Abstract
Previous studies have shown that social ties enhance both physical and mental health, and that social isolation has been linked to increased cognitive decline. As part of our cognitive training platform, we created a socialization intervention to address these issues. The intervention is designed to improve social contact time of older adults with remote family members and friends using a variety of technologies, including Web cameras, Skype software, email and phone. We used usability testing, surveys, interviews and system usage monitoring to develop design guidance for socialization protocols that were appropriate for older adults living independently in their homes. Our early results with this intervention show increased number of social contacts, total communication time (we measure email, phone, and Skype usage) and significant participant satisfaction with the intervention.
I. Introduction
Previous studies have demonstrated an association between social relationships and health, prompting House et al1 in 1988 to propose a causal relationship in which lack of quality social relationships is likened to cigarette smoking and obesity in its capacity to negatively affect health. In the decades following this observation the evidence for this association has grown even stronger. In a recent meta-analysis of 148 reports analyzing the relationship between social relationships and non-suicidal mortality, the authors concluded that, after controlling for other factors, “individuals with adequate social relationships have a 50% greater likelihood of survival compared to those with poor or insufficient social relationships”2—an effect magnitude comparable with that of smoking and exceeding that of risk factors such as obesity, which draw much more media attention.
Although relatively few socialization interventions have been reported in the literature, there have been some relevant experiments. Winningham and Pike compared a 3-month social-cognitive intervention to a control group in a sample of elderly assisted living residents3. Although the intervention did not explicitly provide instruction in a social domain (it was cognitive), the format was highly interactive and involved working together with other residents. After the intervention, the control group was found to have decreased ratings of social satisfaction/increased loneliness, while the intervention group maintained their scores. This study suggests some protective effect of structured social activity intervention against a trend of increasing loneliness.
Routasalo, Pitkala and colleagues conducted a study of a psychosocial intervention with a 3 year follow up in a sample of elderly subjects4–6. This was a facilitated group therapy intervention, aimed at encouraging lonely older adults to share feelings in a small group, support one another, become empowered, and form friendships. The researchers found that subjects in the treatment group reported having made more friends a year later than the control subjects (m=45 % and m=32%, respectively). The treatment group members also were less likely to have died two years later at another follow-up, and used fewer healthcare services in the interim. These studies provide preliminary research on socialization interventions for older adults, but it remains to be seen whether such interventions would have long term effects on cognitive decline and overall health.
In this paper we describe a low-cost and scalable approach to providing a comprehensive socialization intervention for older adults using a health coaching platform for facilitating a health coach in managing health interventions for a large panel of patients.
II. Remote Health Coaching Platform
As part of a series of health coaching projects at the Oregon Center for Aging and Technology (ORCATECH), we developed a general-purpose architecture for providing computer-based health interventions for elders in their homes, facilitated by a professional health coach7–9. This architecture incorporates knowledge representations to enable the use of known principles of health behavior change. For example, we include modules to assess health behavior goals, motivations, barriers and readiness to change. We use this information as part of a dynamic user model that is continuously updated with measures from sensor data in the home. Changes in the user model can be used to trigger alerts and tailored feedback messages. There are two interfaces to the coaching platform: 1) the patient interface and a coach interface. The patient interface has a home page with general news, semi-automated tailored weekly messages from the coach, and an action plan for the week. Other patient pages include specific activities for coaching interventions on
cognitive exercise (adaptive computer games with embedded measures of memory, divided attention, planning, and verbal fluency,7,8)
physical exercise (computer videos with chair exercises)
sleep management (relaxation exercises, sleep hygiene, etc.)
socialization (as described below)
The design of the health coaching platform includes a dynamic user model, incorporating assessments relating to health behavior change principles. These variables include data sharing preferences, baseline health behaviors, readiness-to-change measures, as well as patient-specific motivations and barriers to change. Sensor data from the home provides feedback and updates on the adherence of patients’ activities and adherence to their health goals. This data then triggers active methods for both alerting and automated coaching messages. Our protocol for the health interventions involves having the health coach send out messages of feedback and encouragement at least once per week. These messages are automatically generating from the coaching system with the ability to be additionally edited by the health coach.
