Abstract
This report describes a treatment modification for a patient presented with severely resorbed bilateral edentulous posterior mandible and mobility of the anterior teeth. There was less than 8 mm of bone between the crest of the alveolar ridge and the mandibular canal as revealed by radiographic examination. A modified technique for inferior alveolar nerve lateralization (IANL) in conjunction with ridge expansion was performed using threaded bone expanders, which allowed for better primary stability and placing longer implants. A total of four postextraction implants were in the anterior region of the mandible. The mandible received a total of nine one-piece implants to allow for immediate nonfunctional loading. The definitive ceramometallic prosthesis was delivered 3 months postoperatively. The 10 years clinical and radiographic assessment showed minimal bone resorption around osseointegrated implants. One-piece implants showed great success rate and minimal bone resorption following the modified technique of IANL and immediate implantation.
Keywords: inferior alveolar nerve lateralization, threaded bone expanders, one-piece implants, immediate provisionalization, postextraction implants
During the past 40 years, prosthetic rehabilitation of edentulous patients with implant-supported prosthesis has developed into a viable and predictable treatment option. The fact that long-term studies have reported high-clinical survival rates with the original protocols, has given clinicians and researchers' confidence to further develop and refine the osseointegration technique. Consequently, implants have been used in more challenging situations and for wider indications.1 2
The posterior mandible presents a challenge to clinicians because of the presence of the inferior alveolar nerve (IAN). Bone grafting procedures to increase the bone volume available for implant placement may be a viable treatment option. Such procedures often imply demanding surgical procedures and can be associated with complications, morbidity, and high costs. Therefore, their acceptance by patients is often poor.3 4
Transposition of the IAN has been suggested as an alternative treatment to allow placement of longer implants, better initial stabilization, and reduced treatment time.5 However, the conflicting results from studies that have determined the incidence of IAN dysesthesia with this procedure have created debate as to its appropriate use.6
A similar trend is seen for the timing of implant loading. The original Brånemark protocol recommended long stress-free healing periods to achieve the osseointegration of dental implants. However, in recent years, this clinical suggestion has been challenged. Numerous practitioners now advocate immediate or early loading of implants. The advantages of immediately loaded implants are clear. They require shorter treatment periods and allow immediate recovery of function and esthetics. High success rates of immediately loaded implants are widely reported in previous reviews.4 7
The purpose of this clinical report is to describe the treatment of a patient with a severely resorbed posterior edentulous mandible affecting the removable partial denture's stability. A modified technique of lateralization of the IAN in conjunction with expansion of the mandibular ridge was performed. One-piece implants were then inserted followed by immediate loading. The clinical and radiographic outcomes after 10 years are presented.
Clinical Report
A 53-year-old nonsmoking female patient presented for implant rehabilitation of the mandible. She was systemically healthy, taking no medications, and had no drug allergies. Dental examination revealed a completely edentulous maxilla and a severely resorbed bilateral posterior edentulous mandible and mobility of the lower anterior teeth. The patient had a removable maxillary full arch denture and an unstable removable mandibular partial denture. Radiographic examination revealed severe bone atrophy with pneumatization of both maxillary sinuses and an atrophic mandible with less than 8 mm of bone between the crest of the alveolar ridge and the mandibular canal (Figs. 1 and 2). A written informed consent for the treatment was given by the patient.
Figure 1.

Severely resorbed bilateral posterior edentulous mandible and periodontal disease and calculus on the remaining teeth.
Figure 2.

Preoperative orthopantomogram showing atrophic posterior mandible.
The patient received an injection containing 1 vial of methylprednisolone sodium succinate (Solu-Moderín 125 mg, (Pfizer, Alcobendas, Madrid, Spain)) and 1 vial of lincomycin HCl (Lincocin 600 mg, (Pfizer, Alcobendas, Madrid, Spain)) 1 hour preoperatively, and was asked to rinse with 0.2% chlorhexidine gluconate antiseptic solution immediately before surgery. The surgical procedure was performed under local anesthesia; articaine HCl 4% and epinephrine 1:100.000 (Septocaine, (Septodont, Val-de-Marne, Ile-de-France, France)). Infiltration anesthesia was injected over the crest of the alveolar ridge in conjunction with buccal nerve block and infiltration anesthesia of the lingual nerve.
