Abstract
S100A8 and S100A9 are major leukocyte proteins, known as damage-associated molecular patterns, found at high concentrations in the synovial fluid of patients with rheumatoid arthritis (RA). A heterodimeric complex of S100A8/A9 is secreted by activated leukocytes and binds to Toll-like receptor 4, which mediates downstream signaling and promotes inflammation and autoimmunity. Serum and synovial fluid levels of S100A8/A9 are markedly higher in patients with RA than in patients with osteoarthritis or miscellaneous inflammatory arthritis. Serum levels of S100A8/A9 are significantly correlated with clinical and laboratory markers of inflammation, such as C-reactive protein, erythrocyte sedimentation rate, rheumatoid factor, and the Disease Activity Score for 28 joints. Significant correlations have also been found between S100A8/A9 and radiographic and clinical assessments of joint damage, such as hand radiographs and the Rheumatoid Arthritis Articular Damage score. In addition, among known inflammatory markers, S100A8/A9 has the strongest correlation with total sum scores of ultrasonography assessment. Furthermore, baseline levels of S100A8/A9 are independently associated with progression of joint destruction in longitudinal studies and are responsive to change during conventional and biologic treatments. These findings suggest S100A8/A9 to be a valuable diagnostic and prognostic biomarker for RA.
Keywords: S100A8; S100A9; Arthritis, rheumatoid; Biological markers
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease characterized by synovial inflammation, destruction of joint cartilage and bone erosion. Although the etiopathology of RA remains unclear, the infiltration of inflammatory leukocytes, primarily macrophages, proliferation of synovial fibroblasts and local production of proinflammatory cytokines play significant roles in disease progression [1,2]. The activation of synovial macrophages or synovial fibroblasts may trigger the activation of lymphocytes and subsequent inflammation in synovium since inactivating these cells reduces arthritis in experimental models [3]. Early diagnosis is of particular interest in this potentially aggressive disease to prevent joint deformity and functional impairment.
The management of RA depends on an exact measurement of disease activity, as well as early diagnosis [4,5]. A biomarker reflecting the amount of inflammation and joint destruction would aid in RA prognosis and be clinically helpful in optimizing individualized medical treatment. Early stages of RA development can be predicted using clinical and serological measures [3,6,7]. Inflammatory markers can also facilitate detection of residual disease activity and be used to adjust individual treatment needs. Thus far, the erythrocyte sedimentation rate (ESR) and the acute phase protein C-reactive protein (CRP) are the most widely used laboratory markers for evaluation of inflammatory activity in patients with RA [8-10]. Recently, the multibiomarker disease activity (MBDA) test, measuring various biomarkers, has proven useful for objectively assessing disease activity in patients with RA. However, the currently available biological tests are not predictive for radiographic progression [11].
THE S100 PROTEINS
The S100 proteins are major monocyte/macrophage proteins that bind calcium, constituting ~40% of the cytosolic protein in neutrophil granulocytes [12-15]. Currently, more than 20 members of the S100 family have been identified [16,17]. These proteins belong to the damage-associated molecular patterns family, also called alarmins, and are the endogenous molecules that signal the early phase of tissue and cell damage [18-20]. The major source for extracellular S100 proteins is via active nonclassical secretion rather than passive release from necrotic cells [21]. The S100 proteins have a critical role in inflammation as they can activate the innate immunity pathway mediated by Toll-like receptors (TLR) or receptors for advanced glycation end products (RAGE) [22,23]. The TLR- or RAGE-mediated signal transduction pathways result in up-regulation of a wide range of proinflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-1b, and IL-6 [24,25].
