Abstract
Purpose
To describe peripheral defocus when myopic eyes are corrected with spherical and center-distance multifocal soft contact lenses while looking at distance and near.
Methods
Twenty-five young adults with spherical contact lens-corrected refractive error of −0.50 to −6.00 D participated. Refractive error of each participant’s right eye was measured while it wore a spherical soft contact lens (Biofinity) and again while it wore a center-distance multifocal soft contact lens with a +2.50-D add (Biofinity Multifocal "D"). Measurements were made centrally and along the horizontal meridian at ±20°, ±30°, and ±40° from the line of sight at distance and near (3.33-D demand).
Results
The mean (±SD) age and spherical equivalent refractive error were 23.8 ± 1.3 years and −3.62 ± 1.56 D, respectively. At distance, the multifocal contact lens resulted in significantly more myopic defocus than the spherical contact lens at the 40° and 30° locations on the nasal retina and at the 20° and 30° locations on the temporal retina (p<0.0001). When accommodating to a near target, peripheral defocus was more myopic with the multifocal lens than with the spherical lens (p<0.0001). When viewing the near target with the spherical lens, participants experienced foveal hyperopic defocus and peripheral hyperopic defocus at all but one peripheral location. While participants also experienced foveal hyperopic defocus with the multifocal when looking at near, peripheral defocus was minimal (not significantly different than zero) at several locations (i.e., peripheral emmetropia).
Conclusions
The center-distance multifocal lens created peripheral myopic defocus when looking at distance. When looking at near, the multifocal lens resulted in relatively more myopic (less hyperopic) peripheral defocus than the spherical lens. The defocus profiles experienced with the multifocal contact lens in this study make it a good candidate for studies seeking to examine the effect of peripheral myopic defocus on myopia progression in children.
Keywords: myopia, soft contact lens, bifocal, multifocal, peripheral defocus, accommodation
Peripheral hyperopic retinal defocus was first suggested as a risk factor for myopia in the 1970s.1 Since then, experiments in animal models have provided convincing evidence that peripheral retinal defocus is capable of modifying eye growth even in the presence of a clear foveal image.2, 3 Based on these experiments in animals, it has been hypothesized that peripheral hyperopic defocus in the human eye causes accelerated eye growth and that optical lenses that either eliminate peripheral hyperopic defocus or produce myopic peripheral defocus slow the progression of myopia in children.4
Although uncorrected myopic eyes and emmetropic eyes that ultimately become myopic typically exhibit a hyperopic relative peripheral refraction (RPR) in the horizontal meridian of the eye,5–10 studies have failed to find a meaningful association between the amount of relative peripheral hyperopia in uncorrected eyes and the onset or progression of myopia in children.11, 12 That being said, uncorrected refractive error measurements do not completely describe the peripheral defocus experienced when wearing refractive correction; single vision spectacle lenses that are prescribed to correct myopia have been shown to increase the amount of peripheral hyperopic defocus experienced by myopic eyes.13–15 Studies in animals have found that brief periods of unrestricted vision completely negate the ocular growth signal produced by otherwise full-field hyperopic retinal blur created by a minus lens16–19 and that myopic defocus is a stronger signal to slow eye growth than hyperopic defocus is a signal to accelerate eye growth.20 These data suggest that optical designs incorporating myopic defocus may be a feasible option for slowing myopia progression.
A recent study of myopic children wearing either single vision spectacle lenses or progressive addition lenses (PALs) found that PALs resulted in myopic peripheral defocus on the superior retina (where PALs cause the greatest amount of myopic defocus) while many children wearing single vision spectacles had hyperopic peripheral defocus on the superior retina. Superior myopic peripheral defocus was associated with slower central myopia progression than superior hyperopic defocus, which supports the hypothesis that peripheral myopic defocus slows the progression of myopia.21
Contact lenses are an ideal way to deliver myopic defocus 360° in the periphery because the lens stays relatively centered with eye movements. Several contact lens designs have been studied to evaluate their ability to slow myopia progression. Studies in which myopic children were fitted with orthokeratology lenses have reported decreases in axial elongation,22–26 including one clinical trial.27 The reduction in axial growth with orthokeratology has been hypothesized to be due to the myopic shift in peripheral retinal defocus caused by the corneal shape changes induced by the lenses.28–30 Short-term studies utilizing soft bifocal contact lens designs have reported slower myopia progression in children.31, 32 That being said, no multi-year clinical trial results utilizing soft bifocal contact lenses are available, and the reported presence of a myopic shift in peripheral defocus with soft bifocal contact lenses has been variable.30, 33
Based on the theory that reducing peripheral hyperopic defocus slows myopia progression, a center-distance multifocal design that delivers clear foveal vision with plus power outside of the central distance zone is desired for attempting to control myopia. Many of the commercially available multifocal lenses in the US are center-near designs (full add power in the center transitioning to the distance power in the periphery), which is opposite of the desired power profile to reduce peripheral hyperopic defocus. Center-distance concentric ring designs (alternating rings of full distance and full near power) provide a peripheral myopic shift in defocus; however, autorefraction measurements of concentric ring designs have been reported to be variable,31, 34 possibly due to the close spacing of the alternating distance and near zones. Peripheral defocus has been successfully measured through lenses that include a gradient increase in add power,32 including the commercially available Proclear Multifocal “D” hydrogel lens (CooperVision, Fairport, NY).33, 35
If soft multifocal contact lenses are to be used to attempt to slow the progression of myopia in children, it is important to quantify the effect of these lenses on peripheral defocus. The Biofinity Multifocal “D” lens (CooperVision) is a newer, silicone-hydrogel contact lens with a center-distance design and gradient increase in add power that has not been previously evaluated in the literature. Based on these lens attributes, we chose to examine the ability of this lens to create a peripheral myopic change in defocus. The purpose of this study was to determine the effect of a spherical and a center-distance multifocal soft contact lens on peripheral defocus when viewing at both distance and near.
METHODS
Twenty-five myopic young adults with spherical contact lens-corrected refractive error of −0.50 to −6.00 D participated. The study was approved by the University of Houston Committee for the Protection of Human Subjects and was conducted in accordance with the tenets of the Declaration of Helsinki. Each participant provided written informed consent prior to being enrolled.
All participants completed an examination that included a standardized subjective refraction (most plus, least minus to best visual acuity) and a slit lamp examination. Participants were non-presbyopic, free from ocular disease, did not wear rigid gas permeable contact lenses, and had no history of ocular trauma or surgery. Because the contact lenses fitted in this study were spherical (did not correct astigmatism), participants were required to be correctable to 20/30 or better with a spherical refractive correction of −0.50 to −6.00 D and had less than 1.25 D of astigmatism.
