Abstract
Background
Family accommodation has been studied in obsessive compulsive disorder using the Family Accommodation Scale (FAS) and predicts greater symptom severity, more impairment, and poorer treatment outcomes. However, family accommodation has yet to be systematically studied among families of children with other anxiety disorders. We developed the Family Accommodation Scale—Anxiety (FASA) that includes modified questions from the FAS to study accommodation across childhood anxiety disorders. The objectives of this study were to report on the first study of family accommodation across childhood anxiety disorders and to test the utility of the FASA for assessing the phenomenon.
Methods
Participants were parents (n = 75) of anxious children from two anxiety disorder specialty clinics (n = 50) and a general outpatient clinic (n = 25). Measures included FASA, structured diagnostic interviews, and measures of anxiety and depression.
Results
Accommodation was highly prevalent across all anxiety disorders and particularly associated with separation anxiety. Most parents reported participation in symptoms and modification of family routines as well as distress resulting from accommodation and undesirable consequences of not accommodating. The FASA displayed good internal consistency and convergent and divergent validity. Accommodation correlated significantly with anxious but not depressive symptoms, when controlling for the association between anxiety and depression. Factor analysis of the FASA pointed to a two-factor solution; one relating to modifications, the other to participation in symptoms.
Conclusions
Accommodation is common across childhood anxiety disorders and associated with severity of anxiety symptoms. The FASA shows promise as a means of assessing family accommodation in childhood anxiety disorders.
Keywords: family accommodation, anxiety disorders, family members, treatment outcomes, obsessive compulsive disorder, cognitive behavioral therapy
INTRODUCTION
Family accommodation describes the ways in which family members, particularly parents, change their behavior so as to help a relative to diminish or avoid the distress caused by a disorder.[1] Family accommodation has been extensively studied in obsessive compulsive disorder (OCD), and has been found to be an important variable for both clinical course and treatment outcomes.[2] However, we know of no systematic reports of the phenomenon in other anxiety disorders, outside of OCD. In this article, we briefly review findings regarding accommodation in OCD and present a first study of accommodation in other childhood anxiety disorders, as well as a tool for assessing the phenomenon among parents of anxious children.
ACCOMMODATION IN OCD
In OCD, family accommodation describes modifications to parental behaviors[1, 3] such as participation in rituals, providing reassurance, and assisting a child in avoiding situations that trigger symptoms. In some cases, accommodation may be forcefully imposed by the child, who reacts to attempts to reduce accommodation with coercive and disruptive behaviors that can be quite extreme.[4, 5] The Family Accommodation Scale (FAS)[3] was developed to systematically assess accommodation among the relatives of individuals with OCD and has been increasingly used in studies of both children and adults.[2, 6–9] The FAS is an interviewer-administered tool, but a modified version of the scale, with truncated items, has also been used repeatedly as a self-report measure.[8, 10–12] Overall, the FAS has good internal consistency, discriminant validity, and high interrater reliability.[3, 12, 13]
Studies of accommodation in pediatric OCD have reported high frequency of accommodating behaviors.[13] Accommodation has been linked to the degree of symptom severity and impairment, as well as to treatment outcomes.[6, 7, 10, 11] Higher rates of family accommodation before treatment are associated with less therapeutic gains and more refractoriness, and successful treatment is associated with reduced accommodation.[10, 14–16] An analysis of data from the largest and most systematic trial of OCD treatment in childhood[17] found that family accommodation was one of only five variables that predicted treatment outcomes.[18] Despite this emerging knowledge base, accommodation has rarely been considered in relation to other anxiety disorders.
FAMILY ACCOMMODATION IN ANXIETY DISORDERS
Anxiety disorders are the most common psychiatric problems of childhood.[19] That anxiety in children will generally trigger behaviors that are oriented toward caretakers has long been recognized,[20] and attachment behaviors are generally accepted to be part of the anxious response across mammalian species. Various systemic approaches have described the interpersonal nature of anxiety disorders and the role of a number of family factors has been investigated, including attachment, rearing strategies, and intrafamily conflict.[21–23] The value of involving family members in treatment[24] has also been studied, with mixed results. Some early studies showed an increase in treatment response when a parent component was added to the child’s treatment.[25, 26] Other studies have not supported the added benefit of parental involvement.[27] However, no systematic study of accommodation has as yet been undertaken among families of children with anxiety disorders.
Accommodation in anxiety disorders can take many forms, both similar and different from what is seen in OCD. For example, a child with separation anxiety disorder may require his parents to sleep next to him or to respond to multiple phone calls; one with social phobia may have her parents speak in her place; phobias can cause parents to avoid situations, or even words, that trigger fear; a child with generalized anxiety may seek constant reassurance; or a child with panic symptoms may rely on an adult’s accompaniment. Some accommodation is likely inevitable, and may be the natural expression of empathy for a child’s distress. But, as the findings above suggest, greater accommodation can have negative implications for the course of the disorder and for treatment outcomes.
