Abstract
Myositis ossificans is a disease that is characterized by nonneoplastic, heterotopic bone formation within a muscle. Myositis ossificans traumatica, also called myositis ossificans circumscripta, is a disease in which muscles are ossified presumably following acute trauma, burns, surgical manipulation, or repeated injury. It is often remitted after surgical excision though some patients have repeated recurrences. Myositis ossificans traumatica of masticatory muscles is not frequently reported in the literature, with the most common clinical finding being a progressive limitation of motion in the mandible. The aim of this article is to present and discuss a case of myositis ossificans traumatica of the left medial pterygoid muscle and to review the literature of myositis ossificans of the masticatory muscles.
Keywords: myositis ossificans, myositis ossificans traumatica, masticatory muscles, temporomandibular joint, prosthesis
Myositis ossificans (MO) is a disease that is characterized by nonneoplastic, heterotopic bone formation within a muscle. MO can be classified into MO progressive (or fibrodysplasia ossificans progressive), that is the autosomal dominant disease with multiple, heterotopic ossifications in the systemic muscle, fascia, tendons, and ligaments, and MO traumatica.1 2 3 4 5 6
MO traumatica, also called MO circumscripta, is a disease in which muscles are ossified presumably following acute trauma, burns, surgical manipulation, or repeated injury.1 3 4
Unlike MO progressive, MO traumatica is often remitted after surgical excision though some patients have repeated recurrences.1
MO traumatica of masticatory muscles is not frequently reported in the literature,1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 with the most common clinical finding being a progressive limitation of motion in the mandible.2 3 4
The aim of this article is to present and discuss a case of MO traumatica of the left medial pterygoid muscle and to review the literature of MO of the masticatory muscles.
Case Report
A 37-year-old woman referred to the Division of Maxillofacial Surgery of the University of Turin with a complaint of trismus. She reported a blow to the left side of her face several years before and a progressively increasing limitation of mandibular motion for the last 2 years. Her medical and family history was unremarkable.
At clinical examination, she had trismus, with a maximum interincisal opening of the mouth of 5 mm. The patient was also unable to protrude or produce a left lateral excursion. The occlusion was stable, without significant intraoral findings. Neither swelling nor pain of the left side of her face could be appreciated on palpation (Fig. 1). Submandibular and cervical lymph nodes were nonpalpable and nontender. Results of hemogram and tests for serum phosphatase, parathyroid hormone, and calcitonin were within normal limits. A panoramic radiograph revealed a radiopaque calcified region with apparent bony features in correspondence of the left coronoid process and sigmoid notch. (Fig. 2) Axial and coronal computed tomography (CT) scans confirmed the presence of irregular heterotopic calcification involving the left medial pterygoid muscle (Figs. 3 and 4).
Figure 1.

Preoperative frontal (A) and lateral (B) images of the patient.
Figure 2.

Panoramic radiograph revealing a radiopaque calcified region with apparent bony features in correspondence of the left coronoid process and sigmoid notch.
Figure 3.
