Abstract
This manuscript reports the clinical, microbiological, and genetic characteristics of carbapenem-resistant K. pnuemoniae isolates from pediatric patients at a tertiary-care children's hospital. Although there is an extensive body of literature describing carbapenem-resistant Klebsiella infections in adults, pediatric data are comparatively limited.
Keywords: carbapenemase, Klebsiella pneumoniae, polymyxin
Infections from carbapenem-resistant Klebsiella pneumoniae (CRKP) are prevalent in adult hospitals in the United States and are primarily attributed to sequence-type (ST)-258 [1, 2], although pediatric data are limited. The blaKPC gene, located on transposon Tn4401, encodes carbapenem resistance and is commonly carried on transferable plasmids, which may also host resistance genes for other antibiotic classes [1, 3]. To date, 14 blaKPC gene variants have been described and are typically secondary to nonsynonymous single nucleotide substitutions [4]. Point mutations in the K. pneumoniae outer membrane porin genes, ompK35 and ompK36, may impact antimicrobial susceptibility patterns [5]. We present a comprehensive microbiological and molecular description of CRKP isolated from 5 children hospitalized within a 12-month interval at the Children's Hospital at Montefiore, located adjacent to the institution's adult hospital.
METHODS
Following institutional review board approval, medical records were reviewed for pediatric patients who had K. pneumoniae cultures with evidence of carbapenemase production. Prior to September 2010, potential CRKP isolates were identified by carbapenem minimum inhibitory concentration (MIC) determination by the automated Vitek® 2 system (bioMerieux, Inc, Durham, NC), followed by modified Hodge test when indicated. If isolates were found by Vitek® 2 to be susceptible to both imipenem (MIC ≤ 4 µg/mL) and ertapenem (MIC ≤ 2 µg/mL), it was concluded that carbapenemase production was unlikely. If isolates were intermediate or resistant to either imipenem or ertapenem, the modified Hodge test was then performed. Following September 2010, potential CRKP isolates were instead identified according to the updated Clinical and Laboratory Standards Institute (CLSI) carbapenem breakpoints [6].
When available, isolates included in this study were genotyped by multilocus sequence typing (MLST) [7]. β-Lactamase genes blaCTX-M, blaSHV, blaTEM, blaKPC, blaNDM, blaVIM, blaIMP, blaOXA-48; porin genes ompK35 and ompK36; and transposon Tn4401 isoforms were evaluated by PCR and sequencing [4, 8, 9]. Pulsed-field gel electrophoresis (PFGE) examined the genetic relatedness of pediatric isolates and five CRKP isolates from adult patients at our institution [10]. PFGE results were analyzed by BioNumerics (Applied Maths, Kortrijk, Belgium) using the Dice correlation coefficient and the unweighted pair-group clustering algorithm.
RESULTS
Patient A
An 8-year-old male with a history of cerebral palsy, ventriculoperitoneal (VP) shunt, and tracheostomy was admitted to the pediatric intensive care unit (PICU) with methicillin-resistant Staphylococcus aureus (MRSA) VP shunt infection and bacteremia (Table 1). An endotracheal culture on hospital day 1 yielded CRKP, was attributed to colonization, and CRKP-specific therapy was not initiated.
Table 1.