One reason that accommodation has not been studied systematically in anxiety disorders may be the absence of measures designed for this purpose. However, among children with OCD, family accommodation has been tied with overall anxiety as well as with OCD symptom severity.[7] The goal of the present study was twofold: First, to report on the degree of accommodation reported by parents of anxious children and examine the relation of accommodation to severity of anxiety and depressive symptoms. Second, to test the usability and preliminary psychometric properties of the Family Accommodation Scale—Anxiety (FASA). FASA is an adaptation of the items from the FAS, modified with the authors’ permission for use in all anxiety disorders. To better understand the role of accommodation, we chose to include a comparison sample of children not seen specifically for anxiety disorders, who displayed significant symptoms of anxiety within the context of other problems.
MATERIALS AND METHODS
PARTICIPANTS
Parents of school age children were recruited for the study in three locations: two anxiety disorders specialty clinics (one in the United States N = 29; and one in Israel N = 21) and one general outpatient clinic (in the United States) that serves a diverse population (N = 25).
Participants in the specialty clinics were recruited based on meeting DSM IV TR criteria for a presenting complaint of at least one anxiety disorder. Participants who presented with OCD were excluded from the study. Participants in the general outpatient clinic were recruited based on elevated anxiety symptoms reported at intake, defined as a score above 23 on parent-report Screen for Child Anxiety Related Emotional Disorders (SCARED).[28] Recruiting a sample of children from a nonspecialty clinic allowed for a broader view of accommodation in children experiencing elevated symptoms of anxiety. We report on comparisons between the specialty clinic and general clinic samples. Table 1 summarizes the demographic and clinical characteristic of the sample.
TABLE 1.
Demographic and clinical data for the total sample (n = 75) and by specialty (n = 50) versus general outpatient (n = 25) clinic
| Total (N = 75) | Anxiety specialty clinics (N = 50) | General outpatient clinic (N = 25) | |
|---|---|---|---|
| Age: mean (SD) | 10.65 (2.78) | 10.86 (2.57) | 10.24 (3.18) |
| Males: N (%) | 46 (61.3) | 32 (64) | 14 (56) |
| SES* | 3.28 (1.01) | 3.82 (0.66) | 2.2 (0.2) |
| SCARED | |||
| Mean (SD) | |||
| Total** | 33 (13.9) | 30.2 (14.36) | 38.6 (11.23) |
| Somatic symptoms** | 7 (5.26) | 6 (4.98) | 9 (5.33) |
| Generalized anxiety** | 9 (4.27) | 8.3 (4.32) | 10.6 (3.84) |
| Separation anxiety** | 7.9 (4.29) | 7.2 (4.43) | 9.3 (3.68) |
| Social anxiety | 6.4 (3.86) | 5.8 (3.6) | 7.6 (4.16) |
| School anxiety | 3.1 (2.3) | 2.7 (2.26) | 3.8 (2.26) |
| FASA | |||
| Mean (SD) | |||
| Total | 14.5 (8.92) | 13.24 (8.84) | 17.08 (8.71) |
| Participation | 9.3 (5.26) | 8.5 (5.17) | 10.8 (5.23) |
| Modification | 5.2 (4.9) | 4.7 (5.07) | 6.2 (4.73) |
| Distress: mean (SD) | 1.7 (1.4) | 1.7 (1.4) | 1.6 (1.44) |
| Consequences: mean (SD) | 5.5 (3.93) | 5.3 (3.98) | 5.7 (3.88) |
| MFQ:* mean (SD) | 20.7 (13.02) | 16 (10.36) | 29.7 (13) |
SES was determined on a 5-point scale based on parental income and education.
SCARED, Screen for Child Anxiety Related Emotional Disorder (and subscales); FASA, Family Accommodation Scale—Anxiety (and subscales); MFQ, Mood and Feelings Questionnaire.
Difference significant at the p < .001 level;
Difference significant at the p < .05 level.
Evaluations and diagnoses were made by experienced clinicians with expertise in anxiety. Patients participated in an in-depth expert evaluation, and diagnoses were agreed upon in team meetings led by senior clinicians. Structured interviews were administered by qualified and trained interviewers, blind to the research goals and to any previous clinical evaluations of the patient. Written measures were administered in the clinical setting, in the presence of the interviewer. Participants gave signed informed consent and the study was approved by the respective institutional review boards.
One parent (or other primary caretaker) completed the assessments for each child. The majority of informants were mothers (74.7%), followed by fathers (21.3%) and other primary-caretaker relatives (4%).