A midcrestal incision was designed through the edentulous span and retromolar pad to allow a minimum of 1- to 2-mm keratinized gingiva on both sides of the flap. A full-thickness mucoperiosteal lingual flap was reflected with extreme caution to prevent tears in the periosteum. The buccal aspect of the alveolar ridge was then exposed via subperiosteal dissection.
Corticotomy was designed following the surgical anatomy of the mandibular nerve. The mandibular neurovascular bundle enters the mandibular canal through the mandibular foramen located on the lingual aspect of the mandibular ramus. During the first 8 to 10 mm, the canal runs close to the lingual cortex, and then it moves toward a more central position downward and forward into the mandibular body. It runs 6 to 8 mm from the mandibular base until it reaches the area between the first and second molars. In this area, it reaches its most lingual and inferior position. Then, it moves upward and runs closer to the buccal cortex until it reaches the mental canal in an increasingly sharp curve. The mental canal is located 3 to 4 mm from the buccal surface, through which 3 to 4 mm of the mental branch of the mandibular nerve runs before it leaves the mandibular body apical to, and between, the first and second premolars.8
The corticotomy was performed in the premolars and first molar area lingual to the crest of the alveolar ridge, using the osteotomy inserts of NSK VarioSurg (NSK, Eschborn, Hesse, Germany), increasing the depth slowly and gradually until it reaches the inferior mandibular cortex. Threaded bone expanders (Microdent implants system, Barcelona, Spain) were then used sequentially to displace the buccal wall, containing the neurovascular bundle, buccally without injuring the nerve, thus atraumatically lateralizing the IAN away from the lingual wall. The expanders also served to prepare the implant bed manually avoiding heat generation by the use of drills. Both the right and left sides received two one-piece implants of 3.85-mm width, 12- and 14-mm length (MRT implants, Microdent implants system, Barcelona, Spain).They were