Clinical and Microbiological Characteristics of Carbapenem-Resistant Klebsiella pneumoniae in Pediatric Patients
| Case Age | Comorbidities | Prior Hosp.a | Clinical Syndrome and Culture Source | Duration of Hosp. | Therapy |
Minimum Inhibitory Concentrations (μg/mL)b |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Type | Duration (days) | Days to sterilization | Erta | Imip | Cipr | Pip/taz | Ceft | Tige | PolyB | |||||
| A 8 yrs |
VP shunt MRSA ventriculitis MRSA sepsis Tracheostomy CVC |
2 | 1. Respiratory colonization Endotracheal culture Hospital day 1 |
102 | None | NA | NA | ≥8 | 8 | ≥4 | ≥128 | ≥64 | 0.75 (S) | 1 (S) |
| 2. Bacteremia Blood culture (CVC) Hospital day 37 |
Polymyxin B Rifampin Removal of CVC |
14 | 2 | ≥8 | 8 | ≥4 | ≥128 | ≥64 | 1.5 (S) | 2 (S) | ||||
| B 6 yrs |
Crush/degloving injury | 0 | Peritonitis Peritoneal fluid culture Hospital day 1 |
79 | Tigecycline Peritoneal washout |
42 | NA | 4 | ≤1c | ≥4 | ≥128 | ≥64 | 0.75 (S) | 1.5 (S) |
| C 3 yrs |
Prune-belly syndrome Renal transplantation Grade IV VUR Adenovirusd CMV DNAemiae MRSA wound infection |
14 | 1. Pyelonephritis Urine culture Post transplant day 90 |
46 | Ciprofloxacin Reduced tacrolimus |
14 | 1 | ≥8 | 8 | ≥4 | ≥128 | ≥64 | 1 (S) | 0.5 (S) |
| 2. Wound infection Wound culture Post transplant day 97 |
3 | Linezolid Incision and drainage |
NA | NA | NA | 8 | ≥4 | ≥128 | 32 | 2 (S) | 2 (S) | |||
| 3. Urosepsis Blood culture (peripheral) Urine culture Post transplant day 111 |
27 | Polymyxin B Rifampin Reduced tacrolimus |
14 | 2 (blood) 5 (urine) |
NA NA |
8 8 |
≥4 ≥ 4 |
≥128 ≥ 128 |
≥64 ≥ 64 |
8 16 |
2 2 (S) |
|||
| 4. Urinary colonization Urine culture 10 months post therapy |
NA | None | NA | NA | NA | ≥16 | ≥4 | ≥128 | ≥64 | 1.5 (S) | 0.75 (S) | |||
| D 3 yrs |
Congenital heart defect Congestive heart failure |
0 | Respiratory colonization Endotracheal culture Hospital day 12 |
23 | None | NA | NA | 4 | 8 | ≥4 | ≥128 | 32 | 1.5 (S) | 1 (S) |
| E 11 mos | S. pyogenes sepsis | 0 | Respiratory colonization Endotracheal culture Hospital day 7 |
10 | None | NA | NA | NA | 4 | ≥4 | ≥128 | 16 | NA | NA |
Abbreviations: Ceft, ceftriaxone; Cipr, ciprofloxacin; CMV, cytomegalovirus; CVC, central venous catheter; Erta, ertapenem; Imip, imipenem; MRSA, methicillin-resistant Staphylococcus aureus; NA, not available; Pip/taz, piperacillin/tazobactam; PolyB, polymyxin B; Rifa, rifampin; Tige, tigecycline; VP, ventriculoperitoneal; VUR, vesicoureteral reflux.
aHospitalizations in the previous year.
bAll reported minimum inhibitory concentrations are considered resistant by Clinical and Laboratory Standards Institute breakpoints unless otherwise noted to be susceptible (S).
cModified-Hodge test positive.
d30 days before carbapenem-resistant Klebsiella pneumoniae (CRKP).
e7 days before CRKP.
On hospital day 37, after varying courses of vancomycin, daptomycin, linezolid, meropenem, gentamicin, and piperacillin–tazobactam, the patient developed fever (38.5°C) and respiratory distress. Blood cultures were obtained from the tunneled central venous catheter (CVC), and empiric cefepime was initiated. Blood cultures yielded K. pneumoniae within 12 hours, subsequently confirmed as CRKP, and therapy was changed to polymyxin B and rifampin. The CVC was removed 3 days after first positive blood culture.
Patient B
A 6-year-old previously healthy male with no prior hospitalizations suffered an abdominal crush injury and underwent exploratory laparotomy with bowel reconstruction on hospital day 1. Vancomycin, cefepime, and metronidazole were initiated intraoperatively. The patient was febrile postoperatively (38.1°C–39.9°C). Intraoperative peritoneal fluid cultures displayed no leukocytes or organisms on Gram stain, and primary cultures of peritoneal fluid on selective media yielded no growth. However, after 48 hours of incubation, CRKP and Enterococcus faecalis grew from the thioglycollate broth subculture. Although these results may have represented environmental contamination of the specimen, it was felt that peritonitis could not be excluded in the setting of severe abdominal injuries. Thus, antibiotic therapy was changed to tigecycline. The patient remained febrile for 10 days despite negative blood and urine cultures and no evidence of wound infection or intra-abdominal collection.