MEASURES
Family Accommodation Scale—Anxiety (FASA)
A pilot version of the FAS[1] and the finalized instrument[3] were developed for use with relatives of individuals with OCD. With the author’s permission, we adapted those instruments to create an accommodation scale for use with other anxiety disorders. Reworded versions of the nine accommodation items from the pilot FAS[1] were used for our self-report version of the instrument. Whereas on the pilot FAS three of these items were clinician scored using a scale from “No” to “Extreme,” we coded all nine items on a 5-point Likert-type scale from 0 (Never) to 4 (Daily), to better fit parental self-report. Table 2 presents the items on the FASA and the distribution of responses to each item.
TABLE 2.
FASA items and parents’ responses to them for the total sample (n = 75) and by specialty (n = 50) versus general outpatient (n = 25) clinic
| Item | Family Accommodation Scale – Anxiety (FASA) Participation in symptom-related behaviors during the past month |
Total (N = 75)
|
Specialty clinic (N = 50)
|
General outpatient clinic (N = 25)
|
|||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| 1 | How often did you reassure your child? | ||||||
| Never | 4 | 5.3 | 4 | 8.0 | 0 | 0 | |
| 1–3 times a month | 6 | 8 | 3 | 6.0 | 3 | 12.0 | |
| 1–2 times a week | 14 | 18.7 | 10 | 20.0 | 4 | 16.0 | |
| 3–6 times a week | 17 | 22.7 | 12 | 24.0 | 5 | 20.0 | |
| Daily | 34 | 45.3 | 21 | 42.0 | 13 | 52.0 | |
| 2 | How often did you provide items needed because of anxiety? | ||||||
| Never | 41 | 54.7 | 33 | 66.0 | 8 | 32.0 | |
| 1–3 times a month | 5 | 6.7 | 2 | 4.0 | 3 | 12.0 | |
| 1–2 times a week | 6 | 8 | 3 | 6.0 | 3 | 12.0 | |
| 3–6 times a week | 7 | 9.3 | 4 | 8.0 | 3 | 12.0 | |
| Daily | 16 | 21.3 | 8 | 16.0 | 8 | 32.0 | |
| 3 | How often did you participate in behaviors related to your child’s anxiety? | ||||||
| Never | 22 | 29.3 | 12 | 24.0 | 10 | 40.0 | |
| 1–3 times a month | 8 | 10.7 | 6 | 12.0 | 2 | 8.0 | |
| 1–2 times a week | 12 | 16 | 8 | 16.0 | 4 | 16.0 | |
| 3–6 times a week | 10 | 13.3 | 8 | 16.0 | 2 | 8.0 | |
| Daily | 23 | 30.7 | 16 | 32.0 | 7 | 28.0 | |
| 4 | How often did you assist your child in avoiding things that might make him/her more anxious? | ||||||
| Never | 25 | 33.3 | 21 | 42.0 | 4 | 16.0 | |
| 1–3 times a month | 10 | 13.3 | 7 | 14.0 | 3 | 12.0 | |
| 1–2 times a week | 13 | 17.3 | 7 | 14.0 | 6 | 24.0 | |
| 3–6 times a week | 13 | 17.3 | 8 | 16.0 | 5 | 20.0 | |
| Daily | 14 | 18.7 | 7 | 14.0 | 7 | 28.0 | |
| 5 | Have you avoided doing things, going places, or being with people because of your child’s anxiety? | ||||||
| Never | 38 | 50.7 | 29 | 58.0 | 9 | 36.0 | |
| 1–3 times a month | 10 | 13.3 | 7 | 14.0 | 3 | 12.0 | |
| 1–2 times a week | 10 | 13.3 | 5 | 10.0 | 5 | 20.0 | |
| 3–6 times a week | 9 | 12 | 4 | 8.0 | 5 | 20.0 | |
| Daily | 8 | 10.7 | 5 | 10.0 | 3 | 12.0 | |
| Modification of functioning during the past month | |||||||
| 6 | Have you modified your family routine because of your child’s symptoms? | ||||||
| Never | 28 | 37.3 | 22 | 44.0 | 6 | 24.0 | |
| 1–3 times a month | 10 | 13.3 | 5 | 10.0 | 5 | 20.0 | |
| 1–2 times a week | 19 | 25.3 | 10 | 20.0 | 9 | 36.0 | |
| 3–6 times a week | 8 | 10.7 | 5 | 10.0 | 3 | 12.0 | |
| Daily | 10 | 13.3 | 8 | 16.0 | 2 | 8.0 | |
| 7 | Have you had to do some things that would usually be your child’s responsibility? | ||||||
| Never | 29 | 38.7 | 25 | 50.0 | 4 | 16.0 | |
| 1–3 times a month | 12 | 16.0 | 7 | 14.0 | 5 | 20.0 | |
| 1–2 times a week | 18 | 24.0 | 9 | 18.0 | 9 | 36.0 | |
| 3–6 times a week | 11 | 14.7 | 7 | 14.0 | 4 | 16.0 | |
| Daily | 5 | 6.7 | 2 | 4.0 | 3 | 12.0 | |
| 8 | Have you modified your work schedule because of your child’s anxiety? | ||||||
| Never | 46 | 61.3 | 31 | 62.0 | 15 | 60 | |
| 1–3 times a month | 5 | 6.7 | 5 | 10.0 | 0 | 0 | |
| 1–2 times a week | 9 | 12.0 | 5 | 10.0 | 4 | 16.0 | |
| 3–6 times a week | 3 | 4.0 | 2 | 4.0 | 1 | 4.0 | |
| Daily | 12 | 16.0 | 7 | 14.0 | 5 | 20.0 | |
| 9 | Have you modified your leisure activities because your child’s anxiety? | ||||||
| Never | 36 | 48.0 | 28 | 56.0 | 8 | 32.0 | |
| 1–3 times a month | 8 | 10.7 | 3 | 6.0 | 5 | 20.0 | |
| 1–2 times a week | 14 | 18.7 | 8 | 16.0 | 6 | 24.0 | |
