Abstract
The primary objective of this study was to use step activity monitoring to quantify activity changes after total hip arthroplasty in patients 50 years or less. Secondly, we investigated whether step activity measurements correlated with the Harris hip and UCLA scores.
We prospectively analyzed 37 patients (age ≤50) treated with primary THA. Patient activity was recorded with a step activity monitor. Harris hip and UCLA scores were analyzed.
Total daily stride counts increased by an average of 30.0%. Increases were noted in the percent of daily time spent at high, moderate and low activity. Increases in daily time spent at high activity moderately correlated with the UCLA activity score but did not correlate with the HHS. Both the UCLA score and the HHS did not correlate with mean daily strides.
Following THA, patients ≤ 50 years of age increase their activity by taking more daily strides and improve their activity profile by spending more time at higher activity. Improvements in step activity moderately correlate with improvements in UCLA scores.
Keywords: Total hip arthroplasty, step activity monitor, activity
Introduction
Patients less than 50 years of age with end-stage joint disease represent a population distinct from elderly, relatively inactive patients. One of the key challenges of arthroplasty in this population is returning patients to their desired activity level, which is often higher than their elderly counterparts. 1–3 Traditional hip scoring systems which assess patient pain and daily function, may fail to stratify activity level in a younger, more active population.4 Clinically relevant methods for evaluation of post-operative activity in young hip patients continue to be developed.
Step activity monitoring has been accurately used to monitor changes in gait and activity in a host of musculoskeletal disorders and diseases affecting gait,5–12 including hip arthritis.1,3,5–16 Step activity monitoring relies on the use of ankle based accelerometers to record the number of strides patients take per minute. The sensitivity and cadence of a specific patient’s gait cycle can be specified so that the accelerometer can record not only total strides but the frequency of strides (intensity of activity), durations of sustained activity, and patterns of peak activity and inactivity.5,10,11,13,17 The SAM is more accurate than a pedometer in counting steps, particularly in individuals with higher BMIs3,16 and has an accuracy exceeding 98%. 5,12,14,17 Patterns of activity, such as durations of moderate or high activity as a percentage of total daily activity, are more powerful predictors of changes in functional status than overall step counts or conventional gait analysis.5 The ability of the SAM to differentiate between varying activity levels makes it a potentially valuable tool in the evaluation of activity after total hip arthroplasty, particularly in more active populations.
The primary objective of this study was to use step activity monitoring to quantify activity changes after total hip arthroplasty in patients 50 years or less. Our secondary goal was to correlate step activity data to the Modified Harris Hip Score (MHHS) and University of California, Los Angeles (UCLA) Activity score.
Methods
Patient Characteristics
Institutional review board approval was obtained for this prospective study. From January 2008 to July 2010, 128 patients were identified as possible study participants. Inclusion criteria included symptomatic osteoarthritis (OA), rheumatoid arthritis (RA) or osteonecrosis (ON) unresponsive to conservative therapies, patient age ≤50 and the ability to ambulate independently. All patients were scheduled for hip arthroplasty prior to study enrollment. Of the patients identified, 15 were excluded because they underwent resurfacing rather than conventional arthroplasty. Seventy-six patients were excluded due to inadequate or incomplete step monitoring data. This left 37 patients for analysis.
Of the 37 patients included in our study, 25 patients were female (68%) and twelve (32%) were male. Diagnoses included OA in 32 patients, ON in 4 and RA in 1. The average age of patients at the time of enrollment was 42.1 ±7.2 years (range, 17.8 to 50.3). Preoperatively BMI was 29.0 kg/m2 ± 5.6 (range, 20.1 to 44.3 kg/m2). Mean pre-operatively Modified Harris hip score was 52.2 ±10.3 (range 29.7 to 73.7) and mean preoperative UCLA activity score was 6.0 ± 2.2(range 3.0 to 10.0). Patients were not excluded for concomitant musculoskeletal conditions. One patient had marked knee OA, one had mild OA and one reported a prior ACL tear. Five additional patients reported mild knee pain that did not limit their function.