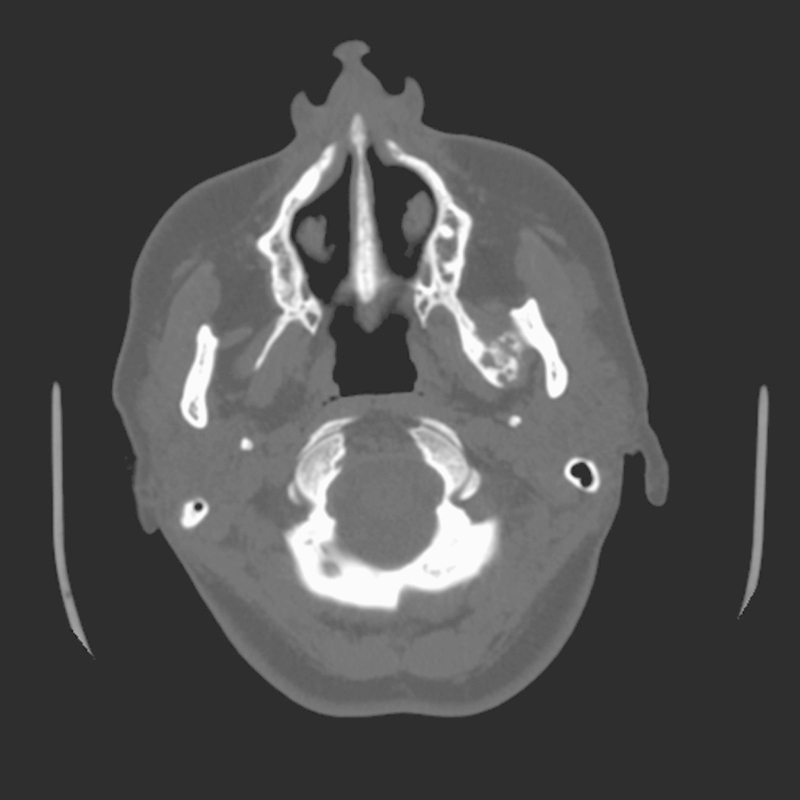
Axial computed tomography scan confirming the presence of irregular heterotopic calcification involving the left medial pterygoid muscle.
Figure 4.
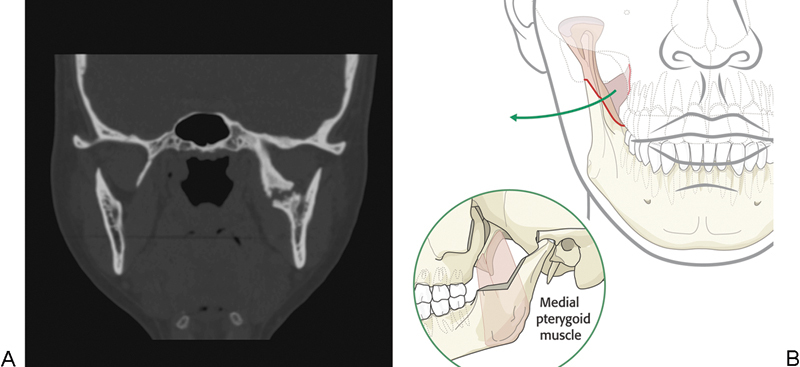
(A) Coronal computed tomography scan confirming the presence of irregular heterotopic calcification involving the left medial pterygoid muscle. (B) The medial pterygoid muscle origin is on the bottom of the mandible, but in this pathological case the ossification of some muscular fibers did not reach the bottom of the mandible. Therefore, the osteotomy was made to remove just the inner corticle and to remove the condyle.
Surgical excision of the ossification was planned under general anesthesia.
After fiber optic-assisted nasotracheal intubation, a combined intraoral and extraoral (submandibular and preauricular) approach was performed. The calcified mass within the left medial pterygoid muscle was exposed and completely excised together with the left coronoid and condyle by surgical burs and trimmer. After removal of the fused mass and site preparation, Biomet/W Lorenz Surgical System temporomandibular joint (TMJ) prosthesis (Biomet/Lorenz, Warsaw, IN) with condylar and fossa components was placed. An intraoperative interincisal mouth opening of 35 mm was achieved. The wound was closed in layers after complete hemostasis.
Histopathological examination showed heterotopic foci of osteoid woven bone, cartilage, and collagen fibers consistent with the diagnosis of MO.
Aggressive jaw physical therapy was started postoperatively. A rigorous physiotherapy was recommended, and the patient was regularly followed up. Follow-up at 30 days confirmed the restoration of the posterior ramus height and the maintained facial symmetry (Fig. 5); furthermore, maximum spontaneous opening mouth recovered to 31 mm. Postoperative radiographs showed excision of the ossification and the correct placement of the TMJ prosthesis (Figs. 6 and 7). Follow-up at 3 years was unremarkable without any evidence of recurrence.
Figure 5.

Postoperative frontal (A) and lateral (B) images of the patient confirming the maintained facial symmetry after surgical treatment.
Figure 6.

