Abstract
Objectives
To compare the efficacy of three suture materials, i.e., poliglecaprone 25, polyglactin 910, and polyamide, as subcuticular skin stitches in post-cesarean women.
Study Design
This was a randomized clinical trial.
Population
The study was conducted in the department of obstetrics and gynecology of a tertiary institute, LTMMC, Sion, Mumbai, India. Only those women undergoing emergency cesarean section were included.
Methods
The study was conducted in the department of obstetrics and gynecology of a tertiary institute, LTMMC, Sion, Mumbai, India. 90 women undergoing emergency cesarean section were included and divided into three groups. In group 1, poliglecaprone 25 was used as subcuticular skin stitches; in group 2, polyglactin 910 was used as subcuticular skin stitches; and in group 3, polyamide was used as subcuticular skin stitches.
Results
Thirty percentage of the patients in group 3 had discomfort on day 10, while it was only 3.3 % in group 1. In group 1, 6.6 % patients had swelling and indurations, while it was 33.3 % in group 2 on day 4. Wound dehiscence was present in 3.3 % patients in group 1, 26.6 % in group 2, and 6.6 % in group 3. Regarding wound healing, 93.3 % patients had excellent wound healing in group 1, 66.6 % in group 2, and 86.6 % in group 3.
Conclusions
The results were almost similar with poliglecaprone and polyamide, except for discomfort which was present more in patients in group 3.
Keywords: Poliglecaprone, Polyamide, Polyglactin
Introduction
In surgery, the choice of suture material has been largely empirical. One learns the art and craft of surgery from one’s chief, and the tendency is to use the suture material used by him. Thus, the use of suture material has not always been scientific. Egyptian literature of about 1600 B.C. mentioned the use of linen strips coated with an adhesive mixture of honey and flour, thereby creating the original skin closure strips. The development of synthetic absorbable sutures began in 1931 with the production of an absorbable synthetic fiber of polyvinyl alcohol. In the second half of the 60s, it was discovered that polyglycolic acid can be processed into an absorbable suture material with very favorable properties. In 1970 and 1971, the first suture material from polyglycolic acid was introduced into clinical practice. Subsequently, glycolide and lactide were combined in suitable proportion to develop a suture known as polyglactin 910. Later on, this was coated to make it smooth. Further research resulted in the development of PDS (polydioxanone), polyglactin 910 rapide, and poliglecaprone25 [3].
Methods
Study Design
This was a randomized clinical trial. Institutional Ethical Committee and departmental review board approval was taken for this study. Informed consent was obtained before enrollment.
Study Setting and Population
The study was conducted in the department of obstetrics and gynecology of a tertiary institute, LTMMC, Sion, Mumbai, India. Only those women undergoing emergency cesarean section were included.
Inclusion Criteria
The inclusion criteria were as follows: hemoglobin more than 10 gm %, all cesarean sections done on an emergency basis in the same operation theater, the same technique of cesarean section used, and cesarean section done by qualified obstetricians.
Exclusion Criteria
The exclusion criteria were as follows: previous abdominal surgeries, medical illness (Koch’s, bronchial asthma, hypertension, diabetes, hematological disorders), and skin infections.
Study Protocol
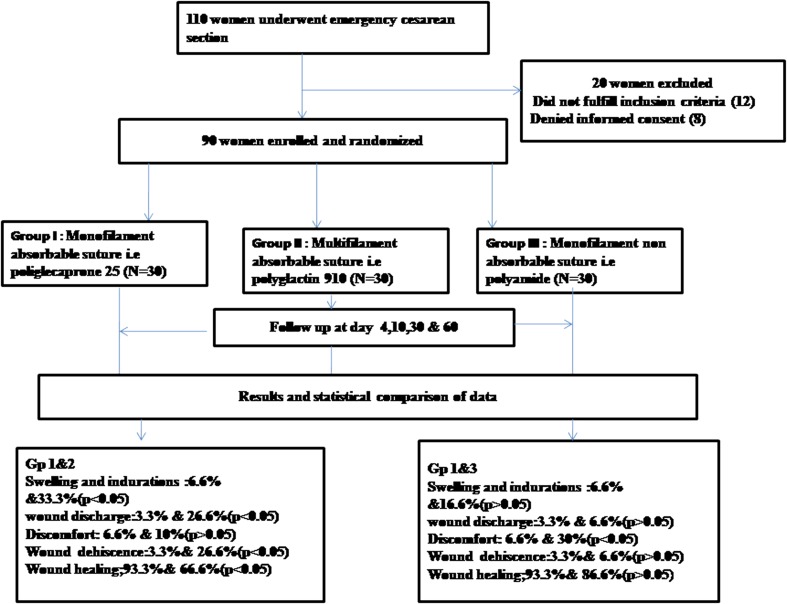
Out of 110 women, 12 women did not fulfill the eligibility criteria. Eight women declined to participate because of long-term follow-up. Once eligibility and exclusion criteria were confirmed and informed consent was obtained, women were randomized by computer-generated randomized numbers and divided into three groups (Fig. 1).