The most familiar S100 protein is S100A8/A9, also known as myeloid-related protein (MRP)-8/MRP-14, calprotectin, the L1 protein [14] or calgranulin A and B [26]. The human S100A8 protein is comprised of 93 amino acids and has a molecular weight of 10.8 kDa. The human S100A9 protein consists of 114 amino acids with a molecular weight of 13.2 kDa [26]. Expression of these S100 proteins in monocytes and macrophages is restricted to early differentiation stages and declines rapidly during maturation. The preferred form for human S100A8 and S100A9 is the S100A8/S100A9 heterodimer [17]. The S100A8/A9 protein is released during the activation and turnover of leukocytes [27] and highly up-regulated in various autoimmune disorders [28]. In RA, levels of S100A8/A9 are increased locally at sites of inflammation, such as in the synovial fluid (SF) [26,29] and synovial tissue, as well as in the circulation [30]. Moreover, S100A8/A9 levels are strongly associated with disease activity in patients with RA [31].
THE S100A8/A9 PROTEIN: THE MOST ABUNDANT PROTEIN IN RA SYNOVIAL FLUID
The synovium-cartilage junction is a critical zone in the development of RA [32], suggesting that disease-specific proteins may be localized in SF rather than in other biological materials. High S100A8/A9 concentrations have been found in the SF from RA patients, while low concentrations were found in osteoarthritic patients [33]. Proteomic analysis of SF in patients suffering from RA, osteoarthritis (OA), and miscellaneous inflammatory arthritis (MIA) confirmed that S100A8, S100A9 and S100A12, another S100 protein, are the most differentially expressed biomarkers and are overexpressed in RA SF, but not in SF from OA or MIA patients [33]. Although synovial levels of these proteins discriminate RA from OA or MIAs with high sensitivity and specificity, no significant correlation was demonstrated between synovial polymorphonuclear cell concentration and S100A8 and S100A9 levels [33]. This suggests that these biomarkers are produced by neutrophil effusion and by the RA synovial membrane. Moreover, an increase in S100A8 and S100A9 mRNA expression by fibroblast-like synoviocytes (FLS) in a murine model of RA has been reported and both S100A8 and S100A9 proteins were detected in synovial resident cells in the cartilage-pannus junction of RA synovial membranes [34]. In a recent report in Korean patients, S100A8/9 levels in RA SF were significantly increased in comparison with OA SF. Additionally S100A8 induced Th17 cell differentiation through upregulation of IL-6 expression by RA FLS via TLR4/phosphoinositide 3-kinase/nuclear factor-kB, and mitogen-activated protein kinase signaling pathways [35].
THE S100A8/A9 PROTEIN: CORRELATION WITH LABORATORY AND CLINICAL ASSESSMENTS
S100A8/A9 has a molecular weight of only 36.5 kDa [36], and may diffuse from inflamed joints into the blood circulation, where it can be measured in serum. Previously, a significant correlation was found between S100A8/A9 levels in serum and SF [26,37]. The serum concentration of this protein may reflect the amount of local inflammation and thus be related to joint damage in RA. In a cross sectional analysis of 145 RA patients, the serum concentration of S100A8/A9 correlated significantly (p < 0.001) with both laboratory tests for CRP and ESR, as well as clinical examinations including Disease Activity Score for 28 joints (DAS28), 28-swollen joint counts (SJC), and physical global visual analogue scale (Table 1) [37]. Considerably higher S100A8/A9 levels (p < 0.001) were found in rheumatoid factor (RF) positive patients compared with RF negative patients [37].
Table 1.
Spearman's rank correlations between serum levels of S100A8/A9 and other laboratory and clinical assessments
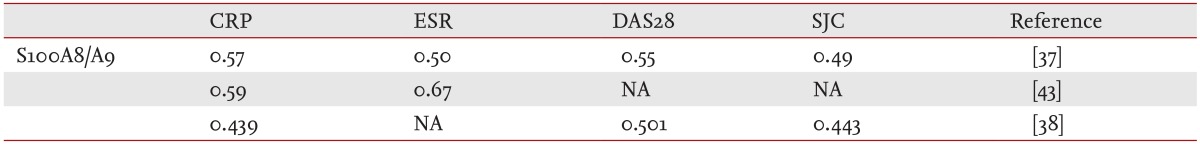
CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; DAS28, Disease Activity Score for 28 joints; SJC, swollen joint counts; NA, not assessed.