Our needs assessment for this project showed that older adults were primarily concerned about maintaining their cognitive health and factors that related to it, including socialization8. In a series of studies leading up to our current platform for cognitive health coaching we have been able to show that older adults (mean age 81.5 ± 6.0 years) were able to maintain computer use and cognitive exercise use over the period of one year7–9. Following this we added coaching protocols for physical exercise and novelty exercise. We have been able to show that participants (average age 76.7 ± 8.2 years) could communicate with a health coach successfully via email, phone, and messaging to a home portal coaching page for a period of 6 months.
The primary benefit of this design approach is that multiple health behavior interventions can be made available using a common architecture and knowledge representation that encourages a principled approach to the delivery of care to the home. We have also focused on a design to facilitate the participation of family members and informal caregivers as part of the care team. The activity data, including sleep quality, degree of physical exercise and cognitive exercise can be fed back to family members for follow-up and “soft” alerts. In addition, with our new socialization module, the family members play a large role in the intervention to improve the older adult’s socialization. In the studies described in the following sections, we explored the feasibility of providing a socialization module, using Web cameras and Skype software to link remote family members with study participants.
III. Feasibility Study using Skype for Socialization
In starting a new health intervention with an older adult population, it is critical to test the feasibility of all aspects of the deployment, including the usability of the technology, the training and training materials required, and the implementation protocol. The following sections describe our feasibility testing of the new socialization intervention.
A. Methods
As a feasibility study of our socialization intervention, we enrolled 9 independently living older adults (mean age 73.8 ± 6.7, 89% female) without dementia (MMSE ≥ 24; CDR ≤ 0.5 at baseline). Each participant and a selected remote family member were provided with a Web camera and Skype video conferencing software. The remote health coach also used Skype video conferencing with the participants to supplement the weekly email and Web communications. The participants were interviewed at 3 months to determine user satisfaction, usability issues with the technology, as well as general impressions and suggestions for future use. In addition, Skype usage and general computer usage were also measured throughout the study.
B. Results of the Feasibility Study
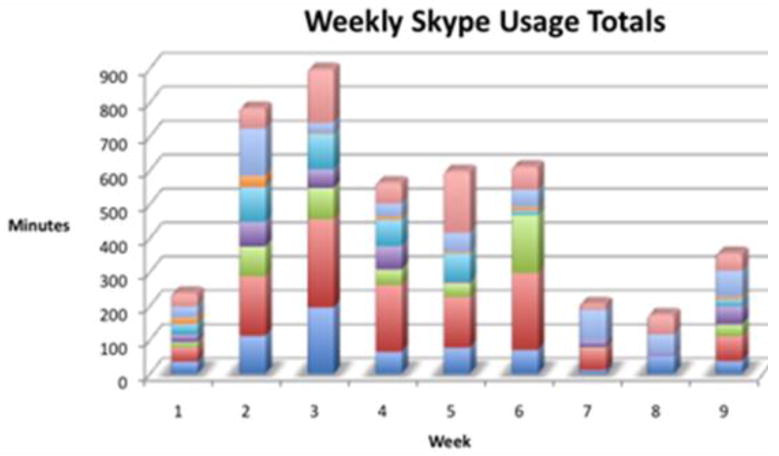
At baseline, only 2/3 of our participants were completely satisfied with their socialization. Our goal was to be able to provide a socialization intervention using Skype that could improve their social network and time interacting with people. Over a nine-week period, the study participants logged 4410 minutes of videoconferencing, with a peak usage occurring during week three (1247 min). Fig. 1 shows a graph of the Skype usage in minutes for each week, with each participant represented as a different color. Although the usage dropped off as time went on, most participants used Skype at least one hour per week.
Fig. 1.