Contact Lenses
The right eye of each participant was fitted in random order with both Biofinity sphere soft contact lenses and Biofinity Multifocal “D” lenses with a +2.50-D add based on the vertex-adjusted spherical equivalent manifest refraction. The Biofinity sphere lens is a silicone-hydrogel lens (comfilcon A) with 48% water content. The lens has an 8.6 base curve, overall diameter of 14.0 mm, and an 8.0 mm optic zone. The Biofinity Multifocal “D” lens is made of the same material and has the same base curve and overall diameter as the Biofinity sphere. The “D” lens is a center-distance multifocal design that, according to the manufacturer, has (from the center of the lens moving outward) a central spherical distance zone, a progressive zone of increasing plus power, and an outer spherical zone with the full add power. Prior to making measurements, the fit of each lens was assessed after allowing at least 5 minutes for the lens to settle.
Instrumentation
A Grand Seiko WAM-5500 open-field autorefractor (Grand Seiko Co. Ltd., Hiroshima, Japan) was used to make refractive error measurements of the right eye while the left eye was patched. The instrument housing was modified to allow for measurements out to ±40° from the line of sight at both distance and near. For distance measurements, a laser diode emitting red light was placed in holding wells mounted on top of the instrument that were positioned to allow for measurements in 10° increments from the line of site. The same laser holding wells also allowed for a near point rod to be placed at the same locations for the purpose of near measurements. A Maltese cross placed at 30 cm (a 3.33-D near demand) was used as the near target, and participants were reminded to keep the near target as clear as possible at all times during testing.
For this experiment, measurements were made centrally and at ±20°, ±30°, and ±40° from the line of sight. For peripheral measurements, the participant’s head was turned to point at the target while keeping the eye in primary gaze in order to minimize any contact lens decentration that might be caused by turning the eye. The participant’s head placement was visually inspected by the examiner prior to measurements at each location. The side on which measurements were made first (nasal or temporal) was randomized for each lens type within a person.
A total of 10 autorefraction measurements were made at each location. The measurement axis of the Grand Seiko autorefractor, which uses an approximately 2.3-mm measurement beam,36, 37 was centered within the entrance pupil for each measurement to ensure accurate peripheral measurements.38 Autorefraction measurements were exported directly into a spreadsheet on an attached computer. Ten measurements at each location were converted to power vectors (M, J0, and J45) using a previously described method and were averaged.39 To calculate the near defocus profile experienced by the eye with each lens, the eye’s average autorefraction defocus measurement (M) at each location, which consists of the combined optics of the accommodating eye and the contact lens, was subtracted from the near demand (3.33 D). After completing all measurements at near, distance measurements with each lens commenced 30 minutes after instilling the first of two drops of 1% tropicamide separated by 5 minutes. Cycloplegia was utilized for distance measurements to ensure that any differences between the lenses were due to the optics of the lens and not due to unexpected fluctuations in accommodation. Measurements at distance were also made without correction.
Statistical Methods
Data analyses were conducted using STATA 12.1 (StataCorp, College Station, TX). Repeated-measures analyses of variance were used to determine whether differences in defocus (M), J0 astigmatism, and J45 astigmatism differed by lens type (sphere or multifocal), retinal location, and testing distance. The magnitude of the contact lens correction was included as a covariate to determine whether contact lens power was associated with the change in relative peripheral defocus caused by the contact lens. When appropriate, post-hoc t-test comparisons were performed using the method described by Tukey and the appropriate mean square error from the model. Statistical significance was set at the alpha < 0.05 level. T-tests were used to determine whether defocus at a specific location was significantly different than zero. Statistical significance was determined at the alpha < 0.05 level using p-values that were adjusted for multiple comparisons using the method described by Benjamini and Hochberg.40
RESULTS
Of the 25 myopic participants, 13 (52%) were female. The mean ± SD age was 23.8 ± 1.3 years (range: 22 to 27 years), and the mean spherical equivalent refractive error was −3.62 ± 1.56 D. Of the 25 participants, 16 had less than 0.50 D of astigmatism, 22 had less than 1.00 D of astigmatism, and all participants had less than 1.25 D of astigmatism.
Defocus (M)
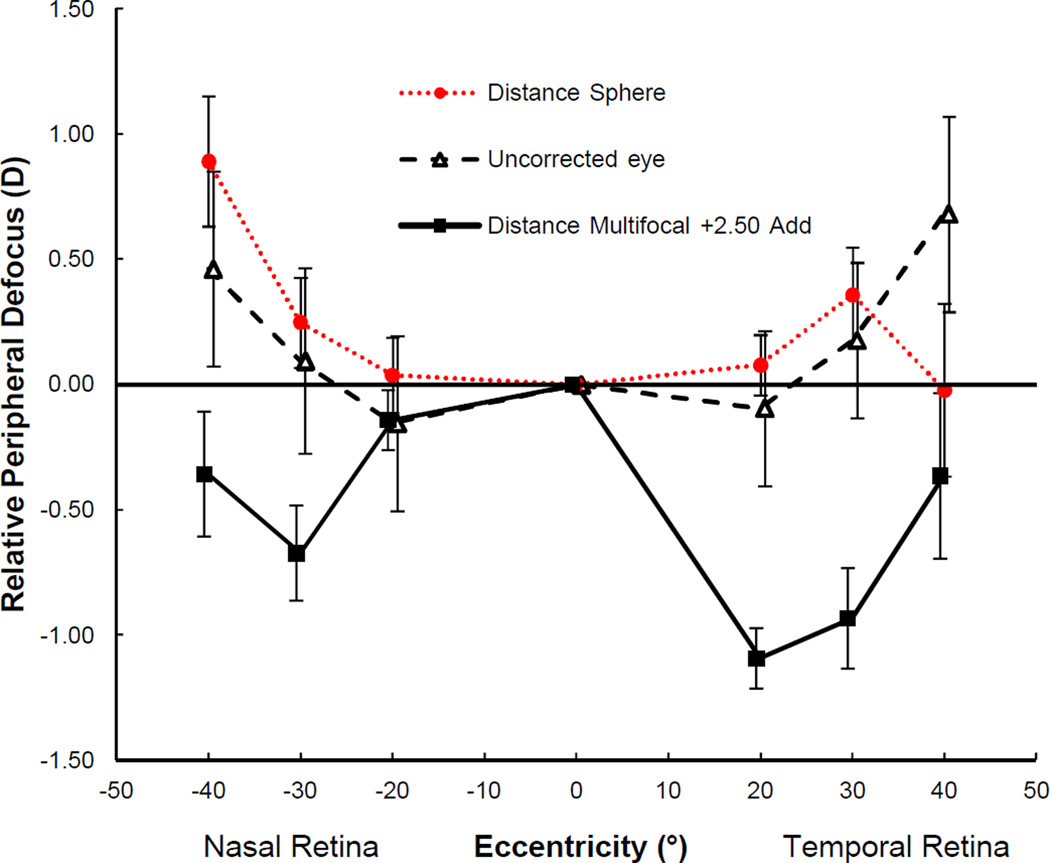
Relative peripheral defocus (peripheral defocus minus central defocus) measured at distance while wearing each contact lens and when the eye was uncorrected is shown in Figure 1. When looking at distance, the difference in peripheral defocus between the spherical and multifocal lens depended on the retinal location that was measured (p < 0.0001). The multifocal contact lens resulted in significantly more myopic defocus than the spherical contact lens at the 40° and 30° locations on the nasal retina and at the 20° and 30° locations on the temporal retina (all p < 0.05; Tukey). The spherical contact lens did not result in significant changes in relative peripheral defocus compared to the unaided eye (RPR).
