Abstract
Background
Cardiovascular disease is a major concern in persons with chronic kidney disease (CKD). We assessed the current burden of cardiovascular risk factors and differences in risk factor treatment and control in the general U.S. adult population by CKD status.
Methods
Cross-sectional study of 10,741 adults aged 20+ years from the 2007-2010 National Health and Nutrition Examination Survey. Persons were categorized into three groups: CKD Stages 3-5 (estimated glomerular filtration rate [eGFR]<60mL/min/1.73m2), CKD Stages 1-2 (urinary albumin-to-creatinine ratio≥30mg/g and eGFR≥60mL/min/1.73m2), and no CKD.
Results
The majority of adults with CKD Stages 3-5 (79.8%) and Stages 1-2 (59.1%) had ≥2 cardiovascular risk factors, substantially higher than adults without CKD (32.7%, p<0.001). Diabetes was the most strongly associated risk factor and was highly specific for CKD Stages 1-2 (prevalence ratio [PR] 2.53, 95% confidence interval [CI] 2.21-2.89) and, to a lesser extent, CKD Stages 3-5 (PR 1.59, 95%CI 1.38-1.84). Most adults with diagnosed risk factors reported medication use for risk factor control, and pharmacologic treatment was more common among those with than without CKD. However, poor risk factor control was also common among persons treated for risk factors with CKD compared to those without CKD.
Conclusions
There continues to be a substantial cardiovascular risk factor burden among adults with CKD Stages 3-5 and, to a lesser extent, adults with CKD Stages 1-2, when compared to adults without CKD. Overall, optimal risk factor control is low in adults with CKD, highlighting the need for aggressive cardiovascular risk reduction in adults with CKD.
Introduction
Chronic kidney disease (CKD) is common in the United States, affecting an estimated 26 million adults.1 In addition to the progression of CKD to kidney failure, cardiovascular disease (CVD) remains a major concern in persons with CKD, as both albuminuria and reduced glomerular filtration rate (GFR) are associated with CVD morbidity and mortality and a high burden of traditional cardiovascular risk factors, including hypertension, diabetes, and dyslipidemia.2-6 Indeed, in the general population, persons with CKD have a higher risk of death from CVD than progression to end-stage renal disease.2, 7 In spite of the excess cardiovascular risk associated with CKD, clinical guidelines for cardiovascular risk reduction differ regarding persons with CKD. The Kidney Disease Outcomes Quality Initiative (K/DOQI) and the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) recommend that persons with CKD be classified as “highest risk” for CVD risk stratification and lower blood pressure treatment goals when treating hypertension in this group than among adults without CKD or diabetes.8, 9 In contrast, the Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults does not consider CKD to be a coronary heart disease (CHD) risk equivalent for cholesterol control.10
Few studies have evaluated recent levels of risk factor burden by CKD status in the U.S. Earlier work from the National Health and Nutrition Examination Survey (NHANES) suggests that the prevalence of hypertension, diabetes, and high cholesterol is high among adults with CKD and albuminuria11 but the prevalence of hypertension and high cholesterol has declined between 1988-1994 and 1999-2004.11 A decreasing trend in the prevalence of uncontrolled blood pressure was also observed among those with and without CKD between 1999 and 2006, but the prevalence of uncontrolled blood pressure remains high among those with CKD.12 Adults with CKD in the community-based Framingham Offspring cohort were more likely to have multiple cardiovascular risk factors and uncontrolled hypertension or diabetes when compared to those without kidney disease.13 Less is known, however, about risk factor combinations observed among adults with and without CKD in the general population. Additionally, while albuminuria and reduced estimated GFR are both independent predictors of CVD and all-cause mortality,4, 5 they are associated with different cardiovascular risk factor profiles.14 The burden of cardiovascular risk factors and their control among adults with albuminuria compared to those with reduced estimated glomerular filtration rate (eGFR) or without CKD has not been previously characterized in the general U.S. population. The objectives of this study were to use the most recent national data available to estimate the prevalence of CVD and its major risk factors including hypertension, hypercholesterolemia, and diabetes by CKD status and to evaluate potential differences in prevalence, treatment, and control of CVD risk factors among U.S. adults by CKD status.
Methods
Study population
We analyzed data from the 2007-10 NHANES, a cross-sectional, multistage, stratified, clustered probability sample of the U.S. civilian non-institutionalized population conducted by the National Center for Health Statistics (NCHS).15 The present analysis included 10,741 adults ≥20 years old who attended the mobile examination center visit, were not pregnant, or missing urinary albumin or creatinine measurements.