Postoperative panoramic radiograph showing the excision of the ossification and the correct placement of the temporomandibular joint prosthesis.
Figure 7.
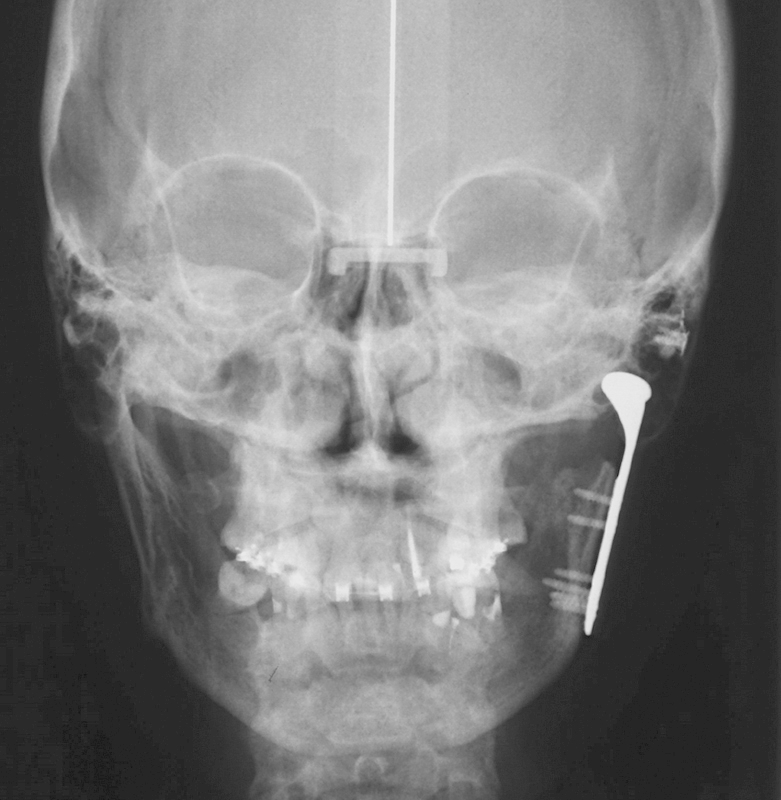
Postoperative posteroanterior cranial radiograph confirming the correct placement of the temporomandibular joint prosthesis.
Discussion
MO traumatica is an extraskeletal bone-forming disease in the head and neck region.4
The term “MO traumatica” may be inadequate to describe this disorder, because in various cases a history of trauma cannot be recognized3 4 7 15 32 and there is little inflammation.
The pathogenesis of MO is still controversial and several theories have been proposed. The most widely accepted theory involves the differentiation of extraosseous cells exposed to bone morphogenic proteins that would have been released from native bone sources following trauma or surgical injury.1 2 4
Other theories suggested the displacement of bony fragments into the surrounding tissue and hematoma with subsequent bony proliferation, the detachment of periosteal fragments into the soft tissue with proliferation of osteoprogenitor cells, or the migration of subperiosteal osteoprogenitor cells into surrounding tissue through periosteal perforations.2
Laboratory tests are usually within normal ranges, except for some cases with a reported elevated alkaline phosphatase level that might be due to disease progression.4
An English literature review revealed 42 cases of MO of the masticatory muscles, including our case. The results are shown in Table 1. Mean age of affected patients is 38.1 years (range, 15–73 y; median, 34 y; standard deviation, 14.2). Men were 29, whereas female patients were 12, with a ratio M:F of 2.4:1.
