Abstract
Background
Human factors and ergonomics (HFE) approaches to patient safety have addressed five different domains: usability of technology; human error and its role in patient safety; the role of healthcare worker performance in patient safety; system resilience; and HFE systems approaches to patient safety.
Methods
A review of various HFE approaches to patient safety and studies on HFE interventions was conducted.
Results
This paper describes specific examples of HFE-based interventions for patient safety. Studies show that HFE can be used in a variety of domains.
Conclusions
HFE is a core element of patient safety improvement. Therefore, every effort should be made to support HFE applications in patient safety.
Keywords: Human factors, Patient safety, Human error
Introduction
Many patient safety incidents are related to lack of attention to human factors and ergonomics (HFE) in the design and implementation of technologies, processes, workflows, jobs, teams and sociotechnical systems. HFE is now recognised as a key discipline to help reduce or mitigate medication errors,1 2 to improve the design and implementation of health IT,3 and to eliminate hazards that contribute to patient falls.4 According to the International Ergonomics Association,5 ‘Ergonomics (or human factors)i is the scientific discipline concerned with the understanding of the interactions among humans and other elements of a system, and the profession that applies theoretical principles, data and methods to design in order to optimise human well-being and overall system performance.’ The objective of HFE-based system design is to improve wellbeing (eg, clinician and patient satisfaction) and overall system performance that includes patient safety.6 From an HFE viewpoint, patient safety activities should not only reduce and mitigate medical errors and improve patient safety, but also improve human wellbeing, such as job satisfaction, motivation and technology acceptance. For instance, patient safety programmes that increase the workload of already busy clinicians would not be considered well designed from the HFE perspective. In this paper we described various HFE approaches and contributions to patient safety, and then provide details on a few illustrative examples of HFE applications in patient safety.
HFE approaches and contributions to patient safety
In this section, we describe a few selected contributions of HFE to various patient safety domains. Other contributions of HFE to patient safety such as teamwork training are reviewed in other papers of this special issue7 and the Agency for Healthcare Research and Quality report on patient safety strategies.8 We also highlight mechanisms that link HFE to patient safety.
Various HFE approaches to patient safety
A significant focus of HFE in healthcare and patient safety has been the design of usable and safe medical devices and health IT,9 such as the redesign of code cart medication drawer.10 Health IT can contribute to patient safety by eliminating hazards,11 but can also create new hazards.12 Usability is one HFE design characteristic that can influence health IT's patient safety benefits, or lack thereof.3
Another major focus of HFE in patient safety has been understanding the nature of human error and identifying the mechanisms of human error involved in patient safety.13 14 The Swiss Cheese model of Reason15 describes the alignment of hazards (or ‘holes’) that can lead to an accident (eg, a patient safety event) and distinguishes between latent failures and active failures. Vincent and colleagues14 adapted Reason's Swiss Cheese model to patient safety, and described management decisions and latent failures that can influence error and create conditions that produce safety violations. In turn, these conditions create problems for care delivery and may lead to unsafe acts (ie, errors and violations), which may then produce an incident if the defences and barriers are not appropriate. The frameworks of Vincent and colleagues14 and Bogner16 can be used by healthcare organisations to investigate patient safety incidents.
Performance obstacles may endanger patients by making it difficult for clinicians to perform tasks and procedures safely.17 A range of physical (eg, lifting, injecting, charting), cognitive (eg, perceiving, attention, communicating, awareness) and social/behavioural (eg, motivation, decision-making) performance processes can influence patient safety.18 Performance obstacles have been identified for intensive care unit nurses,19 20 staff in outpatient surgery centers,21 and hospital nurses.22
Recently, HFE research in patient safety has focused on system resilience,23 or ‘the ability of systems to anticipate and adapt to the potential for surprise and failure’.24 Because not all errors may be prevented, HFE researchers have developed models to understand how errors can be detected, corrected, mitigated, and dealt with by operators.25 Strategies for error detection and recovery have been explored among nurses,26 in particular critical care nurses,27 and among pharmacists.28 29 Resilience engineering builds on and extends the work done by high-reliability organisation (HRO) researchers, in particular the HRO concept of mindfulness, that is, the ability to prepare for the unexpected and to be vigilant about hazards.30
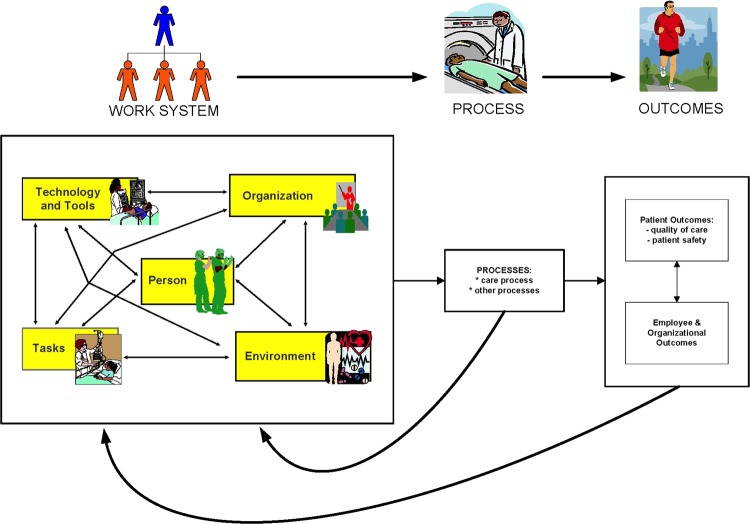
The first four HFE approaches focus on specific aspects of HFE and patient safety: usability of technology, human error, clinician performance and resilience. A number of HFE approaches have been proposed to describe more comprehensive systems of patient care, such as the systems approach proposed by Vincent and colleagues14 31 and the SEIPS (Systems Engineering Initiative for Patient Safety) model of work system and patient safety proposed by Carayon and colleagues.32 Vincent and colleagues14 defined seven types of system factors that can influence clinical practice and lead to patient safety incidents, such as patient factors, task and technology factors, and organisational and management factors. The SEIPS model of work system and patient safety32 identifies a slightly different set of system factors: individual factors (which include characteristics of the staff and patient), tasks, tools and technologies, environment, and organisational factors (which include team factors). In addition to defining the system and emphasising system interactions,33 the SEIPS model describes how system design can influence care processes and other connected processes (eg, delivery of supplies, housekeeping, purchasing of medical equipment). Because the SEIPS model is anchored in HFE, employee and organisational outcomes are addressed along with patient safety, reflecting the fact that patient safety and worker safety and wellbeing are positively correlated and have common system contributing factors.34
