Abstract
Evidence suggests that affect plays a role in the development of psychosis but the underlying mechanism requires further investigation. This study examines the moment-to-moment dynamics between negative affect (NA) and paranoia prospectively in daily life. A female general population sample (n = 515) participated in an experience sampling study. Time-lagged analyses between increases in momentary NA and subsequent momentary paranoia were examined. The impact of childhood adversity, stress sensitivity (impact of momentary stress on momentary NA), and depressive symptoms on these time-lagged associations, as well as associations with follow-up self-reported psychotic symptoms (Community Assessment of Psychic Experiences and the Symptom Checklist-90-Revised) were investigated. Moments of NA increase resulted in a significant increase in paranoia over 180 subsequent minutes. Both stress sensitivity and depressive symptoms impacted on the transfer of NA to paranoia. Stress sensitivity moderated the level of increase in paranoia during the initial NA increase, while depressive symptoms increased persistence of paranoid feelings from moment to moment. Momentary paranoia responses to NA increases were associated with follow-up psychotic symptoms. Examination of microlevel momentary experience may thus yield new insights into the mechanism underlying co-occurrence of altered mood states and psychosis. Knowledge of the underlying mechanism is required in order to determine source and place where remediation should occur.
Key words: momentary assessment methodology, stress, childhood adversity, psychotic symptoms, depressive symptoms
Introduction
Recent evidence indicates that the phenotype of psychosis is dimensional in nature and that the more frequent subclinical psychotic experiences share demographic, etiological, and familial factors with the more severe clinical psychotic symptoms.1 Furthermore, persistence of subclinical experiences of psychosis has been shown to predict transition to clinical symptoms and help-seeking behavior.2
Psychotic symptoms tend to occur more often in a context of negative mood states, at both the subclinical and the clinical level of expression.3,4 In a large general population study, psychotic experiences were reported by 27% of the individuals with an anxiety disorder or depression.5 Furthermore, the presence of psychotic experiences and clinically relevant psychotic symptoms in these individuals was progressively more likely with greater levels of manic or depressive symptoms.4 Also, depression and psychosis share a number of important risk factors such as childhood adversity,6–8 social dysfunction,9,10 social defeat experiences,11 and daily life stress sensitivity.12–15 Together, this suggests that affective alterations may be relevant to the development of both disorders.15 Support for this notion comes from a recent twin study,16 which showed a role for childhood adversity, daily life stress sensitivity, and current depressive symptoms in the shared pathway toward depression and psychotic symptoms. Also, previous studies demonstrated that the above risk factors enhance the experience of negative affect (NA),6,12–15 suggesting that NA could be the key element that increases risk for both depression and psychosis. Cohort studies can show associations between symptom domains; however, they are less suitable to find out why significant factors on the causal pathway contribute to shared risk for both depression and psychosis. To further disentangle the underlying mechanisms, we may have to zoom in to the level of moment-to-moment affective dynamics connecting NA and subclinical feelings of paranoia. This shift from the epidemiological (macro) level to the microlevel of hour-by-hour tracking of emotional dynamics may help explain whether and how exactly affective experiences impact on risk for psychosis,17 and how shared risk factors such as childhood adversity, stress sensitivity, and depressive symptoms may impact on dynamics between NA and subclinical paranoid ideation.
The Experience Sampling Method (ESM) is a technology that allows for prospective tracking of affective and psychotic experiences from moment to moment,18,19 and thus suitable to examine how within-person change in one variable impacts on change in the other variable later on the same day.20
Therefore, the aim of the current study was to use ESM to examine prospectively (1) how moment-to-moment increase in NA impacts on subsequent feelings of paranoia, (2) whether this effect is moderated by childhood adversity, daily life stress sensitivity, and depressive symptoms, and finally (3) whether the dynamics between NA and paranoia are moderated by follow-up course of psychotic symptoms.
Methods
Sample
Data were derived from 621 female individuals (576 twins and 45 non-twin sisters), who were part of a longitudinal, general population twin study on genes, stress sensitivity, and depression. Subjects were aged 18–61 years. They were recruited by mail (for details, see Jacobs and colleagues21) from the East Flanders Prospective Twin Survey (EFPTS) and from birth registers of Flemish municipalities in Belgium. The EFPTS population-based survey has prospectively recorded all multiple births in the province of East Flanders since 196422,23. The project was approved by the local ethics committee. All participants gave written informed consent. Given evidence for qualitative differences in the type of environmental stressors that are associated with depression in men and women,24 the sample was female only.
Procedure
In this study, the ESM was completed at baseline as well as additional measurements of psychopathology. Furthermore, participants completed four follow-up assessments (T1–T4) with measurements of psychopathology. The average number of days between baseline and T1 was 132, 91 between T1 and T2, 116 between T2 and T3, and 91 between T3 and T4. All interviews were administered by trained research psychologists or graduate psychological assistants.
