Abstract
Background
To evaluate intraocular pressure (IOP) changes in patients undergoing robotic-assisted radical prostatectomy and to evaluate complications from increased IOP.
Methods
Thirty-one eyes scheduled for robotic prostatectomy were included. Perioperative IOP measurements were performed as follows: prior to induction of anaesthesia while supine and awake (T1); immediately post-induction while supine (T2); every hour from 0 to 5 h while anaesthetised in a steep Trendelenburg position (T3–T8); prior to awakening while supine (T9); and 30 min after awakening while supine (T10). A complete ophthalmic examination including visual acuity and retinal nerve fibre layer thickness (RNFL) was performed at enrolment and 1 month postoperatively.
Results
Average IOP (mm Hg) for each time point was as follows: T1=18.0, T2=9.8, T3=18.9, T4=21.6, T5=22.5, T6=22.3, T7=24.2, T8=24.0, T9=15.7 and T10=17.9. The proportion of eyes with intraoperative IOP ≧30 mm Hg were as follows: T3=0%, T4=3.23%, T5=9.68%, T6=6.45%, T7=22.22%, and T8=25%. Maximum IOP was 36 mm Hg. Mean visual acuity (logarithm of the minimal angle of resolution) and RNFL showed no statistically significant difference before and after operation and no other ocular complications were found at final examination.
Conclusions
While IOP increased in a time-dependent fashion in anesthaetised patients undergoing robotic-assisted radical prostatectomy in a steep Trendelenburg position, visual function showed no significant change postoperatively and no complications were seen. Steep Trendelenburg positioning during time-limited procedures appears to pose little or no risk from IOP increases in patients without pre-existing ocular disease.
Keywords: Intraocular Pressure, Glaucoma
Introduction
Prostate cancer is the sixth most common cancer and the eighth leading cause of cancer death in Japan. It is estimated that prostate cancer will be the second most common cancer by 2020 and various treatments for prostate cancer are now available in Japan. Among them, robotic-assisted radical prostatectomy is one of the newest and most technically advanced modalities, with advantages that include stereoscopic visualisation and good manoeuvrability within the operating area. In Japan, robotic-assisted surgery (da Vinci S HD Surgical System; Intuitive Surgical, Inc, Sunnyvale, California, USA) began to be covered under government insurance from April 2012. Due to its surgical advantages in prostate cancer, the number of robotic surgeries has increased from 667 in 2011 to 1800 by October 2012.
Robotic-assisted radical prostatectomy requires specific body positioning in which the patients must be placed in a steep (23–45°) Trendelenburg position. Gravity allows the abdominal viscera to be pulled away from the pelvic cavity resulting in a clearer operating field. However, this positioning may lead to complications, with several ocular complications having been reported since the inception of robotic-assisted surgery. In 2007, Weber et al1 first reported posterior ischaemic optic neuropathy after a da Vinci robotic-assisted procedure. Since intraocular pressure (IOP) may theoretically increase due to steep Trendelenburg positioning, monitoring of IOP is warranted and physicians do remain vigilant for ocular complications during this procedure. Nonetheless, there is only one prior report regarding IOP changes during robotic-assisted radical prostatectomy.2 In 2009, Awad et al concluded that IOP reached peak levels after prolonged steep Trendelenburg positioning, on average 13 mm Hg higher than pre-anaesthesia induction values. However, intraoperative IOP changes and their adverse ocular effects have not been clarified yet.
The purpose of this study is thus to evaluate the IOP in patients who underwent robotic-assisted radical prostatectomy and to evaluate the effect on visual function by increased IOP.
Methods
This was a single-centre, prospective, non-randomised study. A total of 31 consecutive patients scheduled for robotic prostatectomy were recruited at St Luke's International Hospital in Tokyo, Japan from 20 January 2012 to 20 August 2012. All patients had their procedures performed within 1 month after recruitment. Patients with preexisting glaucoma or retinal vascular diseases which may affect neuroretinal function, or corneal diseases which may affect IOP measurement, were excluded. All aspects of this study were approved by the Institutional Review Board at the study site, and informed consent was obtained from all patients.