HFE in system design for patient safety
HFE contributes to patient safety via four mechanisms that connect system variables to patient safety (see table 1).35 The first mechanism emphasises the need to incorporate HFE design principles to optimise specific work system elements. These principles can be used to design work systems to eliminate hazards and performance obstacles. For instance, the Handbook of Human Factors in Medical Device Design36 provides a comprehensive set of principles for medical device design. Usability heuristics or rules of thumb for user interface design have been developed for health IT and medical devices.37 The physical design of the work system should minimise perception time, decision time, manipulation time, and the need for excessive physical exertion, and optimise opportunities for physical movement.35 38 From an organisational HFE viewpoint, work systems should be designed so that tasks are reasonably demanding physically and cognitively. Workers should have opportunities to learn, adaptive levels of control over their work system, and access to social and instrumental support (eg, support from coworkers in case of emergency) within the work environment.39 Table 2 provides some examples of HFE design principles; additional information on HFE design for specific work system elements can be found in the Handbook of Human Factors and Ergonomics.40
Table 1.
HFE mechanisms between system design and patient safety
| HFE mechanisms | Objectives of system design |
|---|---|
| 1. A work system that is not designed according to HFE design principles can create opportunities for errors and hazards (see table 2 for examples of design principles) | The objective of HFE-informed system design is to identify and remove system hazards from the design through maintenance phases. |
| 2. Performance obstacles that exist in the work system can hinder clinicians’ ability to perform their work and deliver safe care | If some obstacles cannot be removed, for instance, because they are intrinsic to the job, then strategies should be designed to mitigate the impact of performance obstacles by enhancing other system elements (ie, balance theory of job design)41 42 |
| 3. A work system that does not support resilience can produce circumstances where system operators may not be able to detect, adapt to, and/or recover from errors, hazards, disruptions and disturbances | Work systems should be designed to enhance resilience and support adaptability and flexibility in human work,43 such as allowing problem or variance control at the source44 |
| 4. Because system components interact to influence care processes and patient safety, HFE system design cannot focus on one element of work in isolation.32 35 | Whenever there is a change in the work system, one needs to consider how the change will affect the entire work system, and the entire system needs to be optimised or balanced41 42 |
HFE, human factors and ergonomics.
Table 2.
Examples of HFE design principles
| Focus of HFE | Examples of HFE design principles |
|---|---|
| Physical HFE | To minimise perception time, decision time, and manipulation time |
| To reduce or mitigate need for excessive physical exertion | |
| To optimise opportunities for physical movement | |
| Cognitive HFE | To ensure consistency of interface design |
| To match between technology and the user's mental model | |
| To minimise cognitive load | |
| To allow for error detection and recovery | |
| To provide feedback to users | |
| Organisational HFE | To provide opportunities to workers to learn and develop new skills |
| To allow worker control over work system | |
| To support worker access to social support | |
| To involve users in system design |
HFE, human factors and ergonomics.
Given the systems focus of HFE, it is important not only that each component of the system be designed appropriately, but also that system components be aligned44 and that system interactions be optimised.33 For example, when a new barcoding medication administration (BCMA) system is introduced, it is important to ensure that the technology is designed according to HFE principles (eg, usability heuristics). However, it is also important that the technology fits with the rest of the work system. If there is not sufficient space in which to use the BCMA (interaction between the technology and the physical environment) or if users are not provided with adequate training (interaction between the technology and the organisation), then BCMA may contribute to diminished rather than improved clinician performance and patient safety.
In addition to principles for designing work systems and processes, HFE has developed principles for changing work systems. For instance, in the context of health IT, HFE implementation principles, such as participation, communication and feedback, learning and training, top management commitment and project management are critical to realising the patient safety potential of health IT.45 46 These implementation principles are essential and applicable to the implementation of all kinds of work system design.
HFE-based interventions for patient safety
Studies have used HFE tools and methods to identify system factors that contribute to medical errors; based on these data, researchers or system designers devise recommendations for improving healthcare work systems and processes. These studies are useful for highlighting the importance of HFE to patient safety; however, they do not provide empirical evidence for the value of HFE in improving patient safety. Empirical studies of how HFE-based interventions affect patient safety are few, those that are available have addressed usability of healthcare technologies, concomitant design of healthcare technologies and work system, and design of healthcare processes. This paper is not intended to be a systematic review of HFE-based interventions for patient safety, especially given the broadly different clinical topics and the small number of studies in each clinical topic. Rather, our objective is to highlight the variety of HFE applications and to describe the details of a small number of HFE applications that produced patient safety improvements. Thus we review only six studies to demonstrate various HFE applications. These examples also show that HFE applications for patient safety do not have to wait for accidents to occur; HFE is primarily a proactive system design approach.
