Abstract
Background:
Major Depressive Disorder (MDD) is a heterogeneous disease. More homogeneous psycho(patho)logical dimensions would facilitate MDD research as well as clinical practice. The first aim of this study was to find potential dimensions within a broad psychopathological assessment in depressed patients. Secondly, we aimed at examining how these dimensions predicted course in MDD.
Methods:
Ten psychopathological variables were assessed in 75 MDD inpatients. Factor and regression analyses assessed putative relations between psychopathological factors and depression severity and outcome after 8 weeks of treatment.
Results:
A 3 factor model (eigenvalue: 54.4%) was found, representing a psychomotor change, anhedonia and negative affect factor. Anhedonia and negative affect predicted depression severity (R2=0.37, F=20.86, p<0.0001). Anhedonia predicted non-response (OR 6.00, CI 1.46–24.59) and both negative affect (OR 5.69, CI 1.19–27.20) and anhedonia predicted non-remission (OR 9.28, CI 1.85–46.51).
Limitations:
The sample size of the study was relatively modest, limiting the number of variables included in the analysis.
Conclusions:
Results confirm that psychomotor change, anhedonia and negative affect are key MDD dimensions, two of which are related to treatment outcome.
Keywords: Major depressive disorder, factor analysis, anhedonia, stress, outcome
1. INTRODUCTION
Current neurobiological and behavioral research on the psychopathology of Major depressive disorder (MDD), as well as common clinical practice, increasingly considers MDD as a multidimensional and heterogeneous concept (Hasler et al., 2004; Zimmerman, 2009). Affected individuals are associated with a wide variety of risk factors, symptoms and other clinically relevant variables, such as demographic characteristics, comorbidity, personality traits and characteristics of depressive episodes (Kendler, 1999). A data-driven approach to identify meaningful components or latent dimensions within a heterogeneous diagnostic construct is factor analysis (Comrey at al., 1978). In the past, several studies have used factor analytic strategies to identify subdimensions of MDD, based on clinical rating scales for depression and other symptom measures reflecting DSM-IV criteria (e.g., Carragher et al., 2009; Cassano et al., 2009; Harald and Gordon, 2012). The most commonly identified factors in MDD are a depression severity factor and a somatic factor (Shafer, 2006). A few studies report a positive affect factor and a psychomotor factor (Schrijvers et al., 2008).
However, most of the studies using factor analysis in MDD research have important limitations. First, the proposed factors have been largely limited to clinical symptoms without attempts to correlate the factors with variables across different units of analysis, such as etiological characteristics of MDD. Classifying psychopathology based on dimensions of observable behavior, risk factors as well as psychobiological measures would define dimensions on their basic functions and cutting across categorical disorders as traditionally defined. It seems clear that clusters of self-reported symptoms is constraining advances in understanding the pathophysiology of mental illnesses and in addition hampers the development of better treatments (Insel and Charney, 2003). Second, the clinical relevance in terms of the influence of these factors on outcome in MDD patients has often not been examined in detail. Identifying reliable predictors of outcome in research may allow for the development of novel and more specified interventions (Chen et al., 2000; Insel et al., 2010).
The primary effort of this study was to discover basic dimensions of functioning within MDD, by including variables across different units of analysis, from core MDD symptoms to potentially important underlying risk factors and behaviors. In addition, we evaluated the clinical relevance of these dimensions by investigating their relation to depression severity and their ability to predicting outcome.
To achieve our aims, we conducted a factor analysis based on a broad range of psychopathological characteristics, assessed in 75 depressed inpatients. Ten clinical symptoms of MDD, as well as additional features representing underlying psychopathological vulnerability and environmental factors involved in the development of MDD were included in the factor analysis. In an additional analysis, potential latent dimensions were evaluated with regard to their relationship to outcome after 8 weeks of treatment using logistic regression models. Outcome was operationalized using response and remission rates.
2. MATERIALS AND METHODES
2.1. Participants
Eighty-two depressed patients participated in this study. All patients were hospitalized at the University Psychiatric Center of the University of Leuven, Belgium. The Structured Clinical Interview for DSM-IV-TR (SCID-I) (Spitzer et al., 1992) was used to make DSM-IV diagnoses of MDD. Patients with other mood spectrum disorders, addiction, psychotic disorders or any other unstable medical condition were excluded. All patients received pharmacological and/or psychotherapy treatment, as clinically appropriate. All participants signed an informed consent and the local ethics committee approved the study.
2.2. Design and procedures
This investigation was part of a larger longitudinal study, examining potential endophenotype in MDD, which provided the sample used to test the current hypothesis. Endophenotype research attempts to define an heterogeneous phenotype of a disease with more homogeneous subdimensions based on psychopathology, biology and genes (Hasler et al., 2004). In the longitudinal study, signs and symptoms were chosen based on their specificity and/or clinical and biological plausibility with regards to two potential endophenotypes recently described in MDD: anhedonia and increased stress sensitivity. These are potentially the most biologically and clinically meaningful endophenotypes that can be assessed quantitatively (Vrieze and Claes, 2009).