Patients scheduled for prostatectomy visited our ophthalmology department 1 month prior to and after the operation. A complete ophthalmic examination was performed at enrolment and again 1 month postoperatively, including determination of best-corrected visual acuity (VA), IOP measurement in sitting position by Goldmann applanation tonometer, slit-lamp biomicroscopy, indirect ophthalmoscopy, colour fundus photographs, and optical coherence tomography (OCT). VA was determined with the Snellen chart, and logarithm of the minimal angle of resolution (LogMAR) values were calculated for statistical analysis. The gonioscopic examination was performed and evaluated by Scheie classification. The anterior chamber was evaluated by the van Herick method only preoperatively. The average retinal nerve fibre layer (RNFL) thickness and the inferior RNFL thickness imaged by the Cirrus HD-OCT (Carl Zeiss Meditec Inc, Dublin, California, USA) were calculated to detect RNFL progression. Cut-off for OCT signal strength was 5.
On the day of the operation, IOP measurements were performed on each patient in both eyes with a Tono-pen XL handheld tonometer (Medtronic, Jacksonville, Florida, USA). Four separate measurements were taken, calculating the mean and SD. The tonometer was calibrated according to the manufacturer's guidelines before each reading. Measurements were repeated if the variability between sequential measurements exceeded 5%. The IOP was measured before induction of anaesthesia while supine and awake (T1), and immediately after induction while supine (T2). All patients were placed in a steep Trendelenburg position (23°, head down), after which IOP was measured every 1 h from (0 to 5 h) (T3–T8). Immediately after going back to the supine position postoperatively, IOP was again measured during anaesthesia (T9), as well as 30 min after awakening (T10). The operation time, arterial blood pressure and blood loss were also recorded. The anaesthesia protocol was standardised for drugs used during the procedure. Propofol was used for sedation, remifentanil and fentanyl were used for pain relief, and rocuronium was used for mascular relaxation. The lungs were mechanically ventilated. We maintained ETCO2 at 30–40 mmHg.
The primary endpoint of this study was change in IOP at each point; secondary endpoint was complication rate.
Only measurements from the left eye of each patient were included in this study. Mixed linear models (change in IOP) and paired t-test (change in VA and RNFL thickness) were used to evaluate these outcomes. Time-to-event analysis was performed to determine the cumulative hazard of IOP change at each time point during operation. A p value less than 0.05 was considered statistically significant. All analyses were done with SSPS V.15.0J (SPSS Japan, Tokyo, Japan).
Result
Thirty-one male patients (31 eyes) were enrolled in this study and underwent robotic-assisted radical prostatectomy. Patients’ ages ranged from 54 to 74 years old, with a mean of 66.15±5.40 years. Twenty-nine of 31 eyes (93.5%) were grade IV by the van Herick method; 2 eyes (6.5%) were grade III. In contrast, 27 of 31 eyes (87.1%) were graded wide open by Scheie classification; 4 of 31 eyes (12.9%) were grade I.
Mean operation time was 4.57±0.03 h (range 3 h 47 min–6 h 9 min). Mean blood loss was 364±196 ml (80–810 mL). Mean blood pressure was 104.8±12.1/56.4±5.8 mm Hg at T4, 95.9±11.6/51.8±6.0 mm Hg at T5, 94.3±13.7/52.0±6.9mm Hg at T6, 91.0±9.6/49.8±5.6 mm Hg at T7, and 86.7±5.8/48.8±2.9 mm Hg at T8. Mean VA (LogMAR) was 0.088 preoperatively and 0.089 postoperatively, with no statistically significant difference found before and after operation. Twenty-eight of 31 eyes (90.3%) underwent OCT. Mean average RNFL thickness was not significantly different before (91.0 μm) versus after (92.1 μm) the operation and inferior RNFL thickness was also not significantly different before (117.2 μm) versus after (117.2 μm) the operation. No other ocular complications were found at final examination. One month postoperative data from five patients were not able to be included due to loss to follow-up.