Example 1: HFE in the design of radiotherapy treatment delivery system
In the first example, HFE methods were used in the design of a radiotherapy treatment delivery system.47 48
Step 1: HFE analysis
The researchers first evaluated the existing radiotherapy treatment delivery process. Over a 3-month period, an HFE engineer conducted 30 h of field observations of radiation therapists performing their regular tasks. Workflows of radiation therapists, in particular their interactions with the treatment-delivery system, were recorded. Based on these observations, the researchers compiled a list of tasks regularly performed by radiation therapists during treatment delivery.
Step 2: heuristic usability evaluation
One experienced therapist and two HFE engineers performed a heuristic evaluation of the usability of a treatment-delivery system. Since the two HFE experts were not authorised to operate the system, the therapist performed the tasks and explained the workflow to the engineers. The two HFE experts independently identified HFE issues based on 14 usability heuristics,37 and evaluated the severity of each usability issue; they then compared their ratings and reached consensus on a final list of usability issues and their severity. A total of 75 usability issues were identified; of these, 18 were classified as having a high potential impact on patient safety (ie, high severity), 20 were classified as medium severity and 37 were classified as low severity. For instance, when the therapist entered notes into a patient's file, the notes could be deleted without warning if the therapist selected another patient's file before saving the notes. This usability issue violated the heuristics of feedback, error recovery and ability to undo, and was rated with high severity. The recommendation for technology redesign was to warn therapists that their notes might be deleted if they have not saved them.
Step 3: system redesign and evaluation
The existing treatment delivery system was redesigned based on HFE design principles. Two focus groups with experienced radiation therapists provided feedback on the redesigned treatment delivery system, and the system was further refined. Finally, user testing with 16 radiation therapy students was conducted to compare the current and redesigned treatment delivery systems. Using each of the two systems, students went through four scenarios related to typical treatment-delivery tasks. Three of the four scenarios were designed with a high potential for certain use errors to occur (overlooking an important note, shifting the treatment couch incorrectly, and overlooking a change of approval dates). The error rates and overall time to complete each scenario were measured. At the end of the testing, participants were asked to fill out a questionnaire to compare various attributes of the two systems. Results showed that error rates for overlooking an important note and for overlooking changes in approval dates decreased significantly with the redesigned treatment-delivery system (from 73% to 33% and from 56% to 0% respectively). The redesigned treatment delivery system led to efficiency gains (the mean task completion time was reduced by 5.5%) and improvement in user satisfaction.
Example 2: HFE in the design of ED telemetry system
In the second example, a phased HFE approach with significant end user participation is combined with in situ simulation to assess an existing emergency department (ED) telemetry system and redesign it to improve performance of cardiac arrhythmia detection.49
Step 1: HFE system analysis
The researchers used multiple methods to assess the existing telemetry system and its design deficiencies. Several hardware problems were identified by conducting a hardware inventory and function diagnostic. Field observations and web-based surveys revealed several HFE problems related to the use of the telemetry system, such as limited accessibility, poor usability and utility and alarm fatigue. Informal discussions with clinical staff (eg, physicians, nurses, ED technicians) held during shift change and impromptu on-shift meetings provided additional information on all work-system elements related to the telemetry system (see figure 1). The researchers also gathered input from ED clinical practice and administrative leadership councils and patient safety and simulation workgroups.
Figure 1.
Systems Engineering Initiative for Patient Safety (SEIPS) model of work system and patient safety. Reproduced from Carayon et al32 with permission from BMJ Publishing Group Ltd.
Step 2: HFE system design and implementation
Based on the initial analysis phase, work system constraints and HFE specifications for redesigning the telemetry system were determined by researchers and stakeholders (eg, institutional biomedical engineers, the device manufacturer, clinical staff). Through an iterative process, a multifarious intervention was developed to address the three categories of HFE issues: physical HFE issues—hardware repair and repositioning to enhance alarm audibility and visibility, replacement of traditional keyboard and mouse with touchpad input devices to compensate limited workspace; cognitive HFE issues—adjustment of alarm parameter to reduce false alarms, integration of the telemetry system into nurse charting informational workflow to improve general utility; and organisational HFE issues—coordination of institutional infrastructure for routine maintenance, announcement of study conduct and intervention at ED personnel meetings to increase user awareness, group in-servicing and on-shift in-servicing of ED personnel to tackle knowledge deficit of system operation. The intervention was implemented incrementally over a period of 17 months.
Step 3: evaluation of telemetry system redesign
Twenty pre-intervention, 10 interim and 20 post-intervention arrhythmia simulation sessions were conducted over three separate 2-week periods to evaluate the initial telemetry system and compare it with the redesigned telemetry system. Performance data (eg, time between initiation and detection of simulated arrhythmia, detection method, role of the first responder) were collected in each period. The overall arrhythmia detection rate was 5% at baseline, 40% during the interim period and 55% with the fully redesigned telemetry system. Results of post-intervention user surveys indicated that the redesigned telemetry system empowered clinical providers during patient care duties and had the potential to improve patient care. However, a review of alarm log record showed frequent false-positive alarms with the redesigned telemetry system; this indicates the need for further system redesign efforts to continue to support and improve clinicians’ ability to detect cardiac arrhythmia.