The selection of instruments used in this protocol was chosen to capture key symptom patterns, risk factors and etiological underpinnings of MDD. We limited the number of variables to 10 due to our relative small sample size. All patients were evaluated within the first week of admission. After 8 weeks, a follow-up appointment was made and response and remission measurements were taken. All measures and ratings were completed by a psychiatrist (E.V.) or trained psychiatric research nurse.
2.3. Data collection and reduction
2.3.1. Clinical assessments and measures
Key emotional symptoms of MDD were measured using the Positive and Negative Affect Scale (PANAS) (Davidson 2003; Watson et al., 1995). This 20-item self-rating scale rates negative affect (NA), which represents features such as distress and anxiety, and positive affect (PA), which entails features such as feeling happy, energetic and alert (Watson et al., 1988). Since anhedonia is a specific, core feature and potential endophenotype of MDD (Hasler et al., 2004), subjects also completed the Snaith-Hamilton Pleasure Scale (SHAPS) (Snaith et al., 1995). The SHAPS is a 14-item questionnaire probing participants’ hedonic capacity in a variety of situations (Franken et al., 2007). The CORE Assessment of Psychomotor Change (CORE) was included to assess psychomotor changes (Parker et al., 1994). The CORE scale is specifically designed to differentiate between melancholic and non-melancholic depression and rates 18 observable features in 3 dimensions: non-interactiveness (e.g., inattentiveness, poverty of associations, impaired spontaneity of talk), retardation (e.g., facial immobility, postural slump, delay in verbal response, slowed speech) and agitation (e.g., facial apprehension and agitation, stereotype movements). Before utilizing the CORE-scale, raters were trained by studying the information video and role-playing. Participants completed the NEO-Five Factor Inventory (NEO-FFI) to obtain a measure of the personality dimension neuroticism (Costa and McCrae., 1992), which is considered the most important predisposing personality dimension for MDD (Kendler et al., 2004). The NEO-FFI measures neuroticism by exploring personality aspects of anxiety, irritation, depression, shame, impulsivity, and vulnerability. Only the neurotic subscale of the NEO-FFI was used in this study. The semi-structured trauma questionnaire (STI) was included to assess early life stress (ELS) (Draijer and Langeland, 1999). Environmental factors play an important role in MDD and it is generally assumed that stress is key feature in the etiology of MDD (Kessler, 1997). The trauma interview focuses on assessing severity of childhood experience with sexual and physical violence and early parental separation. Early parental separation is coded positively when subjects are separated from one or both parents for more than 6 months, before the age of 12. Mild ELS is coded when subjects experienced mild physical or sexual trauma before the age of 16. Severe ELS is coded when subjects experienced severe sexual trauma, severe physical trauma or both, before the age of 16. Coding of the interviews was performed by one trained rater. The 17-item Hamilton depression rating scale (HDRS) (Hamilton, 1960) assessed severity of MDD at baseline. The HDRS was repeated 8 weeks following study entry to evaluate both non-response and non-remission rates. Response was defined as a 50% improvement on the HDRS after 8 weeks. Remission was defined as a score of ≤ 7 on the HDRS at 8 weeks.
2.3.2 Reward task
We used a computerized reward learning task to measure reward responsiveness. Reduced reward responsiveness is hypothesized to be an important mechanism in the development of MDD (Eshel and Roiser, 2010). The task relies on signal-detection theory in which correct identifications of two stimuli were differentially rewarded. In 300 trials, divided in 3 blocks of 100 trials, two difficult-to-discriminate stimuli were briefly (100 ms) presented an equal number of times. The participants’ task was to win as much money as possible by accurately identifying which stimulus was presented after each trial. To induce a response bias, an asymmetrical reinforcer schedule was used, such as correct responses for one stimulus (referred to as the ‘rich’) were rewarded three times more frequently than correct responses of the other stimulus (referred to as the ‘lean’). Due to the unequal frequency of reward feedback, participants with high reward responsiveness were expected to develop a response bias in favor of the rich stimulus compared to the lean stimulus over the course of the 3 blocks. Subjects with low reward responsiveness were expected to develop a smaller or no response bias. The task has been described in detail by Pizzagalli et al. (2005) and has proven its ability to objectively measure reward responsiveness in healthy volunteers, as well as MDD (Pizzagalli et al., 2008).