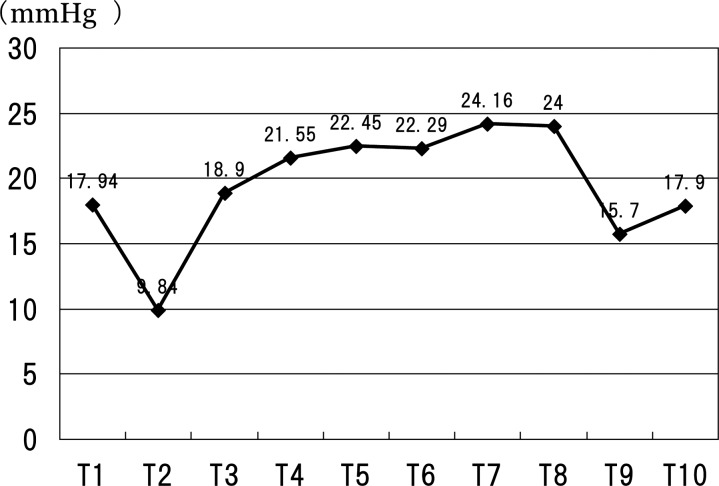
Mean (range) IOP was 13.2 mm Hg (8–20 mm Hg) preoperatively, 18.0 mm Hg (9–29 mm Hg) at T1, 9.8 mm Hg (4–15 mm Hg) at T2, 18.9 mm Hg (5–28 mm Hg) at T3, 21.6 mm Hg (15–31 mm Hg) at T4, 22.5 mm Hg (14–36 mm Hg) at T5, 22.3 mm Hg (9–33 mm Hg) at T6, 24.2 mm Hg (12–33 mm Hg; N=18) at T7, 24.0 mm Hg (14–34 mm Hg; N=4) at T8, 15.7 mm Hg (10–25 mm Hg) at T9, 17.9 mm Hg (8–26 mm Hg) at T10 and 13.2 mm Hg (8–18 mm Hg) postoperatively (figure 1). Compared with baseline, mean IOP was significantly lower at T2 (p < 0.001) and higher at T4 (p=0.005), T5 (p=0.000), T6 (p=0.000), T7 (p=0.000). Compared with T3, mean IOP was significantly higher at T5 (p=0.03), T6 (p=0.05), T7 (p=0.00). The T8 value was not analysed due to a small sample size.
Figure 1.
Scatter plot of mean intraocular pressure (IOP) at each time point. IOP increases time dependently after steep Trendelenburg positioning (T3–T8).
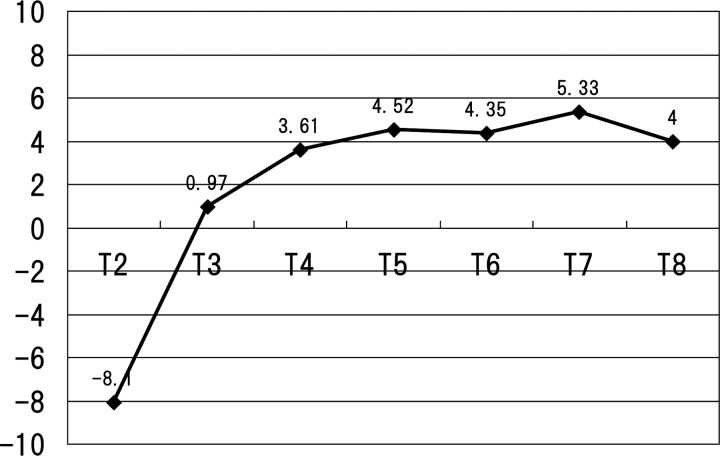
Maximum IOP was 36 mm Hg. The proportion of eyes with IOP ≥ 25 mm Hg during the operation were 0% (0/31 eyes) at T3, 22.58% (7/31 eyes) at T4, 32.26% (10/31 eyes) at T5, 38.70% (12/31 eyes) at T6, 38.89% (7/18 eyes) at T7, and 50% (2/4 eyes) at T8. The proportion of eyes with IOP ≥ 30 mm Hg during the operation were 0% (0/31 eyes) at T3, 3.23% (1/31 eyes) at T4, 9.68% (3/31 eyes) at T5, 6.45% (2/31 eyes) at T6, 22.22% (4/18 eyes) at T7 and 25% (1/4 eyes) at T8. The cumulative hazard in all patients to reach an IOP more than 30 mm Hg was 20% at T8. The mean change in IOP compared with T1 was −8.1 mm Hg at T2, +1.0 mm Hg at T3, +3.6 mm Hg at T4, +4.5 mm Hg at T5, +4.4 mm Hg at T6, +5.3 mm Hg at T7 and +4 mm Hg at T8 (figure 2). Table 1 shows the change in IOP from T1 at each patient.
Figure 2.
Mean change from baseline IOP (T1). IOP increases time dependently after steep Trendelenburg positioning (T3–T8).
Table 1.
