Abstract
An elderly man presented to the emergency department following a motorbike accident. He had sustained chest injuries and a grade 1 splenic laceration. He had a moderate amount of free fluid and some omental standing on trauma CT, which was concerning for occult malignancy. A follow-up CT 4 weeks later showed a marked progression of the ascites and omental stranding. Ascitic tap was negative for malignancy. Tumour markers were normal. The patient developed a proximal small bowel obstruction which appeared to be related to this omental caking in the left upper quadrant on CT. Gastroduodenoscopy did not display any mass lesion. There was an external compression of the duodenum which could not be traversed with the scope. Laparoscopy showed a widespread peritoneal carcinomatosis. Biopsies of the omentum and peritoneum confirmed metastatic signet ring cell carcinoma (cytokeratin 7 and cytokeratin 20 positive). The patient was palliated but died 2 weeks after his diagnosis.
Background
An elderly man presented to the emergency department following a motorbike accident. He had sustained chest injuries and a grade 1 splenic laceration. He had a moderate amount of free fluid and some omental standing on trauma CT, which was concerning for occult malignancy.
A follow-up CT 4 weeks later showed a marked progression of the ascites and omental stranding. Ascitic tap was negative for malignancy. Tumour markers were normal. The patient developed a proximal small bowel obstruction which appeared to be related to this omental caking in the left upper quadrant on CT. Gastroduodenoscopy did not display any mass lesion. There was an external compression of the duodenum which could not be traversed with the scope.
Laparoscopy showed a widespread peritoneal carcinomatosis. Biopsies of the omentum and peritoneum confirmed metastatic signet ring cell carcinoma (cytokeratin 7 (CK7) and cytokeratin 20 (CK 20) positive). The patient was palliated but died 2 weeks after his diagnosis.
This case demonstrates an incidental finding of peritoneal carcinomatosis caused by metastatic signet ring cell carcinoma. The definitive diagnosis was delayed because the patient presented in the setting of trauma, which made interpretation of CT imaging unclear.
This case highlights the aggressive nature of signet ring cell carcinoma and the fact that prompt and focused investigations are required to establish the diagnosis in a timely fashion.
Case presentation
We present the case of a 78-year-old man who presented to the emergency department following a motorbike accident. He was thrown from his motorbike while travelling at approximately 70 km/h and sustained multiple left-sided rib fractures with flail segments and a left-sided haemopneumothorax. There was no clinical evidence of intra-abdominal injury.
Investigations
Initial trauma CT demonstrated a grade 1 splenic laceration, a moderate amount of free fluid and omental stranding. This presumed omental caking with the presence of ascites was thought to be an incidental finding of an occult malignancy (figure 1). A plan was made to repeat the CT scan in 4–6 weeks. The patient was presented to the intensive care unit with thoracic injuries, and was discharged after 7 days with a plan for an outpatient progress CT scan.
Figure 1.
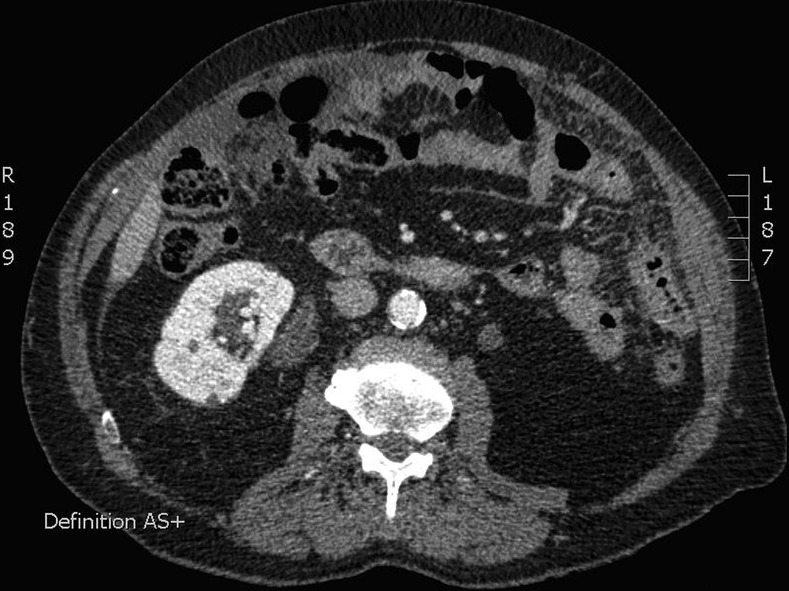
Axial CT displaying omental stranding in the upper abdomen.
The patient re-presented to the emergency department 4 weeks after discharge with abdominal pain and increasing abdominal girth. A CT of the abdomen displayed a marked increase in the previously noted ascites and progression of the omental stranding (figure 2). A diagnostic ascitic tap was performed, which showed mesothelial cells with some reactive charges, but no malignant cells. Blood investigations were all essentially normal, including tissue autoantibody, hepatitis and autoimmune screens. Tumour markers were also normal, including carcinoembryonic antigen, carbohydrate antigen 19.9 and α fetoprotein. Whole body CT failed to display any additional findings to those already mentioned. There was no obvious lymphadenopathy or mass lesions identified. The patient improved clinically and a colonoscopy and gastroduodenoscopy was arranged for the patient as outpatient procedures.
Figure 2.

Axial CT 4 weeks later displaying a marked increase in the volume of ascites.