ESM Assessment
ESM is a momentary assessment technique to prospectively assess momentary experiences of subjects in their daily living environment.13,18,19 Subjects received a digital wristwatch and a set of ESM self-assessment forms collected in a booklet for each day. The wristwatch was programmed to emit a signal (beep) at an unpredictable moment in each of ten 90-min time blocks between 7.30 am and 10.30 pm, on five consecutive days, resulting in a maximum of 50 beeps per person. The study used a semi-random beep design to prevent anticipatory behavior of participants (for more methodological information, see previous ESM literature).13,14,18
Appraisals of minor daily stressful events and momentary feelings were measured. To measure ESM event-related stress, subjects were asked to report the most important event that happened between the current and the previous beep. This event was subsequently rated on a 7-point bipolar scale (from −3 = very unpleasant, 0 = neutral, to 3 = very pleasant). Event appraisals were thus available at each measurement. The scale was reversed so that higher scores represented a greater degree of dislike for the event (event stress). Stress sensitivity was defined as the effect of the (un)pleasantness appraisal of the most important event that had happened since the last beep on NA.6,12–14 Appraised events are thus compared for their level of NA. To create the variable stress sensitivity, the weighted mean NA was regressed on ESM event-related stress, resulting in a separate beta coefficient for each individual (see also Wichers and colleagues13).
Current affective states and feelings of paranoia were assessed as follows: “at this moment I feel....” The items assessing paranoia and other negative affective states were embedded in a list of adjectives comprising both negative and positive affective states. To prevent participants from reporting an overall negative affective experience, positive and negative items were alternated.
Factor analysis identified a single factor representing NA. The items “insecure,” “lonely,” “anxious,” “low,” and “guilty”—weighted for their factor loadings—were averaged to form the measurement of NA (respective loadings were: 0.71, 0.60, 0.66, 0.68, 0.61).
For the current purpose, paranoia was assessed separately with the adjective “suspicious” conforming to previous studies.20,25
Potential Moderators
Childhood Adversity.
Childhood adversity was measured at baseline (T0) using the shortened version Childhood Trauma Questionnaire (CTQ)26,27 comprising 25 items that assess five dimensions of childhood maltreatment: (1) physical abuse, (2) emotional abuse, (3) sexual abuse, (4) physical neglect, and (5) emotional neglect. At the request of Twin Registry, the four most explicit items concerning sexual and physical abuse were omitted, resulting in a 21-item self-report questionnaire. Items were scored on a scale of 1 (never true) to 5 (very often true). The sum score of all items was used as a continuous measure of childhood adversity.
Depressive Symptoms.
A continuous measure of depressive symptoms was obtained using the validated depression subscale (13 items) of the Symptom Checklist-90-Revised (SCL-90-R).28,29 The SCL-90-R depression scores collected at baseline (T0) were used as a measure of current depressive symptoms.
Psychotic Symptoms.
Psychotic symptoms were measured in two ways. First, psychotic symptoms were measured with the SCL-90-R with the two validated subscales paranoid ideation (6 items) and psychoticism (10 items).28,29 The SCL-90-R was administered at all T0–T4 measurement occasions. Baseline psychosis score was assessed at T0. Follow-up SCL-90-R psychosis score was calculated as the mean over the measurements at T1, T2, T3, and T4. The mean of the four follow-up measurements was used to obtain reliable assessments of follow-up psychotic symptoms.
Second, psychotic experiences were assessed with the Community Assessment of Psychic Experiences (CAPE).30 The CAPE is a 42-item validated self-report questionnaire to assess psychopathological experiences in the general population.30 Items resemble positive symptoms of schizophrenia (20 items), negative symptoms (14 items), and depressive symptoms (8 items). The CAPE was administered 3 times, at baseline T0, and at T2 and T4. A baseline psychosis score was constructed using the positive symptom dimension at T0; a follow-up psychosis score was constructed using the mean of this dimension over the follow-ups (T2 and T4).
Statistical Analysis
Analyses were carried out in STATA 11.031. As ESM measurements of NA and paranoia were available for 5 days with a maximum of 10 measurements per day per person with an average 90min in between, the data were ideally suited to explore the dynamic within-subject temporal associations between NA and paranoia. Within-subject fluctuations of paranoia following a within-subject increase in NA were examined. Within-subject increase in NA was defined as reporting higher levels of NA compared with the beep before. An advantage of measurements of within-subject change is that all potential between-person differences in scoring tendencies on the Likert scale are eliminated. To examine paranoia fluctuations following NA increase, all the beep moments with a within-subject increase in NA, compared with the beep before, were selected. Variables were created representing paranoia at beep moments before, during, and following the increase in NA (ie, paranoia at t − 1, t, t + 1, t + 2, t + 3, t + 4, t + 5). Thus, multiple time lags were examined to create a fine-grained “film” of changes in paranoia relating to an increase in NA in daily life. The data were reshaped in long format with a new “time” variable representing the distance in beeps from the moment of “increase in NA.” In this way, a multilevel regression analysis with time as the independent and paranoia as the dependent variable could be carried out. The time value t − 1 (one beep before the increase in NA) was taken as reference value.
