Abstract
Objective
To investigate the feasibility and sample size required for a full-scale randomised controlled trial of the effectiveness of acupuncture with non-steroidal anti-inflammatory drugs (NSAIDs) for chronic neck pain compared with acupuncture or NSAID treatment alone.
Methods
A total of 45 patients with chronic neck pain participated in the study. For 3 weeks the acupuncture with NSAIDs treatment group took NSAIDs (zaltoprofen, 80 mg) daily while receiving acupuncture treatment three times a week. The acupuncture treatment group received treatment three times a week and the NSAID treatment group took NSAIDs daily. The primary outcomes were to determine the feasibility and to calculate the sample size. As secondary outcomes, pain intensity and pain-related symptoms for chronic neck pain were measured.
Results
With regard to enrolment and dropout rates, 88.2% of patients consented to be recruited to the trial and 15.6% of participants were lost to follow-up. The sample size for a full-scale trial was estimated to be 120 patients. Although preliminary, there was a significant change in the visual analogue scale (VAS) for neck pain intensity between the baseline measurement and each point of assessment in all groups. However, there was no difference in VAS scores between the three groups.
Conclusions
This pilot study has provided the feasibility and sample size for a full-scale trial of acupuncture with NSAIDs for chronic neck pain compared with acupuncture or NSAID treatment alone. Further research is needed to validate the effects of acupuncture with NSAIDs.
Clinical Trial Registration
NIH ClinicalTrials.gov NCT01205958.
Keywords: ACUPUNCTURE, PAIN MANAGEMENT, COMPLEMENTARY MEDICINE
Introduction
Chronic neck pain is one of the most common complaints in the general population and can result in substantial problems including the cost of treatment, disability and absence from work.1 2 In many cases chronic neck pain is due to non-specific disorders of the muscles, tendons, joints and bones of the neck in association with unspecified degenerative changes.3
There are many treatments available for neck pain including drugs, physical therapy, manual treatments, immobilisation, local or epidural injection and patient education.4 Acupuncture is sometimes used as an alternative to western conventional treatments for musculoskeletal pain,5 and people are increasingly resorting to acupuncture treatments.6 However, until now there has been a lack of definitive evidence to support acupuncture as an effective treatment in patients with neck pain. A recent systematic review showed that the effect of acupuncture remains uncertain, with some studies showing positive results in the short or long term while others show negative results compared with mobilisation and traction.7
The effectiveness and safety profiles of non-steroidal anti-inflammatory drugs (NSAIDs) are recognised for their appropriate use for chronic diseases such as rheumatoid arthritis and also for acute diseases.8 However, there is no evidence that NSAIDs are positively or negatively associated with clinically important outcomes in the short or long term compared with other medications, non-invasive interventions or sham interventions for neck pain.7
Although complementary treatments have been considered necessary to supplement acupuncture or NSAIDs and improve treatment effectiveness for neck pain, the evidence from large-scale clinical trials remains inconclusive. We therefore undertook a pilot study to investigate the feasibility and sample size of the proposed design prior to a full-scale randomised controlled trial of the effectiveness of acupuncture with NSAIDs for chronic neck pain compared with acupuncture or NSAID treatment alone.
Methods
Study design
This pilot study was an assessor-blinded randomised controlled trial. As a pilot study, the sample size of patients was fixed at 45 patients based on practical considerations and all patients who consented to participate in this study were enrolled.
Participants
Participants between 25 and 55 years of age with chronic neck pain were recruited from November 2009 to October 2010 through advertisements in local newspapers and the hospital’s home page. The inclusion criteria were: (1) men or women aged 25–55 years; (2) symptoms such as neck pain or stiffness in the neck and shoulders lasting for 3 months or more; (3) a score of ≥5 on the visual analogue scale (VAS) at baseline. Patients were excluded if they (1) had received acupuncture or NSAID treatment for neck pain within the past 3 months; (2) had a serious medical disease or cancer; (3) had a history of spinal trauma, had undergone surgery on the neck or had systematic neurological or other skeletal disorders; (4) were pregnant or breast feeding.