In a 10-year follow-up study of patients with RA, strong correlations were found at baseline/follow-up between S100A8/A9 and CRP or ESR [38]. In addition, patients positive for anticyclic citrullinated protein antibodies (anti-CCP), IgA RF, or IgM RF had higher S100A8/A9 levels at baseline and at follow-up than patients who are negative for these serological markers (p < 0.001). Of the inflammatory variables, the magnitude of the regression coefficient for S100A8/A9 was only marginally influenced by addition of CRP, ESR, and anti-CCP, whereas the regression coefficients for CRP and ESR were markedly decreased when S100A8/A9 was added to the linear regression equation [34].
In patients with recent onset disease modifying antirheumatic drug/glucocorticoid (GC)-naïve RA, serum levels of S100A8/9 were significantly elevated compared to those of healthy controls at baseline but were normalized with a significant reduction in disease activity after 3 months of conventional treatment [38]. The levels of S100A8/9 were not affected by different doses of GCs and/or methotrexate. Changes in serum levels of S100A8/9 positively correlated with changes in serum levels of CRP (r = 0.476, p = 0.002), changes in DAS28 (r = 0.390, p = 0.01), and changes in SJC (r = 0.539, p < 0.001). Furthermore, decreases in S100A8/9 rather than CRP levels were associated with improvements in the total number of swollen joints over time (p = 0.001) [38]. This result suggests that decreases in serum S100A8/9 over time can predict improvements in the number of RA affected joints.
In an investigation examining the associations between levels of the inflammatory biomarkers and B-mode/power Doppler (BM/PD) scores from a comprehensive ultrasonography (US) examination over a 12-month period of treatment with adalimumab, significant correlations were found between the levels of S100A8/9 and the US scores [39]. S100A8/9 showed the highest correlation coefficients compared with serum amyloid A (SAA), CRP and ESR and the validity of S100A8/9 as an inflammatory marker was further supported by associations with the clinical evaluation of disease activity. S100A8/9 was also shown to have a higher response to change from biologic treatment than CRP, SAA, or ESR. Regression analyses showed S100A8/A9 was independently associated with both total sum BM and PD scores, even when DAS28 was included in the equation [39]. This finding of associations between S100A8/A9 and the US sum scores suggests that in RA patients a normal S100A8/A9 level may be considered as a marker of clinical remission. Thus, multiple determinations of inflammatory markers, including serum levels of S100A8/A9, can further improve the diagnostic utility of detecting subclinical disease activity in RA patients.
THE S100A8/A9 PROTEIN: CORRELATION WITH RADIOGRAPHIC ASSESSMENT
Radiographic damage is considered a key end-point in clinical studies of RA and is associated with long-term physical disability [40]. Previous studies have shown that acute-phase reactants, RF, and anti-CCP predictED subsequent progression of radiographic damage [40-42], but it has not been possible to develop a clinically useful algorithm for prediction of radiographic progression in early RA.
S100A8/9 has been consistently associated with two measures of joint damage; van der Heijde modified Sharp score and the Rheumatoid Arthritis Articular Damage (RAAD) score [37,43]. After correcting for CRP, ESR, RF, DAS28, gender, and age in a multiple regression analysis, S100A8/9 remained significantly associated with the modified Sharp score (p = 0.018) and RAAD score (p = 0.04). The S100A8/A9 quartiles, which were divided based on the S100A8/A9 concentrations, revealed significant differences (p < 0.001) when they are analyzed based on the modified Sharp and RAAD scores. Of the inflammatory variables, only S100A8/9 was independently associated with joint damage.
The correlation between serum S100A8/A9 and disease progression in the modified Sharp and the RAAD scores was maintained during a 10-year longitudinal study [43]. When the patients were divided into three groups based on baseline levels of S100A8/A9, the SharpProgScore and RAAD score are significantly different between the groups (p < 0.001). Among the inflammatory variables, only baseline S100A8/9 level remained significantly associated with the SharpProgScore (p = 0.045) and RAAD score (p = 0.012) in multiple linear regression analyses with adjustments for baseline levels of CRP, ESR, and anti-CCP, as well as gender, age, and disease duration. Neither CRP nor ESR had significant associations with the two outcome variables for joint damage in corresponding analyses. Importantly, S100A8/9 remained an independent predictor of joint damage in multivariate analyses adjusted for anti-CCP levels [37].