Step Activity Monitoring
Prior to surgery, patients were provided and asked to wear a StepWatch™ Activity Monitor 3.0 (SAM; Cyma Corp., WI, USA) consecutively for 7 days. The SAM is calibrated using the patient’s height and gait characteristics and then records the number of strides taken in one minute intervals. Stride was defined as the heel strike of one foot to the subsequent heel strike of that same foot. After seven days, patients mailed the activity monitor back to our institution where data were downloaded from the device and analyzed with the StepWatch™ Analysis Software. One-year after surgery patients were again asked to wear the activity monitor consecutively for one week with identical instructions. At both time points, activity data was included for analysis if the patient wore the step monitor for at least 10 hours on 4 of the 7 days, including 1 weekend day. Mean time between surgery and the collection of post-operative step activity data was 1.3 ± 0.2 years (range, 0.9 to 1.7 years).
Step activity monitoring data generated included the number of daily strides taken and the percentage of time spent at different activity intensities. Activity intensity was defined as low, moderate or high on the basis of strides taken per minute. Activity was deemed low intensity if the patient took between 1 and 20 strides per minute13 Activity was deemed moderate intensity if the patient took between 21 and 40 strides per minute and high intensity if more than 40 strides per minute. Time spent wherein no strides per minute were performed was deemed inactive time.
All arthroplasties were performed by our senior author (blinded) through a posterior approach utilizing cementless implants. Post-operative reconstruction offset and leg length was assessed radiographically.18–21 Average increase in reconstruction offset was 3.7 mm and average increase in leg length was 5.1 mm. Many hips were intentionally lengthened to correct preoperative leg length inequalities. All patients were encouraged to weight bear as tolerated immediately following surgery per our routine protocol. After the initial postoperative period, patients were encouraged to be active by participating in low impact activities such as swimming, walking, elliptical and cycling. Running was discouraged by the treating surgeon.
Clinical Outcomes and Questionnaires
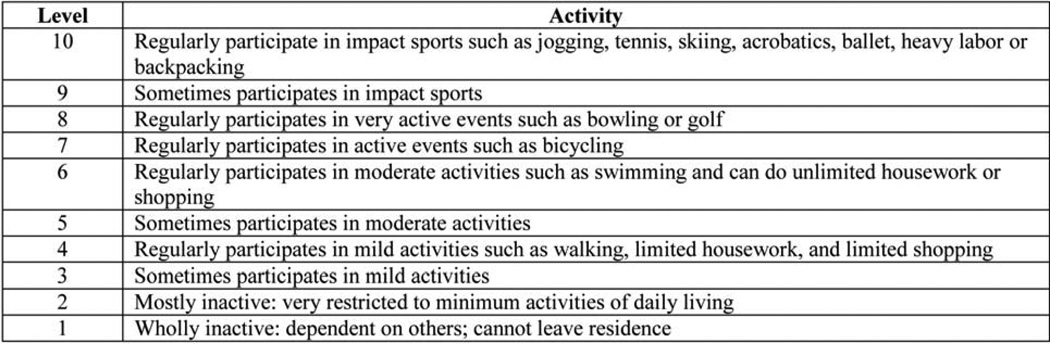
Other clinical outcomes included the MHHS and the UCLA activity score. The MHHS contains domains pertaining to pain and function and is commonly used to quantify hip disorders.22 The UCLA activity score (Figure 1) is a ten point activity scale that evaluates patient activity based on 10 descriptive activity levels ranging from wholly inactive and dependent (level 1) to regular participation in impact sports such as jogging or tennis (level 10).23 Both the MHHS and the UCLA activity score were obtained preoperatively and at one-year follow-up by means of a selfadministered patient questionnaire.
Figure 1.
UCLA Activity-Level Rating
Statistical Analysis
Data are presented as mean ± standard deviation. The difference between preoperative and postoperative step activity and clinical outcome scores were assessed with the use of the paired t-test, except where assumptions were not satisfied and Wilcoxon’s signed rank test was used as an alternative. A p-value of <0.05 was considered to be significant. Correlation was determined by calculating the Spearman or Pearson correlation coefficient as indicated. A Pearson or Spearman product-moment coefficient of correlation (r) of 0.6 or greater indicated a strong correlation, 0.6 to 0.4 a moderate correlation, 0.2 to 0.4 a fair correlation and less than 0.2 no correlation.