| 3–6 times a week | 5 | 6.7 | 3 | 6.0 | 2 | 8.0 | |
| Daily | 12 | 16.0 | 8 | 16.0 | 4 | 16.0 | |
Following the pilot version of FAS, we also administered one item that queries parental distress associated with the accommodation (Does helping your child in these ways cause you distress?) and three items that assess the consequences of not accommodating (Has your child become distressed/anxious when you have not provided assistance?; Has your child become angry/abusive when you have not provided assistance?; Has your child’s anxiety been worse when you have not provided assistance?).
Screen for Child Anxiety Related Emotional Disorders (SCARED)[28]
SCARED is a 41-item measure of childhood anxiety, that provides five factors including somatic, generalized, separation, school, and social anxiety as well as an overall total score.
Anxiety Disorders Interview Schedule For DSM-IV (ADIS)[29]
ADIS is a semistructured diagnostic interview that may be administered to a parent. It has been found to be a reliable and valid measure of anxiety disorders in youth.[30] The ADIS was administered to participants in the anxiety disorders specialty clinics, but not the general outpatient clinic.
Mood and Feelings Questionnaire (MFQ)[31]
MFQ is a 34-item scale consisting of phrases descriptive of symptoms of depression.
DATA ANALYSIS
For each item on the FASA, we report on the percentage of parents who endorsed each possible answer and provide means and standard deviations for the total FASA scores as well as for the accommodation, distress, and consequences item-groups. Results are presented for the anxiety clinics and the general outpatient clinic as well as for the total sample combined. Internal consistency on the FASA is assessed using Cronbach’s α. Divergent and convergent validity are examined using the relation of the FASA to the measures of anxiety and depressive symptoms. Multiple regression is used to probe the relation of accommodation to specific disorders or domains of anxiety and we use rotated principal axis factor analysis to explore the factorial structure of the FASA.
RESULTS
Table 1 summarizes the characteristics of the sample (N = 75) according to their clinic of origin. Only 40% of children met criteria for a single anxiety disorder diagnosis, 26% percent met criteria for two diagnoses, and 34% fit at least three anxiety disorder diagnoses. The most common anxiety disorder was generalized anxiety disorder (68%), followed by separation anxiety and specific phobias (38%), social phobia (22%), and panic disorder with or without agoraphobia (10%). Among children presenting at the general outpatient clinic, 64% met criteria for two diagnoses and the most common diagnoses were adjustment disorders (36%), anxiety disorder not otherwise specified (28%), disruptive behavior disorders (24%), attention deficit hyperactivity disorder (20%), and mood disorders (12%). Comparisons of the two anxiety disorder specialty clinic samples did not reveal significant differences in the prevalence of disorders (χ2 values ranged from <0.1 to 1.9, all p values were >.1), level of accommodation (t(48) = 0.8, p = .42), severity of anxiety symptoms (t(48) = 0.54, p = .59), or age of the children (t(48) = 0.65, p = .51). Therefore, the two specialty clinic samples are combined for the purpose of data analysis. Overall level of anxiety symptoms as measured by SCARED, was higher in the general outpatient sample. However this is most likely an artifact of including only children whose total score was at least 23. Within the anxiety specialty clinic sample, 62% of children met this criterion, and their reported level of accommodation was significantly higher (t(48) = 3.7, p < .01) compared to those whose SCARED scores were below 23. No significant differences were found between specialty and general outpatient samples in age (t(73) = 0.9, p = .37), gender (χ2(1) = 0.4, p = .5), or the level of accommodation reported (t(73) = 1.8, p = .08). Depressive symptoms were significantly higher in the general outpatient clinic sample (t(73) = 4.9, p < .01). Socioeconomic situation (SES), based on highest parent education and income bracket, was lower in the general outpatient sample (t(73) = 7.3, p < .01).