S100A8/A9 AS A COMPONENT OF THE MBDA TEST FOR RHEUMATOID ARTHRITIS
Several studies in RA patients have shown improved outcomes with tight control of disease activity, a strategy employing frequent disease activity measurement and treatment adjustment to reach a specific target disease activity level [44-46]. Treat to target guidelines codified these results into specific recommendations for optimal care including frequent disease activity monitoring for all patients [47].
Current recommendations for treatment of RA advise measuring disease activity as frequently as monthly for patients with moderate to high disease activity, and less frequently every 3 to 6 months for patients with sustained low disease activity or remission [47]. Measurements of disease activity in the clinic may include symptom assessment, joint counts, CRP, ESR, or some combination of these, indexed as a disease activity score based on DAS28, Clinical Disease Activity Index, Simplified Disease Activity Index, or Routine Assessment of Patient Index Data [48,49]. These clinical assessments depend upon patient and/or physician judgments and are subject to intra-assessor and interassessor variability [50,51], whereas laboratory tests-such as ESR and CRP-are general measures of inflammation that can be normal in ~40% of RA patients [52].
Recent advances in biomarker analysis have enabled the development of MBDA tests, which are impacting patient care and outcomes in various therapeutic areas. Tests based on serum protein levels have been introduced for RA and application in RA. An MBDA test measuring serum levels of 12 proteins has proven useful in assessment of RA disease activity [11,53].
The MBDA score was calculated using the concentration of 12 biomarkers (SAA, IL-6, TNF-RI, vascular endothelial growth factor A, matrix metalloproteinase 1 [MMP-1], cartilage glycoprotein 39 [YKL-40], MMP-3, epidermal growth factor, vascular cell adhesion molecule 1, leptin, resistin and CRP). MBDA scores were consistently associated with clinical activity levels, such as SJC, tender joint counts, DAS28-CRP [11,53]. This score using biomarker levels may enable objective measurements of the disease processes underlying RA. However, this MBDA test was not predictive for radiographic progression [11].
Although S100A8/A9 was not included in the present MBDA scores, it has potential as a biomarker. As mentioned above, S100A8/A9 was strongly correlated with clinical disease activity, as well as radiographic assessment. Serum levels of S100A8/A9 have been shown to be a reliable biomarker of diagnosis and prognosis for RA [37]. Further prospective studies are needed to identify the optimal use of a new MBDA score including S100A8/A9 in the management of RA.
CONCLUSIONS
S100A8/A9 is the most enriched protein in RA SF and was correlated significantly and independently with laboratory and clinical assessments of synovial inflammation, as well as radiographic and clinical assessments of joint damage. The validity of S100A8/9 as a biomarker is different from other acute phase proteins since S100A8/9 is released from activated leucocytes in the inflamed synovium, thus directly reflecting the leukocyte levels in inflamed joints of RA patients. In clinical practice, some patients have normal or low levels of CRP and ESR despite extensive arthritis. Therefore, S100A8/9 could be a useful inflammatory marker in these patients.
In a recent long-term follow-up study [43], baseline S100A8/9 levels remained an independent predictor of clinical and radiographic joint damage after 10 years, indicating that S100A8/A9 may be a suitable prognostic biomarker for erosive disease in patients with RA. S100A8/A9 was also associated with the sum scores from a comprehensive US assessment and was responsive to change during anti-TNF treatment [39]. Thus, examination of this leukocyte protein could be of additional value in the assessment of RA patients on biologic treatment. A recent study of patients with juvenile idiopathic arthritis in remission shows that the level of S100A8/A9 was associated with risk of relapse after discontinuing methotrexate [54], adding more value to S100A8/A9 as a predictive biomarker. Furthermore, S100A8/A9 was a sensitive biomarker in cryopyrin-associated periodic syndromes, identifying patients who need to adjust their therapy or should be switched to other drugs [55].