Results
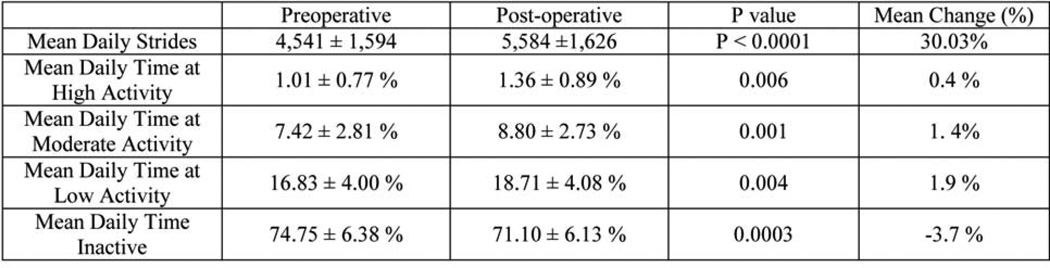
The mean daily strides increased from 4,541 ±1,594 (range 2,186 to 8,857) preoperatively to 5,584 ± 1,626 (range 2,248 to 9,181, p < 0.0001). This constituted a 30.03% increase in mean daily steps. Twenty-nine patients (78.3%) increased their absolute daily step counts postoperatively while 8 patients took fewer mean daily steps at one-year post-operatively. Despite this increase in daily strides, the mean weight increased significantly from 85.2 ± 20.8 kg (range 53.1 to 136.1 kg) preoperatively to 86.3 ± 21.3 kg postoperatively (range 54.0 to 139.7 kg; p=0.026). Mean BMI increased significantly from 29.0 ± 5.58 kg/m2 preoperatively (range 20.1 to 44.3 kg/m2) to 29.3 ± 5.7 kg/m2 postoperatively (range, 20.4 to 45.5 kg/m2; p = 0.022).
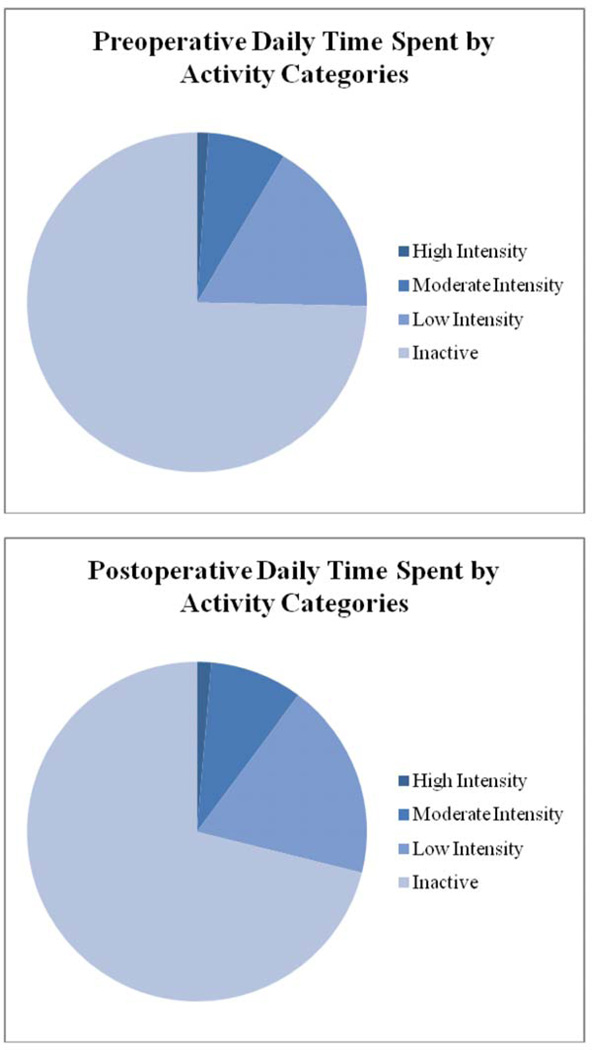
Mean daily time spent at high intensity activity increased from 1.0% ± 0.8 (range, 0.2% to 2.6%) preoperatively to 1.4% ± 0.9 post-operatively (range, 0.2 to 3.2%; p = 0.006). Mean daily time spent at moderate intensity activity increased from 7.4% ± 2.8 (range, 3.2 to 17.4%) preoperatively to 8.8% ± 2.7 postoperatively (range, 4.0 to 15.1%; p=0.001). Mean daily time spent at low intensity activity increased from 16.8% ± 4.0 (range, 9.0 to 23.2%) preoperatively to 18.7% ± 4.1 postoperatively (range, 9.5 to 29.1%; p=0.004). Mean daily time spent inactive decreased from 74.8% ±6.4 (range, 59.2 to 86.6%) preoperatively to 71.1% ± 6.1 postoperatively (range, 57.5 to 86.1; p=0.0003; Figure 2). On average, patients increased their time at high intensity activity by 0.4%. Similarly, patients increased their mean daily time spent at moderate and low activity by 1.4% and 1.9% respectively. Mean daily time spent inactive decreased by 3.7% (Figure 3).