The following models were used: The main effect of NA increase on paranoia over t − 1 to t + 5 was examined by regressing paranoia following the NA increase on time. To test the hypothesis that putative risk factors moderate the effect of time on paranoia following NA increase, paranoia was regressed on the interaction between the risk factor and time. This was done separately for each of the three risk factors, by regressing paranoia on the relevant 2-way interaction (respectively: “childhood adversity × time,” “stress sensitivity × time,” and “current depressive symptoms × time”). To facilitate interpretation of the 2-way interaction analyses, dose-response relationships were graphically displayed. These were assessed by dividing the distributions of the continuous risk factor variables (childhood adversity, stress sensitivity, and current depressive symptoms, respectively) by their tertiles. Stratified effect sizes were calculated by linear combination of the relevant variables in the model containing the interaction, using the STATA LINCOM routine. Main effects and interactions were evaluated statistically with Wald tests. Independence of the different interactions was examined by simultaneously entering all three interactions into the regression model.
Finally, analyses were conducted to examine whether moment-to-moment NA-paranoia dynamics were associated with follow-up course of psychotic symptoms. In this analysis, it was examined whether the effect of time (in beeps) on paranoia was moderated by follow-up SCL-90-R and CAPE psychosis score. These analyses were corrected for baseline psychosis score.
ESM data have a hierarchical structure in which ESM observations (level 1) are clustered within participants (level 2). In addition, in the current data set, participants (level 2) were clustered within twin pairs (level 3). Data were, therefore, analyzed using multilevel random regression analysis with the XTMIXED module. Analyses were adjusted for the absolute amount of NA increase because the amount of emotional change may confound the subsequent response. Continuous variables were standardized to obtain comparable standardized effect sizes.
Results
Subject Characteristics
Of the total subject sample of 621 white females, 610 participated in the ESM procedure. Thirty-one subjects were excluded because they missed more than 30% of valid ESM self-reports.18 This resulted in a subject sample of 579 female subjects. Another 64 individuals were excluded because they did not demonstrate an increase in NA over the total ESM period, resulting in a sample of 515 individuals. An additional 8, 24, and 7 individuals had missing values for childhood adversity, stress sensitivity, and current depressive symptoms, respectively. Furthermore, 2 and 53 individuals had missing values at all follow-up measurements of SCL-90-R and CAPE psychosis scores, respectively.
Mean age of the 515 subjects was 27.7 years (SD = 8.3, range 18–61). Sixty-four percent had a college or university degree, 34% completed secondary education, and 1% had primary education only. The majority were currently employed (60% employed, 37% students, 3% unemployed). At baseline, 66 subjects (12.8%) had one or more Structured Clinical Interview for DSM-IV Axis I disorders (SCID-I) psychotic symptoms. Twenty-five subjects (4.9%) had a current major depression and 86 (16.7%) had a history of major depression. Baseline mean item scores for SCL-90-R depression, SCL-90-R psychosis, CAPE psychosis, and childhood adversity were 1.6 (SD = 0.62), 1.4 (SD = 0.41), 1.3 (SD = 0.21), and 1.7 (SD = 0.63), respectively. Mean stress sensitivity score was.0.2 (SD = 0.29). Correlations between childhood adversity, stress sensitivity, and current SCL-90-R depression were low to moderate, ranging from .14 to .24 and .39.
A total of 37 valid beep reports were completed per individual. At the selected beep moments with a NA increase (N obs = 2906, n subj = 515), the average reported NA (on a scale from 1 to 7) was 2.0 (SD = 0.86), average NA increase was.66 (SD = 0.60), and average paranoia was 1.4 (SD = 1.0). Average reported paranoia before and following increase in NA varied from 1.2 to 1.3. Correlations between paranoia and NA items varied from .11 to .31. Mean follow-up SCL-90-R psychosis item scores ranged from 1 to 3.1 (median of 1.2). Mean follow-up CAPE psychosis item scores ranged from 1 to 1.9 (median of 1.2).
NA and Paranoia Daily Dynamics
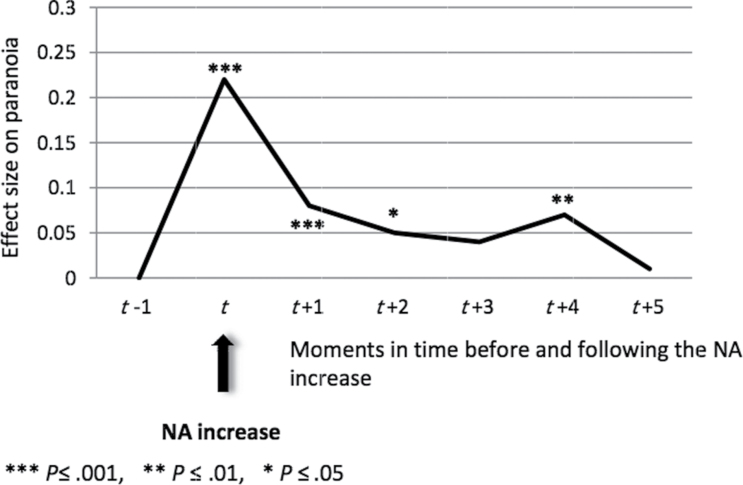
Paranoia was significantly increased at moments following the increase in NA. Up to four beep moments later (at t, t + 1 [±90 min], t + 2 [±180 min], and t + 4 [±360 min]), the increase in paranoia, compared with paranoia at t − 1, was statistically significant (see figure 1).