PREVALENCE OF FAMILY ACCOMMODATION
Virtually all parents (97.3%) endorsed at least some level of family accommodation and most (76%) reported both participation in symptoms and modification of the family’s routines, due to the anxiety. Most parents also reported experiencing distress resulting from accommodation (70.7%), and negative consequences of not accommodating the child’s symptoms (85.3%). Among the negative consequences, exacerbation of the child’s anxiety and distress were most common (73.3%). But the child becoming angry or abusive was also frequently reported (56%). Table 1 summarizes mean scores on the FASA and subscales. Children seen in the specialty anxiety clinics did not differ significantly from anxious children seen in the general outpatient clinic on level of accommodation or specific elements of accommodation, distress, or negative consequences.
Family accommodation was not associated with the age of the anxious child, but child gender was associated with accommodation in the specialty clinic sample, such that parents of girls reported more accommodation than parents of boys (t(48) = 3.14, p < .01). SES was not associated with accommodation. However in the general outpatient sample, there was a moderate trend toward a positive correlation that approached statistical significance (r(23) = .39, p = .054).
To test the relation of specific anxiety disorder diagnoses with the degree of reported accommodation, we conducted a stepwise multiple regression analysis using dichotomous variables, representing the presence or absence of each diagnosis, as predictors. A significant model emerged (F(1,48) = 11.2, p < .01) which explained 17.3% of accommodation variance. Only the presence of separation anxiety disorder was a significant variable (β = 0.435, p < .01). However, total number of diagnoses was significantly correlated with the degree of accommodation (r(48) = .299, p < .05).
Stepwise regression analysis for the relation of SCARED subscales to degree of accommodation, produced a significant model (F(2,72) = 17.4, p < .001) that explained 30.7% of variance. Significant variables included the school anxiety subscale (β = 0.356, p < .01) and generalized anxiety subscale (β = 0.317, p < .01). Multicollinearity between these variables was low, as indicated by tolerance level of 0.81 (VIF = 1.234).
INTERNAL CONSISTENCY
The nine FASA accommodation items displayed high internal consistency in the entire sample, as well as for each locus. Cronbach’s α values were 0.90 and 0.91 for the specialty and general clinics, respectively. Deletion of any one item did not significantly impact α.
FACTORIAL STRUCTURE
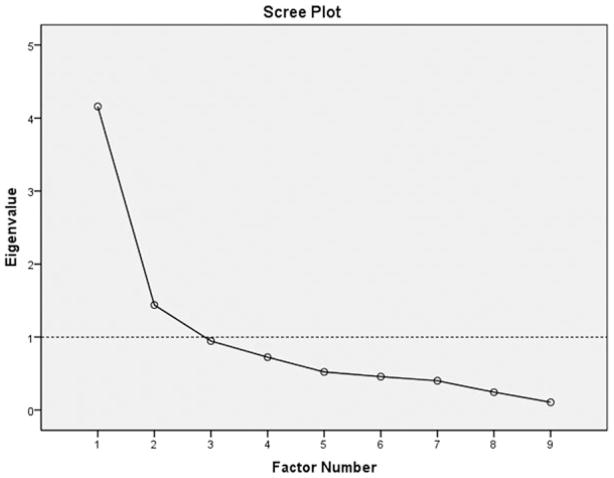
Exploratory factor analysis was employed as this is the first test of the FASA, and because of sample size considerations. To account for potential correlations between factors, rotated principal axis factor analysis (Promax rotations) was conducted on the nine FASA accommodation items. Following Hayton et al. (2004),[32] parallel analysis was used to determine retention criteria. Fifty random data sets with identical dimensions were generated and the 95th percentile of resulting explained variance was used to determine critical eigenvalues. This method produced a two-factor model, corresponding to the Participation and Modification items. Table 3 summarizes the factor-analytical results. The two-factor model determined by the parallel analysis accounted for 62.2% of variance and was supported by the scree-test method, see Figure 1, as well as conforming to the K1 rule for retaining factors with eigenvalues above 1.
TABLE 3.
Component loadings for the (Promax) rotated two-factor solution, percentage of variance explained, and relation with clinical characteristics
| Item | Factor I Modification | Factor II Participation | |
|---|---|---|---|
| 1 | Providing reassurance | 0.251 | 0.252 |
| 2 | Providing items | 0.569 | |
| 3 | Participating in behaviors | 0.803 | |
| 4 | Assisting avoidance | 0.665 | |
| 5 | Avoiding things or places | 0.395 | 0.388 |
| 6 | Modifying routine | 0.756 | |
| 7 | Doing things instead of child | 0.649 | |
| 8 | Modifying work schedule | 0.829 | |
| 9 | Modifying leisure activities | 1.04 | |
| Percent of variance explained | 46.21% | 15.98% |
Correlation between the two factors: r = .492.