Randomisation procedures
Using a computer-generated randomisation table, participants were randomly allocated into the following three groups: acupuncture treatment group (AC), NSAID treatment group (NS) and the acupuncture with NSAIDs treatment group (AN). This allocation was conducted independently of the clinicians involved in the treatment of the patients. As an assessor-blinded randomised controlled study, the researcher evaluating the outcome measure was blinded to the participant’s treatment allocation.
Intervention
The acupuncture treatment in this study is described according to Standards for Reporting Interventions in Clinical Trials of Acupuncture recommendations.9 For 3 weeks the AN group took an NSAID (zaltoprofen, 80 mg daily; C J Pharma Co, Korea) while receiving nine acupuncture sessions, the AC group received nine acupuncture sessions (three times a week) and the NS group took NSAIDs daily.
The AC and AN groups received acupuncture treatment at the acupuncture points for chronic neck pain for 3 weeks by licensed Korean Medicine Doctors (KMDs) with at least 3 years of experience. KMDs discussed and practised the methods of acupuncture treatment mentioned in the protocol. Based on literature reviews of acupuncture for neck pain, the widely-accepted local and distal acupuncture points were selected bilaterally.10–12 The standard points in the cervical region (local points) were SI9, SI10, SI11, SI12, SI14, BL11, BL12, TE14, TE15, TE16, TE17 and GB21 and the standard points on the extremities (distal points) were SI3, SI4 and BL65. In the acupuncture treatment groups, disposable stainless steel needles (0.25 mm×40 mm, Dongbang Acupuncture Needle Co, Korea) were inserted into the muscle to a depth of 20 mm. When the subject felt dull pain or the acupuncture sensation (de qi), the manipulation was stopped and the needle was left in place for 15 min. Patients in the NS and AN groups were instructed to take an NSAID (zaltoprofen, 80 mg) three times a day and record daily in a patient diary any doses and dates of missed medication. At each visit patients were asked to record in the diary any symptoms of illness or discomfort, supplemental medications taken or changes in the use of long-term medications.
Outcome measures
Our primary outcomes were to determine the feasibility and to calculate the sample size prior to carrying out a full-scale trial. The proportion of participants who finished the treatments and the sample size were calculated. Dropout ratios and adverse events were also investigated. As clinical outcomes, pain intensity and pain-related symptoms for chronic neck pain were measured. The patient was asked to mark on a 10 cm VAS the degree of pain in the neck experienced within the most recent week.13 14 The Neck Disability Index (NDI), a validated condition-specific tool that is widely used in neck pain trials, was administerd.15–17 The patient's health-related quality of life was measured using the well-validated SF-36, Beck's Depression Inventory (BDI) and Euroqol 5-D (EQ-5D).18–21 Each measurement was performed at weeks 0 (baseline), 1, 3 (primary end point) and 7 by an independent investigator who had no knowledge of the treatment sequence or the type of treatment the patient had received before each measurement.
Data analysis
SPSS V.18.0 for Windows was used for all statistical analyses. In seven cases there were missing data and, as such, Stochastic Regression Imputation was conducted for intention-to-treat analysis. The demographic and baseline assessments among the three groups were performed by analyses of variance (ANOVA) and χ2 tests. To compare VAS for pain intensity among the three groups at the primary end point, analyses of covariance (ANCOVA) were conducted with the baseline score as a covariate. Repeated-measure analysis of variance was carried out to assess changes between groups, interactions between groups and observed time of VAS. The paired t test and Wilcoxon signed-rank test were used to compare baseline VAS, NDI, SF-36, BDI and EQ-5D data with follow-up at 1, 3 and 7 weeks in each of the three groups. The SD values of the primary end point variables were used to calculate the sample size using G*Power V.3.1.
Results
Baseline characteristics
The baseline characteristics and outcome measurements of the patients allocated to the three groups are shown in table 1. Since the baseline pain intensity was significantly different between the three groups (p<0.05), ANCOVA with the baseline pain as a covariate was used to analyse the VAS for pain intensity.