Figure 1.
Relative peripheral defocus of the uncorrected eye and the sphere and multifocal soft contact lens corrected eye at distance. Peripheral values are normalized to the fovea (peripheral defocus minus central defocus). Error bars represent SEM. A color version of this figure is available online at www.optvissci.com.
When examining the effect of contact lens power on the contact lens-induced change in relative peripheral defocus at distance, the association was different for the spherical and multifocal lens (lens type by lens power interaction; p = 0.039). The association between lens power and the type of lens (spherical or multifocal) did not depend on the retinal location measured (lens type by lens power by retinal location interaction; p = 0.34). With the spherical contact lens, every diopter of more negative contact lens power was associated with a 0.13-D less hyperopic change in relative peripheral defocus (p = 0.027). Restating this result, the change in peripheral defocus was slightly more hyperopic when correcting lower amounts of myopia. With the multifocal lens, the lens power was not associated with the change in relative peripheral defocus caused by the contact lens (p = 0.60). In other words, the multifocal lens resulted in a consistent myopic change in peripheral defocus regardless of the lens power prescribed.
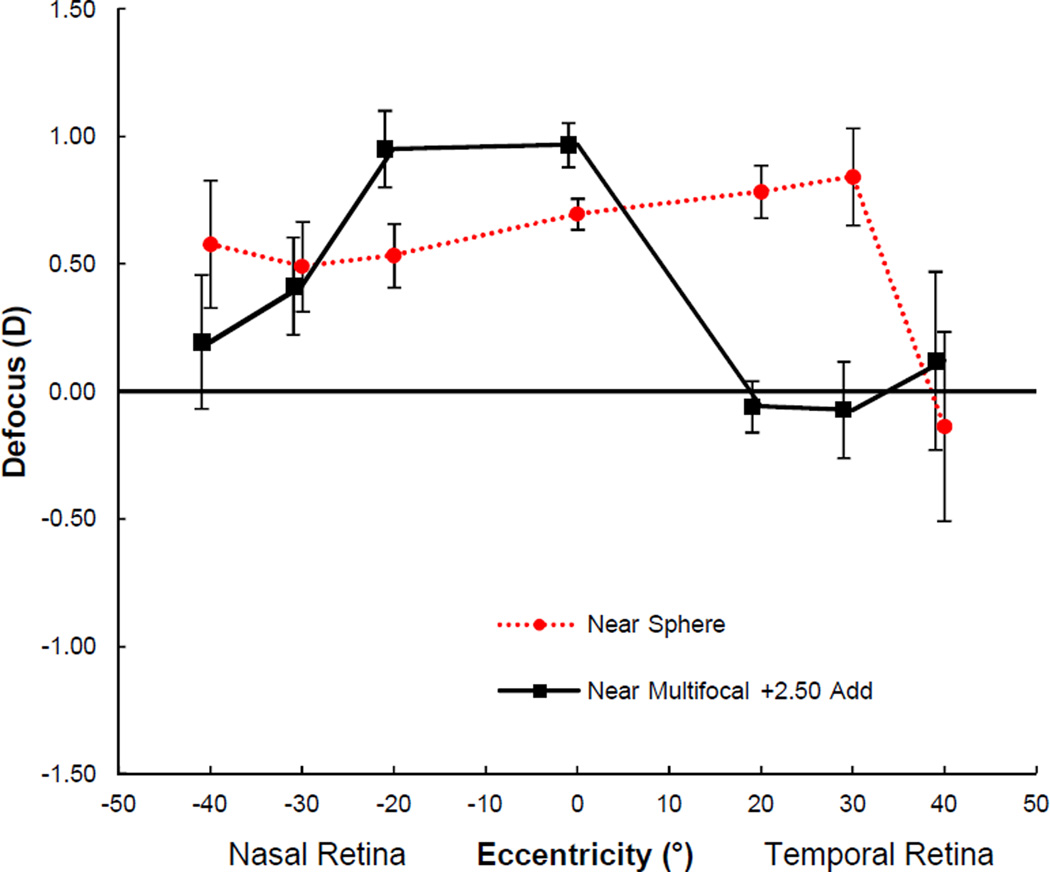
The defocus profile when accommodating to a near target at 30 cm (a 3.33-D demand) is shown in Figure 2. At near, differences in defocus at each location again depended on the lens type (p < 0.0001). The multifocal lens resulted in more myopic defocus than the spherical lens at the 40° nasal and 20° and 30° temporal locations (range of myopic shifts: 0.91 to 0.38 D; all p < 0.05; Tukey) and more hyperopic defocus at both the 20° nasal location (0.42 D) and the central location (0.27 D; both p < 0.05; Tukey). When viewing the near target with the spherical lens, participants experienced hyperopic defocus at all locations measured (all p < 0.04), with the exception of the 40° temporal location (p = 0.72). When viewing the near target with the multifocal lens, although hyperopic defocus was experienced centrally (accommodative lag), peripheral defocus was not significantly different than zero at the 40° and 30° nasal locations and at the 20°, 30°, and 40° temporal locations (all p > 0.09). In other words, participants experienced peripheral emmetropia in multiple peripheral locations when viewing a near target with the multifocal lens but experienced peripheral hyperopia when viewing the same target with the spherical contact lens.
Figure 2.
Peripheral defocus with spherical and multifocal soft contact lens when viewing a 30cm near target. Error bars represent SEM. A color version of this figure is available online at www.optvissci.com.