2.4. Statistical analysis
SAS version 9.2 was used for statistical analyses. Pearson correlations were used to identify potential associations between variables. For the reward task, data reduction was performed as described by Pizzagalli et al. (2005). The main behavioural variable of interest was response bias (RB), which captures participants’ ability to modulate behaviour as a function of reward. RB was analyzed using a one-way within-subject repeated measure design with Block (Block 1,2,3) as repeated measure variable. To directly assess overall reward responsiveness, a difference score (Δresponse bias) between RB over blocks was calculated. Further, discriminability scores (which capture participants’ overall task performance) were analyzed, using a one-way within subject repeated measure analysis with block as repeated variable. Reaction time (RT) and hit rates (% correct responses) were calculated and analyzed to confirm that the reward task produced the intended behavioural effect, and investigated using Block x Stimulus (rich, lean) ANOVAs. Tukey-Kramer corrections were used when appropriate.
To investigate latent factors in this sample, we used principal components analysis (PCA) with VARIMAX rotation. Variables entered into the model were: positive and negative affect, anhedonia, reward responsiveness, retardation, non-interactiveness, agitation, early life stress, early parental separation, and neuroticism. All 10 items were normalized before running the model. For the number of factors considered, Eigenvalues >1.0, Screeplot, and clinical interpretability were taken into account. Item loadings, with values greater than 0.4, were used to describe the components.
We examined the relationship between the calculated new factor variables and depression severity, using a linear regression model, with HDRS score at time of inclusion as dependent variable. Further, potential latent dimensions were evaluated with regard to their relationship to outcome after 8 weeks of treatment using logistic regression models. Outcome was operationalized using response and remission rates. Two logistic regression models were run. In the first model, response rate was entered as dependent variable. In the second model, remission rate was entered as dependent variable. In the remission model, HDRS scores at time of inclusion were entered as covariate. Age and gender were included as covariates in the regression models.
3. RESULTS
3.1. Demographic and clinical data
Eighty-two depressed patients were included in the study. Five participants were excluded from the final statistical analysis because of invalid performance on the reward task. Two participants were excluded due to other missing data. Thirteen participants dropped out before the follow-up assessment. Sociodemographic and clinical data at baseline of our baseline sample (n=75) are reported in Table 1. Pearson correlations showed that HDRS scores were significantly correlated with SHAPS (r=0.46, p<0.0001), PA (r=−0.48, p<0.0001) and NA (r=0.29, p=0.01) scores. SHAPS and PA were inversely correlated (r=−0.39, p=0.0005). NA and neuroticism were significantly correlated (r=0.36, p=0.0002). All 3 subscales of the CORE-scale were correlated (all rs≥0.24, all ps≤0.04). Table 2 lists clinical information of our sample (n=62) after 8 weeks follow-up.
Table 1.
Sociodemographic and clinical characteristics at baseline (N=75).
| Variable | Value |
|---|---|
| Age (mean±SD) | 44.9±11.9 |
| Female (%) | 61.3 |
| Antidepressant treatment at baseline (%) | |
| Selective Serotonine reuptake inhibitors | 42.7 |
| Venlafaxine | 33.3 |
| Tricyclic antidepressants | 8 |
| Mirtazepine | 10.6 |
| None | 7.4 |
| Age of onset (mean±SD) | 35.9±13.1 |
| Number of episodes (%) | |
| First episode | 33 |
| Three or more episodes | 32 |
| HDRS | 16.7±4.9 |
| SHAPS | 7.1±3.5 |
| PANAS positive affect | 18.1±5.8 |
| PANAS negative affect | 33.7±8.4 |
| NEO-FFI neuroticism percentile | 8.1±1.3 |
| CORE (non-interactiveness) | 2.2±2.2 |
| CORE (retardation) | 4.5±3.6 |
| CORE (agitation) | 1.4±1.5 |
| Comorbidity axis I (%) | 58.7 |
| Stressful life events (%) | |
| Early mild sexual or physical trauma | 18.3 |
| Early severe sexual or physical trauma | 16.9 |
| Early parental separation | 26.8 |
HDRS: Hamilton rating scale of depression; SHAPS: Snaith-Hamilton-pleasure-scale; PANAS: Positive and negative affect scale; NEO-FFI: NEO-five factor inventory scale, standardized according to age and gender; CORE: CORE Assessment of psychomotor change scale; Comorbidity: assessed by SCID-I; Stressful life events: assessed by structured trauma inventory scale.
Table 2.
Clinical data after 8 weeks of treatment [N=62].
| Variable | Value |
|---|---|
| HDRS [mean±SD] | 10.9±6.9 |
| Response [%] | 40.3 |
| Remission [%] | 33.9 |
HDRS: Hamilton rating scale of depression; Response=50% improvement on the HDRS after 8 weeks; Remission=≤7 score on the HDRS at 8 weeks.