Cardiovascular risk factor assessment
Age, sex, race/ethnicity, and smoking status were self-reported. Seated systolic and diastolic blood pressures were averaged over up to 4 readings; hemoglobin A1c (HbA1c) and total cholesterol were assayed using standard techniques.15 Hypertension was defined as blood pressure ≥140/90mmHg or a self-reported physician diagnosis of hypertension. Undiagnosed hypertension was defined as blood pressure ≥140/90mmHg among adults without a hypertension diagnosis; diagnosed hypertension was defined as a self-reported physician diagnosis. Hypercholesterolemia was defined as total cholesterol ≥200mg/dL or a self-reported physician diagnosis of high cholesterol. Undiagnosed hypercholesterolemia was defined as a total cholesterol ≥200mg/dL among adults without a diagnosis of high cholesterol; diagnosed hypercholesterolemia was defined as a self-reported physician diagnosis. Diabetes was defined as an HbA1c≥6.5%,16 a self-reported physician diagnosis of diabetes, or self-reported use of diabetes medication. Undiagnosed diabetes was defined as HbA1c≥6.5% among those without a diagnosis of diabetes; diagnosed diabetes was defined as a self-reported physician diagnosis. Participants were classified as having a history of CVD if they reported that a doctor or other health professional has ever told them they had congestive heart failure, CHD, heart attack, or stroke. Among adults reporting physician diagnoses for cardiovascular risk factors, risk factor control was defined as having blood pressure <140/90mmHg for hypertension (<130/80 mmHg for eGFR<60mL/min/1.73m2, urinary albumin-to-creatinine ratio [UACR]>200mg/g, or diabetes9), HbA1c<7% for diabetes, and total cholesterol<200 mg/dL for hypercholesterolemia.
CKD assessment
Serum creatinine was measured using the Jaffe rate method from refrigerated serum samples and urinary albumin and creatinine were measured using enzymatic methods in urine samples collected during the examination.15 The UACR (mg/g) was computed as urinary albumin/urinary creatinine. GFR was estimated (eGFR) using the Chronic Kidney Disease-Epidemiology 2009 equation based on age, sex, race, and serum creatinine.17 We defined three mutually exclusive CKD groups using eGFR and UACR.8 Persons with eGFR<60 mL/min/1.73m2 were classified as CKD Stages 3-5, those with UACR≥30 mg/g and eGFR≥60 mL/min/1.73m2 were classified as CKD Stages 1-2, and those with UACR<30mg/g and eGFR≥60 mL/min/1.73m2 were classified as not having CKD.
Statistical analyses
Statistical analyses were performed using Stata v11.1 (StataCorp, http://www.stata.com/). As recommended by NCHS,15 we estimated standard errors using the Taylor series (linearization) method. We implemented weights that account for oversampling in the complex survey design, non-response, and post-stratification adjustment to produce nationally representative estimates.15, 18 Specifically, we created 4-year sampling weights by assigning ½ of the 2-year cycle weight for each participant, as recommended by NCHS.18 Using 2010 U.S. census population, we estimated the numbers within each CKD group, overall and by demographic subgroups. Adjusted prevalence ratios (PR) of hypertension, hypercholesterolemia, diabetes, and CVD were obtained using Poisson regression,19 adjusting for age, sex, and race. Among adults with diagnosed risk factors, we estimated the prevalence of treatment and control of risk factors across CKD groups.
The NHANES was approved by the NCHS Research Ethics Review Board and participants provided informed consent.20-22 The authors are solely responsible for study design and conduct, all study analyses, the drafting and editing of the paper and its final contents. This research was supported by the National Kidney Foundation, Merck Sharp and Dohme Corp. (professional service agreement to the National Kidney Foundation), and a NIH/NHLBI Cardiovascular Epidemiology Training Grant.