Plot of Skype usage over a 9 week period. Each participant’s time for a give week is indicated in a separate color.
In total, the 9 participants talked to 45 different contacts (individual range: 2–10). On average, each of the 9 participants communicated with over 5 people using Skype during the study period. Although they had been trained and encouraged to communicate with their selected family member, as is typical with this form of communication, one’s person of interest is often not online at the same time. In debriefings, our participants reported that when their family members were not available, they often noticed the familiar names of other study members, who were more likely to be online and on Skype at the same time. Our participants often initiated video calls with other study participants and reported developing fast friendships that extended to other social activities as well.
Although there were some technical challenges in the start-up and training phases, all participants continued to see a benefit from using Skype to communicate with remote family members and friends. In addition to improvements in levels of socialization over the 9 week period, all of the participants saw a significant benefit to using Skype for communicating with family members and all rated the experience as either excellent or good.
All of our participants felt this was a compelling component of the cognitive health coaching intervention and indicated that they were interested in continuing with this aspect of the study.
IV. Socialization as a Broader Health Intervention
A. Exploring the Length of Videoconference Calls
Following our feasibility study of a Skype-based socialization intervention for older adults, we tested our ability to use Skype video for coaching assessments and feedback. In order to determine optimal coaching protocols, we tried various lengths of meeting times to determine how long we could keep a participant on Skype video without tiring the user. Table 1 shows the length of Skype-based coaching calls for 6 participants. Although some participants were able to stay engaged on the phone for a half hour, other sessions were much shorter. It became apparent that we needed to tailor the calls schedule to the individuals. However, for the most part, we determined that Skype calls of 20–30 minutes could be acceptable to study participants.
Table 1.
Coaching session lengths in minutes
| Age | Gender | Session Duration (Minutes) |
|---|---|---|
| 76 | F | 6:45 |
| 83 | F | 23:06 |
| 79 | F | 3:20 |
| 79 | F | 12:59 |
| 85 | F | 28:18 |
| 92 | F | 13:10 |
A. Expanded Socialization Activities
Based on the feedback from our feasibility study, we subsequently developed an expanded set of socialization intervention for older adults, with a goal of offering sufficient variety of socialization activities to keep the participants engaged over a sustained period of 6–12 weeks. The protocol and activities for socialization may occur simultaneously with other coaching activities that are in maintenance phase of behavior change. The activities for the first phase of the intervention (Level 1) are listed in Table 2.
Table 2.
Activity selections for the Level 1 phase of the socialization coaching intervention.
| Technology | Activity | Freq |
|---|---|---|
| Computer | Make a Skype call to family member, friend, study participant, or coach | 1–3 / wk |
| Computer | Participate in group Skype call | 1 / wk |
| Computer | Send email to family member, friend, study participant or coach | 1–3 /wk |
| Computer | Participate in online support group or chat | 1 / wk |
| Computer | Play online card or board game with others | 1 / wk |
| Computer | Use Facebook – new interaction | 1 / wk |
| Phone | Make a phone call to family member, friend, study participant, or coach | 1–3 / wk |
| In Person | Visit with family or friends | 1–2 / wk |
| In Person | Play a board or card game with someone | 1 / wk |
| In Person | Participate in a community event | 1 / wk |
| In Person | Participate in a volunteer activity | 1 / wk |
| In Person | Walk in a public place (mall, park) for at least 10 minutes | 1 / wk |
The first step in starting a socialization intervention with a participant involves determining a baseline social network and level of activities. We characterize this using the Ludden Social Network Scale-Revised (LSNS-R)10, which is a brief instrument measuring social contacts in the categories of family and friends (including neighbors). In addition, we use the UCLA-R Loneliness Scale10 to assess loneliness at baseline and after the intervention.