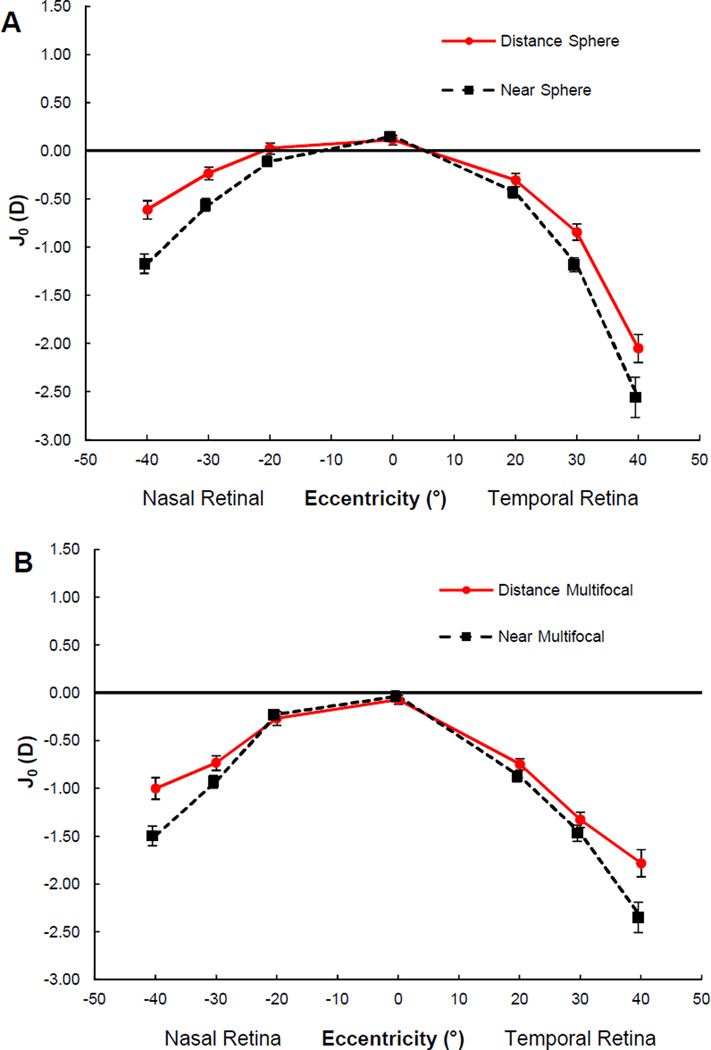
Astigmatism (J0 and J45)
J0 astigmatism when looking at distance and near is shown for both the spherical contact lens (Figure 3a) and the multifocal contact lens (Figure 3b). Peripheral J0 increased significantly when participants accommodated from distance to near (p < 0.0001), and the increase in peripheral J0 due to accommodation was symmetric. The changes in J0 with accommodation did not differ between the spherical and multifocal contact lens (p = 0.48). With the exception of the 40° temporal location, peripheral J0 astigmatism was slightly greater with the multifocal lens than the spherical contact lens (all p < 0.001), possibly due to the gradient increase in add power of the multifocal lens. That being said, the differences were clinically small.
Figure 3.
J0 astigmatism measured at distance and near with the spherical contact lens (A) and the multifocal contact lens (B). Error bars represent SEM. A color version of this figure is available online at www.optvissci.com.
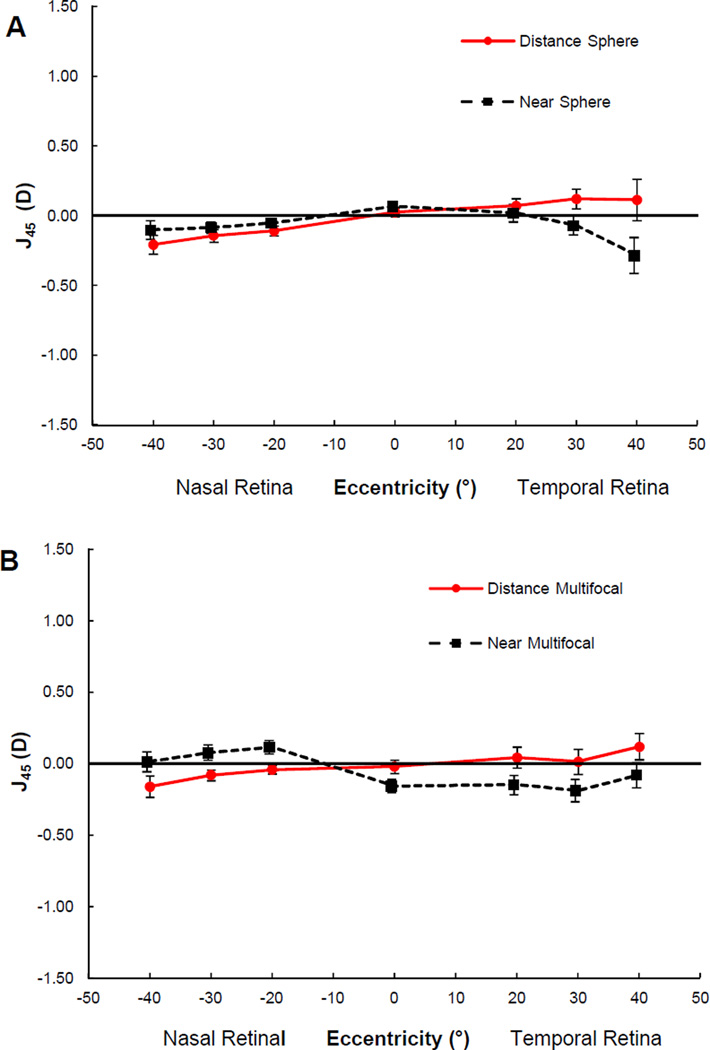
J45 astigmatism measured when looking at distance and near is shown for both the spherical contact lens (Figure 4a) and the multifocal contact lens (Figure 4b). Differences in peripheral J45 with accommodation depended on the location measured (p < 0.001) and again were not significantly different between the sphere and multifocal (p = 0.47). The magnitude and differences in J45 were clinically small.
Figure 4.
J45 astigmatism measured at distance and near with the spherical contact lens (A) and the multifocal contact lens (B). Error bars represent SEM. A color version of this figure is available online at www.optvissci.com.