Figure 2.
Preoperative (A) and Postoperative (B) graphic representations of time spent at various activity levels.
Figure 3.
Step Activity Data for THA Patients
The mean MHHS improved from 52.4 ± 10.3 (range 29.7 to 73.7) preoperatively to 90.2 ± 11.6 postoperatively (range 63 to 100; p < 0.0001). All patients demonstrated an increase in postoperative MHHS. The mean UCLA activity level score increased from 6.0 ± 2.2 preoperatively (range, 3.0 to 10.0) to 7.2 ± 1.6 postoperatively (range 4.0 to 10.0; p = 0.0009). Of the 36 patients with calculated pre and post-operative UCLA activity scores, 23 (63.8%) improved their score postoperatively, 10 (27.7%) maintained their score post-operatively, and 3 (8.3%) decreased their score. Improvements in both the MHHS and the UCLA score were not correlated with increases in mean daily strides (r = −0.15, p = 0.40 and r =0.23, p = 0.17 respectively). Increases in mean daily percentage of time spent at high activity did not correlate with improvement in MHHS (r = 0.11, p = 0.50) but moderately correlated with improvements in UCLA score (r = 0.42, p = 0.01).
Discussion
Surgeons have long relied on physician outcome measures and subjective patient surveys to evaluate functional results of THA. Functional improvement after THA, however, is difficult to describe and quantify. Multiple studies have demonstrated a correlation between advanced age and reduced daily step counts after THA. Zahiri, Silva and Schmalzried have independently demonstrated that THA patients younger than sixty take significantly more daily steps postoperatively (30–78%) than those sixty or older.3,4,24 Sechriest similarly demonstrated that advancing age negatively correlated with total gait cycles following THA, though not to a statistically significant degree.2 Kinkel used step activity monitoring to evaluate walking activity after THA and found that step counts are highest in the < 50 and 50–59 year age groups and decrease significantly with advancing age beyond sixty.1
Higher pre-operative and post-operative activity levels in younger patients make the evaluation of mobility and function more challenging. Traditional hip scoring systems, while useful in describing overall perception of function, do not provide the full extent, intensity and frequency of patient activity. The UCLA activity score describes activity level in terms of the patient’s capacity for function but is not sensitive enough to detect actual variability in activity frequency or intensity. Zahair demonstrated a nearly 15-fold variability between the average number of steps taken among patients with the same UCLA score.4 Sechriest was unable to correlate mean annual gait cycles with improvements in either the Harris hip score, unspecified if original or modified, or UCLA activity scores in young patients (age < 50).2 Similarly, great variability has been demonstrated in the activity levels seen between patients with the original Harris Hip Score.25 Changes in real-life activity may not be reflected in either of these conventional outcomes tests, which are subject to the patients’ recall biases. This evidence, coupled with our collective experience, suggest that a ‘ceiling effect’ exists for active, young patients after arthroplasty, beyond which gains in function are not readily apparent with conventional outcome measures.