Patient C
A 3-year-old kidney transplant recipient with ureteral stent and grade IV vesicoureteral reflux presented 3 months post-transplantation with fever and pyuria. Intravenous ciprofloxacin was initiated empirically. Urine culture revealed 40 000 colonies/mL of E faecalis and >100 000 colonies/mL CRKP. Blood cultures were negative. Despite in vitro fluoroquinolone resistance, the patient defervesced and urine cultures sterilized, potentially secondary to bactericidal urinary antibiotic concentrations. The patient received 14 days of ciprofloxacin.
The patient was admitted 1 week later with wound dehiscence. Two wound cultures were sent from purulent fluid expressed at the bedside, and linezolid therapy was initiated. Both cultures grew MRSA within 24 hours of incubation; one culture also yielded CRKP after 48 hours. Blood and urine cultures were negative. CRKP-specific therapy was not initiated; the wound infection resolved. Two weeks later, the patient again presented with fever and pyuria. Urine and blood cultures revealed gram-negative bacilli, later identified as CRKP, and polymyxin B and rifampin were initiated. The ureteral stent, a possible nidus of infection, was removed on hospital day 15. Subsequent urine cultures intermittently yielded CRKP in the absence of symptoms or pyuria and were not treated with antibiotics. The patient has experienced no graft dysfunction or rejection to date.
Patient D
A 3-year-old female from Pakistan with congestive heart failure secondary to ventricular septal defect was admitted to the PICU for inotropic support. She underwent cardiac catheterization on hospital day 5. On hospital day 8 she developed fever, worsening hypotension, and pulmonary edema. She was intubated and received empiric vancomycin, meropenem, and amikacin. A chest tube was placed and drained serosanguinous fluid (1900 leukocytes/μL with 93% lymphocytes, 6290 erythrocytes/μL, glucose 119 mg/dL, protein 3.5 g/dL); pleural fluid, blood, and urine cultures yielded no organisms. On the fourth day of fever, endotracheal culture yielded CRKP and Stenotrophomonas maltophilia; no organisms were seen on Gram stain. Blood cultures remained negative, there was no significant change in chest radiograph or mechanical ventilation settings, and CRKP-specific therapy was not initiated. She died of cardiopulmonary failure on hospital day 19.
Patient E
An 11-month-old female was admitted to the PICU with Group A streptococcus bacteremia and sepsis. On hospital day 4, she developed new fever. Blood and urine cultures were negative. Endotracheal culture yielded CRKP, S maltophilia, and Moraxella catarrhalis, but no organisms on Gram stain. There was no clinical evidence of pneumonia, and CRKP-specific therapy was not initiated. She was extubated on hospital day 5 and received 14 days of penicillin.
Molecular Analysis
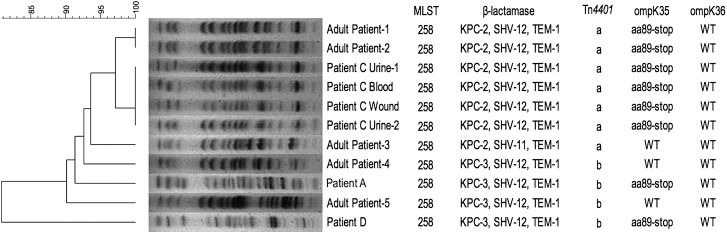
Resistance Gene Testing. Isolates from Patients A, C, and D were available for molecular evaluation (Figure 1). Isolates from patients A and D were ST258 and harbored KPC-3 and extended spectrum β-lactamases SHV-12 and TEM-1. Urine, wound, and blood isolates for Patient C were also ST258 but harbored KPC-2, SHV-12, and TEM-1. A surveillance urine isolate obtained 10 months later from Patient C displayed genotypic and resistance patterns similar to prior isolates. Sequencing of the porin gene ompK35 revealed a guanine insertion at nt121 in all isolates, resulting in a stop codon at amino acid position 89. No mutations were found in ompK36. Tn4401 isoforms a and b were detected in all isolates. Tn4401a is characterized by a 100-bp deletion upstream of the blaKPC gene [9].