Fig. 1.
Paranoia fluctuations over time following negative affect (NA) increase. Levels of paranoia at the different beep moments were tested for significance compared with their baseline level (at t − 1).
Moderation of NA-Paranoia Dynamics by Risk Factors
Childhood Adversity.
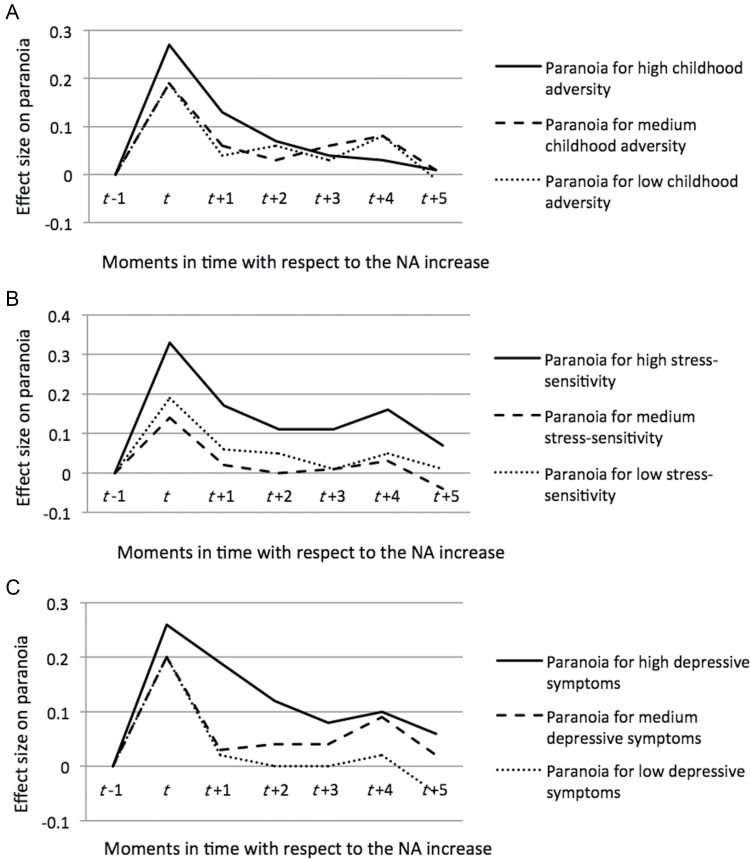
Childhood adversity positively moderated the effect of increase in NA on subsequent paranoia levels. For two consecutive moments (t and t + 1; up to ±90min following the increase in NA), the interaction effect of “time × childhood adversity” on paranoia was significant (table 1), with greatest effect sizes for those in the highest tertile group of childhood adversity (figure 2a).
Table 1.
Moderation by Risk Factors of the Effect of Time (Before and Following Increase in NA) on Paranoia
| Effect on paranoia | Childhood Adversity × Timea | Childhood Adversity × Timea,b | Stress Sensitivity × Timea | Stress Sensitivity × Timea,b | Depression × Timea | Depression × Timea,b | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | χ2 | P | β | χ2 | P | β | χ2 | P | β | χ2 | P | β | χ2 | P | β | χ2 | P | |
| t: During NA increase | .05 | 4.2 | .04 | .02 | 0.8 | .36 | .07 | 9.7 | .002 | .06 | 7.5 | .006 | .03 | 2.0 | .15 | .00 | 0.0 | .99 |
| t + 1: 1 beep later | .06 | 5.1 | .02 | .02 | 0.5 | .49 | .06 | 5.3 | .02 | .04 | 2.3 | .13 | .08 | 10.1 | .002 | .06 | 4.8 | .03 |
| t + 2: 2 beeps later | .04 | 2.8 | .09 | .01 | 0.1 | .80 | .01 | 0.1 | .79 | −.01 | 0.1 | .72 | .05 | 4.6 | .03 | .04 | 2.4 | .12 |
| t + 3: 3 beeps later | .01 | 0.1 | .78 | −.02 | 0.3 | .59 | .03 | 1.6 | .21 | .03 | 0.8 | .38 | .03 | 1.0 | .31 | .02 | 0.6 | .42 |
| t + 4: 4 beeps later | −.02 | 0.6 | .44 | −.05 | 2.1 | .15 | .03 | 0.9 | .35 | .02 | 0.6 | .45 | .02 | 0.4 | .54 | .02 | 0.4 | .53 |
| t + 5: 5 beeps later | .02 | 0.8 | .38 | .01 | 0.0 | .88 | .02 | 0.4 | .54 | .01 | 0.1 | .81 | .05 | 2.4 | .12 | .04 | 1.2 | .28 |
Note: All effects sizes of the interactions were standardized. Significant interaction effects are in bold. The reference category is the moment before the increase in negative affect (NA) (t − 1). Time difference between beeps is on average 90min.
aAnalysis is corrected for absolute increase in NA.
bFull model includes all three 2-way interactions (childhood adversity × time, stress sensitivity × time, and depression × time).
Fig. 2.