Example 3: HFE in the design and implementation of health IT
Various work system factors can affect the acceptance and effective use of healthcare technologies.45 Inadequate planning for implementation and lack of integration of healthcare technologies in existing work systems are associated with work-arounds and technologies falling short of achieving their patient safety goal.50 HFE approaches, which emphasise simultaneous design of the healthcare technology and the work system, are recommended for achieving a balanced work systemii41 42 and fulfilling the full potential of healthcare technology in improving patient safety.
Beuscart-Zéphir and colleagues52 developed an HFE framework for healthcare technology and work system design, along with a set of structured methods to optimise the work system. The HFE framework includes four stages: analysis of the sociotechnical system and the demands of stakeholders; cooperative design of the healthcare technology and the work system with the institution, designers and developers; iterative evaluation and redesign; and assessment of the new work system and its impact on patient safety and overall performance of the sociotechnical system. The HFE framework was used to improve the design and implementation of computerized physician order entry (CPOE).53
Step 1: analysis of medication use process and recommendations for system redesign
Researchers conducted a systematic qualitative analysis of the medication ordering–dispensing–administration process. Field observations and semi-structured interviews were performed with nurses to identify nursing tasks in the medication administration process, to characterise physician–nurse and nurse–nurse communication about medications, and to assess nurses’ interactions with paper patient records. Then more than 7000 paper medication orders written by physicians and the corresponding paper medication-administration records from nurses were reviewed.
Step 2: cooperative system design
The results of observations, interviews and document review were presented to nurses for feedback; software engineering models (eg, UML and Petri Nets) were created to model the distribution of tasks observed. Factors contributing to the safety of medication process were identified at three levels: individual (eg, interactions between nurses and the technology when administering medications), collective (eg, verbal communications supporting cooperation during the medication management process) and organisational (eg, distribution of tasks across different healthcare professionals). Recommendations for work system redesign were proposed, such as the need to provide nurses with specific information at each step of the preparation and administration of medications, and the need for regular physician–nurse communications about patient treatment and changes to the plan of care (eg, daily briefing either before or after medical rounds).
Step 3: usability evaluation of CPOE technology
The researchers also evaluated the usability of the proposed CPOE technology. Five independent HFE experts evaluated the user interface of the software application, using a set of HFE criteria.54 A total of 35 issues related to workload, compatibility, control, homogeneity, guidance and error prevention were identified and rated on a four-point scale for severity.
In a laboratory user testing, eight nurses used the think-aloud method in a simulation of the preparation of medication dispensers and the validation and documentation of medication administration. The laboratory test was designed to reproduce the nurses’ typical work environment. Scenarios were created based on the results of the initial work system analysis. Nurse participants identified a total of 28 usability issues during the test.
Step 4: iterative HFE redesign
In the next phase of CPOE technology redesign, possible solutions for each of the identified usability issues were proposed and evaluated with respect to costs and benefits. Mock-ups and prototypes were developed for those solutions. Iterative usability evaluations and technology redesigns were done until all critical usability issues were addressed. To evaluate the impact of the HFE-based design of healthcare work system on patient safety, the researchers proposed to link the system redesign to the actual identification of adverse events.
In a recent project, the researchers used statistical data mining methods to semi-automatically identify adverse drug events and to link the identified adverse drug events to the analysis and modelling of the work systems. The HFE framework of Beuscart-Zéphir and colleagues is now routinely integrated in IT project management of the Centre Hospitalier Universitaire de Lille, France.
Example 4: HFE in the physical design of operating rooms
In the fourth example, HFE is used to address infection-control problems in the operating room (OR).55 To minimise infection risk, surgical devices were suggested to be positioned within the clean airflow in the OR according to HFE design principles.56 57
Step 1: benchmarking of system
A multidisciplinary team of hospital surgical staff learned from the experience of runway operators at an international airport regarding marking, position of materials, traffic flows, safety rules and regulations, and incident management. They applied this knowledge to OR traffic flows, position of surgical tables and materials, safety management and the process of incident reporting.
Step 2: HFE system design
The multidisciplinary team designed and implemented floor marking to support consistently correct positioning of surgical devices. The implementation was carried out in three steps:
temporary marking was implemented in two of four ORs in February 2009;
temporary marking was implemented in all four ORs by June 2009;
permanent floor marking was implemented in all ORs in December 2009.
Step 3: evaluation of system redesign
Compliance with positioning of surgical devices within the clean airflow was evaluated by observing a total of 182 surgeries before implementation of the floor marking. One month after the implementation of the temporary floor marking in two ORs, compliance data were collected by observing 195 surgeries in ORs with floor markings and 86 surgeries in ORs without floor markings. Four months after implementation of the temporary floor markings in all four ORs, 167 surgeries were observed to collect compliance data. Finally, 199 surgeries were observed 1 month after the implementation of permanent floor markings. Floor marking resulted in significantly increased compliance with recommended positionings of surgical devices in the clean airflow. In addition, post-implementation interviews with three ophthalmic surgeons, three surgical and anaesthesia nurses, and two managers showed enhanced safety awareness among surgical staff. Although the researchers did not use the term ‘HFE’ to describe their study, their approach used a systematic work system analysis and led to a solution firmly rooted in the HFE systems approach.58
Example 5: HFE to identify patient safety hazards in surgery
In the fifth example,59 an HFE approach was used to identify and categorise patient safety hazards in cardiovascular ORs.