3.2. Reward task
Within-subjects ANOVA analyses on RB showed that the Block effect was not significant (F(2,142)=1.30, p=0.28, ε =0.98), suggesting that the participants did not developed a significant increase in RB towards the rich stimulus between blocks over time, consistent with prior reports highlighting blunted reward responsiveness in MDD samples tested with the identical reward task (Pizzagalli et al., 2008). One-way ANOVA on discriminability scores revealed no significant effect of Block (p>0.15), suggesting that task difficulty was stable across blocks. When considering hit rates, the Block (1,2,3) x Stimulus (lean and rich) ANOVA revealed only a significant Stimulus effect (F(1,71)=6.53, p=0.01), which was due to an overall significantly higher scores for the rich relative to the lean stimulus (Tukey-Kramer Adjusted p=0.01). For reaction time, the Block x Stimulus ANOVA highlighted a significant Block effect (F(2,142)=3.20, p=0.04). This effect was due to a significantly lower RT in Blocks 2 compared to Block 1 (Tukey-Kramer Adjusted p=0.03). Altogether, these findings highlight blunted reward responsiveness in the current MDD inpatients, who failed to show reliable behavioral modulations as a function of the asymmetric reinforcement schedule.
Reward learning between Block 1 and Block 2 (Δresponse bias2-1 = RBBlock 2–RBBlock 1) was significantly correlated with SHAPS scores (r=−0.33, p≤0.01). Unexpectedly, overall reward learning (Δresponse bias3-1 = RBBlock 3 – RBBlock 1) did not correlate significantly with SHAPS scores (r=−0.16, p=0.19). In light of these findings, Δresponse bias2-1 was used entered as the measure of reward responsiveness in further analyses.
3.3. Principal Component Analysis
Based on Eigenvalues >1.0, Screeplot, and clinical interpretability, a 3-factor solution was selected to extract valid, independent features, explaining 54.4% of total variance. Table 3 shows the three main components and their VARIMAX rotated item loadings. The first factor captured a psychomotor change dimension, with high loadings on non-interactiveness, retardation and agitation. Factor 2 represented the anhedonic dimension with high loadings on anhedonia, low reward responsiveness, low positive affect and early parental separation. The third factor comprised of negative affect, neuroticism and early life stress and was labeled as the negative affect dimension.
Table 3.
Rotated factor pattern for key values of MDD. Cut-off load is greater than 0.4.
| Scale item | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|
| Non-interactiveness | 0.885 | ||
| Retardation | 0.741 | ||
| Agitation | 0.630 | ||
| Anhedonia | 0.841 | ||
| early parental separation | 0.565 | ||
| Positive affect | −0.438 | ||
| Reward responsiveness | −0.622 | ||
| Negative affect | 0.713 | ||
| Neuroticism | 0.660 | ||
| Early life stress | 0.603 |
Factor 1 represents a psychomotor factor with high loadings on non-interactiveness, retardation and agitation. Factor 2 represents an anhedonia factor, with high loadings on anhedonia, low reward responsiveness, low positive affect and early parental separation. Factor 3 represents a negative affect factor, including negative affect, neuroticism and early life stress.
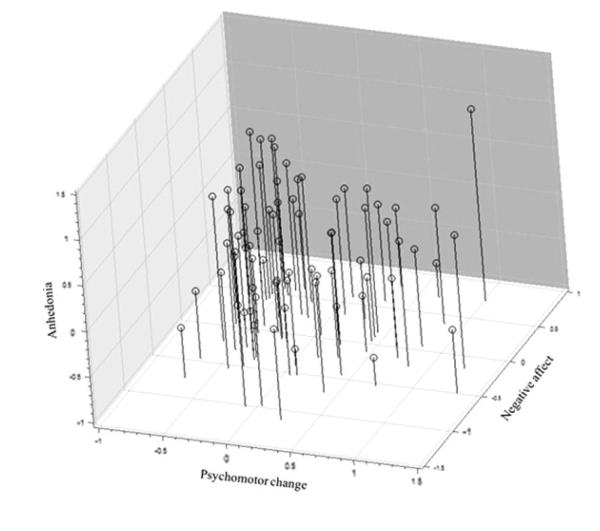
Additional analyses revealed that, based on eigenvalue greater than unity, a solution with 4 principal components should have been chosen as the final model. However, when running this model, we found that factor 1 (marked by high loadings on non-interactiveness and retardation) and 4 (marked by high loadings of agitation and early life trauma) consisted of only two variables with positive intercorrelations (findings available upon request). Factor 2 and 3 had similar loadings compared to the solution with 3 principal components. We decided therefore to discharge the model with 4 principal components, and select the 3-factor solution, which matched the screeplot and was the most interpretable. Three new factor variables for individual patients were computed using a weighted calculation. Pearson correlation analyses confirmed that the 3 principal components were not correlated (all ps>0.05). See Figure 1 to illustrate the relationship between the three factors.
Figure 1.
3D scatter plot illustrating the uncorrelated relationship ((all ps>0.05)) between the three calculated factor dimensions: Psychomotor (factor 1), anhedonia (factor 2) and negative affect (factor 3).