threaded in place with a torque of 40 Ncm. On the left side, in the second molar area distal to the two implants, the pilot drill was used to perform an osteotomy. Bone expanders were used to allow for bone condensation and insertion of another 3.85-mm width, 14-mm length MRT implant. The implant engaged the inferior mandibular border aiming toward a tricortical anchorage (buccal, lingual, and inferior) for greater implant stability. The mucoperiosteal flaps were then sutured back using interrupted and horizontal mattress sutures (Figs. 3 and 4).
Figure 3.
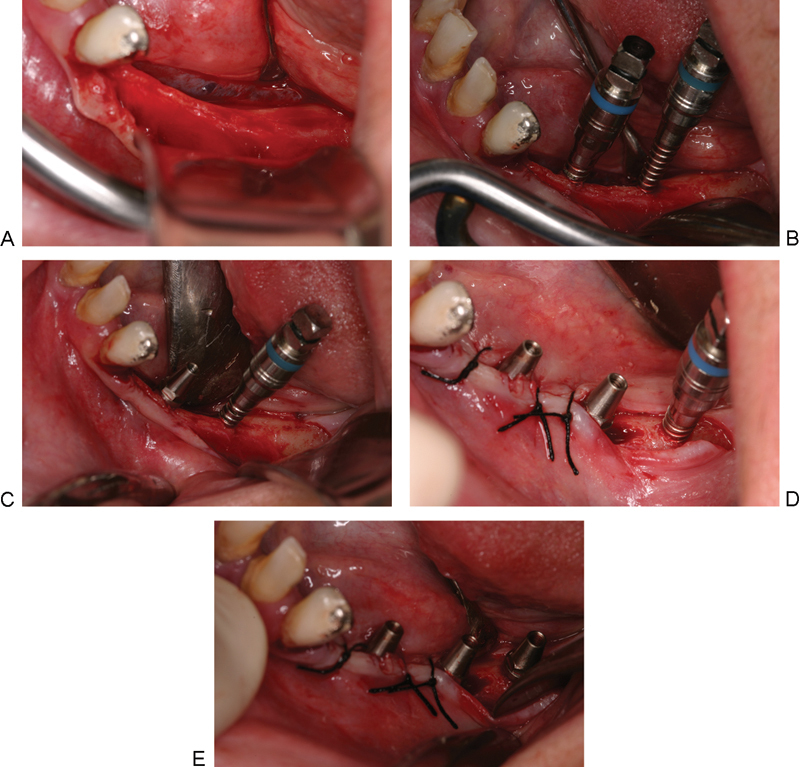
(A) Reflection of the mucoperiosteal flap on the left side and exposure of the alveolar bone, having a width of 2 mm in the premolars area, and 3 mm in the first molar area. (B) Threaded bone expanders no. 2 (color coded, blue) to allow for lateralization of the inferior alveolar nerve and expansion of the resorbed alveolar ridge. (C) The expanders must be maintained in place till the insertion of the implants to avoid collapse of the defect walls. (D) Insertion of two (MRT) implants in the premolars area and bone expander no. 2 in the second molar zone. (E) The three MRT implants in place and suturing back the flap.
Figure 4.
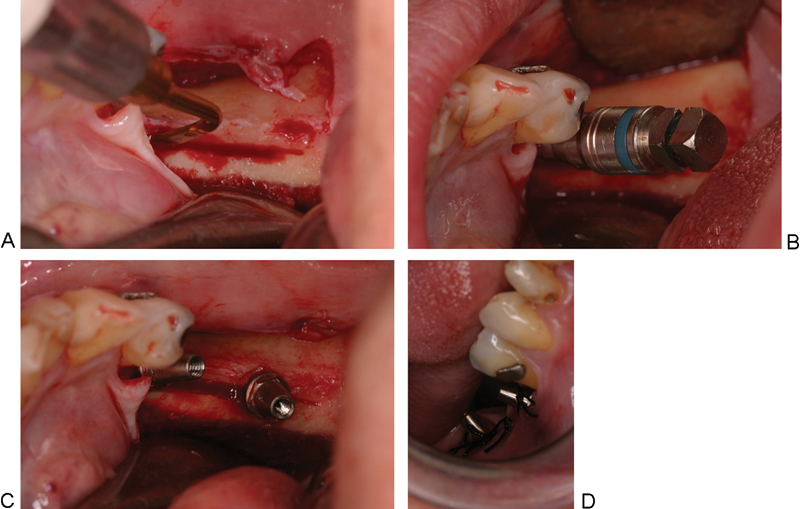
(A) Corticotomy of the right side in the premolar–molar area using piezoelectric surgery. (B) Threaded-bone expander no. 2 to allow for lateralization and expansion. (C) Two MRT implants in place. (D) Suturing back the flap.
The patient was closely observed during the corticotomy procedure for the presence of pain, which indicated closeness to the nerve and thus the need to alter the angulation of the corticotomy. Also, checking regularly the sensation of the lateral side of the lip and chin was fundamental for the presence of any neurosensory disturbance.
Bilateral IAN block anesthesia was then given to the patient and atraumatic simultaneous extraction of the anterior teeth was performed. Four 3.85-mm width MRT postextraction implants were inserted (two implants of 12-mm length and two implants of 14-mm length) (Fig. 5).
Figure 5.