The proportions of eyes that change from baseline intraocular pressure (T1) at each time point
| T2 | T3 | T4 | T5 | T6 | T7 | T8 | |
|---|---|---|---|---|---|---|---|
| More than 5 mm Hg | 0% (0/31) | 25.8% (8/31) | 45.2% (14/31) | 51.6% (16/31) | 48.4% (15/31) | 38.9% (7/18) | 50% (2/4) |
| More than 10 mm Hg | 0% (0/31) | 3.2% (1/31) | 9.7% (3/31) | 19.4% (6/31) | 25.8% (8/31) | 11.1% (2/18) | 0% (0/4) |
| More than 15 mm Hg | 0% (0/31) | 0% (0/31) | 0% (0/31) | 6.5% (2/31) | 12.9% (4/31) | 5.6% (1/18) | 0% (0/4) |
| More than 20 mm Hg | 0% (0/31) | 0% (0/31) | 0% (0/31) | 0% (0/31) | 3.2% (1/31) | 0% (0/18) | 0% (0/4) |
The proportions of eyes with change ≥15 mm Hg ranged from 0% at T3, increasing to 12.9% at T6.
Discussion
This study showed that IOP increases time dependently after steep Trendelenburg positioning in anaesthetised patients undergoing robotic-assisted radical prostatectomy. However, visual function (VA and RNFL thickness) showed no statistically significant changes. The mean IOP was 24.2 mm Hg, while maximum IOP reached 36 mm Hg. The proportion of eyes with IOP ≥ 30 mm Hg ranged from 0% at T3, increasing to 25% at T8. A total of 25.8% of eyes demonstrated an IOP change of 10mm Hg, while a change of ≥15 mm Hg was seen in 12.9%. VA and RNFL thickness did not change after versus before surgery.
Only one prior report by Awad et al2 has been published regarding change in IOP during robotic-assisted radical prostatectomy. However, only IOP data were shown in that report. The current study is the first to assess IOP and change in IOP during operation and its effect on visual function via acuity and RNFL thickness. Awad et al reported that anesthaetised patients had a mean IOP of 25.2 mm Hg measured by a Tono-pen XL handheld tonometer in steep Trendelenburg position (25°, head down), increased to 29.0 mm Hg while still in steep Trendelenburg at the end of the procedure. The reason for higher mean IOP compared with the present study remains unclear, although it is possible that this may reflect a racial difference.
The major determinants of IOP are aqueous humor flow, choroidal blood volume, central venous pressure (CVP) and extraocular muscle tone.3 We hypothesise two major theories to explain IOP increasing during operation. First, gravitational forces increase CVP which, in turn, affect orbital venous pressure and increase IOP. Second, intraperitoneal CO2 causes increased choroidal blood volume, which may result in IOP increase. In 2009, Awad et al2 reported that low end tidal CO2 (ETCO2) was a significant predictor of the IOP increase. As CO2 gas is typically used to induce pneumoperitoneum during robotic surgery, the authors estimated that continuous absorption of intraperitoneal CO2 and increased pressure on the diaphragm resulted in lower delivered tidal volumes and subsequently increased arterial PCO2 levels. This may lead to increased choroidal blood volume and increased IOP.
The present study showed that IOP remained significantly elevated for several hours. There are no previously published data concerning the safe threshold for transient IOP elevation. Numerous glaucoma studies have demonstrated that optic nerve damage depends on IOP, but optic nerve circulation, age, race, genetics and other factors are also critical.4–10 Compared with other ocular procedures which affect IOP, the range of IOP elevation in this study was not marked. In 2010, Höhn and Mirshahi11 assessed IOP after ranibizumab injection, in which mean IOP was 21.2 mm Hg before injection, 54.7, 43.4 and 28.3 mm Hg at 1, 3 and 10 min after injection, respectively. In 2011, Framme et al12 reported IOP after 20-gauge pars-plana vitrectomy. The overall cumulative hazard to reach an IOP ≥ 30 mm Hg after 24 h was 23.9%, while IOP ≥ 40 mm Hg was 8.2%. In the present study, the maximum IOP was 36 mm Hg. The overall cumulative hazard to reach IOP ≥ 30 mm Hg after 5 h was 20%; no patients reached an IOP ≥ 40 mm Hg. Our data suggest that IOP elevation may be limited during robotic-assisted radical prostatectomy compared with other treatments.
In 2007, Weber et al1 first reported a case of a 62-year-old patient who developed posterior ischaemic optic neuropathy after a robotic-assisted procedure lasting 6 h 35 min and with blood loss of 1200 mL. In the present study, the mean operation time was 4.57±0.03 h with mean blood loss of 364±196 mL. Although definitive evidence is lacking, the long operation time and large quantity of blood loss may be related to the occurrence of ischaemic optic neuropathy.