Table 1.
Baseline characteristics and outcome measurements of patients enrolled in the study
| AC group (n=15) | NS group (n=15) | AN group (n=15) | p | |
|---|---|---|---|---|
| Age (years) | 39.1±9.0 | 38.2±10.2 | 39.2±9.1 | 0.434 |
| Gender | ||||
| Men | 7 (46.7) | 6 (40.0) | 3 (20.0) | 0.283 |
| Women | 8 (53.3) | 9 (60.0) | 12 (80.0) | |
| VAS | 6.7±0.7 | 6.07±0.5 | 7.1±1.3 | 0.009* |
| NDI | 23.2±5.9 | 22.3±4.0 | 26.3±5.0 | 0.087 |
| SF-36 | 85.2±1.2 | 86.2±2.0 | 84.2±1.7 | 0.655 |
| BDI | 28.7±4.8 | 30.7±5.6 | 33.1±7.8 | 0.125 |
| EQ-5D | 7.4±1.7 | 7.4±1.5 | 7.5±1.3 | 0.990 |
Values are mean±SD or n (%).
*p<0.05 (one-way ANOVA and χ2 test).
AC group, acupuncture treatment only; AN group, acupuncture with NSAID treatment; BDI, Beck's Depression Inventory; EQ-5D, Euroqol 5-D; NDI, Neck Disability Index; NS group, NSAID treatment only; NSAID, non-steroidal anti-inflammatory drug; VAS, visual analogue scale.
Enrolment rate and dropout ratio
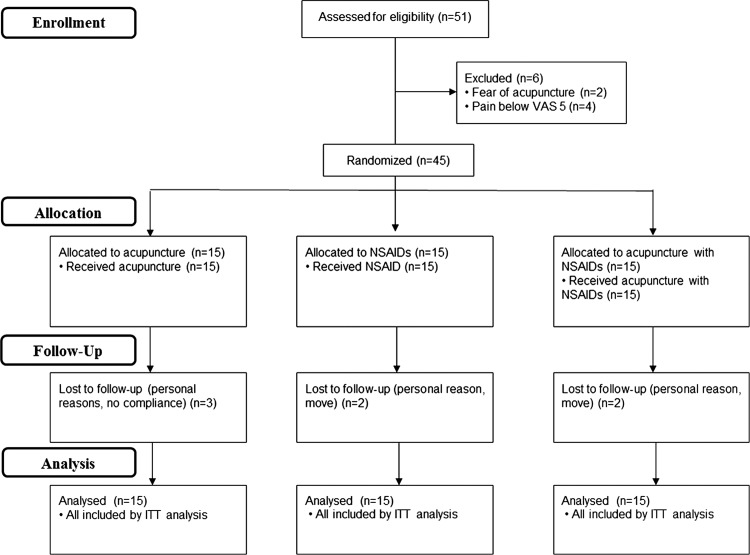
An overall flow diagram of the study design is provided in figure 1. A total of 51 patients were screened to enrol 45 patients in the trial (with an acceptance rate of 88.2%). Of the eligible patients invited to participate, two refused because of the fear of acupuncture while four patients were experiencing pain intensity of <5 on the VAS. Forty-five patients were enrolled and seven patients did not complete the study (two for private reasons, two who rejected treatment, two who moved away and one who did not comply), leaving 38 patients who completed the scheduled protocols for the trial (dropout rate 15.6%).
Figure 1.
Participation flowchart for the study. ITT, intention-to-treat; NSAID, non-steroidal anti-inflammatory drug; VAS, visual analogue scale.
Sample size calculation
The variance in VAS for pain intensity between weeks 0 and 3 was chosen as the primary outcome for the sample size calculation using the one-way ANOVA model. The mean square of the residual variance of VAS scores that included all patients and adjustment of the baseline pain scores was estimated at 4.09, which can be converted to a SD of 2.02. Given the effect size of 0.319 with all three comparisons, the sample size required to detect this difference at 5% significance and 80% power is 33 patients in each group. To allow for loss to follow-up of 15.6% based on our result, a full-scale trial will require a total of 120 patients.