Fig. 1.
Study flow chart
Group 1
Monofilament absorbable suture, i.e., poliglecaprone 25, was used as subcuticular skin stitches.
Group 2
Multifilament absorbable suture, i.e., polyglactin 910, was used as subcuticular skin stitches.
Group 3
Monofilament non-absorbable suture, i.e., polyamide, was used as subcuticular skin stitches.
All women received the same antibiotics and the same analgesics. Effects were studied on day 4, day 10, 1 month, and 2 months post-surgery on the basis of pain and tenderness, swelling and induration, discharge from wound, dehiscence, discomfort, wound healing, and cosmesis. Pain and tenderness were assessed on the basis of the Visual Analog Scale. It has a rating of no pain at one end and unbearable pain at other end. The rest of the parameters were assessed as follows: swelling and induration assessed in the form of erythema and edema; discharge from the wound as serous, serosanguinous, or purulent; wound dehiscence as superficial or deep; discomfort by a different questionnaire; and wound healing and cosmesis by the Modified Hollender Cosmesis Scale [1, 2] which was composed of six items: step off borders, edge inversion, contour irregularities, excess inflammation, wound margin separation, and overall appearance.
Results
Out of 110 women, 12 women did not fulfill the eligibility criteria. Eight women declined to participate because of long-term follow-up. Of the 90 women enrolled, 30 were randomized to group 1, 30 to group 2, and 30 to group 3.
Statistical Analysis
Data were entered in Microsoft Excel and were analyzed using SPSS 11.0 for Windows and Epi Info for Windows.
The statistical test employed was χ2. Where the expected cell count in any one cell was less than five, the P value was taken based on Fischer’s exact test. Two-tailed P values were considered for all the tests.
According to this, P > 0.05—not significant; P < 0.05—significant.
The three groups were similar in age, weight, type of surgery, and type of skin incision. As shown in Tables 1, 2, and 3, there was no difference with respect to pain and tenderness on day 4, 10, and 30. There is no statistically significant difference between the women of group 1 and 2 with respect to the presence of discomfort at suture site as assessed on day 4 and 10, but there is a significant difference between group 1 and 3 on day 4 and 10 (6.6 and 3.3 % in group 1 on day 4 and 10, respectively; 30 and 26.6 % in group 3 on day 4 and 10, respectively). There is no statistically significant difference between patients of group 1 and 3 with respect to swelling and indurations as assessed on day 4 (6.6 % in group 1, 16.6 % in group 3) and 10 (6.6 % in group 1, 13.3 % in group 3), but there is a significant difference between group 1 and 2 on day 4 (6.6 % in group 1, 33.3 % in group 2) and 10 (6.6 % in group 1, 26.6 % in group 2). There is no statistically significant difference between patients of group 1 and 3 with respect to wound discharge as assessed on day 4 (3.3 % in group 1, 6.6 % in group 3) and 10 (6.6 % in group 1, 13.3 % in group 3), but there is a significant difference between group 1 and 2 on day 4 (3.3 % in group 1, 26.6 % in group 2) and 10 (6.6 % in group 1, 30 % in group 2). On day 30, no statistical test was applicable as the number of patients in all three groups was zero. There is no difference between group 1 and 2 on day 4 according to wound dehiscence, but a significant difference on day 10 (3.3 and 26.6 % in group 1 and 2, respectively); there is no difference between group 1 and 3 on day 4 and 10 as shown in the Tables. There is statistically significant difference between group 1 and 2 (93.3 and 66.6 %, respectively) with respect to the status of the wound healing at the suture line at one and 2 months post-surgery, but there is an insignificant difference in group 1 and 3 (93.3 and 86.6 %, respectively) as shown in Table 4.
Table 1.
Day 4
| Parameters | Group I (n = 30) (%) | Group 2 (n = 30) (%) | Group 3 (n = 30) (%) | P value | |
|---|---|---|---|---|---|
| a) Pain and tenderness | 11 (36.6) | 11 (36.6) | 9 (30) | Group 1 and 2 | No difference |
| Group 1 and 3 | P = 0.583 (>0.05) | ||||
| b) Discomfort | 2 (6.6) | 3 (10) | 9 (30) | Group 1 and 2 | P = 1 (>0.05) |
| Group 1 and 3 | P = 0.019 (<0.05) | ||||
| c) Swelling and induration | 2 (6.6) | 10 (33.3) | 5 (16.6) | Group 1 and 2 | P = 0.009 (<0.05) |
| Group 1 and 3 | P = 0.423 (>0.05) | ||||
| d) Wound discharge | 1 (3.3) | 8 (26.6) | 2 (6.6) | Group 1 and 2 | P = 0.025 (<0.05) |
| Group 1 and 3 | P = 1 (>0.05) | ||||
| e) Wound dehiscence | 3 (10) | 6 (20) | 3 (10) | Group 1 and 2 | P = 0.471 (>0.05) |
| Group 1 and 3 | No difference | ||||
Table 2.