Step 1: identification of work system hazards in cardiovascular ORs
A multidisciplinary team of researchers from clinical medicine, health services research, human factors engineering, industrial psychology and organisational sociology identified patient safety hazards in five hospitals through observations, contextual inquiries 60 and pictures of the environment and tools and technologies in cardiovascular ORs. Four team members (a health services researcher, a cardiac anaesthesiologist, a nurse and a human factors engineer) conducted the observations; two of them were present for each surgery. A total of 20 cardiac surgeries were observed over about 160 h, and 84 contextual inquiries were recorded. The four team members reviewed all of the data, including observation notes, contextual inquiries and the pictures, and identified patient safety hazards.
Step 2: categorising the work system hazards
The researchers used deductive and inductive approaches to analyse the qualitative data and categorised the work system hazards in cardiovascular surgeries. The SEIPS model32 (see figure 1) was used in a deductive manner to create high-level categories of patient safety hazards, which were further developed in subcategories based on emerging themes from the data (inductive process). A total of 59 patient safety hazard categories were identified:
care provider: variations in performing procedures, inappropriate professional conduct;
task: increased workload, interruptions in the workflow;
tools and technologies: usability issues, tools and technologies not available in a timely manner;
physical environment: limited physical space in the ORs, poor arrangement of equipment;
organisation: lack of a culture to report patient safety incidents, poor communication;
processes: evidence-based practices not followed, poor supply chain management.
Step 3: proposing solutions for system redesign
Based on the patient safety hazards identified in the study, the researchers propose solutions for system redesign, such as standardisation of care across an organisation, teamwork training for care providers, further analysis with methods such as proactive risk assessment (see next example), use of simulation to evaluate the physical layout of ORs before building them, and use of recommended communication practices such as repeat back.
Example 6: HFE in the design of care processes
HFE can help to improve the design of care processes.61 Proactive risk assessment methods, such as failure mode and effects analysis (FMEA), are HFE methods that can be used to evaluate high-risk processes in healthcare and provide input for healthcare process design.62 63 A number of publications provide guidance for conducting proactive risk assessment such as FMEA62 64 and discuss challenges in performing such analysis.65 66 The sixth study describes an FMEA of the intravenous medication administration process conducted to assess the potential HFE and safety issues of a new intravenous pump.67
Step 1: formation and training of FMEA team
A multidisciplinary team consisting of representatives from anaesthesiology, biomedical engineering central supply, human factors engineering, internal medicine, nursing, pharmacy and quality improvement performed a healthcare Healthcare Failure Modes and Effects Analysis (HFMEA)68 to evaluate the intravenous medication administration process using current intravenous pump and Smart intravenous pump technology. The team members were trained for 1–2 h in the Veteran Affairs’ HFMEA method.68
Step 2: FMEA analysis process
The FMEA process consisted of 46 h of meetings over 4½ months and unfolded in three steps:
process identification and mapping;
failure mode identification and scoring;
determination of interventions and outcome measures.
Multiple data sources were used to develop the intravenous medication administration process map. Two HFE experts conducted a total of 52 observations of nurses administering medications with the current intravenous pump.69 Medication administration and intravenous pump events reported with the current pump were retrieved from the hospital's event reporting system. The FMEA team mapped the medication administration process with the current intravenous pump and then repeated the mapping process with the Smart intravenous pump. In the process map with the current intravenous pump, the team identified 10 steps for retrieving the medication and tubing, and 24 steps for pump programming were identified. For the Smart intravenous pump, the team identified 14 unique pump programming steps and new tubing setup and insertion steps.
Following process mapping, the team analysed failure modes potentially associated with intravenous pump use. About 200 failure modes were identified and scored with respect to severity and probability of occurrence. A hazard score was calculated by using the product of the severity and probability of occurrence ratings. Failure modes with low or low–moderate hazard scores were assessed for detectability, and only non-detectable failure modes were considered for further action. All failure modes with moderate to high hazard scores were considered further.
Step 3: recommendations for process redesign
Recommendations for prioritised failure modes were proposed and categorised into the five elements of the work system32 (see figure 1): policies and procedures; training or education; physical environment; people; and technology software or hardware change. The evaluation of the impact of the FMEA on patient safety was based on: audits of programming of pumps for errors; monitoring of end-user training for time to achieve competency; and monitoring and recording of intravenous medication administration event reports and informal and formal complaints about pump functioning. Post-implementation results suggested that the goal of mitigating risk to patients from potential or known failure modes was achieved.
Conclusions
A study conducted by an HFE leader, Al Chapanis, and his colleague in the early 1960s provided information on medication administration errors and the system factors that contributed to these errors.70–72 Since then, awareness of the importance of HFE in medication safety and other patient safety domains has significantly increased. Patient safety leaders have called for increasing involvement of HFE in helping to characterise system factors that contribute to patient safety and to inform system design interventions.3 73 74 This paper has described examples of HFE contributions to specific patient safety problems. Further research is necessary to document and demonstrate the value of HFE-based interventions and their impact on patient safety. Evidence for the effectiveness of HFE-based interventions should include data on changes in the work system, changes in the process and changes in outcomes (including patient safety and employee outcomes). In general, this evidence is provided through the use of multiple quantitative and qualitative methods.
Numerous patient safety practices can benefit from HFE input. Patient safety practices target some aspect of the work system (see figure 1) and should be designed and implemented according to HFE principles to produce patient safety benefits. For instance, checklists have been shown to improve patient safety.75 76 Checklists can be considered as a tool in the work system (see figure 1), and their patient safety benefits are enhanced when they are designed and implemented to fit the rest of the work system.77 An intervention study at the VA included teamwork training, ongoing coaching, and tools such as a checklist that supported teamwork.78 The checklist acted as a tool to trigger OR communication rather than as a simple memory aid. The checklist is a tool that requires changes in other elements of the work system (see figure 1).
