated obesity on systolic and diastolic left ventricular function. Heart. 2003;89:1152–6. doi: 10.1136/heart.89.10.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bays HE, Gonzalez-Campoy JM, Bray GA, Kitabchi AE, Bergman DA, Schorr AB, Rodbard HW, Henry RR. Pathogenic potential of adipose tissue and metabolic consequences of adipocyte hypertrophy and increased visceral adiposity. Expert Rev Cardiovasc Ther. 2008;6:343–68. doi: 10.1586/14779072.6.3.343. [DOI] [PubMed] [Google Scholar]
- 7.Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB, Sr, O'Donnell CJ. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007;116:39–48. doi: 10.1161/CIRCULATIONAHA.106.675355. [DOI] [PubMed] [Google Scholar]
- 8.Neeland IJ, Turer AT, Ayers CR, Powell-Wiley TM, Vega GL, Farzaneh-Far R, Grundy SM, Khera A, McGuire DK, de Lemos JA. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA. 2012;308:1150–9. doi: 10.1001/2012.jama.11132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vega GL, Adams-Huet B, Peshock R, Willett D, Shah B, Grundy SM. Influence of body fat content and distribution on variation in metabolic risk. J Clin Endocrinol Metab. 2006;91:4459–66. doi: 10.1210/jc.2006-0814. [DOI] [PubMed] [Google Scholar]
- 10.Fox CS, Gona P, Hoffmann U, Porter SA, Salton CJ, Massaro JM, Levy D, Larson MG, D'Agostino RB, Sr, O'Donnell CJ, Manning WJ. Pericardial fat, intrathoracic fat, and measures of left ventricular structure and function: the Framingham Heart Study. Circulation. 2009;119:1586–91. doi: 10.1161/CIRCULATIONAHA.108.828970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu J, Fox CS, Hickson DA, May WL, Ding J, Carr JJ, Taylor HA. Pericardial fat and echocardiographic measures of cardiac abnormalities: the Jackson Heart Study. Diabetes Care. 2011;34:341–6. doi: 10.2337/dc10-1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rider OJ, Francis JM, Ali MK, Byrne J, Clarke K, Neubauer S, Petersen SE. Determinants of left ventricular mass in obesity; a cardiovascular magnetic resonance study. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance. 2009;11:9. doi: 10.1186/1532-429X-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zile MR, Gottdiener JS, Hetzel SJ, McMurray JJ, Komajda M, McKelvie R, Baicu CF, Massie BM, Carson PE, Investigators IP. Prevalence and significance of alterations in cardiac structure and function in patients with heart failure and a preserved ejection fraction. Circulation. 2011;124:2491–501. doi: 10.1161/CIRCULATIONAHA.110.011031. [DOI] [PubMed] [Google Scholar]
- 14.Victor RG, Haley RW, Willett DL, Peshock RM, Vaeth PC, Leonard D, Basit M, Cooper RS, Iannacchione VG, Visscher WA, Staab JM, Hobbs HH. The Dallas Heart Study: a population-based probability sample for the multidisciplinary study of ethnic differences in cardiovascular health. Am J Cardiol. 2004;93:1473–80. doi: 10.1016/j.amjcard.2004.02.058. [DOI] [PubMed] [Google Scholar]
- 15.Deo R, Khera A, McGuire DK, Murphy SA, Meo Neto Jde P, Morrow DA, de Lemos JA. Association among plasma levels of monocyte chemoattractant protein-1, traditional cardiovascular risk factors, and subclinical atherosclerosis. J Am Coll Cardiol. 2004;44:1812–8. doi: 10.1016/j.jacc.2004.07.047. [DOI] [PubMed] [Google Scholar]
- 16.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 17.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 18.Turer AT, Khera A, Ayers CR, Turer CB, Grundy SM, Vega GL, Scherer PE. Adipose tissue mass and location affect circulating adiponectin levels. Diabetologia. 2011;54:2515–24. doi: 10.1007/s00125-011-2252-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdullah SM, Khera A, Leonard D, Das SR, Canham RM, Kamath SA, Vega GL, Grundy SM, McGuire DK, de Lemos JA. Sex differences in the association between leptin and CRP: results from the Dallas Heart Study. Atherosclerosis. 2007;195:404–10. doi: 10.1016/j.atherosclerosis.2006.10.022. [DOI] [PubMed] [Google Scholar]