DISCUSSION
When looking at distance, the center-distance multifocal lens utilized in this study (Biofinity Multifocal “D” with +2.50-D add) resulted in a significant peripheral myopic shift in defocus compared to the spherical contact lens. The hyperopic peripheral defocus profile with the spherical soft contact lens in this study is consistent with reports by several groups of peripheral hyperopic defocus when wearing spherical soft contact lenses41, 42 and single vision spectacle lenses.14, 15 Although a study by Shen et al. reported a slight myopic change in peripheral defocus when myopic eyes wore Acuvue 2 spherical soft contact lenses (Johnson & Johnson; Jacksonville, FL), the overall resultant peripheral refraction was still hyperopic.42 Conversely, a study of myopic eyes by Kang et al. reported a hyperopic shift in peripheral defocus with Proclear Sphere contact lenses (CooperVision).41 One previous study has reported peripheral myopic defocus with spherical soft contact lenses (1-Day Acuvue Moist; Johnson & Johnson); however, that study only included eyes with high myopia (range: −5.00 to −8.00 D) while our study included lower myopic refractive errors (range: −0.50 to −6.00 D).13
Several studies have evaluated peripheral defocus using a center-distance multifocal design. A study that examined the effect of the Proclear Multifocal “D” design with a +2.00-D add on four participants (three emmetropes and one low myope) using a scanning Hartmann-Shack wavefront system (4-mm analysis diameter) found peripheral myopic defocus, but only on the temporal retina.33 Lopes-Ferreira et al. also examined the Proclear Multifocal “D” design with add powers from +1.00 to +4.00 D in 20 emmetropic participants out to ±35° in the horizontal field. They found no significant change with the +1.00-D add, a myopic shift that was similar at all eccentricities with the +2.00-D add (i.e., the myopic shift was not greater peripherally than centrally), and a significantly greater myopic shift with increasing eccentricity with the +3.00-D and +4.00-D add powers.35 In a similar study of Proclear Multifocal “D” lenses that including 28 myopic young adults, the same group found significant myopic changes in relative peripheral defocus compared to the uncorrected eye at 35° in the nasal and temporal retina of −0.13 D and −0.41 D, respectively with a +2.00-D add and −0.73 D and −1.54 D, respectively with a +3.00-D add.43 In the present study of myopic young adults using the Biofinity Multifocal “D” lens with a +2.50-D add, we found significant myopic changes in relative peripheral defocus compared to the uncorrected eye at 30° and 40° of −0.77 D and −0.82 D, respectively on the nasal retina and myopic changes of −1.11 D and −1.04 D, respectively on the temporal retina. Though another study that measured peripheral defocus out to 30° with the Proclear Multifocal “D” lens (+2.00-D add) in myopic eyes did not find peripheral myopic defocus,30 participants were instructed to turn their eyes for peripheral measurements, which the authors suggested may have resulted in lens decentration that affected peripheral measurements. Participants turned their head in the present study while keeping their eyes in primary gaze for peripheral measurements.
While the change in relative peripheral defocus caused by the Biofinity Multifocal “D" lens in our study did not depend on the power of the contact lens (i.e., the induced myopic change in peripheral defocus was consistent across lens powers), this was not the case for the spherical lens. Although the Biofinity sphere resulted in significantly more relative peripheral hyperopia than the Biofinity multifocal at multiple peripheral locations, the change in peripheral defocus caused by the Biofinity sphere was slightly more hyperopic when correcting lower amounts of myopia. Because the Biofinity sphere is reported to have aspheric optics, variations in asphericity across the optic zone that depend on the lens power may explain the association found between lens power and the change in peripheral defocus. This association should be verified in future studies because differences in peripheral defocus as lens power is changed could have implications for myopia progression, assuming the hypothesis that peripheral hyperopia causes myopia progression is correct. In contrast, a study by Kang et al. evaluating Proclear Sphere contact lenses found similar increases in relative peripheral hyperopia when correcting both low and moderate amounts of myopia with that lens.41 The consistent change in peripheral defocus across lens powers with the Biofinity Multifocal “D” lens is a desired attribute in a lens that might be used to attempt to control myopia progression.
When looking at a near target, a central lag of accommodation was measured for both the spherical and multifocal lens, and the differences in peripheral defocus between the lens types was not as large as when looking at a distant object. The amount of central hyperopic defocus (accommodative lag) found in this study with both lens types is consistent with previously reported lag amounts among myopic children44, 45 and demonstrates that the study participants did accommodate when viewing the near target with the multifocal contact lens. Although other studies have reported a lead of accommodation with multifocal contact lenses, these studies were conducted with either center-near designs46 or concentric ring designs,34 which may partially account for the differences between studies. Although the near target was viewed monocularly in this study, which eliminates accommodation due to convergence that is present under binocular conditions, a study using the same instrument and target utilized in our study found the difference between monocular and binocular accommodative lag measurements to be less than 0.12 D for a 3.00-D demand, which is clinically small.34
Though the central amount of hyperopic defocus with the multifocal lens was slightly greater than with the spherical lens when viewing the near target, the multifocal created peripheral emmetropia (especially on the temporal retina) whereas the spherical lens resulted in peripheral hyperopic defocus at all but one peripheral location measured. Brief periods of clear vision have been shown to completely negate the “grow” signal produced by hyperopic retinal blur,16–19 and myopic defocus has been shown to be a stronger signal to slow eye growth than hyperopic defocus is a signal to accelerate eye growth.20 Based on these observations in animal models, even occasional periods of peripheral myopic defocus with the multifocal lens when viewing at distance may provide an adequate signal to slow eye growth. The myopic peripheral defocus at distance combined with decreased peripheral hyperopic defocus at near with the multifocal lens could potentially explain the reduction in myopia progression previously reported in a study that used a center-distance multifocal with a design similar to the lens utilized in our study.47
With the spherical lens, a sudden myopic shift was observed at the 40° temporal location compared to the adjacent 30° temporal location when looking at distance (Figure 1) and at near (Figure 2). A similar sudden myopic shift was not observed at the 40° nasal location with the spherical lens. A possible explanation for the abrupt change in defocus between the 30° and 40° temporal retinal locations is that slight lateral decentration of the spherical contact lens in primary gaze resulted in the junction between the optic zone and the peripheral curve of the lens falling across the autorefractor’s measurement beam at this location. This explanation is supported by the abrupt shift occurring regardless of viewing distance and only at the 40° temporal location.
One might wonder whether accommodation results in a change in the shape of the peripheral defocus profile. Relative peripheral refraction at near does not represent the defocus experienced by the retina when viewing a near object because it eliminates the effect of central accommodative lag; however, the difference in relative peripheral refraction between distance and near describes the change in the peripheral defocus profile that occurs due to accommodation. The change in relative peripheral refraction at each retinal location did not differ between the spherical and multifocal lens (p = 0.17). Statistically significant changes in relative peripheral refraction with accommodation were only observed at the 40° nasal and 40° temporal locations where myopic changes of −0.71 D and −0.65 D were observed, respectively (both p ≤ 0.018). The peripheral myopic shift in relative peripheral refraction can be observed when examining the shape of the distance and near optical profiles of the sphere and multifocal lenses in Figures 1 and 2. The myopic shift 40° nasally and temporally on the retina resulted in an additional small reduction in hyperopic peripheral defocus when looking at near.