HFE is a core element of patient safety strategies.8 Therefore, every effort should be made to support HFE applications in patient safety. Healthcare leaders, executives, administrators and vendors should ensure that HFE is included in any patient safety improvement. This can be accomplished through the use of HFE tools and methods (eg, usability evaluation of health IT), HFE training in healthcare organisations and vendors, or hiring of HFE engineers.79
Acknowledgments
Partial funding was provided by AHRQ through a contract to RAND (HHSA-290-2007-10062I) and by the Clinical and Translational Science Award (CTSA) programme, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contributors: PC: major contribution in the conception and design of the paper, major contribution in drafting and revising the paper, major contribution in final approval of the version to be published. AX and SK: some contribution in the conception and design of the paper, some contribution in drafting and revising the paper, some contribution in final approval of the version to be published.
Funding: Partial funding was provided by AHRQ through a contract to RAND (HHSA-290-2007-10062I) and by the Clinical and Translational Science Award (CTSA) programme, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
‘Human factors’ and ‘ergonomics’ are synonymous names for the discipline; the discipline is often referred to as ‘Human factors and ergonomics’ or HFE. Most human factors professionals receive their HFE education in departments of industrial engineering or psychology.
A work system can be balanced through either compensatory balance when positive work system elements compensate for negative work system elements, or overall system balance when the combination of positive and negative work system elements produces benefits with regard to outcomes.42 The concept of balanced work system is further discussed by Carayon et al51.
References
- 1.Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events. JAMA 1995;274:35–43 [PubMed] [Google Scholar]
- 2.Institute of Medicine Preventing medication errors. Washington, DC: The National Academies Press, 2006 [Google Scholar]
- 3.Institute of Medicine Health IT and patient safety: building safer systems for better care. Washington, DC: The National Academies Press, 2012 [PubMed] [Google Scholar]
- 4.Hignett S, Masud T. A review of environmental hazards associated with in-patient falls. Ergonomics 2006;49:605–16 [DOI] [PubMed] [Google Scholar]
- 5.International Ergonomics Association (IEA) The discipline of ergonomics. http://www.iea.cc/ergonomics/ (accessed 22 Aug 2004)
- 6.Dul J, Bruder R, Buckle P, et al. A strategy for human factors/ergonomics: developing the discipline and profession. Ergonomics 2012;55:377–95 [DOI] [PubMed] [Google Scholar]
- 7.Weaver SJ, Dy SM, Rosend MA. Team-training in health care: a narrative synthesis of the literature. BMJ Qual Saf 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shekelle PG, Wachter R, Pronovost P, et al. Making health care safer II: an updated critical analysis of the evidence for patient safety practices. Comparative Effectiveness Review No 211 prepared by the Southern California-RAND Evidence-based Practice Center under Contract No 290-2007-10062-I Rockville, Maryland: Agency for Healthcare Research and Quality, 2013 [Google Scholar]
- 9.Gosbee JW, Gosbee LL. eds. Using human factors engineering to improve patient safety. Oakbrook Terrrace, Illinois: Joint Commission Resources, 2005 [Google Scholar]
- 10.Rousek JB, Hallbeck MS. Improving medication management through the redesign of the hospital code cart medication drawer. Hum Factors 2011;53:626–36 [DOI] [PubMed] [Google Scholar]
- 11.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med 2003;348:2526–34 [DOI] [PubMed] [Google Scholar]
- 12.Battles JB, Keyes MA. Technology and patient safety: a two-edged sword. Biomed Instrum Technol 2002;36:84–8 [DOI] [PubMed] [Google Scholar]
- 13.Bogner MS. ed. Human error in medicine. Hillsdale, New Jersey: Lawrence Erlbaum Associates, 1994 [Google Scholar]
- 14.Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998;316:1154–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reason J. Managing the risks of organizational accidents. Burlington, Vermont: Ashgate, 1997 [Google Scholar]
- 16.Bogner MS. The artichoke systems approach for identifying the why of error. In: Carayon P. ed. Handbook of human factors in health care and patient safety. Mahwah, New Jersey: Lawrence Erlbaum; 2007:109–26 [Google Scholar]
- 17.Carayon P, Gurses AP, Hundt AS, et al. Performance obstacles and facilitators of healthcare providers. In: Korunka C, Hoffmann P. eds. Change and quality in human service work. Munchen, Germany: Hampp Publishers, 2005:257–76 [Google Scholar]
- 18.Karsh B-T, Holden RJ, Alper SJ, et al. A human factors engineering paradigm for patient safety: designing to support the performance of the healthcare professional. Qual Saf Health Care 2006;15:i59–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gurses AP, Carayon P. Performance obstacles of intensive care nurses. Nurs Res 2007;56:185–94 [DOI] [PubMed] [Google Scholar]