Table 1. Review of cases of myositis ossificans of masticatory muscles in the literature.
| Case | Author | Year | Age | Sex | Location | History of trauma | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | Ivy and Eby7 | 1924 | Masseter | Unknown | Excision/removal of the entire muscle | Immediate full opening, no follow-up | ||
| 2 | Cameron and Stetzer8 | 1945 | 28 | M | Masseter | Fall | Excision | Recurrence in 6 mo, reintervention |
| 3 | Nizel and Prigge9 | 1946 | 21 | M | Masseter | Gunshot | Expansion appliance/exercise | No follow-up |
| 4 | Kostrubala and Talbot10 | 1948 | 21 | M | Masseter | Gunshot | Excision/removal of the entire muscle | Recurrence in 1 mo, second intervention with dermal graft; good function 9 mo later |
| 5 | Davidoff11 | 1955 | 53 | M | Masseter | Contusion | Excision | No follow-up |
| 6 | Goodsell12 | 1962 | 39 | M | Masseter | Blow | Excision | No recurrence |
| 7 | Palumbo et al13 | 1964 | 52 | M | Masseter | Blow | Excision/removal of the entire muscle | No recurrence |
| 8 | Parnes and Hinds14 | 1965 | 27 | M | Masseter | Blow and bite wound | Excision | No recurrence |
| 9 | Hellinger15 | 1965 | 21 | F | Masseter, temporali, lateral pterygoid | Unknown | Biopsy | No follow-up |
| 10 | Shawkat16 | 1967 | 24 | M | Masseter, temporalis | Blow, tooth extraction | Excision | No recurrence |
| 11 | Vernale17 | 1968 | 29 | M | Masseter | Contusion | Excision | No recurrence |
| 12 | Vernale17 | 1968 | 31 | M | Masseter | Traffic accident | Excision | No recurrence |
| 13 | Trester et al18 | 1969 | 29 | F | Masseter | Overturning | Excision | Recurrence in 1 mo |
| 14 | Narang and Dixon19 | 1974 | 49 | M | Medial pterygoid | Tooth extraction | Excision | Recurrence in 1 mo |
| 15 | Plezia et al20 | 1977 | 47 | F | Masseter | Contusion | Excision | No recurrence |
| 16 | Christmas and Ferguson21 | 1982 | 51 | M | Masseter | Fall | Excision | No recurrence |
| 17 | Abdin and Prabhu22 | 1984 | 43 | F | Lateral pterygoid | Drainage after odontogenic infection | Excision | No recurrence |
| 18 | Arima et al23 | 1984 | 25 | M | Masseter | Struck on the cheek | Excision | No recurrence |
| 19 | Lello and Makek24 | 1986 | 31 | F | Masseter | Anesthetic injection | Excision | No recurrence |
| 20 | Lello and Makek24 | 1986 | 32 | M | Masseter | Struck on the cheek | Excision | No recurrence |
| 21 | Lello and Makek24 | 1986 | 34 | M | Temporal, lateral pterygoid | Traffic accident | Excision | No recurrence |
| 22 | Nilner and Petersson25 | 1989 | 57 | M | Medial pterygoid | Anesthetic injection | Physical therapy | Unknown |
| 23 | Parkash and Goyal26 | 1992 | 28 | M | Medial pterygoid | Pericoronitis | Excision, condylectomy, coronoidectomy | No recurrence |
| 24 | Tong et al27 | 1994 | 73 | F | Bilateral medial pterygoid | Anesthetic injection | Biopsy | Unknown |
| 25 | Steiner et al28 | 1997 | 40 | M | Masseter | Mandibular fracture | Excision | No recurrence |
| 26 | Steiner et al28 | 1997 | 15 | F | Masseter | Shotgun wound | Excision, coronoidectomy | No recurrence |
| 27 | Spinazze et al29 | 1998 | 55 | M | Masseter, temporal, lateral pterygoid, medial pterygoid | Periodontal surgery | Coronoidectomy | Twice recurrence (then excision, then arthroplasty plus osteotomy) |
| 28 | Myoken et al30 | 1998 | 53 | M | Bilateral temporal, masseter | Laceration over ear | Excision | Unknown |
| 29 | Geist et al31 | 1998 | 44 | M | Masseter | Mandibular fracture | Excision | Unknown |
| 30 | Takahashi and Sato32 | 1999 | 71 | F | Medial pterygoid | Unknown | Excision | No recurrence |
| 31 | Aoki et al1 | 2002 | 44 | M | Masseter, lateral pterygoid, medial pterygoid | Struck on the cheek | Excision | Recurrence |
| 32 | Kim et al4 | 2002 | 30 | F | Bilateral lateral pterygoid | Unknown | Excision | Recurrence (excision and interpositional fat graft) |
| 33 | Saka et al33 | 2002 | 33 | M | Temporal | Blunt trauma | Excision | No recurrence |
| 34 | Yano et al34 | 2005 | 34 | M | Bilateral masseter | Violence | Excision and coronoidectomy | No recurrence |
| 35 | Rattan et al6 | 2008 | 45 | M | Medial pterygoid | Alcohol injection for trigeminal neuralgia | Excision and buccal fat pad | No recurrence |