Previous studies have reported conflicting findings regarding any change in relative peripheral refraction with accommodation. Smith et al. reported a peripheral myopic shift in the retinal image shell with accommodation levels greater than 3.00 D at 50° and 60° eccentricity.48 A study in which myopic eyes accommodated 3.33 D also reported a significant myopic shift with accommodation of roughly −0.50 D on the 30° nasal and 40° temporal retina and roughly −0.75 D on the 40° nasal retina.49 While Lundström et al. found a myopic shift in the periphery of emmetropic eyes when accommodating 4.00 D, they did not find a myopic shift when myopic eyes accommodated the same amount.50 Two other studies reported no change in relative peripheral refraction with accommodative demands of either 2.50 D or 3.00 D out to 30° eccentricity,51, 52 and another study with up to a 4.00-D demand found no difference in emmetropic eyes out to 45° eccentricity.53 A study by Walker and Mutti has also reported a roughly 0.25-D hyperopic shift 30° on the temporal retina when accommodating 3.00 D.54 Overall, when changes are reported due to accommodation, the changes tend to occur in the far periphery.
Changes in peripheral astigmatism with accommodation found in this study were also consistent with a previous report. Whatham et al. noted increases in J0 astigmatism with accommodation.49 A similar increase in J0 astigmatism that was most prominent in the far periphery was observed in the present study when participants accommodated while wearing both the spherical and multifocal contact lens. Though we also found small differences in J45 astigmatism with accommodation, they were clinically small.
A limitation of the present study is that all measurements were made on young adults rather than children. We would expect the relative change in peripheral defocus due to the contact lens to be the same for both a child and a young adult. The factor determining the final amount of peripheral defocus when looking at distance through the bifocal contact lens would be expected to be the eye’s specific uncorrected relative peripheral refraction (i.e., the relative defocus prior to putting on the contact lens). When looking at near, it is also possible that a child might accommodate differently when wearing a bifocal contact lens than the young adults in this study. A recent study in children examining a dual-focus/concentric-ring bifocal contact lens design found that children still accommodated to a near target when wearing the lens.31 Though the Biofinity multifocal lens utilized in this study is not a concentric ring design, a recent study by Kollbaum et al. found that visual performance was the same with both a concentric ring multifocal (MiSight; CooperVision) and the Proclear Multifocal “D” lens, which is similar in design to the lens used in the present study.55 This finding suggests that it is reasonable to expect that children would accommodate when wearing the Biofinity Multifocal “D” lens similar to the young adults in the present study. That being said, peripheral defocus at near should be measured in any study following children over time to confirm their accommodative state.
There are currently no data from a long-term randomized study to guide us regarding the specific amount of peripheral myopic shift that is necessary to potentially slow myopia progression or whether defocus in certain peripheral locations might be more effective at slowing myopia progression (i.e., we currently do not have data to inform us of the ideal optical profile). That being said, the progressive addition and single vision spectacle lens data described in the introduction section from a randomized clinical trial found that myopic defocus at 30 degrees on a single retinal quadrant when looking at distance while wearing PALs was associated with slowed progression.21 Data from the same study found that children still had a significant amount of accommodative lag when viewing through a +2.00-D add at near (i.e., a treatment effect was still present despite foveal hyperopic defocus during near viewing due to accommodative lag).56 This finding in children is consistent with aforementioned data from animal models finding that the hyperopic defocus “grow” signal produced by a full-field minus lens can be negated by removing the minus lens for brief periods16–19 and that myopic defocus is a stronger signal to slow eye growth than hyperopic defocus is a signal to accelerate eye growth.20 The Biofinity Multifocal “D” lens produced myopic defocus on both the nasal and temporal retina when viewing at distance and would presumably have the same effect 360° around the peripheral retina. Based on the animal and clinical trial data just described, the peripheral myopia at distance and elimination of hyperopic defocus at some peripheral retinal locations when looking at near would be beneficial.
Data from two clinical studies also support the investigation of the Biofinity Multifocal “D” lens in long-term studies. In a non-randomized pilot study of children wearing the Proclear Multifocal “D” lens (+2.00-D add), which is similar in design to the Biofinity Multifocal “D” lens, a significant 51% reduction in axial eye growth after two years was found compared to children wearing the Proclear Sphere lens.47 In another study, a novel gradient contact lens resulted in a 33% reduction in axial elongation after one year despite the fact that the lens only produced a large myopic shift on the temporal retina (nasal field), with little effect on hyperopic defocus on the nasal retina (temporal field).32 The Biofinity Multifocal “D” lens in the present study resulted in a significant myopic shift in peripheral defocus at locations in both the nasal and temporal fields. The results of the clinical studies above combined with the profile found in the present study provide support for this lens design as a good starting point in a clinical trial setting to further our understanding of the effect of peripheral defocus on myopia progression in a randomized sample. While this design is unlikely to ultimately be the perfect design, the evidence above suggests that it would be a good initial candidate lens to utilize in a randomized sample in order to further our knowledge regarding the efficacy of a myopic shift in defocus. Longitudinal data would provide the information needed for optimization of a design in the future.
In summary, when worn by myopic eyes, the center-distance Biofinity Multifocal “D” lens with a +2.50-D add created peripheral myopic defocus when looking at distance. We also examined the defocus profile with each lens when looking at near through both spherical and multifocal contact lenses, which has not previously been reported. Though the defocus profiles of the multifocal and spherical contact lens were similar centrally when looking at a near target, the multifocal lens resulted in a reduction in peripheral hyperopic defocus compared to the spherical lens and eliminated hyperopic defocus at multiple peripheral retinal locations. The defocus profiles experienced with the multifocal contact lens in this study make it a good candidate for clinical studies seeking to examine the effect of peripheral myopic defocus on myopia progression in children.
ACKNOWLEDGMENTS
NIH T35-EY007088 (CEK) and P30-EY07551; Contact lenses provided by CooperVision. The authors thank Chris Kuether for his assistance in modifying the Grand Seiko autorefractor utilized in this study. The authors have no proprietary or financial interests in any of the products utilized in this study.