Five days after discharge, the patient came back to the hospital for outpatient gastroduodenoscopy and colonoscopy, but collapsed in the hospital car park. He was admitted, and found to be hyperkalaemic and in acute renal failure. His ascites had progressed. Another ascitic tap failed to provide any further information about the aetiology of the ascites. The patient developed nausea, vomiting and abdominal pain which was investigated with a CT abdomen. This showed a small bowel obstruction at the level of the duodenojejunal flexure. A push enteroscopy showed extrinsic compression of the duodenum at its distal end. A number of attempts to traverse this stricture failed. Endoscopic examination of the stomach and remainder of the duodenum was normal. The patient was placed on total parenteral nutrition. Colonoscopy was not attempted due to the inability to adequately prepare the bowel due to proximal bowel obstruction. Following discussion that a percutaneous biopsy of the omentum could not be carried out safely, a diagnostic laparoscopy was performed. This displayed serous and gelatinous ascites. There was fibrous matting of the small and large bowel, with clumping of bowel loops in the left upper quadrant, which accounted from the proximal small bowel obstruction. The omentum was grossly thickened and there were multiple white plaques throughout the peritoneum (figure 3). Biopsies of the peritoneum and omentum were taken. It was not possible to relieve or bypass the small bowel obstruction due to the extent of the small bowel adhesions.
Figure 3.
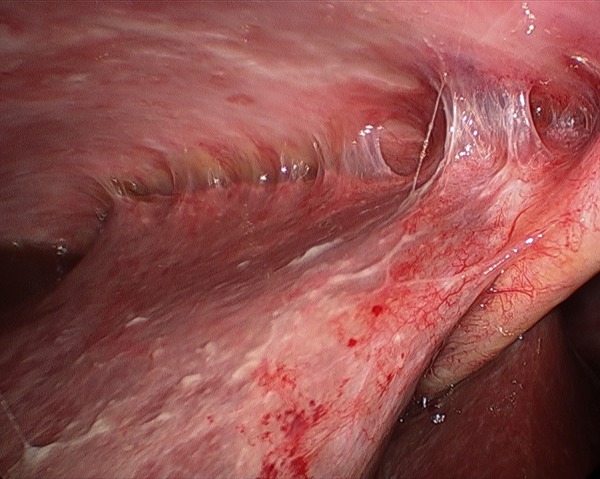
Laparoscopic image showing malignant peritoneal carcinomatosis over the liver.
Differential diagnosis
Histology from the peritoneal biopsies confirmed metastatic signet ring cell carcinoma (CK 7 positive and CK 20 positive). A further attempt at endoscopic placement of a jejunal feeding tube beyond the level of obstruction failed. Multidisciplinary discussion concluded that the patient was for palliation only. He died 2 weeks later. In total, the patient survived 3 months since initial presentation.
Treatment
Palliation only.
Discussion
Signet ring cell carcinoma is a poorly differentiated adenocarcinoma which is characterised by the histological appearance of signet ring cells.1 These malignancies are rare. They originate primarily from a number of tissues, including stomach, colon, pancreas, gallbladder, breast, thyroid, prostate and bladder.2–5 Signet ring cell carcinoma poses diagnostic and treatment difficulties as they tend to be very aggressive and present at an advanced stage.6 The majority of patients develop peritoneal carcinomatosis early in the course of the disease.7 Surgical and chemotherapeutic treatments have been found to have limited efficacy, and overall survival rates remain dismal.8
This case highlights a late, incidental presentation of this aggressive disease, where a primary lesion was not identified. It highlights the rapid progression of signet ring cell carcinoma and the requirement for prompt focused investigations to establish its diagnosis and aid to expedite treatment or, indeed, supportive strategies.
Learning points.
Signet ring cell carcinoma is a rare but aggressive malignancy.
A large proportion of these cancers present late, and most will have peritoneal carcinomatosis at presentation. The overall survival rate is dismal.
Prompt and focused investigations are required for diagnosis, which normally involves colonoscopy and gastroduodenoscopy.
Findings suspicious for peritoneal carcinomatosis or omental caking on CT require prompt investigation.
Acknowledgments
Dr David Parker, Consultant General Surgeon, Gold Coast University Hospital, QLD, Australia.
Footnotes
Contributors: DOK was responsible for drafting the case report, planning and collecting data, and is the guarantor. KD, RN, SC were responsible for planning and collecting data.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.El-Zimaity H, Itani K, Graham D. Early diagnosis of signet ring cell carcinoma of the stomach: role of the Genta stain. J Clin Pathol 1997;50: 867–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warner J, Nakamura L, Pacelli A, et al. Primary signet ring cell carcinoma of the prostate. Mayo Clin Proc 2010;85:1130–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim J, Park S, Park M, et al. Early-stage primary signet ring cell carcinoma of the colon. World J Gastroenterol 2013;19:3895–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandhu J, Dubey V, Makkar M, et al. Pure primary signet ring cell carcinoma breast: a rare cytological diagnosis. J Cytol 2013;30:204–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwon W-A, Oh T, Ahn S, et al. Primary signet ring cell carcinoma of the prostate. Can Urol Assoc J 2013;7:768–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sim H-L, Tan K-Y, Poon P-L, et al. Primary rectal signet ring cell carcinoma with peritoneal dissemination and gastric secondaries. World J Gastroenterol 2008;14:2118–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chua TC, Pelz JO, Kerscher A, et al. Critical analysis of 33 patients with peritoneal carcinomatosis secondary to colorectal and appendiceal signet ring cell carcinoma. Ann Surg Onco l 2009;16:2765–70 [DOI] [PubMed] [Google Scholar]
- 8.Lieu C, Lambert L, Wolff R, et al. Systemic chemotherapy and surgical cytoreduction for poorly differentiated and signet ring cell adenocarcinomas of the appendix. Ann Oncol 2012;23:652–8 [DOI] [PMC free article] [PubMed] [Google Scholar]