Day 10
| Parameters | Group I (n = 30) (%) | Group II (n = 30) (%) | Group III (n = 30) (%) | P value | |
|---|---|---|---|---|---|
| 1) Pain and Tenderness | 6 (20) | 6 (20) | 8 (26.6) | Group 1 and 2 | No difference |
| Group 1 and 3 | P = 0.541 (>0.05) | ||||
| 2) Discomfort | 1 (3.3) | 6 (20) | 8 (26.6) | Group 1 and 2 | P = 0.102 (>0.05) |
| Group 1 and 3 | P = 0.025 (<0.05) | ||||
| 3) Swelling and Induration | 2 (6.6) | 8 (26.6) | 4 (13.3) | Group 1 and 2 | P = 0.037 (<0.05) |
| Group 1 and 3 | P = 0.670 (>0.05) | ||||
| 4) Wound discharge | 2 (6.6) | 9 (30) | 4 (13.3) | Group 1 and 2 | P = 0.019 (<0.05) |
| Group 1 and 3 | P = 0.670 (>0.05) | ||||
| 5) Wound dehiscence | 1 (3.3) | 8 (26.6) | 2 (6.6) | Group 1 and 2 | P = 0.025 (<0.05) |
| Group 1 and 3 | P = 1 (>0.05) | ||||
Table 3.
Day 30
| Parameters | Group I (n = 30) (%) | Group II (n = 30) (%) | Group III (n = 30) (%) | P value | |
|---|---|---|---|---|---|
| 1) Pain and Tenderness | 1 (3.3) | 1 (3.3) | 2 (6.6) | Group 1 and II | No difference |
| P > 0.05 | |||||
| 2) Discomfort | 0 (0) | 1 (3.3) | 4 (13.3) | Test invalid, as no patient in group 1 | |
| 3) Swelling and Induration | 0 (0) | 1 (3.3) | 1 (3.3) | Test invalid | |
| 4) Wound discharge | 0 (0) | 0 (0) | 0 (0) | No difference | |
| 5) Wound dehiscence | 0 (0) | 4 (13.3) | 2 (6.6) | Test invalid | |
Table 4.
Distribution of patients with respect to status of wound healing at suture line at 1 and 2 months post-surgery
| Group (n = 30) | Excellent wound healing 6/6 | 1 month | 2 month | |
|---|---|---|---|---|
| 1 month (%) | 2 month (%) | |||
| Group I | 26 (86.6) | 28 (93.3) | Group 1 and 2 | Group 1 and 2 |
| P = 0.019 (<0.05) | P = 0.009 (<0.05) | |||
| Group II | 18 (60) | 20 (66.6) | Group 1 and 3 | Group 1 and 3 |
| Group III | 22 (73.3) | 26 (86.6) | P = 0.196 (>0.05) | P = 0.670 (>0.05) |
Discussion
The most pliable monofilament absorbable suture poliglecaprone 25 has excellent handling properties; it has a very smooth surface and passes through tissue with greater ease than catgut or braided absorbable sutures. Finally, poliglecaprone 25 has equivalent knot security compared to the other major absorbable sutures such as catgut, coated polyglactin 910, and PDS II.
To our knowledge, this is the first study that has analyzed cosmetic outcomes and complications of skin closure of cesarean section patients using absorbable versus non-absorbable and monofilament versus polyfilament sutures. There seems to be no universal agreement among authorities in choosing the ideal type of suture material for wound repair. The studies attempted to show that there is no appreciable difference with respect to cosmetic outcome and wound complications in operative wounds closed with absorbable suture material, compared with those closed with non-absorbable suture material in cosmetic surgery [3–6]. But, repair with absorbable sutures is clearly advantageous in that any further emotional and physical trauma is avoided during subsequent removal. Sheety et al. [7] conducted a 5-year retrospective review of 102 adult patients with hand lacerations and compared the quality of scar formation in scars repaired with 5–0 vicryl versus those repaired with 5–0 nylon. They recommended absorbable suture material as an acceptable alternative to non-absorbable sutures in the repair of hand lacerations. Breed et al. [8] compared the possible influence of two absorbable suture materials on the formation of scar tissue in women undergoing reduction mammoplasty. The scars were examined after periods of 2 weeks, 3 months, and 1 year. The monofilament poliglecaprone 25 produced significantly narrower scars than polyglactin 910. Osther et al. [9] in a randomized control trial compared polyglycolic acid and monofilament polyglyconate sutures for abdominal fascial closure after laparotomy in patients with suspected impaired wound healing. Wound infection demanding surgical intervention was found in 7 % of patients with polyglyconate and 16 % with polyglycolic acid sutures (P 0.04). In our study, the number of patients having wound discharge and induration was significantly more (P < 0.05) in group 2 where polyglactin suture was used as compared to poliglecaprone and polyamide. Parell and Becker [10] compared absorbable with non-absorbable sutures in the closure of facial skin wounds and found no significant difference between the areas closed with prolene and those closed with vicryl rapide. Our study suggests that the risk of wound dehiscence was more where polyglactin suture was used in comparison to poliglecaprone, as it is a multifilament suture and has more chances of infection. When wound healing was reviewed 2 months after surgery, the number of cases showing excellent healing was more in group 1 (P < 0.05) where poliglecaprone suture was used. The results were almost similar with polyamide.