REFERENCES
- 1.Hoogerheide J, Rempt F, Hoogenboom WP. Acquired myopia in young pilots. Ophthalmologica. 1971;163:209–215. doi: 10.1159/000306646. [DOI] [PubMed] [Google Scholar]
- 2.Irving EL, Callender MG, Sivak JG. Inducing ametropias in hatchling chicks by defocus--aperture effects and cylindrical lenses. Vision Res. 1995;35:1165–1174. doi: 10.1016/0042-6989(94)00235-e. [DOI] [PubMed] [Google Scholar]
- 3.Smith EL, 3rd, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49:2386–2392. doi: 10.1016/j.visres.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith EL., 3rd Prentice Award Lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011;88:1029–1044. doi: 10.1097/OPX.0b013e3182279cfa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atchison DA, Pritchard N, Schmid KL. Peripheral refraction along the horizontal and vertical visual fields in myopia. Vision Res. 2006;46:1450–1458. doi: 10.1016/j.visres.2005.10.023. [DOI] [PubMed] [Google Scholar]
- 6.Millodot M. Effect of ametropia on peripheral refraction. Am J Optom Physiol Opt. 1981;58:691–695. doi: 10.1097/00006324-198109000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Logan NS, Gilmartin B, Wildsoet CF, Dunne MC. Posterior retinal contour in adult human anisomyopia. Invest Ophthalmol Vis Sci. 2004;45:2152–2162. doi: 10.1167/iovs.03-0875. [DOI] [PubMed] [Google Scholar]
- 8.Seidemann A, Schaeffel F, Guirao A, Lopez-Gil N, Artal P. Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. J Opt Soc Am (A) 2002;19:2363–2373. doi: 10.1364/josaa.19.002363. [DOI] [PubMed] [Google Scholar]
- 9.Mutti DO, Sholtz RI, Friedman NE, Zadnik K. Peripheral refraction and ocular shape in children. Invest Ophthalmol Vis Sci. 2000;41:1022–1030. [PubMed] [Google Scholar]
- 10.Mutti DO, Hayes JR, Mitchell GL, Jones LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. The CLEERE Study Group. Invest Ophthalmol Vis Sci. 2007;48:2510–2519. doi: 10.1167/iovs.06-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mutti DO, Sinnott LT, Mitchell GL, Jones-Jordan LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K. Relative peripheral refractive error and the risk of onset and progression of myopia in children. Invest Ophthalmol Vis Sci. 2011;52:199–205. doi: 10.1167/iovs.09-4826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sng CC, Lin XY, Gazzard G, Chang B, Dirani M, Lim L, Selvaraj P, Ian K, Drobe B, Wong TY, Saw SM. Change in peripheral refraction over time in Singapore Chinese children. Invest Ophthalmol Vis Sci. 2011;52:7880–7887. doi: 10.1167/iovs.11-7290. [DOI] [PubMed] [Google Scholar]
- 13.Backhouse S, Fox S, Ibrahim B, Phillips JR. Peripheral refraction in myopia corrected with spectacles versus contact lenses. Ophthalmic Physiol Opt. 2012;32:294–303. doi: 10.1111/j.1475-1313.2012.00912.x. [DOI] [PubMed] [Google Scholar]
- 14.Lin Z, Martinez A, Chen X, Li L, Sankaridurg P, Holden BA, Ge J. Peripheral defocus with single-vision spectacle lenses in myopic children. Optom Vis Sci. 2010;87:4–9. doi: 10.1097/OPX.0b013e3181c078f1. [DOI] [PubMed] [Google Scholar]
- 15.Tabernero J, Vazquez D, Seidemann A, Uttenweiler D, Schaeffel F. Effects of myopic spectacle correction and radial refractive gradient spectacles on peripheral refraction. Vision Res. 2009;49:2176–2186. doi: 10.1016/j.visres.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 16.Shaikh AW, Siegwart JT, Jr., Norton TT. Effect of interrupted lens wear on compensation for a minus lens in tree shrews. Optom Vis Sci. 1999;76:308–315. doi: 10.1097/00006324-199905000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Schmid KL, Wildsoet CF. Effects on the compensatory responses to positive and negative lenses of intermittent lens wear and ciliary nerve section in chicks. Vision Res. 1996;36:1023–1036. doi: 10.1016/0042-6989(95)00191-3. [DOI] [PubMed] [Google Scholar]
- 18.Zhu X, Winawer JA, Wallman J. Potency of myopic defocus in spectacle lens compensation. Invest Ophthalmol Vis Sci. 2003;44:2818–2827. doi: 10.1167/iovs.02-0606. [DOI] [PubMed] [Google Scholar]
- 19.Norton TT, Siegwart JT, Jr., Amedo AO. Effectiveness of hyperopic defocus, minimal defocus, or myopic defocus in competition with a myopiagenic stimulus in tree shrew eyes. Invest Ophthalmol Vis Sci. 2006;47:4687–4699. doi: 10.1167/iovs.05-1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu Y, Wildsoet C. The effect of two-zone concentric bifocal spectacle lenses on refractive error development and eye growth in young chicks. Invest Ophthalmol Vis Sci. 2011;52:1078–1086. doi: 10.1167/iovs.10-5716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berntsen DA, Barr CD, Mutti DO, Zadnik K. Peripheral defocus and myopia progression in myopic children randomly assigned to wear single vision and progressive addition lenses. Invest Ophthalmol Vis Sci. 2013 doi: 10.1167/iovs.13-11904. Epub ahead of print: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93:1181–1185. doi: 10.1136/bjo.2008.151365. [DOI] [PubMed] [Google Scholar]
- 23.Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30:71–80. doi: 10.1080/02713680590907256. [DOI] [PubMed] [Google Scholar]
- 24.Kakita T, Hiraoka T, Oshika T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Invest Ophthalmol Vis Sci. 2011;52:2170–2174. doi: 10.1167/iovs.10-5485. [DOI] [PubMed] [Google Scholar]
- 25.Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutierrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53:5060–5065. doi: 10.1167/iovs.11-8005. [DOI] [PubMed] [Google Scholar]
- 26.Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012;53:3913–3919. doi: 10.1167/iovs.11-8453. [DOI] [PubMed] [Google Scholar]
- 27.Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53:7077–7085. doi: 10.1167/iovs.12-10565. [DOI] [PubMed] [Google Scholar]
- 28.Kang P, Swarbrick H. Peripheral refraction in myopic children wearing orthokeratology and gas-permeable lenses. Optom Vis Sci. 2011;88:476–482. doi: 10.1097/OPX.0b013e31820f16fb. [DOI] [PubMed] [Google Scholar]