Validation criteria for biomarkers need to be developed in a larger cohort of patients to address structural damage outcomes, assay reproducibility, and reliability. In addition, further longitudinal studies employing a large population of RA patients without destructive disease are required to address whether S100A8/9 levels improve the prediction of long-term joint damage in a highly sensitive and reliable manner in patients with RA. Determination of S100A8/A9 level, in addition to levels of existing inflammatory markers, can assist in the detection of subclinical and residual disease activity and could be valuable in adjusting individual treatment in RA patients.
Acknowledgments
This study was supported by a grant from the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI09C1555).
Footnotes
No potential conflict of interest relevant to this article is reported.
References
- 1.Andersson AK, Li C, Brennan FM. Recent developments in the immunobiology of rheumatoid arthritis. Arthritis Res Ther. 2008;10:204. doi: 10.1186/ar2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huber LC, Distler O, Tarner I, Gay RE, Gay S, Pap T. Synovial fibroblasts: key players in rheumatoid arthritis. Rheumatology (Oxford) 2006;45:669–675. doi: 10.1093/rheumatology/kel065. [DOI] [PubMed] [Google Scholar]
- 3.McInnes IB, Schett G. Cytokines in the pathogenesis of rheumatoid arthritis. Nat Rev Immunol. 2007;7:429–442. doi: 10.1038/nri2094. [DOI] [PubMed] [Google Scholar]
- 4.Park SH. New diagnostic method of rheumatoid arthritis. Korean J Med. 2009;76:7–11. [Google Scholar]
- 5.Park SH. Guideline for treatment or rheumatoid arthritis. Korean J Med. 2010;79:s455–s458. [Google Scholar]
- 6.Leclerc E, Fritz G, Vetter SW, Heizmann CW. Binding of S100 proteins to RAGE: an update. Biochim Biophys Acta. 2009;1793:993–1007. doi: 10.1016/j.bbamcr.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Vogl T, Tenbrock K, Ludwig S, et al. Mrp8 and Mrp14 are endogenous activators of Toll-like receptor 4, promoting lethal, endotoxin-induced shock. Nat Med. 2007;13:1042–1049. doi: 10.1038/nm1638. [DOI] [PubMed] [Google Scholar]
- 8.Berntzen HB, Munthe E, Fagerhol MK. A longitudinal study of the leukocyte protein L1 as an indicator of disease activity in patients with rheumatoid arthritis. J Rheumatol. 1989;16:1416–1420. [PubMed] [Google Scholar]
- 9.Brun JG, Haga HJ, Boe E, et al. Calprotectin in patients with rheumatoid arthritis: relation to clinical and laboratory variables of disease activity. J Rheumatol. 1992;19:859–862. [PubMed] [Google Scholar]
- 10.Brun JG, Jonsson R, Haga HJ. Measurement of plasma calprotectin as an indicator of arthritis and disease activity in patients with inflammatory rheumatic diseases. J Rheumatol. 1994;21:733–738. [PubMed] [Google Scholar]
- 11.Bakker MF, Cavet G, Jacobs JW, et al. Performance of a multi-biomarker score measuring rheumatoid arthritis disease activity in the CAMERA tight control study. Ann Rheum Dis. 2012;71:1692–1697. doi: 10.1136/annrheumdis-2011-200963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dale I, Brandtzaeg P, Fagerhol MK, Scott H. Distribution of a new myelomonocytic antigen (L1) in human peripheral blood leukocytes: immunofluorescence and immunoperoxidase staining features in comparison with lysozyme and lactoferrin. Am J Clin Pathol. 1985;84:24–34. doi: 10.1093/ajcp/84.1.24. [DOI] [PubMed] [Google Scholar]
- 13.Foell D, Roth J. Proinflammatory S100 proteins in arthritis and autoimmune disease. Arthritis Rheum. 2004;50:3762–3771. doi: 10.1002/art.20631. [DOI] [PubMed] [Google Scholar]