| 36 | Conner and Duffy2 | 2009 | 18 | F | Medial pterygoid, temporal | Surgical extraction of third molars | Excision and coronoidectomy | Twice recurrence (then mandibular resection, then condylar disarticulation) |
| 37 | Ramieri et al5 | 2010 | 64 | M | Lateral pterygoid, temporal. Then Medial pterygoid | Tooth extraction | High condylectomy, then excision | Unknown |
| 38 | Trautmann et al35 | 2010 | 33 | M | Medial pterygoid | Anesthetic injection, coronoidectomy | Excision | Unknown |
| 39 | Godhi et al3 | 2011 | 21 | M | Temporal, bilateral lateral pterygoid | Unknown | Excision | No recurrence |
| 40 | Thangavelu et al36 | 2011 | 36 | F | Medial pterygoid | Tooth extraction | Excision and interpositional fat graft | No recurrence |
| 41 | Ebbert et al37 | 2012 | 45 | M | Bilateral medial and lateral pterygoid | Tooth extraction | Surgery deferred | Unknown |
| 42 | Present case | 2012 | 37 | F | Medial pterygoid | Unknown | Excision, condylectomy and TMJ prosthesis | No recurrence |
Abbreviation: F, female; M, male; mo, month(s).
In 29 patients only a masticatory muscle was involved, while in the remaining 13 cases two or more muscles were affected by MO. Masseter was the most frequently involved muscle, with 25 patients, followed by medial pterygoid muscle (14 patients), lateral pterygoid muscle (9 patients), and temporalis muscle (5 patients).
The higher incidence of MO of masseter may be attributed to the external position of this muscle that is likely to receive a direct trauma.1
The most frequent subjective symptom of MO is trismus,1 3 that should be differentiated from trismus related to perimandibular inflammation or abscess, tumor, trauma, or TMJ diseases.38 39
Diagnosis of MO may be challenging, and an accurate history is essential, as a history of trauma, previous surgical intervention, or injection was recognized in 35 cases.2
On plain radiographs, that are usually performed first, it may be difficult to identify the real amount and site of ossification because of the superimposition of the cranial bones.1 2 CT scans are fundamental to perform a correct diagnosis, and to accurately plan a surgical treatment.
The pathognomonic feature of MO is a well-circumscribed, high-attenuating periphery with a low-attenuating central portion, whereas lesions may or may not be attached to the adjacent bone depending on the maturity of MO.
As Kim et al4 said, early lesions of the axial skeletons are reported to appear as amorphous calcifications within soft tissue, more mature lesions appear well circumscribed with a ring of calcification surrounding a relatively radiolucent central portion, and finally long-standing lesions may appear diffusely calcified and attached to the adjacent bone.
Histopathologically, MO typically present a peripheral zone with mature lamellar bone and active osteoclasts, an intermediate area made up of osteoid and cartilage, and a central cellular area with proliferating fibroblasts, spindle cells, and prominent giant mesenchymal cells.4 33
Several different treatment strategies of MO have been proposed in the literature: mostly, a simple excision of the calcified mass was performed (25 cases). Some surgeons proposed a further surgical phase in addition to the excision of the mass: the removal of the entire muscle (3 cases), a coronoidectomy and/or condylectomy (6 cases), or an interpositional fat graft (2 cases). Interestingly, some authors just performed a biopsy or suggested functional exercise.9 15 25 27
Therefore, treatment of MO is controversial and may be challenging. There are no treatment protocols, as the literature almost always just includes single case reports, and authors are often unclear as for surgical timing.2 In particular, some authors insist that early surgical intervention (within 3–6 wk postinjury) is ideal for curative excision,14 23 whereas others have stated that surgical intervention should be initiated only when the disease has completely halted.2 Biopsy is usually contraindicated, though a biopsy is often performed to exclude the possibility of malignant tumors.3 However, complete excision of the ossified mass seems to be the universally accepted treatment for this disease.
