Introduction
Uterine leiomyoma is the most common tumor found in women of reproductive age group. The clinical symptoms and severity usually depend upon the size, position, and number of fibroids present. The incidence of sarcomas in patients operated for leiomyomas is 0.23 % [1], with leiomyosarcoma being rarer estimated to be between 0.13 and 0.29 % [1, 2]. Uterine leiomyosarcoma comprises ~1 % of all uterine malignancies—average age of occurrence being 40–50 years. Metastasis from leiomyosarcoma of uterus occurs mainly to lung, liver, brain, kidney, and bones. Secondaries to ovary from uterine leiomyosarcomas are, however, very rare (3.5 %).
Case History
A 65-year-old female presented to our hospital with the complaints of vaginal bleeding since 7 months along with pain in abdomen and lump in abdomen since 3 months. Her general condition was poor. Pallor was present. On per abdominal examination, a lump of size 15 × 5 cm was felt in right hypochondrium. Ultrasonography of abdomen revealed multiple uterine fibroids with a pelvic mass. Uterus was seen separate from mass. Right-sided ovary was not seen separately; however, left ovary was visualized normally. The clinical diagnosis was ovarian sarcoma. Total abdominal hysterectomy with bilateral salpingo-oophorectomy was done. However, patient was lost for follow up. On gross examination, uterus measured 10 × 13 × 7 cm. Externally, it was lobulated. Right ovary was enlarged measuring 11 × 7 × 4 cm. Externally, it was multinodular. On cut surface, uterus showed multiple, well-circumscribed tumor masses with gray white, whorled appearance (Fig. 1). Left ovary was unremarkable. On microscopic examination, leiomyomas presented as bland, spindly cells arranged in fascicles and bundles with minimal mitotic activity. Part of the leiomyoma near the isthmus showed features of high grade leiomyosarcoma (Fig. 1) with ovoid spindle shaped cells having hyperchromatic, pleomorphic nuclei with prominent nucleoli. Mitosis (10–12) per high field (phf) was seen with areas of necrosis. Ovarian tumor on cut section had a similar appearance as that of uterine leiomyomas (Fig. 1) with similar histomorphology (Fig. 1) as that of malignant counterpart of leiomyoma. Immunohistochemistry of leiomyosarcoma revealed strong immunoreactivity for SMA and low for Ki-67.
Fig. 1.
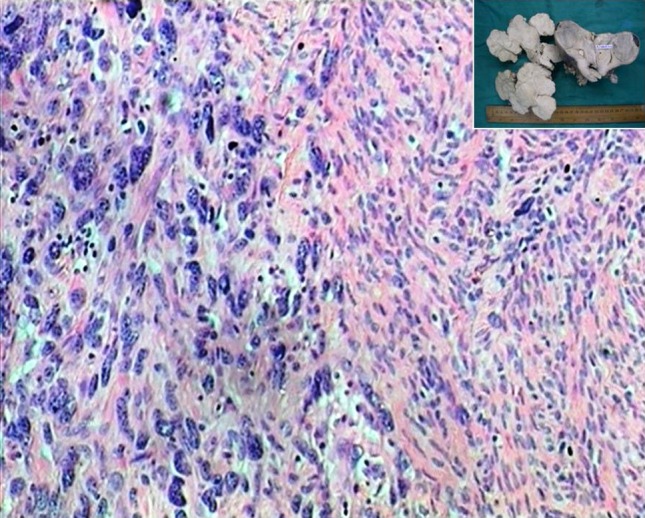
Microphotograph showing transition from benign leiomyoma to leiomyosarcoma. (H&E ×20). Inset Cut surface of uterus and ovary showed multiple, well-circumscribed, grayish-white tumor masses with an whorled appearance
Discussion
Leiomyomas of the uterus are the commonest benign tumors of the female genital tract. They affect 20–30 % of women older than 35 years. Leiomyomas can undergo various degenerative changes including malignant degeneration. In a 10-year study, the US National Cancer Institute’s Surveillance Epidemiology and End Results (SEER) database reported 2098 women with uterine sarcomas with an average age of 63 years [3]; however, a review of the literature found a mean age of 36 years in women who had undergone myomectomy [1]. Cases of uterine leiomyosarcoma arising in leiomyoma have been reported, suggesting that leiomyosarcomas may arise from preexisting leiomyomas [2]. Leibsohn et al. [2] reported that out of 1,429 patients who underwent hysterectomies for benign leiomyomas, leiomyosarcoma was histopathologically diagnosed in seven patients (0.5 %). Ours was a similar case. Uterine leiomyosarcoma is a rare gynecologic malignancy, comprising about 1 % of all uterine malignancies and 25–36 % of uterine sarcomas. The most frequent symptoms of uterine leiomyosarcoma are abnormal vaginal bleeding and palpable mass followed by weight loss and weakness. Our patient also presented with similar symptoms. Unusual microscopic features of ovarian tumor prompted closer inspection of gross and microscopy of all uterine leiomyomas. This led to detection of malignant transformation of one of the leiomyoma with metastasis to the right ovary. In a study done by Leitao et al. [4], percentage of ovarian metastasis secondary to uterine leiomyosarcoma was 5.4 %. In such cases, an important consideration of frozen section would be useful to give the diagnosis as well as deciding the staging of the tumor and hence the extent of the surgery. However, the incidence of ovarian metastasis in a case of uterine leiomyosarcoma in India is not exactly documented.
Conclusion
Leiomyomas with any deviant feature should be subjected to microscopy, so that their atypical features are not missed. An important consideration of frozen section is important to be kept in mind, as it is a very useful aid to decide the extent of surgical management. For any unusual tumor in the ovary, a metastatic tumor should be suspected, and search for the primary should be made in all known sites including uterus (though rarer).
References
- 1.Parker WH, Fu YS, Berek JS. Uterine sarcoma in patients operated on for presumed leiomyoma and rapidly growing leiomyoma. Obstet Gynecol. 1994;83:414–418. [PubMed] [Google Scholar]
- 2.Leibsohn S, d’Ablaing G, Mishell DR, Jr, et al. Leiomyosarcoma in a series of hysterectomies performed for presumed uterine leiomyomas. Am J Obst Gynecol. 1990;162:968–974. doi: 10.1016/0002-9378(90)91298-Q. [DOI] [PubMed] [Google Scholar]
- 3.Brooks SE, Zhan M, Cote T, et al. Surveillance, epidemiology, and end results analysis of 2677 cases of uterine sarcoma 1989–1999. Gynecol Oncol. 2004;93:204–208. doi: 10.1016/j.ygyno.2003.12.029. [DOI] [PubMed] [Google Scholar]
- 4.Leitao MM, Sonoda Y, Brennan MF, et al. Incidence of lymph node and ovarian metastasis in leiomyosarcoma. Gynecol oncol. 2003;91:209–212. doi: 10.1016/S0090-8258(03)00478-5. [DOI] [PubMed] [Google Scholar]