- 14.Fagerhol MK, Dale I, Andersson T. A radioimmunoassay for a granulocyte protein as a marker in studies on the turnover of such cells. Bull Eur Physiopathol Respir. 1980;16(Suppl):273–282. doi: 10.1016/b978-0-08-027379-2.50028-4. [DOI] [PubMed] [Google Scholar]
- 15.Edgeworth J, Gorman M, Bennett R, Freemont P, Hogg N. Identification of p8,14 as a highly abundant heterodimeric calcium binding protein complex of myeloid cells. J Biol Chem. 1991;266:7706–7713. [PubMed] [Google Scholar]
- 16.Wolf R, Howard OM, Dong HF, et al. Chemotactic activity of S100A7 (Psoriasin) is mediated by the receptor for advanced glycation end products and potentiates inflammation with highly homologous but functionally distinct S100A15. J Immunol. 2008;181:1499–1506. doi: 10.4049/jimmunol.181.2.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ehrchen JM, Sunderkotter C, Foell D, Vogl T, Roth J. The endogenous Toll-like receptor 4 agonist S100A8/S100A9 (calprotectin) as innate amplifier of infection, autoimmunity, and cancer. J Leukoc Biol. 2009;86:557–566. doi: 10.1189/jlb.1008647. [DOI] [PubMed] [Google Scholar]
- 18.Bianchi ME. DAMPs, PAMPs and alarmins: all we need to know about danger. J Leukoc Biol. 2007;81:1–5. doi: 10.1189/jlb.0306164. [DOI] [PubMed] [Google Scholar]
- 19.Foell D, Wittkowski H, Vogl T, Roth J. S100 proteins expressed in phagocytes: a novel group of damage-associated molecular pattern molecules. J Leukoc Biol. 2007;81:28–37. doi: 10.1189/jlb.0306170. [DOI] [PubMed] [Google Scholar]
- 20.Foell D, Wittkowski H, Roth J. Mechanisms of disease: a 'DAMP' view of inflammatory arthritis. Nat Clin Pract Rheumatol. 2007;3:382–390. doi: 10.1038/ncprheum0531. [DOI] [PubMed] [Google Scholar]
- 21.Rammes A, Roth J, Goebeler M, Klempt M, Hartmann M, Sorg C. Myeloid-related protein (MRP) 8 and MRP14, calcium-binding proteins of the S100 family, are secreted by activated monocytes via a novel, tubulin-dependent pathway. J Biol Chem. 1997;272:9496–9502. doi: 10.1074/jbc.272.14.9496. [DOI] [PubMed] [Google Scholar]
- 22.Ghavami S, Rashedi I, Dattilo BM, et al. S100A8/A9 at low concentration promotes tumor cell growth via RAGE ligation and MAP kinase-dependent pathway. J Leukoc Biol. 2008;83:1484–1492. doi: 10.1189/jlb.0607397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tamaki Y, Takakubo Y, Hirayama T, et al. Expression of Toll-like receptors and their signaling pathways in rheumatoid synovitis. J Rheumatol. 2011;38:810–820. doi: 10.3899/jrheum.100732. [DOI] [PubMed] [Google Scholar]
- 24.Malemud CJ. Myeloid-related protein activity in rheumatoid arthritis. Int J Inflam. 2011;2011:580295. doi: 10.4061/2011/580295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goh FG, Midwood KS. Intrinsic danger: activation of Toll-like receptors in rheumatoid arthritis. Rheumatology (Oxford) 2012;51:7–23. doi: 10.1093/rheumatology/ker257. [DOI] [PubMed] [Google Scholar]
- 26.Frosch M, Strey A, Vogl T, et al. Myeloid-related proteins 8 and 14 are specifically secreted during interaction of phagocytes and activated endothelium and are useful markers for monitoring disease activity in pauciarticular-onset juvenile rheumatoid arthritis. Arthritis Rheum. 2000;43:628–637. doi: 10.1002/1529-0131(200003)43:3<628::AID-ANR20>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 27.Johne B, Fagerhol MK, Lyberg T, et al. Functional and clinical aspects of the myelomonocyte protein calprotectin. Mol Pathol. 1997;50:113–123. doi: 10.1136/mp.50.3.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loser K, Vogl T, Voskort M, et al. The Toll-like receptor 4 ligands Mrp8 and Mrp14 are crucial in the development of autoreactive CD8+ T cells. Nat Med. 2010;16:713–717. doi: 10.1038/nm.2150. [DOI] [PubMed] [Google Scholar]