3.4. Prediction models
The factor variables were related to overall depression severity and outcome scores. First, we found that HDRS scores correlated significantly with the anhedonia factor (r=0.58, p≤0.0001) and negative affect factor (r=0.31, p=0.007), but not with the psychomotor factor (r=0.09, p>0.5). Next, all three factor variables were included as independent variables in a prediction model of HDRS. Stepwise linear regression analysis revealed an overall significant effect (F=20.86, p<0.0001), including the anhedonia factor (t=5.56, p≤0.001) and negative affect factor (t=1.98, p=0.05) as predictors of the HDRS scores after 8 weeks of treatment. 36.7% of HDRS variance was accounted for in the analysis. Second, using logistic regression with stepwise selection, we included the three factors as independent variables in two prediction models (one for non-response and one for non-remission). Non-remission at 8 weeks was predicted by the anhedonia factor (OR 9.28, CI 1.85–46.51, p=0.007), as well as the negative affect factor (OR 5.69, CI 1.19–27.20, p=0.03). The anhedonia factor was the only predictor left in the model of non-response at 8 weeks (OR 6.00, CI 1.46–24.59, p=0.01). Follow-up analyses indicated that none of the individual variables included in the anhedonia and negative affect factors was predictive of non-response or non-remission on its own, suggesting that only the combination of the components resulted in the predictive ability of the two dimensions.
4. DISCUSSION
The first aim of the present study was to identify latent factors, based on variables across different units of analysis, within an inpatient MDD sample. Secondly, we examined the clinical validity of these factors by assessing their relationship with overall depression severity and their ability to predict clinical outcome. A principal component analysis revealed three independent latent factors. Psychomotor change was extracted as the first factor, characterized by non-interactiveness, retardation and agitation. Factor 2 was labeled as the anhedonia factor, characterized in descending order by subjective anhedonic experience, blunted reward responsiveness (as assessed by a laboratory-based reward task), early parental separation and positive affect. Factor 3 included negative affect, neuroticism and early life stress and was labeled as the negative affect factor. When evaluating the clinical validity of the 3 factors, we found that HDRS score at time of inclusion was predicted by the anhedonia and negative affect factors. Moreover, the anhedonia factor was a strong predictor of non-response and non-remission. The negative affect factor predicted non-remission as well.
The emergence of the psychomotor factor was not surprising, since psychomotor change is commonly associated with MDD, especially in a melancholic subgroup of MDD and in combination with a more severe depression and anhedonic symptoms (Lemke et al., 1999; Taylor and Fink, 2008). However, our findings showed that psychomotor change was segregated from anhedonia, suggesting that these two symptoms represented two separate typologies among the current inpatient depressed sample. In addition, the psychomotor change factor was not associated with depression severity and did not play a significant role in predicting clinical outcome, raising the possibility that psychomotor symptoms are a state characteristic in MDD (Parker et al., 2000; Sobin et al., 1997).
The finding of the anhedonia factor is in line with and extended prior reports describing anhedonia as an important dimension of functioning within the MDD construct (APA, 1994; Fawcett et al., 1983). Proponents of the dimensional perspective hypothesize that chronic socio-environmental stressors in childhood may induce mild anhedonic-like behavior at an early age, resulting in a vulnerability to develop MDD in later life (Laos, 1996; Konkle et al., 2003), which may explain why early parental separation loaded on factor 2. This is strengthened by the fact that recent findings have suggested the involvement of both oxytocinergic and dopaminergic reward systems as the neurobiological basis of neglect in childhood, associating behaviors such as anhedonia to the development of the attachment system in childhood on a neurobiological level (Strathearn, 2011; Rilling, 2013). Furthermore, increasing neurobiological and behavioural research confirms the association of an hedonic trait with the conditioned response to reinforcement (or reward responsiveness) and goal-directed behavior (Keedwell et al., 2005; Vrieze et al. 2013). In addition, we found that the anhedonia factor was a strong predictor of depression severity and outcome after 8 weeks. These findings validate the common assumption that depressed subjects with prominent anhedonic features are more severely depressed and are associated with worse outcome scores compared to depressed subjects without these features (Burke et al., 2005; Kash et al., 2002). Moreover, the relation with outcome suggests that the factor is potentially a trait dimension, representing a continuum from normal to pathological dysfunction (Flett et al., 1997), and underline the relevance of monitoring anhedonia-associated psychopathology in early stages of treatment to refine the diagnosis of MDD and improve clinical decision making.