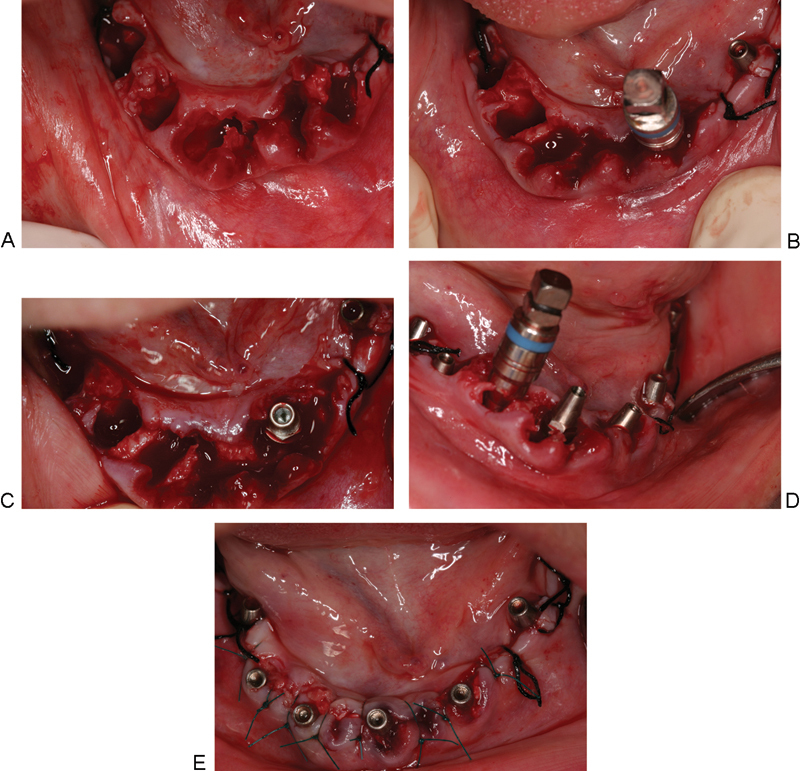
(A) Atraumatic extraction of the six anterior teeth followed by curettage of the sockets and removing any bony spicules using bone rongeur. (B) Drilling 3 mm in the depth of the lingual wall using pilot drill followed by threaded bone expander no. 2 to allow for bone condensation against the walls of the osteotomy, which aids in better implant stability and positioning the implant buccally without compromising esthetics. (C) MRT implant in place. (D) Continue the same procedure in other sockets. (E) Four postextraction MRT implants and positioning back the flap.
All implants had primary stability and were immediately loaded by the fabrication of a nonfunctional simple acrylic resin fixed denture. An orthopantomogram was then performed to check the direction and position of the implants and the passive contact between the provisional prosthesis and the implants.
The postsurgical therapy protocol consisted of injecting the patient with the methylprednisolone sodium succinate 125 mg and Lincomycin 600 mg mixture for 2 days after surgery, together with ibuprofen 600 mg twice daily for 3 days. A soft diet and appropriate oral hygiene were prescribed for 2 weeks, including rinsing with 0.2% chlorhexidine gluconate twice daily. The sutures were removed 10 days after the operation without any postoperative complication. At 12 weeks, impressions were made for the fabrication of the final ceramometallic fixed denture, which was completed using conventional fabrication and prosthetic techniques. It was fabricated in three parts; the anterior four implants and the left side received screw-retained prosthesis, while the right side received cement-retained prosthesis (Fig. 6).
Figure 6.