- 29.Liao H, Wu J, Kuhn E, et al. Use of mass spectrometry to identify protein biomarkers of disease severity in the synovial fluid and serum of patients with rheumatoid arthritis. Arthritis Rheum. 2004;50:3792–3803. doi: 10.1002/art.20720. [DOI] [PubMed] [Google Scholar]
- 30.Sunahori K, Yamamura M, Yamana J, et al. The S100A8/A9 heterodimer amplifies proinflammatory cytokine production by macrophages via activation of nuclear factor kappa B and p38 mitogen-activated protein kinase in rheumatoid arthritis. Arthritis Res Ther. 2006;8:R69. doi: 10.1186/ar1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hammer HB, Haavardsholm EA, Kvien TK. Calprotectin (a major leucocyte protein) is associated with the levels of anti-CCP and rheumatoid factor in a longitudinal study of patients with very early rheumatoid arthritis. Scand J Rheumatol. 2008;37:179–182. doi: 10.1080/03009740701874451. [DOI] [PubMed] [Google Scholar]
- 32.Pap T, Muller-Ladner U, Gay RE, Gay S. Fibroblast biology: role of synovial fibroblasts in the pathogenesis of rheumatoid arthritis. Arthritis Res. 2000;2:361–367. doi: 10.1186/ar113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baillet A, Trocme C, Berthier S, et al. Synovial fluid proteomic fingerprint: S100A8, S100A9 and S100A12 proteins discriminate rheumatoid arthritis from other inflammatory joint diseases. Rheumatology (Oxford) 2010;49:671–682. doi: 10.1093/rheumatology/kep452. [DOI] [PubMed] [Google Scholar]
- 34.Youssef P, Roth J, Frosch M, et al. Expression of myeloid related proteins (MRP) 8 and 14 and the MRP8/14 heterodimer in rheumatoid arthritis synovial membrane. J Rheumatol. 1999;26:2523–2528. [PubMed] [Google Scholar]
- 35.Lee DG, Woo JW, Kwok SK, Cho ML, Park SH. MRP8 promotes Th17 differentiation via upregulation of IL-6 production by fibroblast-like synoviocytes in rheumatoid arthritis. Exp Mol Med. 2013;45:e20. doi: 10.1038/emm.2013.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dale I, Fagerhol MK, Naesgaard I. Purification and partial characterization of a highly immunogenic human leukocyte protein, the L1 antigen. Eur J Biochem. 1983;134:1–6. doi: 10.1111/j.1432-1033.1983.tb07522.x. [DOI] [PubMed] [Google Scholar]
- 37.Hammer HB, Odegard S, Fagerhol MK, et al. Calprotectin (a major leucocyte protein) is strongly and independently correlated with joint inflammation and damage in rheumatoid arthritis. Ann Rheum Dis. 2007;66:1093–1097. doi: 10.1136/ard.2006.064741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andres Cerezo L, Mann H, Pecha O, et al. Decreases in serum levels of S100A8/9 (calprotectin) correlate with improvements in total swollen joint count in patients with recent-onset rheumatoid arthritis. Arthritis Res Ther. 2011;13:R122. doi: 10.1186/ar3426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hammer HB, Fagerhol MK, Wien TN, Kvien TK. The soluble biomarker calprotectin (an S100 protein) is associated to ultrasonographic synovitis scores and is sensitive to change in patients with rheumatoid arthritis treated with adalimumab. Arthritis Res Ther. 2011;13:R178. doi: 10.1186/ar3503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Odegard S, Landewe R, van der Heijde D, Kvien TK, Mowinckel P, Uhlig T. Association of early radiographic damage with impaired physical function in rheumatoid arthritis: a ten-year, longitudinal observational study in 238 patients. Arthritis Rheum. 2006;54:68–75. doi: 10.1002/art.21548. [DOI] [PubMed] [Google Scholar]