For coaching purposes, we also use motivational interviewing to assess motivations, barriers and readiness-to-change for each selected activity. In the first level (Level1) the coach begins by recommending at least 1 activity from the computer, phone, and in-person options. In subsequent weeks, if the participant dislikes a particular activity or is more comfortable in another, the plan is altered to reflect that. The coach and automated system strive to improve the individual’s degree of social interactions while maintaining comfort.
When a participant progresses to Level 2, they are asked to choose at least 2 activities from each category and to raise the frequency of interactions. The feedback and recording of their participation in the intervention is based on unobtrusive sensors in the home, as described below.
A. Unobtrusive Monitoring of Socialization
The Health Coaching Study participants have a standard set of sensors in the home. These include passive IR motion sensors for measuring activity in each room. These sensors are used to estimate cognitive performance, motor speed, sleep quality, and to infer activities of daily living. We monitor cognitive performance using interactions with the computer, ranging from motor speed estimates from typing behavior, to linguistic complexity analysis, and estimates for memory, divided attention, planning and verbal fluency from embedded measures in our adaptive cognitive computer games. In addition, for socialization, we use a metric that combines time spent in the video and chat aspects of Skype use, time and number of contacts in email, and time and contacts on the phone. In addition, with information from door switches, we are able to determine time out of the home, which we presume to be social to some degree. This information is used as input to the algorithms that construct feedback messages and summaries for the coach to relay to the participant.
V. Discussion
We have shown that video conferencing software is a feasible technology for facilitating socialization among older adults in a home environment. All of our participants felt this was a compelling component of the cognitive health coaching intervention and indicated that they were interested in continuing with this aspect of the study. In addition, it is possible to monitor various aspects of social contacts, including Skype use, email contacts and time, phone contacts and time, as well as time out of the apartment or home.
We have developed a set of socialization activities that may be useful in increasing social interactions for older adults, but it remains to be seen if these can be sustained over time. A side benefit of having people enrolled in a study where all are using Skype and are motivation to increase socialization is that the study partners themselves become available as contacts. This aspect was seen as one of the most compelling aspects of the project.
VI. Conclusion
Previous studies have shown that social ties enhance both physical and mental health, and that social isolation has been linked to increased cognitive decline. As part of our cognitive training platform, we offer a socialization intervention to address these issues. The intervention is designed to improve the social contact time of older adults in the home with family members and friends using a variety of technologies, including Web cameras, Skype software, email and phone. The main focus of the recommend protocols for improving socialization was on the video conferencing component of Skype. We currently coach more than 20 elderly participants who routinely use computers as part of our coaching project. Each participant selected a remote family member or friend to also be enrolled in the study. All were provided with Logitech cameras and Skype videoconferencing software. After basic training in using the system, participants are able to then videoconference or use the real-time chat feature to communicate directly with the coach, remote family member or friend, as well as other study participants. The coach works with each participant to assign weekly activities and target socialization goals as part of an individualized action plan. Typical activities include recommendations for Skype activities such as “Skype at least one new person this week” or Skype Adventure (a guided activity of jointly creating text stories using the Chat feature. In addition, we offer phone and email recommendations, as well face-to-face encounters. Our early results with this intervention show increased number of social contacts, total communication time (we measure email, phone, and Skype usage) and significant participant satisfaction with the intervention.
Acknowledgments
The authors would like to acknowledge the support and assistance of the staff associated with ORCATECH, the Oregon Center for Aging and Technology. In addition, we would like to thank the participants enrolled in the ORCATECH Living Lab for their continuing support and instructive feedback.
Footnotes
This work was supported the National Institute on Aging (Grants NIA P30AG024978 and ASMMI0116ST) and the Alzheimer’s Association.
Contributor Information
Holly B. Jimison, Email: jimisonh@ohsu.edu.
Krystal A. Klein, Email: kleinkr@ohsu.edu.
Jennifer L. Marcoe, Email: marcoej@ohsu.edu.