Effect of time on paranoia following negative affect (NA) increase stratified by level of childhood adversity (a), stress sensitivity (b), or current depressive symptoms (c), respectively.
Stress Sensitivity.
Stress sensitivity positively moderated the effect of an increase in NA on subsequent paranoia levels (see table 1). For two consecutive moments (t and t + 1; up to ±90min following the increase in NA), the interaction effect of “time × stress sensitivity” on paranoia was significant, again with greatest effect sizes being apparent for those in the highest tertile group of stress sensitivity (figure 2b).
Current Depressive Symptoms.
Current depressive symptoms positively moderated the effect of NA increase on subsequent paranoia levels (see table 1). For two consecutive moments (t + 1 and t + 2; from ±90 up to ±180min following the increase in NA), the interaction effect between depressive symptoms and time on paranoia was significant, again with greatest effect sizes for those in the highest tertile group of current depressive symptoms (figure 2c).
Independence of Effects of Childhood Adversity, Stress Sensitivity, and Current Depressive Symptoms
When all three 2-way interaction variables were entered simultaneously in the model (table 1), the significance of “childhood adversity (continuous) × time” on paranoia following the NA increase at both t and t + 1 was lost (8% and 26% drop in effect size, respectively). The moderation of the effect by stress sensitivity remained significant only at the moment of NA increase (effect sizes dropped 2% at t and 16% at t + 1, respectively). The moderation of the effect by “current depressive symptoms” remained significant at t + 1, but not at t + 2 (9% and 11% drop in effect size, respectively).
The Association Between the Paranoia Response to NA Increase in Daily Life and Follow-Up Psychotic Symptoms
Follow-up psychotic symptoms positively moderated the effect of NA increase on subsequent paranoia levels. For three consecutive moments (t, t + 1, and t + 2; up to ±180min following the increase in NA), the interaction effect between mean follow-up SCL-90-R psychosis score and time following NA increase on paranoia was significant (table 2).
Table 2.
Moderation of the Effect of Time (Before and Following Increase in NA) on Paranoia by Follow-Up Psychotic Symptoms
| Effect on Paranoia | Follow-Up SCL-90-R Psychosis | Follow-Up CAPE Psychosis | ||||
|---|---|---|---|---|---|---|
| β | χ2 | P | β | χ2 | P | |
| t: Paranoia at NA increase | .08 | 14.1 | ≤.001 | .07 | 9.8 | .002 |
| t + 1: Paranoia 1 beep later | .10 | 15.5 | ≤.001 | .06 | 4.9 | .03 |
| t + 2: Paranoia 2 beeps later | .05 | 4.0 | .05 | .06 | 4.2 | .04 |
| t + 3: Paranoia 3 beeps later | .04 | 2.5 | .11 | .03 | 1.1 | .30 |
| t + 4: Paranoia 4 beeps later | .04 | 1.7 | .19 | .06 | 3.5 | .06 |
| t + 5: Paranoia 5 beeps later | .06 | 3.4 | .07 | .08 | 5.4 | .02 |
Note: CAPE, Community Assessment of Psychic Experiences; NA, negative affect; SCL-90-R, Symptom Checklist-90-Revised. All effects sizes of the interactions were standardized. Significant interaction effects are in bold. The reference category is the moment before the increase in NA (t − 1). Time difference between beeps is on average 90min. All analyses were corrected for baseline levels of psychotic experiences.
The interaction effect between mean follow-up CAPE psychosis and time following NA increase on paranoia was significant at four beep moments (t, t + 1, t + 2, and t + 5; up to 450min following the increase in NA) (see table 2).
Discussion
This study showed a subtle moment-to-moment dynamic interplay between NA and feelings of paranoia. An increase in NA resulted in a simultaneous increase in feelings of paranoia that remained significant up to 3h afterward. Furthermore, childhood adversity, stress sensitivity, and current depressive symptoms differentially affected the dynamic interplay between NA and paranoia, in terms of changes in increase and persistence of the paranoia response to the change in NA. Finally, individuals with higher SCL-90-R and CAPE follow-up psychotic symptoms showed increased transfer of NA to feelings of paranoia. Thus, paranoia following subtle everyday feelings of NA was associated with future course of symptoms, indicating that daily life microdynamics between NA and paranoia are relevant for future symptomatology.