Figure 1.
Scree plot of rotated principal axis factor analysis (Promax) for nine FASA accommodation items.
CONVERGENT AND DIVERGENT VALIDITY
Family accommodation, as measured by total FASA score, was significantly correlated with the severity of anxiety symptoms, as measured by SCARED, in the total sample (r(73) = .45, p < .001) and specialty anxiety clinics (r(48) = .45, p < .001). In the smaller sample of anxious children seen at the general outpatient clinic the correlation of FASA with SCARED was nonsignificant (r(23) = .267, p = .196).
Divergent validity was assessed by testing the association of FASA scores to depression, as measured by MFQ. When controlling for the significant correlation between depressive and anxious symptoms, the partial correlation of FASA to MFQ was insignificant (r(70) = .17, p = .155). By contrast, partial correlation of FASA to SCARED remained significant even after controlling for MFQ scores (r(70) = .29, p < .05).
DISCUSSION
We report on family accommodation in a sample of children and adolescents presenting with anxiety disorders at two specialty clinics for pediatric anxiety, and a comparison sample of high-anxiety children presenting at a general outpatient clinic. Overall, results confirm that family accommodation is prevalent among families of children suffering from various anxiety disorders, as has previously been shown to be the case in OCD.[2, 6, 7] In fact, the results closely resemble those that have been reported in OCD. Additionally, the results support the potential of the FASA as a brief parent-report tool for assessing family accommodation among families of children with anxiety disorders, as well as children presenting for other reasons who exhibit elevated anxiety. Moreover, the similar results obtained from the samples included in this study support the hypothesis that the construct of family accommodation is broadly applicable across anxiety disorders, as well as cultural milieus. Factor analysis produced an intuitively valid two-factor structure, including participation and modification, that largely concurs with what has been reported in OCD.[33]
Family accommodation was found to be positively correlated with the overall severity of anxiety symptoms. Within the subsample of children seen in a general out-patient clinic, the relation of accommodation to the level of reported anxiety was nonsignificant. However, this may be due in part to the truncated range of SCARED scores in that sample. Investigation of particular domains of anxiety and their relation to family accommodation produced mixed results. Among the anxiety disorders specialty clinic sample, the disorder that predicted most accommodation was separation anxiety. This is intuitively understandable as separation anxiety is both more common in younger children[34] who are likely to look to their parents for reassurance and regulation, and because the disorder is inherently parent-bound. The core symptoms of separation anxiety, that is, the unwillingness to separate from parents, make it a natural fit for accommodation to occur. By contrast, specific phobia which is likely to be more isolated and less tied to other forms of anxiety was actually nonsignificantly related to lower levels of accommodation in this sample. However, using the SCARED subscales as predictors and including the entire sample in the analysis revealed symptoms of generalized anxiety and school anxiety to be the most powerful predictors of accommodation.
The most important implication of this study is the need for more research into the role that family accommodation may play in shaping the clinical course of anxiety disorders, and their treatment. In the case of OCD, accommodation has been repeatedly found to be an important predictor of poorer treatment outcomes, for both behavioral and pharmacological interventions.[18] Accommodation has also been shown to be reduced when treatment is successful.[2] If this holds true across a broader range of anxiety disorders, it would point to the importance of treatment interventions that specifically target family accommodation. Other questions relate to the particular kinds of accommodation that are most important, and to the means with which children may impose accommodation on their families. Coercive behaviors among children with OCD have been reported to be very common, leading to greater accommodation and are associated with greater symptom severity.[4, 5, 35]
The overall similar results from two heterogeneous samples point to the applicability of the construct and the measure across different situations. Parents of children seen in the general outpatient clinic reported similar levels of accommodation to those seen specifically for anxiety related problems. The negative consequences of not accommodating and the degree of distress that accommodating caused the parents also did not differ between the two samples. In addition, children seen in specialty clinics in two different countries did not differ significantly in the level of accommodation reported by their parents.
The results of this study must be interpreted in light of some limitations. One limitation is the absence of parent characterization, apart from SES. Data on parental levels of anxiety or other symptomatology would enrich our understanding of the complex interactions between parent and child characteristics in the context of family accommodation. This is particularly important in light of previously reported links between parental anxiety and symptoms of childhood anxiety.[36] In the absence of multiple informants and repeated time points, it is also difficult to ascertain with confidence the reliability of the scale or its sensitivity to change and treatment effects. This limitation is mitigated however by the very close adoption of the items from the FAS, which has demonstrated high reliability and good overall psychometric properties.[3, 12, 13] Sample size was small for factor analysis. No accepted guidelines exist, but two widely used rules of thumb call for either five[37] or ten[38] participants per scale item and the current sample size falls between these two parameters. Nevertheless, more research into the properties of the FASA, as well as its relation to other clinical data is required and underway.