Results
Participant characteristics and risk factor burden
CKD Stages 3-5 and Stages 1-2 were present in 6.4% and 7.1% of adults aged 20 or older, respectively, corresponding to 14 million U.S. adults with CKD Stages 3-5 and 16 million with CKD Stages 1-2 in 2010 (Table 1). Persons with CKD Stages 3-5 were substantially older, more likely to be female and non-Hispanic white, and less likely to be current smokers than adults who have CKD Stages 1-2 or without CKD (Table 2). In all three CKD groups, a high proportion with hypertension (79-83%), diabetes (75-86%), and hypercholesterolemia (61-80%) reported a physician diagnosis of these conditions. We observed a shift in risk factor frequency across CKD groups (Figure 1, Supplemental Table 1); ≥2 risk factors were present in 79.8% of adults with CKD Stages 3-5 compared to 59.1% of adults with CKD Stages 1-2 and 32.7% of adults without CKD.
Table 1. Prevalence and estimated number of adults age 20 years and older within each chronic kidney disease (CKD) group based on 2010 U.S. Census.
| Prevalence (%) | 2010 Population Estimates (in millions)* | |||||
|---|---|---|---|---|---|---|
| No CKD | CKD Stages 1-2 | CKD Stages 3-5 | No CKD | CKD Stages 1-2 | CKD Stages 3-5 | |
| Overall | 86.5 | 7.1 | 6.4 | 195.0 | 16.0 | 14.5 |
| Age | ||||||
| <65 years | 92.1 | 6.1 | 1.7 | 170.6 | 11.4 | 3.2 |
| ≥65 years | 59.1 | 11.7 | 29.2 | 23.8 | 4.7 | 11.8 |
| Sex | ||||||
| Women | 84.8 | 7.6 | 7.6 | 98.6 | 8.9 | 8.8 |
| Men | 88.3 | 6.5 | 5.2 | 96.4 | 7.1 | 5.7 |
| Race | ||||||
| Non-Hispanic White | 86.1 | 6.4 | 7.5 | 130.8 | 9.7 | 11.5 |
| Non-Hispanic Black | 85.0 | 9.0 | 5.9 | 22.1 | 2.4 | 1.5 |
| Hispanic | 88.2 | 9.1 | 2.7 | 27.8 | 2.9 | 0.8 |
Subgroup totals may not sum to the overall estimates due to rounding.
Table 2. Characteristics and cardiovascular disease (CVD) risk factor burden by chronic kidney disease (CKD) group, U.S. adults aged 20 years or older, NHANES 2007-2010.
| Characteristic | No CKD | CKD Stages 1-2 | CKD Stages 3-5 |
|---|---|---|---|
| NHANES participants, n* | 8809 | 984 | 948 |
| Age (years) | 44.9 (0.3) | 52.1 (0.6) | 71.2 (0.7) |
| Sex (% women) | 49.7 (0.5) | 55.2 (1.8) | 60.7 (1.9) |
| Race/ethnicity (%) | |||
| Non-Hispanic White | 69.3 (2.5) | 62.7 (3.7) | 81.6 (2.1) |
| Non-Hispanic Black | 10.3 (1.0) | 13.4 (1.5) | 9.6 (1.3) |
| Hispanic† | 13.7 (1.7) | 17.3 (2.6) | 5.6 (1.3) |
| Other‡ | 6.7 (0.8) | 6.5 (1.6) | 3.1 (0.8) |
| Smoking status (%) | |||
| Current | 22.1 (0.9) | 24.2 (1.6) | 9.2 (1.0) |
| Former | 23.5 (0.8) | 24.8 (1.5) | 39.0 (1.7) |
| Never | 54.3 (1.3) | 51.0 (2.0) | 51.7 (2.1) |
| Body Mass Index (kg/m2) | 28.4 (0.1) | 29.8 (0.4) | 29.4 (0.2) |
| Estimated glomerular filtration rate (mL/min/1.73m2) | 98.2 (0.5) | 94.5 (0.8) | 47.5 (0.5) |
| Urinary albumin-to-creatinine ratio (mg/g) | 5.8 [4.0, 8.8] | 61.8 [40.5, 131.5] | 12.1 [5.9, 38.4] |
| Hypertension (%) | 31.7 (0.8) | 57.8 (2.0) | 85.6 (2.0) |