On the other hand, reconstruction options vary widely and are much more controversial. In fact, several authors did not perform any reconstruction after the removal of the ossified mass, whereas few articles mentioned the use of interpositional fat graft.6 36
Literature data about recurrences are quite poor, as few articles offer follow-up greater than 1 year.2
We decided to perform a total TMJ replacement in addition to the removal of the mass, the coronoidectomy, and the condylectomy. The aim of this treatment was to avoid a relapse of the disease and to allow a reestablished mandibular motion. The use of a total alloplastic TMJ prosthesis may give several advantages in comparison with other surgical reconstruction techniques: in fact, physical therapy can begin immediately, there is no need of donor site, the restoration of the posterior ramus height can be immediately obtained after the removal of the mass, and last but not the least facial symmetry can be maintained too.
In conclusion, recommendations about treatment of MO should be cautiously made as limited data are available about recurrences and long-term follow-up.
Note
This article was exempt from Institutional Review Board approval being a case report. We followed Helsinki declaration guidelines.
References
- 1.Aoki T, Naito H, Ota Y, Shiiki K. Myositis ossificans traumatica of the masticatory muscles: review of the literature and report of a case. J Oral Maxillofac Surg. 2002;60(9):1083–1088. doi: 10.1053/joms.2002.34427. [DOI] [PubMed] [Google Scholar]
- 2.Conner G A, Duffy M. Myositis ossificans: a case report of multiple recurrences following third molar extractions and review of the literature. J Oral Maxillofac Surg. 2009;67(4):920–926. doi: 10.1016/j.joms.2008.06.106. [DOI] [PubMed] [Google Scholar]
- 3.Godhi S S, Singh A, Kukreja P, Singh V. Myositis ossificans circumscripta involving bilateral masticatory muscles. J Craniofac Surg. 2011;22(6):e11–e13. doi: 10.1097/SCS.0b013e31822ec7cc. [DOI] [PubMed] [Google Scholar]
- 4.Kim D D, Lazow S K, Har-El G, Berger J R. Myositis ossificans traumatica of masticatory musculature: A case report and literature review. J Oral Maxillofac Surg. 2002;60(9):1072–1076. doi: 10.1053/joms.2002.34424. [DOI] [PubMed] [Google Scholar]
- 5.Ramieri V, Bianca C, Arangio P, Cascone P. Myositis ossificans of the medial pterygoid muscle. J Craniofac Surg. 2010;21(4):1202–1204. doi: 10.1097/SCS.0b013e3181e17cfa. [DOI] [PubMed] [Google Scholar]
- 6.Rattan V, Rai S, Vaiphei K. Use of buccal pad of fat to prevent heterotopic bone formation after excision of myositis ossificans of medial pterygoid muscle. J Oral Maxillofac Surg. 2008;66(7):1518–1522. doi: 10.1016/j.joms.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 7.US Army Surgeon General's Office. The Medical Department of the United States Army in the World War, volume 11: Surgery; Part One, General Surgery, Orthopedic Surgery, Neurosurgery In: Washington, DC: Otis Historical Archives, National Museum of Health and Medicine; 1927458 [Google Scholar]
- 8.Cameron J R, Stetzer J J. Myositis ossificans of right masseter muscle: Report of a case. J Oral Surg. 1945;3:170–173. [Google Scholar]