CONCLUSION
Family accommodation, which is an important construct in OCD, is common across childhood anxiety disorders and is associated with the severity of anxiety symptoms. The FASA is a brief, easily administered tool that shows promise as a means of assessing the presence, magnitude, and character of family accommodation in childhood anxiety disorders. The FASA can inform clinical care as well as serving in future research into this important phenomenon.
Acknowledgments
Eli Lebowitz is grateful for the support of the Messer Anxiety Program at the Yale Child Study Center. Dr. Lebowitz has received royalties from John Wiley and Sons. Dr. Leckman has received research support from the National Institutes of Health and the Tourette Syndrome Association. He has received royalties from John Wiley and Sons, McGraw Hill, and Oxford University Press. Dr. Scahill serves as a consultant for BioMarin, Boehringer-Ingelheim, Neruosearch, and Pfizer.
Footnotes
All other authors have no conflicts to disclose.
References
- 1.Calvocoressi L, Lewis B, Harris M, et al. Family accommodation in obsessive-compulsive disorder. Am J Psychiatry. 1995;152(3):441–443. doi: 10.1176/ajp.152.3.441. [DOI] [PubMed] [Google Scholar]
- 2.Lebowitz ER, Panza KE, Su J, Bloch MH. Family accommodation in obsessive–compulsive disorder. Expert Rev Neurother. 2012;12(2):229–238. doi: 10.1586/ern.11.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calvocoressi L, Mazure CM, Kasl SV, et al. Family accommodation of obsessive-compulsive symptoms: instrument development and assessment of family behavior. J Nerv Ment Dis. 1999;187(10):636–642. doi: 10.1097/00005053-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Lebowitz ER, Vitulano LA, Mataix-Cols D, Leckman J. Editorial perspective: when OCD takes over … the family! Coercive and disruptive behaviours in paediatric obsessive compulsive disorder. J Child Psychol Psychiatry. 2011;52(12):1249–1250. doi: 10.1111/j.1469-7610.2011.02480.x. [DOI] [PubMed] [Google Scholar]
- 5.Lebowitz ER, Vitulano LA, Omer H. Coercive and disruptive behaviors in pediatric obsessive compulsive disorder: A qualitative analysis. Psychiatry. 2011;74(4):362–371. doi: 10.1521/psyc.2011.74.4.362. [DOI] [PubMed] [Google Scholar]
- 6.Caporino N, Morgan J, Beckstead J, Phares V, Murphy T, Storch E. A structural equation analysis of family accommodation in pediatric obsessive-compulsive disorder. J Abnorm Child Psychol. 2012;40(1):133–143. doi: 10.1007/s10802-011-9549-8. [DOI] [PubMed] [Google Scholar]
- 7.Flessner CA, Freeman JB, Sapyta J, et al. Predictors of parental accommodation in pediatric obsessive-compulsive disorder: findings from the Pediatric Obsessive-Compulsive Disorder Treatment Study (POTS) Trial. J Am Acad Child Adolesc Psychiatry. 2011;50(7):716–725. doi: 10.1016/j.jaac.2011.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J. Correlates of accommodation of pediatric obsessive-compulsive disorder: parent, child, and family characteristics. J Am Acad Child Adolesc Psychiatry. 2008;47(10):1173–1181. doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waters TL, Barrett PM. The role of the family in childhood obsessive-compulsive disorder. Clin Child Fam Psychol Rev. 2000;3(3):173–184. doi: 10.1023/a:1009551325629. [DOI] [PubMed] [Google Scholar]
- 10.Merlo L, Lehmkuhl H, Geffken G, Storch E. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. J Consult Clin Psychol. 2009;77(2):355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Storch E, Larson M, Muroff J, et al. Predictors of functional impairment in pediatric obsessive-compulsive disorder. J Anxiety Disord. 2010;24(2):275–283. doi: 10.1016/j.janxdis.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Flessner CA, Sapyta J, Garcia A, et al. Examining the psychometric properties of the Family Accommodation Scale-Parent-Report (FAS-PR) J Psychopathol Behav Assess. 2011;33(1):38–46. doi: 10.1007/s10862-010-9196-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Storch EA, Geffken GR, Merlo LJ, et al. Family accommodation in pediatric obsessive-compulsive disorder. J Clin Child Adolesc Psychol. 2007;36(2):207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- 14.Ferrao Y, Shavitt R, Bedin N, et al. Clinical features associated to refractory obsessive-compulsive disorder. J Affect Disord. 2006;94(1–3):199–209. doi: 10.1016/j.jad.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 15.Storch E, Geffken G, Merlo L, et al. Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: comparison of intensive and weekly approaches. J Am Acad Child Adolesc Psychiatry. 2007;46(4):469–478. doi: 10.1097/chi.0b013e31803062e7. [DOI] [PubMed] [Google Scholar]