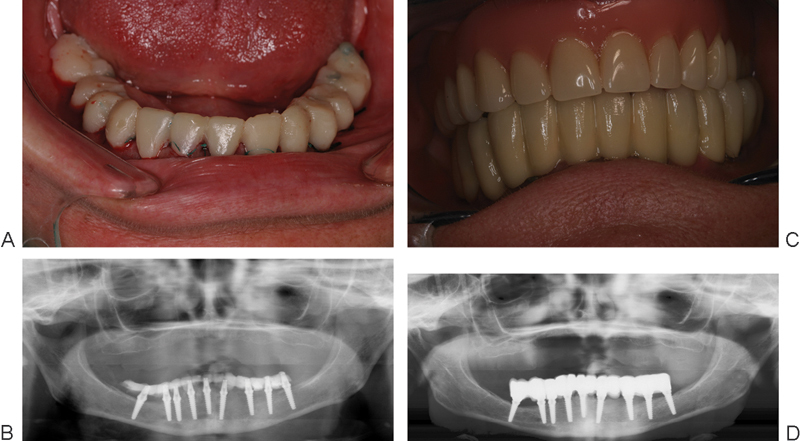
(A and B) Position and angulation of implants, noting the posterior implants where the inferior alveolar nerve was lateralized in both sides. (C) Final ceramometallic fixed prosthesis delivered 3 months postoperatively. (D) Orthopantomogram with the final restoration in place.
The patient after receiving the final prosthesis did not show up for any of her scheduled appointments. She returned after 10 years complaining of looseness of the prosthesis on the right side (cement-retained prosthesis). We removed the prosthesis completely to check for implant mobility and examine the gingival state.
All implants were completely osseointegrated without any signs of mobility. In three implants, one thread was observed supragingival and one implant showed two threads, without affecting the osseointegration. A low-grade gingival inflammation was observed in some parts, which was due to plaque accumulation on the undersurface of the prosthesis. Ultrasonic cleansing of the prosthesis and the implants was performed and the prosthesis was screw-retained prosthesis in place and the right part was cemented (Fig. 7).
Figure 7.
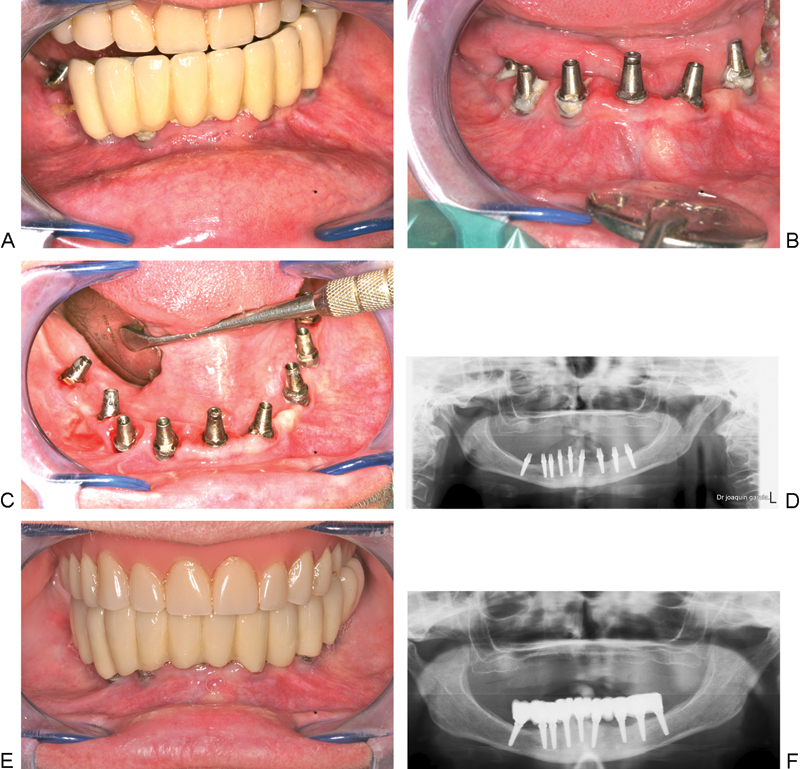
(A and B) Prosthesis and implants after 10 years showing accumulation of plaque and gingival inflammation. (C) Ultrasonic cleaning of implants. (D) 10 years follow-up orthopantomogram showing minimal bone resorption around implants compared with the immediate postoperative radiograph. (E) Screwing back the prosthesis. (F) Orthopantomogram after screwing and cementing back the prosthesis.