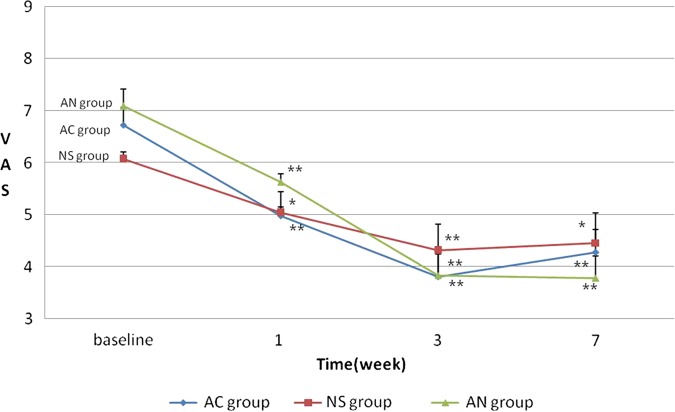
Pain intensity outcome measure
There were statistically significant changes in the VAS scores between baseline and each point of assessment in the three groups. However, ANCOVA and repeated measures ANOVA did not show significant differences in the VAS scores between the three groups (table 2, figure 2).
Table 2.
Changes in visual analogue scale (VAS) score for chronic neck pain
| F(p) | ||||||
|---|---|---|---|---|---|---|
| Group | Baseline | Week 1 | Week 3 | Week 7 | Time | Group×time |
| AC group | 6.7±0.7 | 5.0±1.9** | 3.8±2.4** | 4.3±2.0** | 43.3† (0.001) | 1.901 (0.101) |
| NS group | 6.1±0.5 | 5.0±1.9* | 4.3±1.7** | 4.5±2.2* | ||
| AN group | 7.1±1.3 | 5.6±0.7** | 3.8±1.8** | 3.8±1.6** | ||
Values represent mean±SD VAS score.
p Values (paired t test) between baseline measurement and measurements at 1, 3 and 7 weeks: *p<0.05; **p<0.01.
p Values repeated measure analysis of variance, analysis of covariant: †p<0.05.
AC group, acupuncture treatment only; AN group, acupuncture with NSAID treatment; NS group, NSAID treatment only.
Figure 2.
Changes in visual analogue scale (VAS) score for chronic neck pain. There were significant reductions in pain intensity in the three groups at each point of assessment compared with baseline (*p<0.05, **p<0.01) but there was no difference between the three groups (repeated measure analysis of variance, analysis of covariate). AC group, acupuncture treatment only; NS group, NSAID treatment only; AN group, acupuncture with NSAIDs.
Pain-related questionnaires
All questionnaire data are presented in table 3. The NDI scores assessed at each time point compared with baseline were significantly reduced in all groups (p<0.05). The changes in BDI and EQ-5D scores differed in each group, while the scores on the SF-36 questionnaire did not change significantly at any time in any of the groups.
Table 3.