While many studies attempt to quantify activity after total hip arthroplasty, there is a paucity of data on the quality of real-life activity in young patients after total hip arthroplasty. Where activity monitoring has been utilized in the arthroplasty literature, it has been used to simply count steps rather than to differentiate step intensities or to quantify ambulatory activity. No study to our knowledge has previously used activity intensity levels to define activity after THA. We hypothesized that young patients would both increase stride counts after arthroplasty and improve their step activity profiles by taking quicker steps. Our study asserts this hypothesis. At one year postoperatively, our patients increased their mean daily stride counts by 30.03%, a finding consistent with previous studies.3,4,15 Additionally, mean daily inactive time in our patient population decreased by 3.7% . Both MHHS and UCLA activity scores improved significantly at a rate similar to other studies in young patients.2,26,27 The novel component of our study is that we evaluated changes in the intensity of activity (“activity profile”) post-operatively, as reported by increases in the percentage of time spent at high, moderate and low intensity activities. When compared to preoperative data, mean daily time spent at high intensity activity increased by 6.4%, moderate intensity activity increased by 1.4% and low intensity activity increased by 1.9%. Although statistically significant, these percent increases represent relatively small changes in percent of daily time.
We were unable to correlate increased daily step counts with either improved UCLA activity or Modified Harris Hip scores. Increases in mean daily time spent at high activity, however, moderately correlated with improvements in UCLA activity score. This moderate correlation suggests that UCLA activity scores fail to fully characterize activity following THA. We were unable to correlate improved activity profiles with improvements in MHHS. Collectively, these data suggest that when compared to the MHHS and UCLA scores SAM is recording unique outcome data not captured by conventional clinical outcome measures.
Despite an increase in activity, post-operative weight and BMI increased slightly (but significant) from preoperative values. This finding is in concert with previous studies, which suggest that BMI after arthroplasty increases despite increased activity and decreased pain.2,28–30 One of the primary benefits of the SAM is the ability to correlate activity and energy expenditure.14 We would have predicted that improvements in activity profile would be reflected by decreases in weight and BMI. While calculations of energy expenditure are beyond the scope of this study, we speculate that the observed increases in weight and BMI are a function of increased caloric intake rather than decreased energy expenditure in our patients.
The strengths of our study are its prospective nature and the homogeneity of our patient population, surgical technique and post-operative protocol. The weaknesses of our study lie in its relatively small number of subjects (n =37) and its short outcome. Studies suggest that functional improvements and walking ability after total hip arthroplasty should be significantly improved at six months, but that patients may continue to make gains up to 24 months postoperatively. 31–34 Certainly longer follow-up would demonstrate whether or not functional gains are maintained. Other musculoskeletal conditions may also affect activity level. Eight patients reported the presence of knee OA or knee pain. These patients confirmed their knee condition did not affect their function, we therefore chose to include them in the study. No other musculoskeletal conditions were reported, however we recognize that concomitant spine issues may have gone unreported. Additionally, patient compliance with the SAM protocol was problematic. Loss of 76 patients due to noncompliance may introduce bias to the study as noncompliance may correlate with specific activity profiles. This is an important observation regarding the use of SAM as a clinical outcome measure. We had strict inclusion criteria. Patients had to wear the monitor for 10 hours at least four of the seven days including at least one weekend day. Non-compliance was common leading to the exclusion of many patients. Future studies with this device will require improved patient monitoring to obtain more generalizable data. Finally, we recognize that future studies are needed to elucidate the clinical significance of the reported alterations in ambulatory function.
Conclusions
In the young, active patient return to high intensity activity is difficult to interpret with traditional scoring systems. Our study provides the early results of activity in patients 50 years of age or less who have been treated with THA. These patients significantly improve both overall strides and the overall intensity profile of their activity. Improvements in activity profile are only moderately correlated with improvements in UCLA activity scores and are not correlated with MHHS. Step activity monitoring allows for a more complete understanding of changes in activity in young patients after THA.