Discussion
Implant rehabilitation is used in an increasing number of partially edentulous patients. In most of these patients, the standard method can be used to place the implants with satisfactory results. However, with increasing alveolar resorption, modifications of the standard procedure must be applied. Bone grafting, distraction osteogenesis, the use of shorter implants, and inferior alveolar nerve lateralization (IANL) are some techniques employed to address a lack of bone height.9
The described clinical report offers some alternative suggestions to overcome the difficulties and limitations associated with the prosthetic rehabilitation of severely resorbed posterior mandibles. The osteotomies were performed using piezoelectric surgery. The latest studies present piezosurgery to be feasible in ridge splitting and IANL, because it favors smaller osteotomies and preservation of the neurovascular bundle.10 11 This was confirmed by Sohn et al,12 who applied the piezoelectric technique in various oral surgical situations and concluded that this system achieves deep micrometric bone cuts resulting in precise and easy-to-control osteotomies, in contrast to rotary burs or reciprocation saws. Moreover, they stated that the piezosurgery system can split a very narrow ridge with minimal loss or perforation of bone. In addition, this device reduces patients' fear and stress during surgery performed under local anesthesia as it reduces noise and vibration compared with conventional rotary instruments.
This was followed by expanding the buccal wall engaging the IAN away from the opposite wall atraumatically using threaded bone expanders, thus performing lateralization of the nerve and at the same time expansion of the narrow ridge. This technique allows the implants to pass alongside and not into the nerve canal, thus preserving the integrity of the nerve. Moreover, it allowed placement of longer implants and engaging the inferior mandibular cortex for better primary stability.
Threaded bone expanders were initially used for expansion of narrow ridges with great success because of their atraumatic nature. In addition, the manual technique takes advantage of the natural elasticity of the bone, thus allowing expansion of the ridge and at the same time condensation of trabecular bone, which increases bone density leading to enhanced osseointegration of dental implants.13 This is in accordance with Rambla-Ferrer et al14 who concluded that the bone expansion technique offers the possibility of placing implants in cases of bone atrophy without the need for other more complex treatments. In addition, it improves the quality of bone surrounding the implants and reduces the rehabilitation time.
Moreover, Chiapasco et al,15 studied 392 patients treated with bone splitting/expansion of narrow edentulous ridges and immediate placement of implants. They reported that the survival and success rates of implants placed in expanded ridges are consistent with those related to implants placed in native, nonreconstructed bone and that they seem to withstand the biomechanical demands of loading.
This technique is considered the first technique approaching the IAN through the crest of the alveolar ridge in cases of severely resorbed mandibles which do not accommodate dental implants of sufficient length to allow better stability and were recommended for either bone grafting techniques or lateralization of the IAN. The key factor for the success of this procedure is the administration of infiltration anesthesia which allows the patient to warn the surgeon if the surgical procedure is endangering the IAN, thus preserving its integrity. Also, utilizing the piezosurgery which ensures that no nerve injury takes place even if direct contact of the working tip with the nerve is to be assumed.16 The presented case did not show any immediate nor late postoperative neurosensory disturbance contrary to other conventional IANL studies.17
Currently, it is well established that submerged healing periods of several months are not required to achieve osseointegration, and implants may be placed in a single stage and loaded immediately with a provisional prosthesis, provided the occlusal loads are controlled and the implants are placed with primary stability and a torque of 30 Ncm.18 19 The immediate provisionalization and functional loading have shown high-success rates in different clinical reports and has several advantages compared with a delayed treatment protocol, including fewer surgical interventions, shorter treatment time, and less trauma to the patient.20 Furthermore, immediate implant placement after extraction may preserve alveolar bone height and width, and also provides optimal soft tissue esthetics.21
Therefore, in an attempt to avoid two surgical procedures, one-piece implants were used, where the transmucosal abutment is incorporated as an integral part of the implant thus eliminating the structural weakness built in two-piece implants. One-piece implant is intended for immediate function as well as for immediate placement in fresh extraction sockets.20 21 22
The 10 years follow-up of the patient showed a 100% survival rate of the immediately loaded one-piece implants and minimal bone resorption, which supports the findings of several authors that one-piece implants demonstrated the ability to preserve both peri-implant hard and soft tissues.20 23 24 This was explained by Broggini et al25 that the absence of implant–abutment interface (microgap) at the bone crest in one-piece implants was associated with reduced peri-implant inflammatory cell accumulation and minimal bone loss. The one-piece implant design enables undisturbed healing of the peri-implant soft tissue and avoids disruption of the soft tissue seal when placing the definitive prosthetic restoration.