Changes in NDI, BDI, SF-36 and EQ-5D scores for chronic neck pain
| Variable | Group | Baseline | Week 1 | Week 3 | Week 7 |
|---|---|---|---|---|---|
| NDI | AC group | 22.2±5.9 | 19.1±4.0** | 17.6±4.8** | 17.5±4.9** |
| NS group | 22.3±4.0 | 19.7±3.3* | 16.9±4.9** | 17.3±5.7** | |
| AN group | 26.3±5.0 | 23.1±4.8** | 19.4±4.4** | 17.7±5.4** | |
| BDI | AC group | 28.7±4.8 | 27.2±5.4 | 27.7±4.9 | 25.7±4.4* |
| NS group | 30.7±5.6 | 30.2±5.4 | 28.0±5.4* | 28.5±7.3* | |
| AN group | 33.1±7.8 | 31.2±6.0* | 28.9±6.7* | 27.2±6.3* | |
| SF-36 | AC group | 85.2±1.2 | 85.1±1.9 | 87.7±1.7 | 83.9±1.9 |
| NS group | 86.2±2.0 | 85.3±1.5 | 88.6±2.9 | 88.6±1.5 | |
| AN group | 84.2±1.7 | 82.8±2.4 | 84.4±2.6 | 84.3±1.1 | |
| EQ-5D | AC group | 7.4±1.7 | 6.6±1.1* | 6.6±1.4* | 7.0±1.3 |
| NS group | 7.4±1.5 | 7.5±1.4** | 7.0±1.7** | 7.3±1.9** | |
| AN group | 7.5±1.3 | 8.0±1.8 | 6.8±1.7 | 6.7±1.7 |
Values represent mean±SD.
p Values (Wilcoxon signed-rank test) between baseline measurement and measurements at 1, 3 and 7 weeks in each group: *p<0.05; **p<0.01.
AC group, acupuncture treatment only; AN group, acupuncture with NSAID treatment; BDI, Beck's Depression Inventory; EQ-5D, Euroqol 5-D; NDI, Neck Disability Index; NS group, NSAID treatment only.
Adverse events
Participants were asked to record unexpected events during treatment in the subjective answers. Acupuncture and NSAIDs were well tolerated with few adverse events. Only one patient in the AN group experienced a skin rash and burning sensation that was deemed unrelated to acupuncture or NSAIDs. No serious adverse events were reported.
Discussion
This pilot study provides useful data for the design of a full-scale trial on the effect of acupuncture with NSAIDs for chronic neck pain in comparison with acupuncture or NSAID treatment alone. With regard to enrolment rate and dropout rate, 88.2% of patients consented to be recruited to the trial and 15.6% of participants were lost to follow-up. We also found that a sample size of 120 patients would be required in a full-scale trial. Although there were no serious adverse events, the sample size of this study was so small that safety should be carefully considered for future large-scale trials. The evidence from our study suggests that this recruitment design is feasible.
To date there has been no randomised controlled study combining acupuncture and NSAID treatments for chronic neck pain. Two systematic reviews of non-specific neck pain reported that acupuncture may be more effective at reducing pain and improving quality of life than sham acupuncture or drug treatments including analgesics, NSAIDs, antidepressants and muscle relaxants.7 22 Only one trial comparing NSAIDs with manual therapy for the treatment of neck pain showed that osteopathic manipulative treatment resulted in positive pain reduction compared with ketorolac tromethamine (30 mg).23 In such an ambiguous situation, we planned this study design based on the assumption that acupuncture with NSAIDs is superior to acupuncture or NSAIDs alone for the treatment of chronic neck pain.
Although the clinical outcome measures used in this pilot study were intended to detect specific changes, there was a statistically significant reduction in pain and functional recovery in all three treatment groups when baseline measurements were compared with each follow-up assessment. However, there was no distinct difference in the size of pain reduction between the three groups. These findings are contradictory to those of other studies in which it was reported that the acupuncture effect may be facilitated and/or enhanced when combined with other treatments such as NSAIDs and muscle relaxants in patients with osteoarthritis, low back pain, fibromyalgia and tonsillectomy pain.24–29 One theoretical possibility for the similar outcomes among the three groups in this study could be that the analgesic mechanisms of acupuncture and NSAID treatments are similar in patients with chronic neck pain. Traditionally, acupuncture has been thought to stimulate the small diameter afferent fibres that activate the descending inhibitory and/or diffuse noxious inhibitory controls in the CNS which then reduce the pain signals, inhibiting pain discrimination and perception.30 On the other hand, NSAIDs exert an analgesic effect through peripheral prostaglandin synthesis inhibition as well as various other central mechanisms. This central effect is considered to be the result of prostaglandin formation suppression within the CNS and the central action mediated by endogenous opioid peptide.31
As the first study of the effectiveness of acupuncture combined with NSAIDs on chronic neck pain, we are aware of its limitations. The first limitation was related to the blinding of the study. Since it is impossible for acupuncture practitioners to be blinded to the acupuncture intervention, it is much more important to blind assessors. The second limitation is our inclusion of patients having a positive belief regarding either acupuncture or NSAIDs treatment, and therefore a future large-scale trial should consider including a question as part of the screening questionnaire about patients’ expectations regarding each treatment. The third limitation arises from the duration of the study. The effectiveness among the three groups was compared for 7 weeks after the baseline measurements so that long-term analgesic effects could not be investigated. Long-term investigations using a different study design are necessary in this regard.