Acknowledgment
This work was supported in part by the Hip Society / OREF grant titled “Measuring Outcomes in Young Hip Patients”. This work was also supported in part by the Curing Hip Disease Fund.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kinkel S, Wollmerstedt N, Kleinhans JA, Hendrich C, Heisel C. Patient activity after total hip arthroplasty declines with advancing age. Clin Orthop Relat Res. 2009;467:2053–2058. doi: 10.1007/s11999-009-0756-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sechriest VF, 2nd, Kyle RF, Marek DJ, Spates JD, Saleh KJ, Kuskowski M. Activity level in young patients with primary total hip arthroplasty: a 5-year minimum follow-up. J Arthroplasty. 2007;22:39–47. doi: 10.1016/j.arth.2006.02.083. [DOI] [PubMed] [Google Scholar]
- 3.Silva M, Shepherd EF, Jackson WO, Dorey FJ, Schmalzried TP. Average patient walking activity approaches 2 million cycles per year: pedometers under-record walking activity. J Arthroplasty. 2002;17:693–697. doi: 10.1054/arth.2002.32699. [DOI] [PubMed] [Google Scholar]
- 4.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/s0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 5.Boone DA, Coleman KL. Use of a step activity monitor in determining outcomes. SSC Proceedings; 2006;2006:86–92. [Google Scholar]
- 6.Busse ME, Pearson OR, Van Deursen R, Wiles CM. Quantified measurement of activity provides insight into motor function and recovery in neurological disease. J Neurol Neurosurg Psychiatry. 2004;75:884–888. doi: 10.1136/jnnp.2003.020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chambers HG, Sutherland DH. A practical guide to gait analysis. J Am Acad Orthop Surg. 2002;10:222–231. doi: 10.5435/00124635-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Haeuber E, Shaughnessy M, Forrester LW, Coleman KL, Macko RF. Accelerometer monitoring of home- and community-based ambulatory activity after stroke. Arch Phys Med Rehabil. 2004;85:1997–2001. doi: 10.1016/j.apmr.2003.11.035. [DOI] [PubMed] [Google Scholar]
- 9.Macko RF, Haeuber E, Shaughnessy M, et al. Microprocessor-based ambulatory activity monitoring in stroke patients. Med Sci Sports Exerc. 2002;34:394–399. doi: 10.1097/00005768-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 10.McDonald CM, Widman LM, Walsh DD, Walsh SA, Abresch RT. Use of step activity monitoring for continuous physical activity assessment in boys with Duchenne muscular dystrophy. Arch Phys Med Rehabil. 2005;86:802–808. doi: 10.1016/j.apmr.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 11.Pearson OR, Busse ME, van Deursen RW, Wiles CM. Quantification of walking mobility in neurological disorders. QJM. 2004;97:463–475. doi: 10.1093/qjmed/hch084. [DOI] [PubMed] [Google Scholar]
- 12.Shaughnessy M, Michael KM, Sorkin JD, Macko RF. Steps after stroke: capturing ambulatory recovery. Stroke. 2005;36:1305–1307. doi: 10.1161/01.STR.0000166202.00669.d2. [DOI] [PubMed] [Google Scholar]
- 13.Brandes M, Schomaker R, Mollenhoff G, Rosenbaum D. Quantity versus quality of gait and quality of life in patients with osteoarthritis. Gait Posture. 2008;28:74–79. doi: 10.1016/j.gaitpost.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Foster RC, Lanningham-Foster LM, Manohar C, et al. Precision and accuracy of an ankle-worn accelerometer-based pedometer in step counting and energy expenditure. Prev Med. 2005;41:778–783. doi: 10.1016/j.ypmed.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 15.Schmalzried TP, Huk OL. Patient factors and wear in total hip arthroplasty. Clin Orthop Relat Res. 2004:94–97. doi: 10.1097/00003086-200401000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Shepherd EF, Toloza E, McClung CD, Schmalzried TP. Step activity monitor: increased accuracy in quantifying ambulatory activity. J Orthop Res. 1999;17:703–708. doi: 10.1002/jor.1100170512. [DOI] [PubMed] [Google Scholar]