- 20.Tikuisis P, Meunier P, Jubenville CE. Human body surface area: measurement and prediction using three dimensional body scans. Eur J Appl Physiol. 2001;85:264–71. doi: 10.1007/s004210100484. [DOI] [PubMed] [Google Scholar]
- 21.Abate N, Garg A, Coleman R, Grundy SM, Peshock RM. Prediction of total subcutaneous abdominal, intraperitoneal, and retroperitoneal adipose tissue masses in men by a single axial magnetic resonance imaging slice. Am J Clin Nutr. 1997;65:403–8. doi: 10.1093/ajcn/65.2.403. [DOI] [PubMed] [Google Scholar]
- 22.Drazner MH, Dries DL, Peshock RM, Cooper RS, Klassen C, Kazi F, Willett D, Victor RG. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: the Dallas Heart Study. Hypertension. 2005;46:124–9. doi: 10.1161/01.HYP.0000169972.96201.8e. [DOI] [PubMed] [Google Scholar]
- 23.Karason K, Sjostrom L, Wallentin I, Peltonen M. Impact of blood pressure and insulin on the relationship between body fat and left ventricular structure. Eur Heart J. 2003;24:1500–5. doi: 10.1016/s0195-668x(03)00312-9. [DOI] [PubMed] [Google Scholar]
- 24.Bella JN, Devereux RB, Roman MJ, O'Grady MJ, Welty TK, Lee ET, Fabsitz RR, Howard BV. Relations of left ventricular mass to fat-free and adipose body mass: the strong heart study. The Strong Heart Study Investigators. Circulation. 1998;98:2538–44. doi: 10.1161/01.cir.98.23.2538. [DOI] [PubMed] [Google Scholar]
- 25.Neeland IJ, Ayers CR, Rohatgi AK, Turer AT, Berry JD, Das SR, Vega GL, Khera A, McGuire DK, Grundy SM, de Lemos JA. Associations of visceral and abdominal subcutaneous adipose tissue with markers of cardiac and metabolic risk in obese adults. Obesity (Silver Spring) 2012 Nov 6; doi: 10.1002/oby.20135. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, Keaney JF, Jr, Meigs JB, Lipinska I, Kathiresan S, Murabito JM, O'Donnell CJ, Benjamin EJ, Fox CS. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation. 2007;116:1234–41. doi: 10.1161/CIRCULATIONAHA.107.710509. [DOI] [PubMed] [Google Scholar]
- 27.Fox ER, Sarpong DF, Cook JC, Samdarshi TE, Nagarajarao HS, Liebson PR, Sims M, Howard G, Garrison R, Taylor HA., Jr The relation of diabetes, impaired fasting blood glucose, and insulin resistance to left ventricular structure and function in African Americans: the Jackson Heart Study. Diabetes Care. 2011;34:507–9. doi: 10.2337/dc10-0838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nikolaidis LA, Sturzu A, Stolarski C, Elahi D, Shen YT, Shannon RP. The development of myocardial insulin resistance in conscious dogs with advanced dilated cardiomyopathy. Cardiovascular Research. 2004;61:297–306. doi: 10.1016/j.cardiores.2003.11.027. [DOI] [PubMed] [Google Scholar]
- 29.Baglioni S, Cantini G, Poli G, Francalanci M, Squecco R, Di Franco A, Borgogni E, Frontera S, Nesi G, Liotta F, Lucchese M, Perigli G, Francini F, Forti G, Serio M, Luconi M. Functional differences in visceral and subcutaneous fat pads originate from differences in the adipose stem cell. PLoS One. 2012;7:e36569. doi: 10.1371/journal.pone.0036569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rame JE. Chronic heart failure: a reversible metabolic syndrome? Circulation. 2012;125:2809–11. doi: 10.1161/CIRCULATIONAHA.112.108316. [DOI] [PubMed] [Google Scholar]
- 31.Manolopoulos KN, Karpe F, Frayn KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes (Lond) 2010;34:949–59. doi: 10.1038/ijo.2009.286. [DOI] [PubMed] [Google Scholar]
- 32.Snijder MB, Henry RM, Visser M, Dekker JM, Seidell JC, Ferreira I, Bouter LM, Yudkin JS, Westerhof N, Stehouwer CD. Regional body composition as a determinant of arterial stiffness in the elderly: The Hoorn Study. J Hypertens. 2004;22:2339–47. doi: 10.1097/00004872-200412000-00016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.