| Undiagnosed | 17.0 (1.3) | 21.1 (1.8) | 17.0 (1.3) |
| Diagnosed | 83.0 (1.3) | 78.9 (1.8) | 83.0 (1.3) |
| Diabetes (%) | 8.0 (0.4) | 29.7 (2.0) | 30.7 (1.7) |
| Undiagnosed | 24.8 (1.6) | 17.1 (2.5) | 13.5 (2.5) |
| Diagnosed | 75.2 (1.6) | 82.9 (2.5) | 86.5 (2.5) |
| Hypercholesterolemia (% with ≥200 mg/dL) | 69.8 (0.7) | 72.2 (2.3) | 74.3 (2.4) |
| Undiagnosed | 39.1 (1.0) | 30.0 (1.0) | 20.0 (1.0) |
| Diagnosed | 60.9 (1.0) | 70.0 (2.4) | 80.0 (2.2) |
| History of CVD (%) | 5.5 (0.3) | 13.0 (1.4) | 29.6 (2.2) |
| History of coronary heart disease or myocardial infarction (%) | 3.7 (0.3) | 8.0 (1.1) | 17.6 (1.4) |
| History of stroke (%) | 1.9 (0.2) | 5.3 (0.8) | 12.0 (1.7) |
| History of congestive heart failure (%) | 1.3 (0.1) | 3.9 (0.6) | 11.1 (1.5) |
Note: Presented as weighted mean (standard error) for continuous and weighted proportions for categorical characteristics
Corresponds to 195 million adults with no CKD, 16 million with CKD Stages 1-2, and 14 million with CKD Stages 3-5 in 2010 when weighted estimates from the NHANES 2007-10 are applied to the 2010 U.S. Census
Includes Mexican American and Other Hispanic
Includes all other race/ethnic groups, including multiracial
Figure 1.
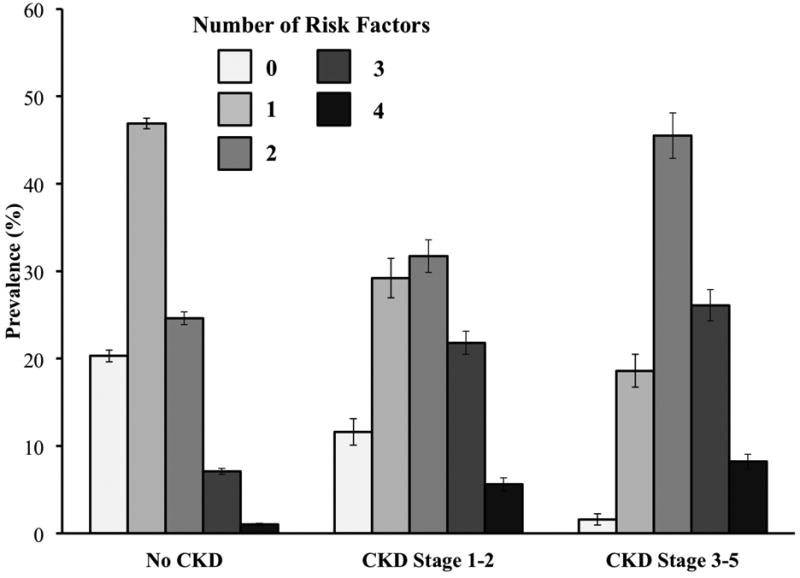
Number of prevalent cardiovascular risk factors among U.S. adults by chronic kidney disease (CKD) group. Error bars represent +/- the standard error.
CVD was present among 29.6% and 13.0% of adults with CKD Stages 3-5 and Stages 1-2, respectively, compared to 5.5% of those without CKD; this elevated prevalence persisted after accounting for age, sex, and race (adjusted PR 1.50 and 1.44, respectively, both p≤0.001; Table 3, unadjusted PR in Supplemental Table 2). Hypertension was present among 85.6% of persons with CKD Stages 3-5, compared to 57.8% of those with CKD Stages 1-2 and only 31.7% of those without CKD (Table 2). The higher prevalence of hypertension among adults with CKD Stages 3-5 or CKD Stages 1-2 was attenuated but persisted even after accounting for age, sex, and race (adjusted PRs 1.19 and 1.37, respectively, compared to no CKD, both p<0.001; Table 3, unadjusted PRs in Supplemental Table 2). Diabetes was present in 30.7% of adults with CKD Stages 3-5 and 29.7% of adults with CKD Stages 1-2 compared to only 8.0% of adults without CKD (Table 2). Adults with CKD Stages 3-5 were 1.6-times more likely, and adults with CKD Stages 1-2 were 2.5-times more likely, to have diabetes than those without CKD (Table 3; both p<0.001). In contrast, the prevalence of hypercholesterolemia was similar across CKD groups before adjustment for basic demographic factors, ranging from 69.8-74.3%. After adjusting for age, sex, and race, adults with CKD Stages 3-5 were less likely to have hypercholesterolemia than those without CKD (Table 3; adjusted PR 0.90, p=0.004). PR estimates for hypertension, diabetes, and hypercholesterolemia were similar in adults with and without a history of CVD (Table 3).