Conclusions
The immediate nonfunctional loading of one-piece implants in conjunction with IANL using threaded-bone expanders can be employed predictably to patients suffering from severely resorbed posterior mandible as it allows placement of longer implants for greater primary stability, and at the same time expansion of narrow ridges. Also, the long-term observation of this clinical case showed great success.
References
- 1.Albrektsson T, Brånemark P I, Hansson H A, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155–170. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 2.Östman P O, Hellman M, Sennerby L, Wennerberg A. Temporary implant-supported prosthesis for immediate loading according to a chair-side concept: technical note and results from 37 consecutive cases. Clin Implant Dent Relat Res. 2008;10(2):71–77. doi: 10.1111/j.1708-8208.2007.00069.x. [DOI] [PubMed] [Google Scholar]
- 3.Proussaefs P. Vertical alveolar ridge augmentation prior to inferior alveolar nerve repositioning: a patient report. Int J Oral Maxillofac Implants. 2005;20(2):296–301. [PubMed] [Google Scholar]
- 4.Agliardi E, Panigatti S, Clericò M, Villa C, Malò P. Immediate rehabilitation of the edentulous jaws with full fixed prostheses supported by four implants: interim results of a single cohort prospective study. Clin Oral Implants Res. 2010;21(5):459–465. doi: 10.1111/j.1600-0501.2009.01852.x. [DOI] [PubMed] [Google Scholar]
- 5.Kan J Y, Lozada J L, Goodacre C J, Davis W H, Hanisch O. Endosseous implant placement in conjunction with inferior alveolar nerve transposition: an evaluation of neurosensory disturbance. Int J Oral Maxillofac Implants. 1997;12(4):463–471. [PubMed] [Google Scholar]
- 6.Morrison A, Chiarot M, Kirby S. Mental nerve function after inferior alveolar nerve transposition for placement of dental implants. J Can Dent Assoc. 2002;68(1):46–50. [PubMed] [Google Scholar]
- 7.Kim J H, Kim Y K, Yi Y J. et al. Results of immediate loading for implant restoration in partially edentulous patients: a 6-month preliminary prospective study using SinusQuick™ EB implant system. J Adv Prosthodont. 2009;1(3):136–139. doi: 10.4047/jap.2009.1.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andersson L, Kahnberg K E, Pogrel M A. Oxford, United Kingdom: Blackwell Publishing Ltd; 2010. Oral and Maxillofacial Surgery; pp. 367–368. [Google Scholar]
- 9.Luna A H, Passeri L A, de Moraes M, Moreira R W. Endosseous implant placement in conjunction with inferior alveolar nerve transposition: a report of an unusual complication and surgical management. Int J Oral Maxillofac Implants. 2008;23(1):133–136. [PubMed] [Google Scholar]
- 10.Escoda-Francolí J, Rodríguez-Rodríguez A, Berini-Aytés L, Gay-Escoda C. Application of ultrasound in bone surgery: two case reports. Med Oral Patol Oral Cir Bucal. 2010;15(6):e902–e905. [PubMed] [Google Scholar]
- 11.Danza M, Guidi R, Carinci F. Comparison between implants inserted into piezo split and unsplit alveolar crests. J Oral Maxillofac Surg. 2009;67(11):2460–2465. doi: 10.1016/j.joms.2009.04.041. [DOI] [PubMed] [Google Scholar]
- 12.Sohn D S, Ahn M R, Lee W H, Yeo D S, Lim S Y. Piezoelectric osteotomy for intraoral harvesting of bone blocks. Int J Periodontics Restorative Dent. 2007;27(2):127–131. [PubMed] [Google Scholar]