- 41.Jansen LM, van der Horst-Bruinsma IE, van Schaardenburg D, Bezemer PD, Dijkmans BA. Predictors of radiographic joint damage in patients with early rheumatoid arthritis. Ann Rheum Dis. 2001;60:924–927. doi: 10.1136/ard.60.10.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jansen LM, van Schaardenburg D, van der Horst-Bruinsma I, van der Stadt RJ, de Koning MH, Dijkmans BA. The predictive value of anti-cyclic citrullinated peptide antibodies in early arthritis. J Rheumatol. 2003;30:1691–1695. [PubMed] [Google Scholar]
- 43.Hammer HB, Odegard S, Syversen SW, et al. Calprotectin (a major S100 leucocyte protein) predicts 10-year radiographic progression in patients with rheumatoid arthritis. Ann Rheum Dis. 2010;69:150–154. doi: 10.1136/ard.2008.103739. [DOI] [PubMed] [Google Scholar]
- 44.Mease PJ. Improving the routine management of rheumatoid arthritis: the value of tight control. J Rheumatol. 2010;37:1570–1578. doi: 10.3899/jrheum.091064. [DOI] [PubMed] [Google Scholar]
- 45.Verstappen SM, Jacobs JW, van der Veen MJ, et al. Intensive treatment with methotrexate in early rheumatoid arthritis: aiming for remission: Computer Assisted Management in Early Rheumatoid Arthritis (CAMERA, an open-label strategy trial) Ann Rheum Dis. 2007;66:1443–1449. doi: 10.1136/ard.2007.071092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bakker MF, Jacobs JW, Verstappen SM, Bijlsma JW. Tight control in the treatment of rheumatoid arthritis: efficacy and feasibility. Ann Rheum Dis. 2007;66(Suppl 3):iii56–iii60. doi: 10.1136/ard.2007.078360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smolen JS, Aletaha D, Bijlsma JW, et al. Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis. 2010;69:631–637. doi: 10.1136/ard.2009.123919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Prevoo ML, van't Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–48. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 49.Aletaha D, Smolen JS. The Simplified Disease Activity Index (SDAI) and Clinical Disease Activity Index (CDAI) to monitor patients in standard clinical care. Best Pract Res Clin Rheumatol. 2007;21:663–675. doi: 10.1016/j.berh.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 50.Uhlig T, Kvien TK, Pincus T. Test-retest reliability of disease activity core set measures and indices in rheumatoid arthritis. Ann Rheum Dis. 2009;68:972–975. doi: 10.1136/ard.2008.097345. [DOI] [PubMed] [Google Scholar]
- 51.Thompson PW, Hart LE, Goldsmith CH, Spector TD, Bell MJ, Ramsden MF. Comparison of four articular indices for use in clinical trials in rheumatoid arthritis: patient, order and observer variation. J Rheumatol. 1991;18:661–665. [PubMed] [Google Scholar]
- 52.Pincus T. The American College of Rheumatology (ACR) core data set and derivative "patient only" indices to assess rheumatoid arthritis. Clin Exp Rheumatol. 2005;23(5 Suppl 39):S109–S113. [PubMed] [Google Scholar]
- 53.Centola M, Cavet G, Shen Y, et al. Development of a multi-biomarker disease activity test for rheumatoid arthritis. PLoS One. 2013;8:e60635. doi: 10.1371/journal.pone.0060635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Foell D, Wulffraat N, Wedderburn LR, et al. Methotrexate withdrawal at 6 vs 12 months in juvenile idiopathic arthritis in remission: a randomized clinical trial. JAMA. 2010;303:1266–1273. doi: 10.1001/jama.2010.375. [DOI] [PubMed] [Google Scholar]
- 55.Wittkowski H, Kuemmerle-Deschner JB, Austermann J, et al. MRP8 and MRP14, phagocyte-specific danger signals, are sensitive biomarkers of disease activity in cryopyrin-associated periodic syndromes. Ann Rheum Dis. 2011;70:2075–2081. doi: 10.1136/ard.2011.152496. [DOI] [PMC free article] [PubMed] [Google Scholar]