Figure 1.
Pulsed-field gel electrophoresis and genotyping results of carbapenem-resistant Klebsiella pneumoniae isolates from pediatric and adult patients. XbaI chromosomal restriction patterns were analyzed to examine the genetic relatedness of pediatric and adult isolates. Isolates were genotyped by multilocus sequence typing (MLST). β-Lactamase genes blaCTX-M, blaSHV, blaTEM, blaKPC, blaNDM, blaVIM, blaIMP, blaOXA-48, porin genes ompK35 and ompK36, and transposon Tn4401 isoforms were detected by polymerase chain reaction and sequencing. Isolates from Patient C (urine, blood, and wound) and Patient A (blood) display banding patterns similar to those observed for representative adult isolates. The isolate from Patient D displays a banding pattern distinct from the other isolates. “Patient C Urine—2” represents an isolate obtained in the absence of symptoms and is similar to the prior blood, urine, and wound isolates from this patient. All pediatric isolates were ST258 and expressed either KPC-2 or 3, SHV-12, and TEM-1. All pediatric isolates were found to contain a guanine insertion at nt121 within ompK35, resulting in a stop codon at amino acid position 89 (aa89-stop). All ompK36 genes were found to be wild-type (WT). All isolates from Patient C were Tn4401a isoform, while isolates from Patient A and D were Tn4401b isoform.
Genetic Relatedness and Clonality. PFGE banding patterns for isolates for Patients A and C were similar to representative and randomly selected ST258 adult isolates from our institution (Figure 1), suggesting clonal spread of ST258. The isolate from Patient D exhibited a banding pattern distinct from that observed in the other pediatric and adult isolates.
DISCUSSION
Risk factors for CRKP are well described for adults and include prolonged duration of hospitalization [11]. The mean number of hospital days preceding CRKP detection in our series was relatively short (11.8 days), and CRKP was detected on the first day of hospitalization in two patients (A and B). Patient A was hospitalized twice in the year prior to CRKP detection and could have been exposed to CRKP by his home nursing attendant or by his mother, a hospital custodian. Patient B had no history of prior hospitalizations; this isolate could represent community acquisition or environmental contamination of peritoneal fluid cultures.
No children in our series died as a result of CRKP infection or exhibited adverse effects from CRKP-specific therapy, which likely reflects our small sample size. PCR analysis of isolates from Patients A, C, and D revealed an ompK35 porin gene mutation that resulted in termination of translation of the porin channel and presumably decreased antibiotic permeation. However, outer-membrane porins also transport bacterial nutrients; therefore, ompK35 and ompK36 mutations may instead result in decreased virulence [5] and may have contributed to the overall positive outcomes observed. The impact of ompK mutations on clinical outcomes requires further investigation.
At our pediatric hospital, the estimated CRKP prevalence by CLSI breakpoints [6] among inpatient Klebsiella isolates from typically sterile sites is 3%; the prevalence at our adult institution is 4% by KPC gene detection (personal communication, Dr Michael Levi). The five cases described in this report occurred at our institution within a 12-month period. CRKP cases may have been missed prior to September 2010 and the subsequent lowering of carbapenem breakpoints at our institution. Conversely, one CRKP isolate in our series was identified by modified Hodge test; false-positive results have been reported for this assay [12]. In addition, two isolates in our study were not available for molecular characterization, and it is therefore impossible to confirm CRKP status for these isolates.
Genetic analyses and PFGE suggested clonal spread of the predominant ST258 strain, with the exception of Patient D's isolate, which could represent an alternate source or a minor clone within our institution. The similarity of MLST and PFGE patterns suggested genetic relatedness and possible clonal spread of strains from Patients A and C. However, the KPC gene is located on transposon Tn4401 on variable plasmids, which may easily transfer between different strains, species, and genera. Thus, isolates from Patients A and C are genetically related based on chromosome structure (MLST and PFGE) but may differ by KPC-harboring plasmids and/or Tn4401 transposons. Isolates from Patients A and D harbored KPC-3, and isolates from Patient C harbored KPC-2. KPC-2 and KPC-3 differ only by a single amino acid substitution, which results from a single nucleotide polymorphism mutation at nt814 of the blaKPC gene [4], and have similar catalytic efficiency against β-lactam antimicrobials [13].