References
- 1.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 2.Holt-Lunstad J, Smith TB, Layton JB. Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Winningham RG, Pike NL. A cognitive intervention to enhance institutionalized older adults’ social support networks and decrease loneliness. Aging & Mental Hlth. 2007;11:716–721. doi: 10.1080/13607860701366228. [DOI] [PubMed] [Google Scholar]
- 4.Routasalo PE, Tilvis RS, Kautiainen H, Pitkala KH. Effects of psychosocial group rehabilitation on social functioning, loneliness and well-being of lonely, older people: randomized controlled trial. Journal of Advanced Nursing. 2009;65:297–305. doi: 10.1111/j.1365-2648.2008.04837.x. [DOI] [PubMed] [Google Scholar]
- 5.Pitkala KH, Routasalo P, Kautiainen H, Tilvis RS. Effects of Psychosocial Group Rehabilitation on Health, Use of Health Care Services, and Mortality of Older Persons Suffering From Loneliness: A Randomized, Controlled Trial. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2009;64A:792–800. doi: 10.1093/gerona/glp011. [DOI] [PubMed] [Google Scholar]
- 6.Pitkala KH, Routasalo P, Kautiainen H, Sintonen H, Tilvis RS. Effects of socially stimulating group intervention on lonely older people’s cognition: a randomized controlled trial. American Journal of Geriatric Psychiatry. 2011;19:654–663. doi: 10.1097/JGP.0b013e3181f7d8b0. [DOI] [PubMed] [Google Scholar]
- 7.Jimison HB, Pavel M, Bissell P, McKanna J. A framework for cognitive monitoring using computer game interactions. Studies in health technology and informatics. 2007;129:1073–1077. [PubMed] [Google Scholar]
- 8.Jimison HB, Pavel M. Integrating Computer-Based Health Coaching into Elder Home Care. In: Mihailidis A, Boger J, Kautz H, Normie L, editors. Technology and Aging. IOS Press; Amsterdam, The Netherlands: 2008. [Google Scholar]
- 9.Jimison HB, Pavel M, Larimer N, Mullen P. A General Architecture for Computer Based Health Coaching. Proceedings of the International Conference on Technology & Aging; Toronto. 2007. [Google Scholar]
- 10.Zunzunegui MV, Alvarado BE, Del Ser T, Otero A. Social networks, social integration, and social engagement determine cognitive decline in community-dwelling Spanish older adults. J Gerontol B Psychol Sci Soc Sci. 2003;58:S93–S100. doi: 10.1093/geronb/58.2.s93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuhrer R. How gender affects patterns of social relations and their impact on health: a comparison of one or multiple sources of support from “close persons. Social Science & Medicine. 2002;54:811–825. doi: 10.1016/s0277-9536(01)00111-3. [DOI] [PubMed] [Google Scholar]
- 12.Cutrona CE. Objective determinants of perceived social support. J Pers Soc Psychol. 1986;50:349–355. doi: 10.1037//0022-3514.50.2.349. [DOI] [PubMed] [Google Scholar]
- 13.Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39:472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- 14.Luanaigh CÓ, Lawlor BA. Loneliness and the health of older people. Int J Geriat Psychiatry. 2008;23:1213–1221. doi: 10.1002/gps.2054. [DOI] [PubMed] [Google Scholar]
- 15.Ertel KA, Glymour MM, Berkman LF. Effects of Social Integration on Preserving Memory Function in a Nationally Representative US Elderly Population. American Journal of Public Health. 2008;98:1215–1220. doi: 10.2105/AJPH.2007.113654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crooks VC, Lubben J, Petitti DB, Little D, Chiu V. Social Network, Cognitive Function, and Dementia Incidence Among Elderly Women. American Journal of Public Health. 2008;98:1221–1227. doi: 10.2105/AJPH.2007.115923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bassuk SS, Glass TA, Berkman LF. Social disengagement and incident cognitive decline in community-dwelling elderly persons. Ann Intern Med. 1999;131:165–173. doi: 10.7326/0003-4819-131-3-199908030-00002. [DOI] [PubMed] [Google Scholar]