Emotional Dynamics: A Differentiation Between Amplitude and Persistence
The current results illustrate how affective risk factors exert their effects at the microlevel of daily life experiences. Results demonstrated that childhood adversity, stress sensitivity, and current depressive symptoms all impacted on the dynamic interplay between NA and paranoia. However, the effect of childhood adversity was no longer significant when the interactions of all risk factors were entered into the model simultaneously. Because childhood adversity is known to increase stress sensitivity,6 variance previously explained by childhood adversity was likely explained by stress sensitivity in the latter model. Stress sensitivity and depressive symptoms, however, did show independent effects on the transfer of NA to paranoid feelings, but differed in the mechanism by which they impacted on this transfer. While stress sensitivity exerted an immediate effect, the effect of current depressive symptoms on paranoia had a delayed onset. Stress sensitivity increased the amplitude of the paranoia boost at the moment of NA increase, possibly reflecting altered attentional focus on negative valence.32,33 Depressive symptoms, on the other hand, did not significantly influence the amplitude at the moment of NA increase, but affected the persistence of paranoia. Depressive symptoms thus increased the time that paranoid feelings remained present over the day. Alterations in rumination, a response-focused emotion regulation strategy, or alterations in capacity for cognitive reappraisal, an antecedent-focused emotion regulation strategy, may play a role in persistence of paranoid feelings in individuals with depressive symptoms.32–36 Epidemiological studies found that, at the macrolevel, persistence of psychotic symptoms is a strong risk factor for developing clinically relevant psychotic symptoms.2 It should be further investigated whether this is also true for psychotic experiences at the level of moment-to-moment persistence. This study showed that both stress sensitivity and depressive symptoms impacted on the dynamic interplay between NA and paranoia. This contrasts with a previous study,16 which showed that depressive symptoms, but not daily life stress sensitivity, was the final mediator on the pathway from childhood adversity to psychosis. However, it is possible that persistence of paranoia, associated here with depressive symptoms, has a stronger influence on future course than moment-specific higher levels of paranoia, associated here with stress sensitivity.
Insights Into the Affective Pathway of Psychosis: Combining Knowledge of the Macro- and the Microlevels of Experience
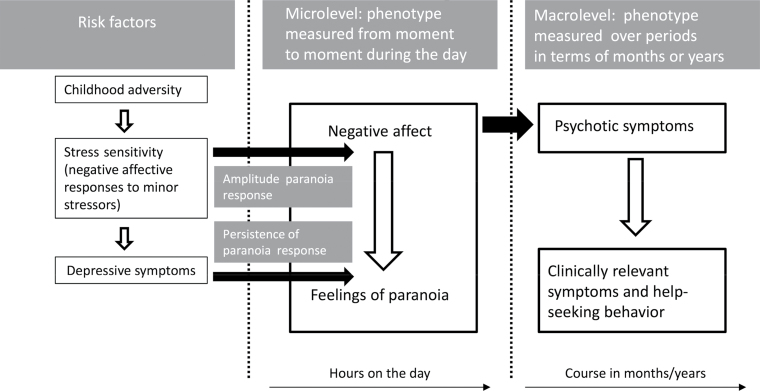
The current results provide further insights into the underlying mechanisms of the co-occurrence of affective symptomatology and psychosis (see figure 3). At the epidemiological (macro) level, it has been shown that (1) childhood adversity is a risk factor for both depressive and psychotic symptoms,6,7 (2) childhood adversity predicts increased negative affective responses to stress in daily life,6,15 (3) stress sensitivity in turn predicts depressive and psychotic symptoms,13,14 and (4) depressive symptoms mediate the pathway from childhood adversity to psychotic symptoms.16 Furthermore, psychotic symptoms, especially when persistent, constitute a risk factor for later clinical symptoms, help-seeking behavior, and, finally, the development of diagnosable psychotic disorder.2,17 The shift to the microlevel in the current study adds insights into how and why risk factors for NA may impact on the later development of psychosis. It seems that at the momentary level NA may drive the experience of low-level paranoid feelings. Repetitively such increases in paranoia experiences following boosts of NA may sensitize individuals and build up to something more clinically relevant.37 This study showed indeed that the accumulation of everyday subtle paranoia following increase in NA predicted future course of psychotic symptoms. The findings of the current study thus support the idea that the smallest and most subtle emotional patterns and interaffective responses in daily life cumulatively may result in observable psychotic symptoms months later. Zooming in to the microlevel may, therefore, constitute a way to uncover the smallest building blocks of the dimensional development of psychosis. Knowledge of these underlying mechanisms is highly relevant to get closer to the exact source and place where remediation should take place.
Fig. 3.
The figure shows schematically how and why risk factors for psychosis may exert their influence on later macrolevel course of psychotic symptoms by their impact on microlevel hour-to-hour emotional dynamics. Risk factors change the microlevel hour-to-hour interplay between negative affect (NA) and paranoia by increasing the amplitude or persistence of paranoia experiences following NA boosts. These subtle changes in repetitive everyday emotional dynamics are found associated with follow-up course of psychotic symptoms measured over periods of months. These psychotic symptoms, when persistent, may eventually result in clinical psychosis and help-seeking behavior.
The findings should be interpreted in the light of current knowledge on emotion regulation, the processes by which humans modify negative and positive emotions with regard to their intensity, when they occur, how long they last, and how they are expressed.32 The “Process Model” by Gross32,33 is the leading model of emotion regulation. It proposes that emotions unfold as a multicomponential process, whereby a situation occurs (either external or internal) that is then attended to, giving rise to an appraisal of the situation’s valence and motivational relevance, which results in a series of experiential, behavioral, and neurophysiological response changes. As discussed above, both antecedent-focused (situation selection, situation modification, attentional deployment, cognitive change/reappraisal) and response-focused (response modulation/affective suppression/rumination) emotion regulation strategies may be relevant in explaining the findings. Therefore, interventions teaching individuals to use emotion regulation strategies, as developed for use in anxiety disorders and depression,36 may be relevant in this context. For example, emotion regulation therapies directed at teaching reappraisal may decrease the types of negative experiences that give rise to paranoia and psychosis.33,35,36 Future studies are needed to examine how potentially predictive real-life patterns of paranoia can assist in improving personalized risk assessment and clinical decision making.38
Methodological Issues
A critical remark is that effect sizes in this study are relatively small (under 0.2).39 However, unlike effects reported in most unilevel studies, these effects do not impact once, but impact repeatedly on daily life experience. Therefore, effect sizes reported in the current study, although below Cohen’s39 indication of 0.2, cumulatively may well be clinically significant.