In conclusion, this pilot study has provided the feasibility, safety and sample size for a full-scale trial of acupuncture with NSAIDs for chronic neck pain in comparison with acupuncture or NSAID treatment alone. Although preliminary, the finding that acupuncture with NSAIDs provides no greater benefit than acupuncture or NSAIDs alone raises questions about the mechanism of reciprocal action. Further research is needed to determine the relative contributions of the physiological effects of acupuncture and NSAIDs. Additional studies are therefore expected that include more control groups and conditions to identify the detailed mechanism of action between acupuncture and NSAIDs.
Summary points.
A pilot study was performed to investigate acupuncture combined with NSAIDs compared with acupuncture alone and NSAIDs alone in patients with chronic neck pain
A randomised controlled trial is feasible and would require 120 participants
Significant changes in pain scores were seen, but with no differences between treatment groups
Footnotes
Contributors: JHL was responsible for design of the study, interpretation of the analysis, THN undertook data collection and commented on drafts of the paper, JHC undertook data analysis and commented on the articles, KTK contributed to the design and analysis of the interviews and commented on the draft of the paper.
Funding: This study was funded by the program of the Kyung Hee University for young medical researcher in 2009 (KHU-20100763).
Competing interests: None.
Patient consent: All participants agreed with the procedures of this study and submitted informed consents in written form.
Ethics approval: The Institutional Review Board of the Kyung Hee University Hospital at Gangdong approved the research protocols (KHNMC-OH-IRB 2009-011).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Trinh KV, Graham N, Gross AR, et al. Acupuncture for neck disorders. Cochrane Database Syst Rev 2006;19(3):CD004870. [DOI] [PubMed] [Google Scholar]
- 2.Borghouts JA, Koes BW, Vondeling H, et al. Cost-of-illness of neck pain in the Netherlands in 1996. Pain 1999;80:629–36 [DOI] [PubMed] [Google Scholar]
- 3.Itoh K, Katsumi Y, Hirota S, et al. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complement Ther Med 2007;15:172–9 [DOI] [PubMed] [Google Scholar]
- 4.Aker PD, Gross AR, Goldsmith CH, et al. Conservative management of mechanical neck pain: systematic overview and meta-analysis. BMJ 1996;313:1291–6 [PMC free article] [PubMed] [Google Scholar]
- 5.Trinh KV, Graham N, Gross AR, et al. Acupuncture for neck disorders. Spine (Phila Pa 1976) 2007;32:236–43 [DOI] [PubMed] [Google Scholar]
- 6.Thomas K, Coleman P. Use of complementary or alternative medicine in a general population in Great Britain. Results from the National Omnibus Survey. J Public Health (Oxf) 2004;26:152–7 [DOI] [PubMed] [Google Scholar]
- 7.Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative Physiol Ther 2009;32:S141–75 [DOI] [PubMed] [Google Scholar]
- 8.Azuma A, Kudoh S, Nakashima M, et al. A double-blind study of zaltoprofen for the treatment of upper respiratory tract infection. Pharmacology 2010;85:41–7 [DOI] [PubMed] [Google Scholar]
- 9.MacPherson H, Altman DG, Hammerschlag R, et al. Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med 2010;28:83–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.He D, Veiersted KB, Hostmark AT, et al. Effect of acupuncture treatment on chronic neck and shoulder pain in sedentary female workers: a 6-month and 3-year follow-up study. Pain 2004;109:299–307 [DOI] [PubMed] [Google Scholar]