- 20.Gurses A, Carayon P. Exploring performance obstacles of intensive care nurses. Appl Ergon 2009;40:509–18 [DOI] [PubMed] [Google Scholar]
- 21.Carayon P, Alvarado CJ, Hundt AS, et al. Patient safety in outpatient surgery: the viewpoint of the healthcare providers. Ergonomics 2006;49:470–85 [DOI] [PubMed] [Google Scholar]
- 22.Tucker AL. The impact of operational failures on hospital nurses and their patients. J Oper Manag 2004; 22:151–69 [Google Scholar]
- 23.Jeffcott S, Ibrahim J, Cameron P. Resilience in healthcare and clinical handover. Qual Saf Health Care 2009;18:256–60 [DOI] [PubMed] [Google Scholar]
- 24.Woods DD, Hollnagel E. Prologue: Resilience engineering concepts. In: Hollnagel E, Woods DD, Leveson N. eds. Resilience engineering—concepts and precepts. Hampshire, UK: Ashgate; 2006:1–6 [Google Scholar]
- 25.Habraken MMP, van der Schaaf TW. If only…: failed, missed and absent error recovery opportunities in medication errors. Qual Saf Health Care 2010;19:37–41 [DOI] [PubMed] [Google Scholar]
- 26.Rogers AE, Dean GE, Hwang WT, et al. Role of registered nurses in error prevention, discovery and correction. Qual Saf Health Care 2008;17:117–21 [DOI] [PubMed] [Google Scholar]
- 27.Faye H, Rivera-Rodriguez AJ, Karsh BT, et al. Involving intensive care unit nurses in a proactive risk assessment of the medication management process. Jt Comm J Qual Patient Saf 2010;36:376–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kanse L, Van der Schaaf TW, Vrijland ND, et al. Error recovery in hospital pharmacy. Ergonomics 2006;49:503–16 [DOI] [PubMed] [Google Scholar]
- 29.Rothschild JM, Churchill W, Erickson A, et al. Medication errors recovered by emergency department pharmacists. Ann Emerg Med 2010;55:513–21 [DOI] [PubMed] [Google Scholar]
- 30.Weick KE, Sutcliffe KM. Managing the unexpected—resilient performance in an age of uncertainty. 2nd edn. San Francisco, California: John Wiley & Sons, 2007 [Google Scholar]
- 31.Vincent CA. Analysis of clinical incidents: a window on the system not a search for root causes. Qual Saf Health Care 2004;13:242–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carayon P, Hundt AS, Karsh B-T, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care 2006;15:i50–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilson JR. Fundamentals of ergonomics in theory and practice. Appl Ergon 2000;31:557–67 [DOI] [PubMed] [Google Scholar]
- 34.Taylor JA, Dominici F, Agnew J, et al. Do nurse and patient injuries share common antecedents? An analysis of associations with safety climate and working conditions. BMJ Qual Saf 2011 [DOI] [PubMed] [Google Scholar]
- 35.Carayon P, Alvarado C, Hundt AS. Work design and patient safety. Theor Issues Ergon 2007;8:395–428 [Google Scholar]
- 36.Weinger MB, Wiklund M, Gardner-Bonneau DJ. eds. Handbook of human factors in medical device design. Boca Raton, Florida: Taylor & Francis, 2011 [Google Scholar]
- 37.Zhang J, Johnson TR, Patel VL, et al. Using usability heuristics to evaluate patient safety of medical devices. J Biomed Inform 2003;36:23–30 [DOI] [PubMed] [Google Scholar]
- 38.Kroemer KHE, Kroemer H, Kroemer-Elbert K. Ergonomics—how to design for ease and efficiency. 2nd edn. Upper Saddle River, New Jersey: Prentice Hall, 2001 [Google Scholar]
- 39.Cherns A. The principles of sociotechnical design. Hum Relat 1976;29:783–92 [Google Scholar]
- 40.Salvendy G. Handbook of human factors and ergonomics. Hoboken, New Jersey: John Wiley & Sons, 2012 [Google Scholar]
- 41.Carayon P. The balance theory and the work system model… Twenty years later. Int J Hum Comput Interact 2009;25:313–27 [Google Scholar]
- 42.Smith MJ, Carayon-Sainfort P. A balance theory of job design for stress reduction. Int J Ind Ergon 1989;4:67–79 [Google Scholar]
- 43.Hollnagel E, Woods DD, Leveson N. eds. Resilience engineering—concepts and precepts. Burlington, Vermont: Ashgate, 2006 [Google Scholar]
- 44.Clegg CW. Sociotechnical principles for system design. Appl Ergon 2000;31:463–77 [DOI] [PubMed] [Google Scholar]
- 45.Karsh B-T. Beyond usability: designing effective technology implementation systems to promote patient safety. Qual Saf Health Care 2004;13:388–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smith MJ, Carayon P. New technology, automation, and work organization: stress problems and improved technology implementation strategies. Int J Hum Factor Man 1995;5:99–116 [Google Scholar]
- 47.Chan AJ, Islam MK, Rosewall T, et al. The use of human factors methods to identify and mitigate safety issues in radiation therapy. Radiother Oncol 2010;97:596–600 [DOI] [PubMed] [Google Scholar]
- 48.Chan AJ, Islam MK, Rosewall T, et al. Applying usability heuristics to radiotherapy systems. Radiother Oncol 2011;102:142–47 [DOI] [PubMed] [Google Scholar]
- 49.Kobayashi L, Parchuri R, Gardiner FG, et al. Use of in situ simulation and human factors engineering to assess and improve emergency department clinical systems for timely telemetry-based detection of life-threatening arrhythmias. BMJ Qual Saf 2013;22:72–83 [DOI] [PubMed] [Google Scholar]
- 50.Karsh BT, Weinger MB, Abbott PA, et al. Health information technology: fallacies and sober realities. JAMIA 2010;17:617–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beuscart-Zephir MC, Elkin P, Pelayo S, et al. The human factors engineering approach to biomedical informatics projects: state of the art, results, benefits and challenges. Yearb Med Inform 2007:109–27 [PubMed] [Google Scholar]