Table 3. Age-, sex-, and race-adjusted prevalence ratios of the association of CKD status with cardiovascular disease risk factors, overall and by history of CVD, U.S. adults aged 20 or older.
| No CKD | CKD stage 1-2 | CKD stage 3-5 | |
|---|---|---|---|
| Overall Sample | |||
| Hypertension | 1.00 (Ref) | 1.37 (1.27, 1.48) p<0.001 | 1.19 (1.12, 1.27) p<0.001 |
| Hypercholesterolemia | 1.00 (Ref) | 0.98 (0.92, 1.05) p=0.56 | 0.90 (0.84, 0.97) p=0.004 |
| Diabetes | 1.00 (Ref) | 2.53 (2.21, 2.89) p<0.001 | 1.59 (1.38, 1.84) p<0.001 |
| History of CVD | 1.00 (Ref) | 1.44 (1.18, 1.77) p<0.001 | 1.50 (1.24, 1.81) p=0.001 |
| Adults with history of CVD | |||
| Hypertension | 1.00 (Ref) | 1.21 (1.09, 1.33) p<0.001 | 1.19 (1.00, 1.28) p=0.05 |
| Hypercholesterolemia | 1.00 (Ref) | 1.04 (0.89, 1.22) p=0.60 | 0.98 (0.86, 1.11) p=0.70 |
| Diabetes | 1.00 (Ref) | 2.15 (1.74, 2.66) p<0.001 | 1.59 (1.26, 2.01) p<0.001 |
| Adults with no history of CVD | |||
| Hypertension | 1.00 (Ref) | 1.39 (1.29, 1.51) p<0.001 | 1.27 (1.18, 1.36) p<0.001 |
| Hypercholesterolemia | 1.00 (Ref) | 0.98 (0.92, 1.04) p=0.47 | 0.91 (0.84, 0.98) p=0.02 |
| Diabetes | 1.00 (Ref) | 2.55 (2.22, 2.93) p<0.001 | 1.52 (1.28, 1.81) p<0.001 |
Cardiovascular risk factor treatment and control
Among adults with diagnosed hypertension, the prevalence of anti-hypertensive medication use was high, although it was more common in adults with CKD than in adults without CKD (Table 4). However, only 44% of persons with CKD Stages 3-5 and 42% of persons with CKD Stages 1-2, compared to 69% of those without CKD, achieved adequate blood pressure control while on treatment. Diabetes medication use was also high among adults with diagnosed diabetes in all three groups, although the proportion achieving optimal HbA1c (<7.0%) while on treatment was low; only 55% with CKD Stages 3-5 and less than half with CKD Stages 1-2 or without CKD had achieved optimal HbA1c. The proportion of adults with diagnosed hypercholesterolemia reporting medication use was lower than observed for hypertension and diabetes, and controlled hypercholesterolemia was present in 68% of adults with CKD Stages 3-5 compared to 59% of adults with CKD Stages 1-2 and 56% of those without CKD.
Table 4. Prevalence of risk factor treatment and control in adults with self-reported physician diagnoses of hypertension, diabetes, or hypercholesterolemia by chronic kidney disease (CKD).
| No CKD | CKD stage 1-2 | CKD stage 3-5 | |
|---|---|---|---|
| % (S.E.) | % (S.E.) | % (S.E.) | |
| Diagnosed Hypertension* | |||
| Untreated | 20 (1.3) | 9.7 (1.9) | 2.5 (0.7) |
| Treated† | 80 (1.3) | 90.2 (1.9) | 97.5 (0.7) |
| Treated, Uncontrolled Blood Pressure‡ | 31 (1.3) | 58 (3.9) | 56 (2.4) |
| Treated, Controlled Blood Pressure‡ | 69 (1.5) | 42 (3.9) | 44 (2.4) |
| Diagnosed Diabetes* | |||
| Untreated | 15 (2.2) | 8.1 (1.5) | 7.8 (1.7) |
| Treated† | 85 (2.2) | 91.9 (1.5) | 92.2 (1.7) |
| Treated, Uncontrolled HbA1c§ | 52 (3.7) | 58 (4.8) | 44 (3.5) |
| Treated, Controlled HbA1c§ | 48 (3.7) | 42 (4.8) | 55 (3.5) |
| Diagnosed Hypercholesterolemia* | |||
| Untreated | 39 (1.6) | 24 (2.4) | 15 (1.7) |
| Treated† | 61 (1.6) | 76 (2.4) | 85 (1.7) |
| Treated, Uncontrolled Hypercholesterolemia¶ | 44 (1.6) | 41 (3.9) | 32 (2.4) |
| Treated, Controlled Hypercholesterolemia¶ | 56 (1.6) | 59 (3.9) | 68 (2.4) |
Diagnosed hypertension, diabetes, and hypercholesterolemia are defined as a physician or health care professional diagnosis based on self-report.