- 11.Zhu XM, Polus B. A controlled trial on acupuncture for chronic neck pain. Am J Chin Med 2002;30:13–28 [DOI] [PubMed] [Google Scholar]
- 12.Irnich D, Behrens N, Gleditsch JM, et al. Immediate effects of dry needling and acupuncture at distant points in chronic neck pain: results of a randomized, double-blind, sham-controlled crossover trial. Pain 2002;99:83–9 [DOI] [PubMed] [Google Scholar]
- 13.Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983;16:87–101 [DOI] [PubMed] [Google Scholar]
- 14.Revill SI, Robinson JO, Rosen M, et al. The reliability of a linear analogue for evaluating pain. Anaesthesia 1976;31:1191–8 [DOI] [PubMed] [Google Scholar]
- 15.Young IA, Cleland JA, Michener LA, et al. Reliability, construct validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am J Phys Med Rehabil 2010;89:831–9 [DOI] [PubMed] [Google Scholar]
- 16.Cleland JA, Fritz JM, Whitman JM, et al. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976) 2006;31:598–602 [DOI] [PubMed] [Google Scholar]
- 17.Song KJ, Choi BW, Choi BR, et al. Cross-cultural adaptation and validation of the Korean version of the neck disability index. Spine (Phila Pa 1976) 2011;35:E1045–9 [DOI] [PubMed] [Google Scholar]
- 18.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83 [PubMed] [Google Scholar]
- 19.Nam B, Lee S. Testing the validity of the Korean SF-36 health survey. J Korean Soc Health Stat 2003;28:3–24 [Google Scholar]
- 20.Lee Y, Song J. A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. Korean J Clin Psychol 1991;10:98–113 [Google Scholar]
- 21.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337–43 [DOI] [PubMed] [Google Scholar]
- 22.Binder AI. Neck pain. Clin Evid (Online) 2008;4:1103. [PMC free article] [PubMed] [Google Scholar]
- 23.McReynolds TM, Sheridan BJ. Intramuscular ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc 2005;105:57–68 [PubMed] [Google Scholar]
- 24.Qin XY, Li XX, Berghea F, et al. Comparative study on Chinese medicine and western medicine for treatment of osteoarthritis of the knee in Caucasian patients. Zhongguo Zhen Jiu 2008;28:459–62 [PubMed] [Google Scholar]
- 25.Zaringhalam J, Manaheji H, Rastqar A, et al. Reduction of chronic non-specific low back pain: a randomised controlled clinical trial on acupuncture and baclofen. Chin Med 2010;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X, Du YH, Xiong J. Survey on clinical evidence of acupuncture therapy for fibromyalgia syndrome. Zhen Ci Yan Jiu 2011;36:230–5 [PubMed] [Google Scholar]
- 27.Witt CM, Jena S, Selim D, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol 2006;164:487–96 [DOI] [PubMed] [Google Scholar]
- 28.Sertel S, Herrmann S, Greten HJ, et al. Additional use of acupuncture to NSAID effectively reduces post-tonsillectomy pain. Eur Arch Otorhinolaryngol 2009;266: 919–25 [DOI] [PubMed] [Google Scholar]
- 29.Molsberger AF, Mau J, Pawelec DB, et al. Does acupuncture improve the orthopedic management of chronic low back pain–a randomized, blinded, controlled trial with 3 months follow up. Pain 2002;99:579–87 [DOI] [PubMed] [Google Scholar]
- 30.Kawakita K, Gotoh K. Role of polymodal receptors in the acupuncture-mediated endogenous pain inhibitory systems. Prog Brain Res 1996;113:507–23 [DOI] [PubMed] [Google Scholar]
- 31.Cashman JN. The mechanisms of action of NSAIDs in analgesia. Drugs 1996;52(Suppl 5):13–23 [DOI] [PubMed] [Google Scholar]