- 13.Siddiqui A A, Sosovicka M. Lateral bone condensing and expansion for placement of endosseous dental implants: a new technique. J Oral Implantol. 2006;32(2):87–94. doi: 10.1563/786.1. [DOI] [PubMed] [Google Scholar]
- 14.Rambla-Ferrer J, Peñarrocha-Diago M, Guarinos-Carbó J. Analysis of the use of expansion osteotomes for the creation of implant beds. Technical contributions and review of the literature. Med Oral Patol Oral Cir Bucal. 2006;11(3):E267–E271. [PubMed] [Google Scholar]
- 15.Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006;17(2) 02:136–159. doi: 10.1111/j.1600-0501.2006.01357.x. [DOI] [PubMed] [Google Scholar]
- 16.Wagner M E, Rana M, Traenkenschuh W, Kokemueller H, Eckardt A M, Gellrich N C. Piezoelectric-assisted removal of a benign fibrous histiocytoma of the mandible: an innovative technique for prevention of dentoalveolar nerve injury. Head Face Med. 2011;7:20. doi: 10.1186/1746-160X-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoshimoto M, König B J, Coelho P G, Allegrini S J, Luiz F F. A light and scanning electron microscopy study of bone healing following inferior alveolar nerve lateralization: an experimental study in rabbits. Int J Oral Maxillofac Implants. 2008;23(3):457–462. [PubMed] [Google Scholar]
- 18.Attard N J, Zarb G A. Immediate and early implant loading protocols: a literature review of clinical studies. J Prosthet Dent. 2005;94(3):242–258. doi: 10.1016/j.prosdent.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 19.Lindeboom J A, Frenken J W, Dubois L, Frank M, Abbink I, Kroon F H. Immediate loading versus immediate provisionalization of maxillary single-tooth replacements: a prospective randomized study with BioComp implants. J Oral Maxillofac Surg. 2006;64(6):936–942. doi: 10.1016/j.joms.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 20.Hahn J A. Clinical and radiographic evaluation of one-piece implants used for immediate function. J Oral Implantol. 2007;33(3):152–155. doi: 10.1563/1548-1336(2007)33[152:CAREOO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Zembić A, Johannesen L H, Schou S. et al. Immediately restored one-piece single-tooth implants with reduced diameter: one-year results of a multi-center study. Clin Oral Implants Res. 2012;23(1):49–54. doi: 10.1111/j.1600-0501.2011.02174.x. [DOI] [PubMed] [Google Scholar]
- 22.Froum S J, Cho S C, Elian N. et al. Survival rate of one-piece dental implants placed with a flapless or flap protocol—a randomized, controlled study: 12-month results. Int J Periodontics Restorative Dent. 2011;31(6):591–601. [PubMed] [Google Scholar]
- 23.Sohn D S, Bae M S, Heo J U, Park J S, Yea S H, Romanos G E. Retrospective multicenter analysis of immediate provisionalization using one-piece narrow-diameter (3.0-mm) implants. Int J Oral Maxillofac Implants. 2011;26(1):163–168. [PubMed] [Google Scholar]
- 24.Finne K, Rompen E, Toljanic J. Clinical evaluation of a prospective multicenter study on 1-piece implants. part 1: marginal bone level evaluation after 1. year of follow-up. Int J Oral Maxillofac Implants. 2007;22(2):226–234. [PubMed] [Google Scholar]
- 25.Broggini N, McManus L M, Hermann J S. et al. Persistent acute inflammation at the implant-abutment interface. J Dent Res. 2003;82(3):232–237. doi: 10.1177/154405910308200316. [DOI] [PubMed] [Google Scholar]