- 53.Beuscart-Zephir MC, Pelayo S, Bernonville S. Example of a human factors engineering approach to a medication administration work system: potential impact on patient safety. Int J Med Inform 2010;79:e43–57 [DOI] [PubMed] [Google Scholar]
- 54.Bastien C, Scapin DL. Ergonomic criteria for the evaluation of human–computer interfaces. Rocquencourt: INRIA, 1993 [Google Scholar]
- 55.de Korne DF, van Wijngaarden JDH, van Rooij J, et al. Safety by design: effects of operating room floor marking on the position of surgical devices to promote clean air flow compliance and minimise infection risks. BMJ Qual Saf 2011;21:746–52 [DOI] [PubMed] [Google Scholar]
- 56.Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999;20:250–78; quiz 79–80 [DOI] [PubMed] [Google Scholar]
- 57.Pasquarella C, Sansebastiano GE, Ferretti S, et al. A mobile laminar airflow unit to reduce air bacterial contamination at surgical area in a conventionally ventilated operating theatre. J Hosp Infect 2007;66:313–19 [DOI] [PubMed] [Google Scholar]
- 58.Norris BJ. Systems human factors: how far have we come? BMJ Qual Saf 2011;21:713–14 [DOI] [PubMed] [Google Scholar]
- 59.Gurses AP, Kim G, Martinez EA, et al. Identifying and categorising patient safety hazards in cardiovascular operating rooms using an interdisciplinary approach: a multisite study. BMJ Qual Saf 2012;21:810–18 [DOI] [PubMed] [Google Scholar]
- 60.Beyer H, Holtzblatt K. Contextual design: defining customer-centered systems. San Francisco, California: Morgan Kaufmann Publishers, 1997 [Google Scholar]
- 61.Institute of Medicine Committee on Quality of Health Care in America Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press, 2001 [Google Scholar]
- 62.Carayon P, Faye H, Hundt AS, et al. Patient safety and proactive risk assessment. In: Yuehwern Y. ed. Handbook of healthcare delivery systems. Boca Raton, Florida: Taylor & Francis, 2011:12-1/12-15 [Google Scholar]
- 63.Bonnabry P, Despont-Gros C, Grauser D, et al. A risk analysis method to evaluate the impact of a computerized provider order entry system on patient safety. JAMIA 2008;15:453–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lyons M. Towards a framework to select techniques for error prediction: supporting novice users in the healthcare sector. Appl Ergon 2009;40:379–95 [DOI] [PubMed] [Google Scholar]
- 65.Dean Franklin B, Shebl NA, Barber N. Failure mode and effects analysis: too little for too much? BMJ Qual Saf 2012;21:607–11 [DOI] [PubMed] [Google Scholar]
- 66.Wetterneck TB, Skibinski K, Schroeder M, et al. Challenges with the performance of failure mode and effects analysis in healthcare organizations: an IV medication administration HFMEATM. In: The Human Factors and Ergonomics Society, ed. Annual Conference of the Human Factors and Ergonomics Society. New Orleans, LA: The Human Factors and Ergonomics Society, 2004 [Google Scholar]
- 67.Wetterneck TB, Skibinski KA, Roberts TL, et al. Using failure mode and effects analysis to plan implementation of Smart intravenous pump technology. Am J Health Syst Pharm 2006;63:1528–38 [DOI] [PubMed] [Google Scholar]
- 68.DeRosier J, Stalhandske E, Bagian JP, et al. Using health care failure mode and effect analysis: the VA National Center for Patient Safety's prospective risk analysis system. Jt Comm J Qual Improv 2002;28:248–67, 09 [DOI] [PubMed] [Google Scholar]
- 69.Carayon P, Wetterneck T, Hundt AS, et al. Observing nurse interaction with infusion pump technologies. In: Henriksen K, Battles JB, Marks E, et al. eds. Advances in patient safety: from research to implementation. Rockville, Maryland: Agency for Healthcare Research and Quality, 2005:349–64 [PubMed] [Google Scholar]
- 70.Safren MA, Chapanis A. A critical incident study of hospital medication errors—Part 1. Hospitals 1960;34:32–4;57–66. [PubMed] [Google Scholar]
- 71.Safren MA, Chapanis A. A critical incident study of hospital medication errors—Part 2. Hospitals 1960;34:65–8 [PubMed] [Google Scholar]
- 72.Chapanis A, Safrin MA. Of misses and medicines. J Chronic Dis 1960;12:403–08 [DOI] [PubMed] [Google Scholar]
- 73.Leape L. Human factors meets health care: the ultimate challenge. Ergon Des 2004;12:6–12 [Google Scholar]
- 74.Pronovost PJ, Goeschel CA, Marsteller JA, et al. Framework for patient safety research and improvement. Circulation 2009;119:330–37 [DOI] [PubMed] [Google Scholar]
- 75.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009;360:491–99 [DOI] [PubMed] [Google Scholar]
- 76.Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006;355:2725–32 [DOI] [PubMed] [Google Scholar]
- 77.Gawande AA. The Checklist Manifesto. New York: Metropolitan Books, 2009 [Google Scholar]
- 78.Neily J, Mills PD, Lee P, et al. Medical team training and coaching in the veterans health administration; assessment and impact on the first 32 facilities in the programme. Qual Saf Health Care 2010;19:360–64 [DOI] [PubMed] [Google Scholar]
- 79.Carayon P. Human factors in patient safety as an innovation. Appl Ergon 2010;41:657–65 [DOI] [PMC free article] [PubMed] [Google Scholar]