All patients in this series were placed on contact isolation following detection of CRKP. We could not identify common epidemiological factors linking these cases, and an outbreak investigation was not performed in real time. Two of our patients had CRKP isolated only by endotracheal culture; endotracheal cultures yielding resistant organisms are often considered ubiquitous in the ICU environment. However, a recent outbreak investigation identified asymptomatically colonized patients, as well as mechanical ventilators and hospital plumbing, as reservoirs of CRKP that facilitate nosocomial spread despite rigorous infection control procedures [14]. Thus, there is an urgent need for novel CRKP prevention and treatment strategies, particularly in pediatric patients.
Acknowledgments
This work was supported by Public Health Service grants K23AI089271 (to R. P. M.) and 1R01AI090155 (to B. N. K.).
Disclaimer. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Kitchel B, et al. Molecular epidemiology of KPC-producing Klebsiella pneumoniae isolates in the United States: Clonal expansion of multilocus sequence type 258. Antimicrob Agents Chemother. 2009;53:3365–70. doi: 10.1128/AAC.00126-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacob JT, et al. Vital signs: Carbapenem-resistant. Enterobacteriaceae MMWR. 2013;62:165–70. [PMC free article] [PubMed] [Google Scholar]
- 3.Nordmann P, Naas T, Poirel L. Global spread of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 2011;17:1791–8. doi: 10.3201/eid1710.110655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen L, et al. Multiplex real-time PCR assay for detection and classification of Klebsiella pneumoniae carbapenemase gene (bla KPC) variants. J. Clin Microbiol. 2011;49:579–85. doi: 10.1128/JCM.01588-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai YK, et al. Klebsiella pneumoniae outer membrane porins OmpK35 and OmpK36 play roles in both antimicrobial resistance and virulence Antimicrob Agents Chemother. 2011;55:1485–93. doi: 10.1128/AAC.01275-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CLSI document M100-S23. Wayne, PA: Clinical and Laboratory Standards Institute; 2013. In: Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Third Informational Supplement. [Google Scholar]
- 7.Diancourt L, et al. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol. 2005;43:4178–82. doi: 10.1128/JCM.43.8.4178-4182.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaczmarek FM, et al. High-level carbapenem resistance in a Klebsiella pneumoniae clinical isolate is due to the combination of bla(ACT-1) beta-lactamase production, porin OmpK35/36 insertional inactivation, and down-regulation of the phosphate transport porin phoe. Antimicrob Agents Chemother. 2006;50:3396–406. doi: 10.1128/AAC.00285-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naas T, et al. Genetic structures at the origin of acquisition of the beta-lactamase bla KPC gene. Antimicrob Agents Chemother. 2008;52:1257–63. doi: 10.1128/AAC.01451-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ribot EM, et al. Standardization of pulsed-field gel electrophoresis protocols for the subtyping of Escherichia coli O157:H7, Salmonella, and Shigella for PulseNet. Foodborne Pathog Dis. 2006;3:59–67. doi: 10.1089/fpd.2006.3.59. [DOI] [PubMed] [Google Scholar]
- 11.Patel G, et al. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008;29:1099–106. doi: 10.1086/592412. [DOI] [PubMed] [Google Scholar]
- 12.Pasteran F, et al. Sensitive screening tests for suspected class A carbapenemase production in species of Enterobacteriaceae. J Clin Microbiol. 2009;47:1631–9. doi: 10.1128/JCM.00130-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alba J, et al. Kinetics study of KPC-3, a plasmid-encoded class A carbapenem-hydrolyzing beta-lactamase. Antimicrob Agents Chemother. 2005;49:4760–2. doi: 10.1128/AAC.49.11.4760-4762.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Snitkin ES, et al. Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci Transl Med. 2012;4 doi: 10.1126/scitranslmed.3004129. p148ra116. [DOI] [PMC free article] [PubMed] [Google Scholar]