The negative affect factor captured elevation on a continuum of stress sensitivity in MDD (Hammen 2005; Wichers et al., 2007). First, it has been reported that subjects with elevated neuroticism experience stressful events more negatively and show poorer coping skills, leading to more emotional reactivity in reaction to stress (negative affect) as well as increasing a person’s vulnerability for the onset of MDD (Kendler et al., 2004). Second, early life stress (ELS) is known to increase the risk to develop MDD and it has been hypothesized that ELS may permanently shape neural circuit development, resulting in increased stress sensitivity in later life (Wichers et al., 2008). Finally, we found that overall depression severity, as well as non-remission was predicted by the negative affect factor, supporting the dimensional concept of stress sensitivity. Interestingly, the anhedonia factor was a much stronger predictor of response and remission scores, in comparison to negative affect, implying the notion that anhedonia is more a trait characteristic of MDD than the negative affect factor. This is in support of research stating that improvement of (more state-like) depressive symptoms is potentially primarily based on changes in (bio)psychopathology associated with stress and resilience (Wichers et al. 2012) and in line with the fact that antidepressants may primarily influences resilience-like mechanisms and not anhedonic (trait) characteristics (Geschwind et al. 2011).
Some important limitations of our study should be acknowledged. First, the sample size was relatively modest, particularly for a study involving principal component analyses. In order to address this limitation, we balanced the number of patients with the number of variables included in the statistical analyses; nevertheless, future studies should evaluate the generalizability of our findings. Second, participants were recruited from different psychiatric wards in an academic hospital. Mood data, such as depression severity scores ranged broadly and, on average, HDRS scores at time of inclusion were moderate. Nonetheless, all participants were diagnosed with MDD by a trained psychiatrist using DSM-IV criteria. Therefore, this sample represented the average MDD population seen in a regular clinical practice. Moreover, in light of our research aims, the broad variance of signs and symptoms in the patient group benefited our study. Third, it could be argued that the anhedonia dimension simply reflected a measure of depression severity, as suggested by its role as a predictor of depression severity and the strong correlation between HDRS scores at time of inclusion and the anhedonia dimension. This would make our prediction model of the outcome measures invalid due to an overlap of the explanatory and predictive variables. To avoid this issue, baseline HDRS scores were added as an independent variable into the prediction model of remission. Finally, in our PCA, we included descriptive symptoms (e.g., positive and negative affect), functional variables (e.g., reward responsiveness) and etiological variables (e.g., early parental separation). Mixing different ‘levels’ of variables may result in a biased view of the outcome of the PCA. On the other hand, as we stated before, our approach enabeled us to provide a more representative measure of each factor variable, compared to other factor analytic studies. However, it is important to emphasize that conclusions stemming from this study await future replications, which will contributed to elucidate the precise components involved in potential factor variables of MDD.
In spite of the limitations, this study identified psychomotor change, anhedonia and negative affect as independent MDD dimensions of functioning. The effort to define basic dimensions of functioning to be studied across multiple units of analysis is a novel approach and will help in improving integrative understanding of psychopathology for mental illnesses (Insel et al., 2010). The anhedonia and negative affect factor were both predictors of course and treatment response in MDD, which is an important addition to the findings. Identifying reliable predictors in research may allow for the development of novel and more personalized interventions. Moreover, in clinical practice, the ability to predict response and outcome before starting treatment might enable physicians to identify at-risk individuals and select complementary treatment options.
Acknowledgments
Role of funding source
This project was supported by a unrestricted research grant from Johnson and Johnson, by a research grant (OT06/60) from the University of Leuven (KUL) and by a grant (ELG-B5588-G.0193.07) from the Fund for Scientific Research, Flanders, Belgium (FWO).
Footnotes
Conflict of interest
Prof. Claes is Senior Clinical Investigator of the FWO. Dr Schmidt and de Boer are employees of Janssen Research and Development. Dr. Pizzagalli was supported by NIMH grant R01MH68376 and R21MH078979 and over the past 3 years has received consulting fees from Shire, AstraZeneca, Ono Pharma USA and Johnson & Johnson as well as honoraria from AstraZeneca for projects unrelated to the current study. Koen Demytennaere reports no conflict of interest directly related to the submitted manuscript. He is a board member and has received grants and served as a speaker in capacities unrelated to the manuscript. The other authors declare no competing financial interests.