- 9.Nizel A E, Prigge E K. Trismus due to myositis ossificans traumatica; report of a case. J Oral Surg (Chic) 1946;4:93–101. [PubMed] [Google Scholar]
- 10.Kostrubala J G, Talbot R J. Myositis ossificans of the masseter muscle. A case report. Plast Reconstr Surg. 1948;3:52–55. [PubMed] [Google Scholar]
- 11.Davidoff S M. Ein fall von posttraumatischer myositis ossificans des linken masseter. Dtsch Stomatol. 1955;5:554–558. [Google Scholar]
- 12.Goodsell J O. Traumatic myositis ossificans of the masseter muscle: review of the literature and report of a case. J Oral Surg Anesth Hosp Dent Serv. 1962;20:116–122. [PubMed] [Google Scholar]
- 13.Palumbo V D, Sills A H, Hinds E C. Limited mandibular motion associated with bone pathosis. Report of cases. J Oral Surg. 1964;22:531–537. [Google Scholar]
- 14.Parnes E I, Hinds E C. Traumatic myositis ossificans of the masseter muscle. Report of a case. J Oral Surg. 1965;23:245–250. [PubMed] [Google Scholar]
- 15.Hellinger M J. Myositis ossificans of the muscles of mastication. Oral Surg Oral Med Oral Pathol. 1965;19:581–587. doi: 10.1016/0030-4220(65)90398-1. [DOI] [PubMed] [Google Scholar]
- 16.Shawkat A H. Myositis ossificans. Report of a case. Oral Surg Oral Med Oral Pathol. 1967;23(6):751–754. doi: 10.1016/0030-4220(67)90364-7. [DOI] [PubMed] [Google Scholar]
- 17.Vernale C A. Traumatic myositis ossificans of the masseter muscle. Report of two cases. Oral Surg Oral Med Oral Pathol. 1968;26(1):8–17. doi: 10.1016/0030-4220(68)90215-6. [DOI] [PubMed] [Google Scholar]
- 18.Trester P H, Markovitch E, Zambito R F, Stratigos G T. Myositis ossificans, circumscripta and progressiva, with surgical correction of the masseter muscle: report of two cases. J Oral Surg. 1969;27(3):201–205. [PubMed] [Google Scholar]
- 19.Narang R, Dixon R A Jr. Myositis ossificans: medial pterygoid muscle—a case report. Br J Oral Surg. 1974;12(2):229–234. doi: 10.1016/0007-117x(74)90130-9. [DOI] [PubMed] [Google Scholar]
- 20.Plezia R A, Mintz S M, Calligaro P. Myositis ossificans traumatica of the masseter muscle. Report of a case. Oral Surg Oral Med Oral Pathol. 1977;44(3):351–357. doi: 10.1016/0030-4220(77)90402-9. [DOI] [PubMed] [Google Scholar]
- 21.Christmas P I, Ferguson J W. Traumatic myositis ossificans. Br J Oral Surg. 1982;20(3):196–199. doi: 10.1016/s0007-117x(82)80038-3. [DOI] [PubMed] [Google Scholar]
- 22.Abdin H A, Prabhu S R. Traumatic myositis ossificans of lateral pterygoid muscle. J Oral Med. 1984;39(1):54–56. [PubMed] [Google Scholar]
- 23.Arima R, Shiba R, Hayashi T. Traumatic myositis ossificans in the masseter muscle. J Oral Maxillofac Surg. 1984;42(8):521–526. doi: 10.1016/0278-2391(84)90011-9. [DOI] [PubMed] [Google Scholar]
- 24.Lello G E, Makek M. Traumatic myositis ossificans in masticatory muscles. J Maxillofac Surg. 1986;14(4):231–237. doi: 10.1016/s0301-0503(86)80295-8. [DOI] [PubMed] [Google Scholar]
- 25.Nilner M, Petersson A. Mandibular limitation due to enlarged pterygoid process and calcification of the medial pterygoid muscle. A case report. Cranio. 1989;7(3):230–234. doi: 10.1080/08869634.1989.11678289. [DOI] [PubMed] [Google Scholar]
- 26.Parkash H, Goyal M. Myositis ossificans of medial pterygoid muscle. A cause for temporomandibular joint ankylosis. Oral Surg Oral Med Oral Pathol. 1992;73(1):27–28. doi: 10.1016/0030-4220(92)90149-k. [DOI] [PubMed] [Google Scholar]