Treated and untreated hypertension, diabetes, or hypercholesterolemia defined as medication use for these risk factors based on self-report.
Uncontrolled blood pressure: ≥140/90 mmHg (≥130/80 mmHg for eGFR <60mL/min/1.73m2, UACR>200 mg/g, or diabetes); controlled blood pressure: <140/90 mmHg (<130/80 mmHg for eGFR <60mL/min/1.73m2, UACR>200 mg/g, or diabetes)
Uncontrolled HbA1c: ≥7.0%; controlled HbA1c: <7.0%
Uncontrolled hypercholesterolemia: total cholesterol ≥200 mg/dL; controlled hypercholesterolemia: total cholesterol <200 mg/dL.
Discussion
There is a substantial burden of CVD and its risk factors among U.S. adults with CKD Stages 3-5 and, to a lesser extent, for adults with CKD Stages 1-2 even after accounting for differences in age, sex, and race. Our findings represent the most current estimates of the cardiovascular risk factor burden and control among adults with and without CKD in the U.S. We found that adults with CKD compared to those without CKD are more likely to have multiple clinically recognized cardiovascular risk factors, and while the majority of adults with clinically recognized risk factors reported medication use for risk factor control, pharmacologic treatment was more common among those with than without CKD, suggesting more contact with the health care system in this group.
Few studies have focused on the burden of CVD and its risk factors in moderate forms of CKD in the general population.11, 13, 14 In NHANES 1999-2004, the prevalence of hypertension, diagnosed diabetes, and high cholesterol was 70.5%, 16.8%, and 44.4%, respectively, in adults with CKD Stage 3 (eGFR 30-59 mL/min/1.73m2; adults with eGFR<30mL/min/1.73m2 were excluded) and 57.4%, 21.6%, and 33.6%, respectively, in adults with albuminuria (UACR≥30 mg/g), all substantially higher than the prevalence observed in adults without stage 3 CKD (eGFR ≥60mL/min/1.73m2) or without albuminuria (UACR<30mg/g).11 Similarly in the Framingham Offspring cohort (1998-2001), the burden of hypertension (71.2% vs. 42.7%), diabetes (23.5% vs. 11.9%), and prevalent CVD (32.0% vs. 10.7%) was higher among those with CKD (eGFR <59 mL/min/1.73m2 in men; <64 mL/min/1.73m2 in women) as compared to those without CKD.13 Our findings extend the current literature to report on cardiovascular risk factor burden separately in persons with reduced eGFR regardless of albuminuria status (CKD Stages 3-5) and those with albuminuria without reduced eGFR (CKD Stages 1-2). Given the differences in kidney disease categorization and risk factor definitions, direct comparisons between our findings and prior work are not straightforward, although our findings are consistent with prior studies in that the burden of hypertension, diabetes, and prevalent CVD continue to be significantly higher in U.S. adults with CKD when compared to those without CKD.
We found that the prevalence of hypercholesterolemia was similar across the three groups based on kidney disease status in contrast to prior NHANES work which defined high cholesterol using a higher cut point (total cholesterol ≥240 mg/dL).11 Nevertheless the importance of serum lipids levels in CKD should not be overlooked. Adults with CKD can have altered lipid profiles even in early stages of CKD, such as elevated triglycerides and decreased HDL cholesterol in the presence of low-to-normal LDL cholesterol.23 The extent of these differences in the lipid profile may not be fully captured by total cholesterol alone, potentially underestimating the role of serum lipids in CVD risk in this population.