5. References
- American Psychiatric Association (A.P.A.) Diagnostic and Statistical Manual of Mental Disorders. 4th. American Psychiatric Association; Washington, DC: 1994. Revised. [Google Scholar]
- Burke HM, Davis MC, Otte C, Mohr DC. Depression and cortisol responses to psychological stress: a meta-analysis. Psychoneuroendocrinology. 2005;30(9):846–56. doi: 10.1016/j.psyneuen.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Carragher N, Adamson G, Bunting B, McCann S. Subtypes of depression in a nationally representative sample. J. Affect. Disord. 2009;113(1-2):88–99. doi: 10.1016/j.jad.2008.05.015. [DOI] [PubMed] [Google Scholar]
- Cassano GB, Benvenuti A, Miniati M, Calugi S, Mula M, Maggi L, Rucci P, Fagiolini A, Perris F , Frank E. The factor structure of lifetime depressive spectrum in patients with unipolar depression. J. Affect. Disord. 2009;115(1-2):87–99. doi: 10.1016/j.jad.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Eaton WW, Gallo JJ, Nestadt G. Understanding the heterogeneity of depression through the triad of symptoms, course and risk factors: a longitudinal, population-based study. J. Affect. Disord. 2000;59(1):1–11. doi: 10.1016/s0165-0327(99)00132-9. [DOI] [PubMed] [Google Scholar]
- Comrey AL, Soufi A, Backer TE. Psychiatric screening with the Comrey personality scales. Psychol. Rep. 1978;42:1127–30. doi: 10.2466/pr0.1978.42.3c.1127. 3 Pt 2. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Psychological Assessment Resources. Odessa; Florida, USA: 1992. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) manual. [Google Scholar]
- Davidson RJ. Affective neuroscience and psychophysiology: toward a synthesis. Psychophysiology. 2003;40(5):655–65. doi: 10.1111/1469-8986.00067. [DOI] [PubMed] [Google Scholar]
- Draijer N, Langeland W. Childhood trauma and perceived parental dysfunction in the etiology of dissociative symptoms in psychiatric inpatients. Am. J. Psychiatry. 1999;156(3):379–85. doi: 10.1176/ajp.156.3.379. [DOI] [PubMed] [Google Scholar]
- Eshel N, Roiser JP. Reward and punishment processing in depression. Biol. Psychiatry. 2010;68(2):118–24. doi: 10.1016/j.biopsych.2010.01.027. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Clark DC, Scheftner WA, Hedeker D. Differences between anhedonic and normally hedonic depressive states. Am. J. Psychiatry. 1983;140(8):1027–30. doi: 10.1176/ajp.140.8.1027. [DOI] [PubMed] [Google Scholar]
- Flett GL, Vredenburg K, Krames L. The continuity of depression in clinical and nonclinical samples. Psychol. Bull. 1997;121(3):395–416. doi: 10.1037/0033-2909.121.3.395. [DOI] [PubMed] [Google Scholar]
- Franken IH, Rassin E, Muris P. The assessment of anhedonia in clinical and non-clinical populations: further validation of the Snaith-Hamilton Pleasure Scale (SHAPS) J. Affect. Disord. 2007;99(1-3):83–9. doi: 10.1016/j.jad.2006.08.020. [DOI] [PubMed] [Google Scholar]
- Geschwind N, Nicolson NA, Peeters F, van Os J, Barge-Schaapveld D, Wichers M. Early improvement in positive rather than negative emotion predicts remission from depression after pharmacotherapy. Eur Neuropsychopharmacol. 2011;21(3):241–7. doi: 10.1016/j.euroneuro.2010.11.004. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Ann. Rev. Clin. Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Harald B, Gordon P. Meta-review of depressive subtyping models. J. Affect. Disord. 2012;139(2):126–40. doi: 10.1016/j.jad.2011.07.015. [DOI] [PubMed] [Google Scholar]
- Hasler G, Drevets WC, Manji HK, Charney DS. Discovering endophenotypes for major depression. Neuropsychopharmacology. 2004;29(10):1765–81. doi: 10.1038/sj.npp.1300506. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R. Pine D.S., Quinn K. Sanislow C., Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–51. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Insel TR, Charney DS. Research on major depression: strategies and priorities. JAMA. 2003;289(23):3167–8. doi: 10.1001/jama.289.23.3167. [DOI] [PubMed] [Google Scholar]
- Kasch KL, Rottenberg J, Arnow BA, Gotlib IH. Behavioral activation and inhibition systems and the severity and course of depression. J. Abnorm. Psychol. 2002;111(4):589–97. doi: 10.1037//0021-843x.111.4.589. [DOI] [PubMed] [Google Scholar]
- Keedwell PA, Andrew C, Williams SCR, Brammer MJ, Philips ML. The neural correlates of anhedonia in major depressive disorder. Biol. Psychiatry. 2005;58:843–853. doi: 10.1016/j.biopsych.2005.05.019. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am. J. Psychiatry. 2004;161(4):631–6. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Setting boundaries for psychiatric disorders. Am. J. Psychiatry. 1999;156(12):1845–8. doi: 10.1176/ajp.156.12.1845. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The effect of stressful life events on depression. Ann. Ev. Psychol. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Konkle AT, Baker SL, Kentner AC, Barbagallo LS, Merali Z, Bielajew C. Evaluation of the effects of chronic mild stressors on hedonic and physiological responses: sex and strain compared. Brain Res. 2003;992(2):227–38. doi: 10.1016/j.brainres.2003.08.047. [DOI] [PubMed] [Google Scholar]