- 16.Storch EA, Lehmkuhl HD, Ricketts E, Geffken GR, Marien W, Murphy TK. An open trial of intensive family based cognitive-behavioral therapy in youth with obsessive-compulsive disorder who are medication partial responders or nonresponders. J Clin Child Adolesc Psychol. 2010;39(2):260–268. doi: 10.1080/15374410903532676. [DOI] [PubMed] [Google Scholar]
- 17.Pediatric OCD Treatment Study Team. Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder. J Am Med Assoc. 2004;292(16):1969–1976. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- 18.Garcia A, Sapyta J, Moore P, et al. Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I) J Am Acad Child Adolesc Psychiatry. 2010;49(10):1024–1033. doi: 10.1016/j.jaac.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and co-morbidity. Child Adolesc Psychiatr Clin N Am. 2005;14(4):631–648. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Bowlby J. Attachment and Loss. London: Institute of PsychoAnalysis; 1969. [Google Scholar]
- 21.Bögels SM, Brechman-Toussaint ML. Family issues in child anxiety: attachment, family functioning, parental rearing and beliefs. Clin Psychol Rev. 2006;26(7):834–856. doi: 10.1016/j.cpr.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 22.Hudson JL, Rapee RM. Parent-child interactions and anxiety disorders: an observational study. Behav Res Ther. 2001;39(12):1411–1427. doi: 10.1016/s0005-7967(00)00107-8. [DOI] [PubMed] [Google Scholar]
- 23.Hudson JL, Rapee RM. Parent-child interactions in clinically anxious children and their siblings. J Clin Child Adolesc Psychol. 2002;31(4):548–555. doi: 10.1207/S15374424JCCP3104_13. [DOI] [PubMed] [Google Scholar]
- 24.Ginsburg GS, Siqueland L, Masia-Warner C, Hedtke KA. Anxiety disorders in children: family matters. Cogn Behav Pract. 2004;11(1):28–43. [Google Scholar]
- 25.Barrett P, Healy-Farrell L, March JS. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: a controlled trial. J Am Acad Child Adolesc Psychiatry. 2004;43(1):46–62. doi: 10.1097/00004583-200401000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: a controlled trial. J Consult Clin Psychol. 1996;64(2):333–342. doi: 10.1037//0022-006x.64.2.333. [DOI] [PubMed] [Google Scholar]
- 27.Breinholst S, Esbjorn BH, Reinholdt-Dunne ML, Stallard P. CBT for the treatment of child anxiety disorders: a review of why parental involvement has not enhanced outcomes. J Anxiety Disord. 2012;26(3):416–424. doi: 10.1016/j.janxdis.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 28.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Silverman WK, Albano AM. Anxiety Disorders Interview Schedule (ADIS-IV) parent interview schedule. New York: Oxford University Press; 1996. [Google Scholar]
- 30.Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. J Am Acad Child Adolesc Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- 31.Angold A, Costello EJ. Mood and Feelings Questionnaire. Durham, NC: Developmental Epidemiology Program, Duke University; 1987. [Google Scholar]
- 32.Hayton JC, Allen DG, Scarpello V. Factor retention decisions in exploratory factor analysis: a tutorial on parallel analysis. Organ Res Methods. 2004;7(2):191–205. [Google Scholar]
- 33.Albert U, Bogetto F, Maina G, Saracco P, Brunatto C, Mataix-Cols D. Family accommodation in obsessive-compulsive disorder: relation to symptom dimensions, clinical and family characteristics. Psychiatry Res. 2010;179(2):204–211. doi: 10.1016/j.psychres.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 34.Foley DL, Rowe R, Maes H, Silberg J, Eaves L, Pickles A. The relationship between separation anxiety and impairment. J Anxiety Disord. 2008;22(4):635–641. doi: 10.1016/j.janxdis.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lebowitz ER, Omer H, Leckman JF. Coercive and disruptive behaviors in pediatric obsessive–compulsive disorder. Depress Anxiety. 2011;28(10):899–905. doi: 10.1002/da.20858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wood JJ, McLeod BD, Sigman M, Hwang WC, Chu BC. Parenting and childhood anxiety: theory, empirical findings, and future directions. J Child Psychol Psychiatry. 2003;44(1):134–151. doi: 10.1111/1469-7610.00106. [DOI] [PubMed] [Google Scholar]
- 37.Bryant FB, Yarnold PR. Principal-components analysis and exploratory and confirmatory factor analysis. In: Grimm LG, Yarnold PR, editors. Reading and Understanding Multivariate Statistics. Washington, DC: American Psychological Association; 1995. pp. 99–136. [Google Scholar]
- 38.Costello AB. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1–9. [Google Scholar]