Conclusions
Poliglecaprone absorbable suture is associated with significantly less discomfort at the suture site (P < 0.05) as compared to non-absorbable polyamide suture.
The incidence of swelling and induration is significantly (P < 0.05) less with poliglecaprone and polyamide, both monofilament sutures as compared to the multifilament polyglactin suture. Wound discharge is significantly (P < 0.05) less with poliglecaprone and polyamide as compared to multifilament polyglactin suture. Wound dehiscence and requirement of resuturing are significantly (P < 0.05) less with poliglecaprone as compared to the polyglactin suture. The polyamide suture has shown results almost similar to poliglecaprone.
Wound healing is excellent with poliglecaprone and polyamide.
Acknowledgments
None.
Conflict of interest
None.
Ethical Standards
The study protocol was approved by Institutional Ethics Committee of our institute LTMMC and LTMGH staff and research society Bombay public trust act. Reg. no. F/1669 of 21-9-1968. Date of approval :21.01.08. Ref: PS/IEC-HR/DISS/04/(01/08).
Contributor Information
Urvashi Vats, Phone: +9559493008, Email: urvashision@rediffmail.com.
Narayan Pandit Suchitra, Phone: +9820416474, Email: suchipan56@rediffmail.com.
References
- 1.Hollander JE, Singer AJ, Valentine S, et al. Wound registry: development and validation. Ann Emerg Med. 1995;25:475–485. doi: 10.1016/S0196-0644(95)70183-4. [DOI] [PubMed] [Google Scholar]
- 2.Quinn JV, Drzwiecki AE, Stiell IG, et al. ElmslieTJ. appearance scales to measure cosmetic outcomes of healed lacerations. Am J Emerg Med. 1995;13:229–231. doi: 10.1016/0735-6757(95)90100-0. [DOI] [PubMed] [Google Scholar]
- 3.LaBagnara J., Jr A review of absorbable suture material in head and neck surgery and introduction of monocryl: a new absorbable suture. Ear Nose Throat J. 1995;74:409–415. [PubMed] [Google Scholar]
- 4.Gys T, Hubens A. A prospective comparative clinical study between monofilament absorbable and nonabsorbable sutures for abdominal wall closure. Acta Chir Belg. 1989;89:265–270. [PubMed] [Google Scholar]
- 5.Guyuron B, Vaugahn C. A comparision of absorbable and non-absorbable suture materials for skin repair. Plast Reconstr Surg. 1992;89:234–236. doi: 10.1097/00006534-199202000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Canarelli JP, Ricard J, Collet LM, et al. Use of fast absorbable material for skin closure in young children. Int Surg. 1988;73:151–152. [PubMed] [Google Scholar]
- 7.Sheety PC, Dicksheet S, Scalea TM. Emergency department repair of hand lacerations using absorbable vicryl sutures. J Emerg Med. 1997;15:673–674. doi: 10.1016/S0736-4679(97)00147-9. [DOI] [PubMed] [Google Scholar]
- 8.Breed CM, Van der Biezen JJ, Marck KW, et al. Comparision of two absorbable suture materials on the formation of scar tissue, in patients who had undergone reduction mammoplasty. Euro J Plast surg. 1998;22:251–254. doi: 10.1007/s002380050198. [DOI] [Google Scholar]
- 9.Osther PJ, Gjode P, Mortensen PB, et al. Randomised comparision of polyglyconate sutures for abdominal fascial closure after laparotomy in patients with suspected impaired wound healing. Br J Surg. 1995;82:1080–1082. doi: 10.1002/bjs.1800820824. [DOI] [PubMed] [Google Scholar]
- 10.Parell GJ, Becker GD. Comparision of absorbable with nonabsorbable sutures in closure of facial skin wounds. Arch Facial Plast Surg. 2003;5:488–490. doi: 10.1001/archfaci.5.6.488. [DOI] [PubMed] [Google Scholar]