- 29.Queiros A, Gonzalez-Meijome JM, Jorge J, Villa-Collar C, Gutierrez AR. Peripheral refraction in myopic patients after orthokeratology. Optom Vis Sci. 2010;87:323–329. doi: 10.1097/OPX.0b013e3181d951f7. [DOI] [PubMed] [Google Scholar]
- 30.Ticak A, Walline JJ. Peripheral optics with bifocal soft and corneal reshaping contact lenses. Optom Vis Sci. 2013;90:3–8. doi: 10.1097/OPX.0b013e3182781868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118:1152–1161. doi: 10.1016/j.ophtha.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 32.Sankaridurg P, Holden B, Smith E, 3rd, Naduvilath T, Chen X, de la Jara PL, Martinez A, Kwan J, Ho A, Frick K, Ge J. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52:9362–9367. doi: 10.1167/iovs.11-7260. [DOI] [PubMed] [Google Scholar]
- 33.Rosen R, Jaeken B, Lindskoog Petterson A, Artal P, Unsbo P, Lundstrom L. Evaluating the peripheral optical effect of multifocal contact lenses. Ophthalmic Physiol Opt. 2012;32:527–534. doi: 10.1111/j.1475-1313.2012.00937.x. [DOI] [PubMed] [Google Scholar]
- 34.Tarrant J, Severson H, Wildsoet CF. Accommodation in emmetropic and myopic young adults wearing bifocal soft contact lenses. Ophthalmic Physiol Opt. 2008;28:62–72. doi: 10.1111/j.1475-1313.2007.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lopes-Ferreira D, Ribeiro C, Maia R, Garcia-Porta N, Queiros A, Villa-Collar C, Gonzalez-Meijome JM. Peripheral myopization using a dominant design multifocal contact lens. J Optom. 2011;4:14–21. [Google Scholar]
- 36.Bailey MD, Twa MD, Mitchell GL, Dhaliwal DK, Jones LA, McMahon TT. Repeatability of autorefraction and axial length measurements after laser in situ keratomileusis. J Cataract Refract Surg. 2005;31:1025–1034. doi: 10.1016/j.jcrs.2004.12.040. [DOI] [PubMed] [Google Scholar]
- 37.Fedtke C, Ehrmann K, Holden BA. A review of peripheral refraction techniques. Optom Vis Sci. 2009;86:429–446. doi: 10.1097/OPX.0b013e31819fa727. [DOI] [PubMed] [Google Scholar]
- 38.Fedtke C, Ehrmann K, Ho A, Holden BA. Lateral pupil alignment tolerance in peripheral refractometry. Optom Vis Sci. 2011;88:570–579. doi: 10.1097/OPX.0b013e31821041e2. [DOI] [PubMed] [Google Scholar]
- 39.Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci. 1997;74:367–375. doi: 10.1097/00006324-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 40.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc (B) 1995;57:289–300. [Google Scholar]
- 41.Kang P, Fan Y, Oh K, Trac K, Zhang F, Swarbrick H. Effect of single vision soft contact lenses on peripheral refraction. Optom Vis Sci. 2012;89:1014–1021. doi: 10.1097/OPX.0b013e31825da339. [DOI] [PubMed] [Google Scholar]
- 42.Shen J, Clark CA, Soni PS, Thibos LN. Peripheral refraction with and without contact lens correction. Optom Vis Sci. 2010;87:642–655. doi: 10.1097/OPX.0b013e3181ea16ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lopes-Ferreira D, Ribeiro C, Neves H, Faria-Ribeiro M, Queiros A, Villa-Collar C, Jorge J, Gonzalez-Meijome JM. Peripheral refraction with dominant design multifocal contact lenses in young myopes. J Optom. 2013;6:85–94. [Google Scholar]
- 44.Mutti DO, Mitchell GL, Hayes JR, Jones LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K. Accommodative lag before and after the onset of myopia. The CLEERE Study Group. Invest Ophthalmol Vis Sci. 2006;47:837–846. doi: 10.1167/iovs.05-0888. [DOI] [PubMed] [Google Scholar]
- 45.Nakatsuka C, Hasebe S, Nonaka F, Ohtsuki H. Accommodative lag under habitual seeing conditions: comparison between myopic and emmetropic children. Jpn J Ophthalmol. 2005;49:189–194. doi: 10.1007/s10384-004-0175-7. [DOI] [PubMed] [Google Scholar]
- 46.Madrid-Costa D, Ruiz-Alcocer J, Radhakrishnan H, Ferrer-Blasco T, Montes-Mico R. Changes in accommodative responses with multifocal contact lenses: a pilot study. Optom Vis Sci. 2011;88:1309–1316. doi: 10.1097/OPX.0b013e31822be35a. [DOI] [PubMed] [Google Scholar]
- 47.Walline JJ, Jones-Jordan LA. Axial elongation with corneal reshaping, soft bifocal, and spherical contact lens wear. Optom Vis Sci. 2012;89 E-abstract 120062. [Google Scholar]
- 48.Smith G, Millodot M, McBrien NA. The effect of accommodation on oblique astigmatism and field curvature of the human eye. Clin Exp Optom. 1988;71:119–125. [Google Scholar]
- 49.Whatham A, Zimmermann F, Martinez A, Delgado S, de la Jara PL, Sankaridurg P, Ho A. Influence of accommodation on off-axis refractive errors in myopic eyes. J Vis. 2009;9:1–3. doi: 10.1167/9.3.14. 14. [DOI] [PubMed] [Google Scholar]
- 50.Lundstrom L, Mira-Agudelo A, Artal P. Peripheral optical errors and their change with accommodation differ between emmetropic and myopic eyes. J Vis. 2009;9:1–11. doi: 10.1167/9.6.17. 17. [DOI] [PubMed] [Google Scholar]
- 51.Davies LN, Mallen EA. Influence of accommodation and refractive status on the peripheral refractive profile. Br J Ophthalmol. 2009;93:1186–1190. doi: 10.1136/bjo.2009.159053. [DOI] [PubMed] [Google Scholar]
- 52.Calver R, Radhakrishnan H, Osuobeni E, O'Leary D. Peripheral refraction for distance and near vision in emmetropes and myopes. Ophthalmic Physiol Opt. 2007;27:584–593. doi: 10.1111/j.1475-1313.2007.00518.x. [DOI] [PubMed] [Google Scholar]
- 53.Tabernero J, Schaeffel F. Fast scanning photoretinoscope for measuring peripheral refraction as a function of accommodation. J Opt Soc Am (A) 2009;26:2206–2210. doi: 10.1364/JOSAA.26.002206. [DOI] [PubMed] [Google Scholar]
- 54.Walker TW, Mutti DO. The effect of accommodation on ocular shape. Optom Vis Sci. 2002;79:424–430. doi: 10.1097/00006324-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 55.Kollbaum PS, Jansen ME, Tan J, Meyer DM, Rickert ME. Vision performance with a contact lens designed to slow myopia progression. Optom Vis Sci. 2013;90:205–214. doi: 10.1097/OPX.0b013e3182812205. [DOI] [PubMed] [Google Scholar]
- 56.Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci. 2012;53:640–649. doi: 10.1167/iovs.11-7769. [DOI] [PMC free article] [PubMed] [Google Scholar]