We do not exclude the possibility that continuation of NA itself also induced continuation of paranoia over time. Thus, paranoia persistence may not be independent of co-occurring NA. However, in our opinion, this does not diminish the clinical relevance of the findings. Instead, it shows how closely NA is involved in the development of subtle experiences of paranoia, which eventually and cumulatively may contribute to development of psychotic symptomatology.
Second, childhood adversity was measured retrospec tively with a self-report questionnaire, which was adapted on request of the Flemish Twin Register. The total average childhood adversity score may be somewhat lower due to the omission of the four most explicit items. This may have resulted in reduced effect sizes of early adversity on paranoia following the NA increase. Also, twins may differ from singletons in that they may experience more social support (compared with non-twins) that buffers against psychopathology. If this is the case, then the current results likely reflect a conservative estimation of the effects in the general population. The low average childhood adversity score and its limited variability may also indicate that the subjects sample is a privileged and relatively healthy group.
Furthermore, ESM measurements of affect, stress sensitivity, and paranoia are based on subjective reports. However, the prospective nature of the study and in-the-moment collection of observations minimalized influences of recall bias or cognitive reinterpretation. Also, self-reported compliance, as assessed electronically in a subsample, was very high (96.4%).40 However, the use of an electronic ESM device in which the exact time of answering the questions is recorded will enhance accuracy of measurements.
Finally, subjects were female with a high mean educational level. Due to gender differences in risk factors for different pathways to psychosis,15 the results of the study may not be generalized to men and those with lower educational level.
Funding
This research was supported by the Netherlands Organi sation for Scientific Research. Since its origin, the East Flanders Prospective Survey has been partly supported by grants from the Fund of Scientific Research, Flanders and Twins, a nonprofit Association for Scientific Re search in Multiple Births (Belgium). Dr M.W. was supported by the Netherlands Organisation for Scientific Research (VENI grant nr. 916.76.147) and by ZON-MW (grant nr. 171001002). Prof. Dr I.M.-G. was supported by a 006NARSAD Young Investigator Award and by the Netherlands Organisation for Scientific Research (VIDI grant nr. 917.76.341).
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009; 39: 179–195 [DOI] [PubMed] [Google Scholar]
- 2. Wigman JT, van Winkel R, Raaijmakers QA, et al. Evidence for a persistent, environment-dependent and deteriorating subtype of subclinical psychotic experiences: a 6-year longitudinal general population study. Psychol Med. 2011; 41: 2317–2329 [DOI] [PubMed] [Google Scholar]
- 3. Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009; 35: 383–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van Rossum I, Dominguez MD, Lieb R, Wittchen HU, van Os J. Affective dysregulation and reality distortion: a 10-year prospective study of their association and clinical relevance. Schizophr Bull. 2011; 37: 561–571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wigman JT, van Nierop M, Vollebergh WA, et al. Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity-implications for diagnosis and ultra-high risk research. Schizophr Bull. 2012; 38: 247–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wichers M, Schrijvers D, Geschwind N, et al. Mechanisms of gene-environment interactions in depression: evidence that genes potentiate multiple sources of adversity. Psychol Med. 2009; 39: 1077–1086 [DOI] [PubMed] [Google Scholar]
- 7. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012; 38: 661–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Freeman D, Fowler D. Routes to psychotic symptoms: trauma, anxiety and psychosis-like experiences. Psychiatry Res. 2009; 169: 107–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Corcoran CM, Kimhy D, Parrilla-Escobar MA, et al. The relationship of social function to depressive and negative symptoms in individuals at clinical high risk for psychosis. Psychol Med. 2011; 41: 251–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van Rijn S, Schothorst P, Wout Mv, et al. Affective dysfunctions in adolescents at risk for psychosis: emotion awareness and social functioning. Psychiatry Res. 2011; 187: 100–105 [DOI] [PubMed] [Google Scholar]
- 11. Selten JP, Cantor-Graae E. Social defeat: risk factor for schizophrenia? Br J Psychiatry. 2005; 187: 101–102 [DOI] [PubMed] [Google Scholar]