In this study, no patient experienced any ocular complications related to IOP increase, including ischaemic optic neuropathy. However, IOP was noted to increase in a time-dependent fashion. Along with previous reports, this suggests that longer operation times may induce substantially more risk for harmful IOP increases. More aggressive evaluation for elevated IOP may be warranted when operation times exceed 5 h, and acetazolamide may be considered. IOP would change much more with a larger head down degree. Moreover, patients with advanced glaucoma may not be good candidates for robotic surgery; thorough informed consent is prudent before robotic surgery because of the risk of ocular complications.
It should be mentioned that the relatively small number of patients in this study may limit the study conclusions. Moreover, as an ophthalmic examination was performed at only 1 month postoperatively, a reversible adverse effect can occur within this 1-month time period. Nonetheless, these data suggest that further study is necessary to ascertain IOP increase and its effect on visual function in the setting of extreme surgical positioning.
In conclusion, we found that IOP increased in a time-dependent fashion in anaesthetised patients undergoing robotic-assisted radical prostatectomy in a steep Trendelenburg position. Despite this increase, visual function showed no significant change postoperatively and no complications were seen.
Footnotes
Contributors: YH: conception and design, analysis and interpretation, writing the article, data collection, literature search. KO: critical revision of the article, final approval of the article. OT: statistical expertise. GAD: edited the English. NT, SS, MH, KI, KT, JK, NE and SF: data collection. No sponsor involvement.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Weber ED, Colyer MH, Lesser RL, et al. Posterior ischemic optic neuropathy after minimally invasive prostatectomy. J Neuroophthalmol 2007;27:285–7 [DOI] [PubMed] [Google Scholar]
- 2.Awad H, Santilli S, Ohr M, et al. The effects of steep Trendelenburg positioning on intraocular pressure during robotic radical prostatectomy. Anesth Analg 2009;109:473–8 [DOI] [PubMed] [Google Scholar]
- 3.Donlon JV, Jr, Doyle DJ, Feld man MA. Anethesia for eye, ear, nose and throat surgery. In Miller RD, ed. Miller's anesthesia. 6th edn Philadelphia: Elsevier, Churchill Livingstone, 2005 [Google Scholar]
- 4.Grunwald JE, Pitz J, Hariprasad SM, et al. Optic nerve and choroidal circulation in glaucoma. Invest Ophthalmol Vis Sci 1998;39:2329–36 [PubMed] [Google Scholar]
- 5.Buskirk EMV, Cioffi GA. Glaucomatous optic neuropathy. Am J Ophthalmol 1992;113:447–52 [DOI] [PubMed] [Google Scholar]
- 6.Leske MC, Connell AMS, Wu S, et al. The Barbados Eye Study Group. Risk factors for open-angle glaucoma. The Barbados Eye Study. Arch Ophthalmol 1995;113:918–24 [DOI] [PubMed] [Google Scholar]
- 7.Klein BEK, Klein R, Sponsel WE, et al. Prevalence of glaucoma. The Beaver Dam Eye Study. Ophthalmology 1992;99:1499–504 [DOI] [PubMed] [Google Scholar]
- 8.Wensor MD, McCarty CA, Stanislavsky YL, et al. The prevalence of glaucoma in the Melbourne visual impairment project. Ophthalmology 1998;105:733–9 [DOI] [PubMed] [Google Scholar]
- 9.Mitchell P, Smith W, Attebo K, et al. Prevalence of open-angle glaucoma in Australia. The Blue Mountains Eye Study. Ophthalmology 1996;103:1661–9 [DOI] [PubMed] [Google Scholar]
- 10.Mabuchi F, Tang S, Kashiwagi K, et al. The OPA1 gene polymorphism is associated with normal tension and high tension glaucoma. Am J Ophthalmol 2007;143:125–30 [DOI] [PubMed] [Google Scholar]
- 11.Höhn F, Mirshahi A. Impact of injection techniques on intraocular pressure (IOP) increase after intravitreal ranibizumab application. Graefes Arch Clin Exp Ophthalmol 2010;248:1371–5 [DOI] [PubMed] [Google Scholar]
- 12.Framme C, Klotz S, Wolf-Schnurrbusch UE, et al. Intraocular pressure changes following 20G pars-plana vitrectomy. Acta Ophthalmol 2012;90:744–9 [DOI] [PubMed] [Google Scholar]