- 27.Tong K A, Christiansen E L, Heisler W, Hinshaw D B Jr, Hasso A N. Asymptomatic myositis ossificans of the medial pterygoid muscles: a case report. J Orofac Pain. 1994;8(2):223–226. [PubMed] [Google Scholar]
- 28.Steiner M, Gould A R, Kushner G M, Lutchka B, Flint R. Myositis ossificans traumatica of the masseter muscle: review of the literature and report of two additional cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(6):703–707. doi: 10.1016/s1079-2104(97)90376-0. [DOI] [PubMed] [Google Scholar]
- 29.Spinazze R P, Heffez L B, Bays R A. Chronic, progressive limitation of mouth opening. J Oral Maxillofac Surg. 1998;56(10):1178–1186. doi: 10.1016/s0278-2391(98)90767-4. [DOI] [PubMed] [Google Scholar]
- 30.Myoken Y, Sugata T, Tanaka S. Traumatic myositis ossificans of the temporal and masseter muscle. Br J Oral Maxillofac Surg. 1998;36(1):76. doi: 10.1016/s0266-4356(98)90767-7. [DOI] [PubMed] [Google Scholar]
- 31.Geist J R, Bhatti P, Plezia R A, Wesley R K. Fibrodysplasia ossificans circumscripta of the masseter muscle. Dentomaxillofac Radiol. 1998;27(3):182–185. doi: 10.1038/sj/dmfr/4600341. [DOI] [PubMed] [Google Scholar]
- 32.Takahashi K, Sato K. Myositis ossificans traumatica of the medial pterygoid muscle. J Oral Maxillofac Surg. 1999;57(4):451–456. doi: 10.1016/s0278-2391(99)90289-6. [DOI] [PubMed] [Google Scholar]
- 33.Saka B, Stropahl G, Gundlach K K. Traumatic myositis ossificans (ossifying pseudotumor) of temporal muscle. Int J Oral Maxillofac Surg. 2002;31(1):110–111. doi: 10.1054/ijom.2001.0118. [DOI] [PubMed] [Google Scholar]
- 34.Yano H, Yamamoto H, Hirata R, Hirano A. Post-traumatic severe trismus caused by impairment of the masticatory muscle. J Craniofac Surg. 2005;16(2):277–280. doi: 10.1097/00001665-200503000-00014. [DOI] [PubMed] [Google Scholar]
- 35.Trautmann F, Moura Pd, Fernandes T L, Gondak R O, Castilho J C, Filho E M. Myositis ossificans traumatica of the medial pterygoid muscle: a case report. J Oral Sci. 2010;52(3):485–489. doi: 10.2334/josnusd.52.485. [DOI] [PubMed] [Google Scholar]
- 36.Thangavelu A, Vaidhyanathan A, Narendar R. Myositis ossificans traumatica of the medial pterygoid. Int J Oral Maxillofac Surg. 2011;40(5):545–549. doi: 10.1016/j.ijom.2010.10.024. [DOI] [PubMed] [Google Scholar]
- 37.Ebbert T L, Baima J J Jr, Smoker W R. Radiology quiz case 1. Myositis ossificans of the bilateral medial and lateral pterygoid muscles. Arch Otolaryngol Head Neck Surg. 2012;138(4):422–423. doi: 10.1001/archoto.2012.62a. [DOI] [PubMed] [Google Scholar]
- 38.Gerbino G, Boffano P, Tosco P, Berrone S. Long-term clinical and radiological outcomes for the surgical treatment of mandibular condylar fractures. J Oral Maxillofac Surg. 2009;67(5):1009–1014. doi: 10.1016/j.joms.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 39.Boffano P, Roccia F, Pittoni D, Di Dio D, Forni P, Gallesio C. Management of 112 hospitalized patients with spreading odontogenic infections: correlation with DMFT and oral health impact profile 14 indexes. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(2):207–213. doi: 10.1016/j.tripleo.2011.02.006. [DOI] [PubMed] [Google Scholar]