- 17.Coleman KL, Smith DG, Boone DA, Joseph AW, del Aguila MA. Step activity monitor: long-term, continuous recording of ambulatory function. J Rehabil Res Dev. 1999;36:8–18. [PubMed] [Google Scholar]
- 18.Clark CR, Huddleston HD, Schoch EP, 3rd, Thomas BJ. Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:38–45. doi: 10.5435/00124635-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Dastane M, Dorr LD, Tarwala R, Wan Z. Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clin Orthop Relat Res. 2011;469:429–436. doi: 10.1007/s11999-010-1554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karachalios T, Hartofilakidis G, Zacharakis N, Tsekoura M. A 12- to 18-year radiographic follow-up study of Charnley low-friction arthroplasty. The role of the center of rotation. Clin Orthop Relat Res. 1993:140–147. [PubMed] [Google Scholar]
- 21.Maloney WJ, Keeney JA. Leg length discrepancy after total hip arthroplasty. J Arthroplasty. 2004;19:108–110. doi: 10.1016/j.arth.2004.02.018. [DOI] [PubMed] [Google Scholar]
- 22.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16(6):578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 23.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 24.Schmalzried TP, Szuszczewicz ES, Northfield MR, et al. Quantitative assessment of walking activity after total hip or knee replacement. J Bone Joint Surg Am. 1998;80:54–59. [PubMed] [Google Scholar]
- 25.Bauman S, Williams D, Petruccelli D, Elliott W, de Beer J. Physical activity after total joint replacement: a cross-sectional survey. Clin J Sport Med. 2007;17:104–108. doi: 10.1097/JSM.0b013e3180379b6a. [DOI] [PubMed] [Google Scholar]
- 26.Kim YH, Kook HK, Kim JS. Total hip replacement with a cementless acetabular component and a cemented femoral component in patients younger than fifty years of age. J Bone Joint Surg Am. 2002;84-A:770–774. doi: 10.2106/00004623-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Kim YH, Oh SH, Kim JS. Primary total hip arthroplasty with a second-generation cementless total hip prosthesis in patients younger than fifty years of age. J Bone Joint Surg Am. 2003;85-A:109–114. doi: 10.2106/00004623-200301000-00017. [DOI] [PubMed] [Google Scholar]
- 28.Heisel C, Silva M, dela Rosa MA, Schmalzried TP. The effects of lower-extremity total joint replacement for arthritis on obesity. Orthopedics. 2005;28:157–159. doi: 10.3928/0147-7447-20050201-18. [DOI] [PubMed] [Google Scholar]
- 29.Jain SA, Roach RT, Travlos J. Changes in body mass index following primary elective total hip arthroplasty. Correlation with outcome at 2 years. Acta Orthop Belg. 2003;69:421–425. [PubMed] [Google Scholar]
- 30.Middleton FR, Boardman DR. Total hip arthroplasty does not aid weight loss. Ann R Coll Surg Engl. 2007;89:288–291. doi: 10.1308/003588407X179017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bertocci GE, Munin MC, Frost KL, Burdett R, Wassinger CA, Fitzgerald SG. Isokinetic performance after total hip replacement. Am J Phys Med Rehabil. 2004;83:1–9. doi: 10.1097/01.PHM.0000098047.26314.93. [DOI] [PubMed] [Google Scholar]
- 32.Braeken AM, Lochhaas-Gerlach JA, Gollish JD, Myles JD, Mackenzie TA. Determinants of 6–12 month postoperative functional status and pain after elective total hip replacement. Int J Qual Health Care. 1997;9:413–418. doi: 10.1093/intqhc/9.6.413. [DOI] [PubMed] [Google Scholar]
- 33.Laupacis A, Bourne R, Rorabeck C, et al. The effect of elective total hip replacement on health-related quality of life. J Bone Joint Surg Am. 1993;75:1619–1626. doi: 10.2106/00004623-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Murray MP, Brewer BJ, Gore DR, Zuege RC. Kinesiology after McKee-Farrar total hip replacement. A two-year follow-up of one hundred cases. J Bone Joint Surg Am. 1975;57:337–342. [PubMed] [Google Scholar]