- Lemke MR, Puhl P, Koethe N, Winkler T. Psychomotor retardation and anhedonia in depression. Acta Psychiatr. Scand. 1999;99(4):252–6. doi: 10.1111/j.1600-0447.1999.tb07221.x. [DOI] [PubMed] [Google Scholar]
- Loas G. Vulnerability to depression: a model centered on anhedonia. J. Affect. Disord. 1996;41:39–53. doi: 10.1016/0165-0327(96)00065-1. [DOI] [PubMed] [Google Scholar]
- Parker G, Roy K, Hadzi-Pavlovic D, Mitchell P, Wilhelm K, Menkes DB, Snowdon J, Loo C, Schweitzer I. Subtyping depression by clinical features: the Australasian database. Acta Psychiatr. Scand. 2000;101(1):21–8. doi: 10.1034/j.1600-0447.2000.101001021.x. [DOI] [PubMed] [Google Scholar]
- Parker G, Hadzi-Pavlovic D, Wilhelm K, Hickie I, Brodaty H, Boyce P, Mitchell P, Eyers K. Defining melancholia: properties of a refined sign-based measure. Br. J. Psychiatry. 1994;164(3):316–26. doi: 10.1192/bjp.164.3.316. [DOI] [PubMed] [Google Scholar]
- Pizzagalli DA, Jahn AL, O'Shea JP. Toward an objective characterization of an anhedonic phenotype: a signal-detection approach. Biol. Psychiatry. 2005;57(4):319–27. doi: 10.1016/j.biopsych.2004.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Iosifescu D, Hallett LA, Ratner KG, Fava M. Reduced hedonic capacity in major depressive disorder: evidence from a probabilistic reward task. J Psychiatr Res. 2008;43(1):76–87. doi: 10.1016/j.jpsychires.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rilling JK. The neural and hormonal bases of human parental care. Neuropsychologia. 2013;51(4):731–47. doi: 10.1016/j.neuropsychologia.2012.12.017. [DOI] [PubMed] [Google Scholar]
- Schrijvers D, Hulstijn W, Sabbe BG. Psychomotor symptoms in depression: a diagnostic, pathophysiological and therapeutic tool. J. Affect. Disord. 2008;109(1-2):1–20. doi: 10.1016/j.jad.2007.10.019. [DOI] [PubMed] [Google Scholar]
- Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. J. Clin. Psychol. 2006;62(1):123–46. doi: 10.1002/jclp.20213. [DOI] [PubMed] [Google Scholar]
- Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. Br. J. Psychiatry. 1995;167(1):99–103. doi: 10.1192/bjp.167.1.99. [DOI] [PubMed] [Google Scholar]
- Sobin C, Sackeim HA. Psychomotor symptoms of depression. Am. J. Psychiatry. 1997;154(1):4–17. doi: 10.1176/ajp.154.1.4. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID) I: History, rationale, and description. Arch. Gen. Psychiatry. 1992;49(8):624–9. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Strathearn L. Maternal neglect: oxytocin, dopamine and the neurobiology of attachment. J Neuroendocrinol. 2011;23(11):1054–65. doi: 10.1111/j.1365-2826.2011.02228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor MA, Fink M. Restoring melancholia in the classification of mood disorders. J. Affect. Disord. 2008;105(1-3):1–14. doi: 10.1016/j.jad.2007.05.023. [DOI] [PubMed] [Google Scholar]
- Vrieze E, Ceccarini J, Pizzagalli DA, Bormans G, Vandenbulcke M, Demyttenaere K. Van Laere K., Claes S. Measuring extrastriatal dopamine release during a reward learning task. Hum Brain Mapp. 2013;34(3):575–86. doi: 10.1002/hbm.21456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrieze E, Claes SJ. Anhedonia and Increased Stress Sensitivity: Two Promising Endophenotypes for Major Depression. Curr. Psychiatry Reviews. 2009;5(3):143–152. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J. Pers. Soc. Psychol. 1988;54(6):1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. J. Abnorm. Psychol. 1995;104(3):542–5. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- Wichers M, Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, Vlietinck R, Delespaul P, Van Os J. Genetic risk of depression and stress-induced negative affect in daily life. Br. J. Psychiatry. 2007;191:218–23. doi: 10.1192/bjp.bp.106.032201. [DOI] [PubMed] [Google Scholar]
- Wichers M, Schrijvers D, Geschwind N, Jacobs N, Myin-Germeys I, Thiery E, Derom C, Sabbe B, Peeters F, Delespaul P, van Os J. Mechanisms of gene-environment interactions in depression: evidence that genes potentiate multiple sources of adversity. Psychol. Med. 2008;6:1–10. doi: 10.1017/S0033291708004388. [DOI] [PubMed] [Google Scholar]
- Wichers M, Lothmann C, Simons CJ, Nicolson NA, Peeters F. The dynamic interplay between negative and positive emotions in daily life predicts response to treatment in depression: a momentary assessment study. Br J of Clin Psychology. 2012;51(2):206–22. doi: 10.1111/j.2044-8260.2011.02021.x. [DOI] [PubMed] [Google Scholar]
- Zimmerman M. Introduction: selecting an antidepressant. CNS Spectr. 2009;14(12 Suppl 12):4–7. doi: 10.1017/s1092852900026341. [DOI] [PubMed] [Google Scholar]