- 12. Wichers M, Geschwind N, Jacobs N, et al. Transition from stress sensitivity to a depressive state: longitudinal twin study. Br J Psychiatry. 2009; 195: 498–503 [DOI] [PubMed] [Google Scholar]
- 13. Wichers M, Myin-Germeys I, Jacobs N, et al. Genetic risk of depression and stress-induced negative affect in daily life. Br J Psychiatry. 2007; 191: 218–223 [DOI] [PubMed] [Google Scholar]
- 14. Myin-Germeys I, van Os J, Schwartz JE, Stone AA, Delespaul PA. Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry. 2001; 58: 1137–1144 [DOI] [PubMed] [Google Scholar]
- 15. Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007; 27: 409–424 [DOI] [PubMed] [Google Scholar]
- 16. Kramer IMA, Simons CJP, Myin-Germeys I, et al. Evidence that genes for depression impact on the pathway from trauma to psychotic-like symptoms by occasioning emotional dysregulation. Psychol Med. 2012; 42: 283–294 [DOI] [PubMed] [Google Scholar]
- 17. van Os J, Linscott RJ. Introduction: the extended psychosis phenotype–relationship with schizophrenia and with ultrahigh risk status for psychosis. Schizophr Bull. 2012; 38: 227–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Delespaul P. Assessing Schizophrenia in Daily Life: The Experience Sampling Method. Maastricht, the Netherlands: University of Limburg; 1995. [Google Scholar]
- 19. Csikszentmihalyi M, Larson R. Validity and reliability of the Experience-Sampling Method. J Nerv Ment Dis. 1987; 175 526–536 [DOI] [PubMed] [Google Scholar]
- 20. Thewissen V, Bentall RP, Oorschot M, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Clin Psychol. 2011; 50: 178–195 [DOI] [PubMed] [Google Scholar]
- 21. Jacobs N, Myin-Germeys I, Derom C, Vlietinck R, van Os J. Deconstructing the familiality of the emotive component of psychotic experiences in the general population. Acta Psychiatr Scand. 2005; 112: 394–401 [DOI] [PubMed] [Google Scholar]
- 22. Loos R, Derom C, Vlietinck R, Derom R. The East Flanders Prospective Twin Survey (Belgium): a population-based register. Twin Res. 1998; 1: 167–175 [DOI] [PubMed] [Google Scholar]
- 23. Derom CA, Vlietinck RF, Thiery EW, Leroy FO, Fryns JP, Derom RM. The East Flanders Prospective Twin Survey (EFPTS). Twin Res Hum Genet. 2006; 9: 733–738 [DOI] [PubMed] [Google Scholar]
- 24. Kendler KS, Thornton LM, Prescott CA. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry. 2001; 158: 587–593 [DOI] [PubMed] [Google Scholar]
- 25. Simons CJ, Wichers M, Derom C, et al. Subtle gene-environment interactions driving paranoia in daily life. Genes Brain Behav. 2009; 8: 5–12 [DOI] [PubMed] [Google Scholar]
- 26. Arntz A, Wessel I. Jeugd Trauma Vragenlijst [Dutch Version of the Childhood Trauma Questionnaire]. Maastricht, the Netherlands: Author; 1996. [Google Scholar]
- 27. Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003; 27: 169–190 [DOI] [PubMed] [Google Scholar]
- 28. Arrindel W, Ettema J. SCL-90. Een multidimensionele psychopathologie indicator [The SCL90. A Multidimensional Instrument for the Assessment of Psychopathology]. Lisse, the Netherlands: Swets & Zeitlinger; 1986. [Google Scholar]
- 29. Derogatis LR. SCL90: Administration, Scoring and Procedures Manual-1 for the Revised Edition. Baltimore, MD: John Hopkins School of Medicine; 1977. [Google Scholar]
- 30. Stefanis NC, Hanssen M, Smirnis NK, et al. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. 2002; 32: 347–358 [DOI] [PubMed] [Google Scholar]
- 31. StatCorp STATA Statistical Software: Release 11. College Station, TX: Statacorp LP; 2009. [Google Scholar]
- 32. Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol. 1998; 2: 271–299 [Google Scholar]
- 33. Gross JJ. Emotion regulation: affective, cognitive, and social consequences. Psychophysiology. 2002; 39: 281–291 [DOI] [PubMed] [Google Scholar]
- 34. Kimhy D, Vakhrusheva J, Jobson-Ahmed L, Tarrier N, Malaspina D, Gross JJ. Emotion awareness and regulation in individuals with schizophrenia: implications for social functioning [published online ahead of print July 03, 2012]. Psychiatry Res. 10.1016/j.psychres.2012.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003; 85: 348–362 [DOI] [PubMed] [Google Scholar]
- 36. Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behav Ther. 2004; 35: 205–230 [DOI] [PubMed] [Google Scholar]
- 37. Collip D, Myin-Germeys I, Van Os J. Does the concept of “sensitization” provide a plausible mechanism for the putative link between the environment and schizophrenia? Schizophr Bull. 2008; 34: 220–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wichers M, Simons CJP, Kramer IMA, et al. Momentary assessment technology as a tool to help patients with depression help themselves. Acta Psychiatr Scand. 2012; 124: 262–272 [DOI] [PubMed] [Google Scholar]
- 39. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 40. Jacobs N, Nicolson NA, Derom C, Delespaul P, van Os J, Myin-Germeys I. Electronic monitoring of salivary cortisol sampling compliance in daily life. Life Sci. 2005; 76: 2431–2443 [DOI] [PubMed] [Google Scholar]