Prior work investigating cardiovascular risk factor treatment and control in moderate forms of CKD has focused on hypertension. In NHANES 1999-2002, the prevalence of uncontrolled blood pressure in adults with hypertension was higher in those who also had CKD (Stages 3-4, with eGFR ≥15 and <60 mL/min/1.73m2, 71.8%) than in adults who did not have CKD (eGFR ≥60mL/min/1.73m2, 56.4%).12 By 2003-06, the prevalence of uncontrolled blood pressure in hypertension decreased both in adults with CKD (66.3%) and without CKD (47.3%).12 Our findings from NHANES 2007-10 are consistent with a continued decline in the prevalence uncontrolled blood pressure in hypertension in adults with and without CKD. We also found, however, that the prevalence of uncontrolled hypertension was higher in adults CKD Stages 1-2 compared to CKD stages 3-5, suggesting that adults with albuminuria could benefit from targeted interventions to improve blood pressure control.
The increased prevalence of clinically recognized CVD, risk factors, and their treatment among adults with CKD may be partially attributable to the older age of persons with CKD and more frequent contact with the health care system. The increased prevalence of risk factor treatment in adults with CKD is consistent with current K/DOQI and JNC-7 guidelines, which recommend that adults with CKD be considered high risk for CVD risk stratification and the application of lower blood pressure treatment goals.8, 9 Nevertheless, despite the higher prevalence of treatment for hypertension, diabetes, and hypercholesterolemia, the proportion of adults with CKD currently achieving risk factor control was low. This suboptimal risk factor control in spite of higher treatment rates may be due to the low disease awareness of CKD among patients and clinicians.24, 25 Estimates from the 1999-2008 NHANES demonstrate that only 6-9% of adults with CKD are aware of their disease.24, 25 Low patient awareness may also reflect low physician awareness of the importance of CKD, potentially leading to less intensive treatment in patients who may benefit from more aggressive risk factor control. Increasing awareness of CKD and its associated high CVD risk in both patients and health care providers may improve adherence and treatment intensification to reduce CVD risk and may lead to improvements in prevention and early detection of CKD. A greater emphasis in current guidelines on CKD as a CHD risk equivalent in guidelines for cardiovascular risk factor control could help towards achieving this goal.
While we focused on the burden of CVD and its major risk factors in CKD, it is also important to consider the impact of CKD in CVD. CKD and CVD share several risk factors and CKD is an established risk factor for cardiovascular events.26 The burden of CKD in adults with CVD is also high and has increased considerably in the past two decades in the US, from 25.4% in 1988-94 to 40.8% in 2005-10.27
Several limitations of this study deserve consideration. The cross-sectional design limits our ability to assess the directionality of observed associations. In contrast to hypertension, diabetes, and hypercholesterolemia, prevalent CVD was assessed based solely on self-reported physician diagnoses. Adults with CVD, with a more adverse cardiovascular risk factor profile, and/or with severe forms of kidney disease are at increased risk of mortality and may be less likely to participate in NHANES. Thus, it is possible that our findings underestimate the prevalence of CVD and its risk factors. Undiagnosed diabetes was identified using a single HbA1c measurement; it is likely that we would identify additional cases if our definition included fasting plasma glucose. However, fasting plasma glucose is only available in a subsample of participants whereas HbA1c was measured in all participants who provided a blood sample. Current guidelines define CKD as reduced GFR or albuminuria for a period of at least three months,8 whereas we assessed kidney function based on single measurements of serum creatinine and UACR, which may have resulted in misclassification and overestimation of CKD, particularly for albuminuria in CKD Stages 1-2. The use of single spot urine samples for UACR may also underestimate risk factor burden among adults with CKD stages 1-2, as while repeated UACR measurements may identify fewer adults with albuminuria, those identified would have more severe disease. Thus, our findings likely represent a conservative risk burden estimate in this group.
There are several strengths of this study. This study benefited from the large nationally representative sample and its cross-sectional design, which is ideal for estimating risk factor burden in the general population. Our study sample was comprised of persons from the two most recent NHANES cycles and our findings represent the most current estimates of cardiovascular risk factor burden among adults with and without CKD in the U.S. Furthermore, all clinical measures used to assess kidney function and cardiovascular risk factors were obtained using standardized protocols and trained personnel.
In summary, we have updated estimates of the high burden of CVD and its risk factors among U.S. adults with CKD and demonstrated the differences between CKD stages marked by reduced kidney function or only albuminuria. Treatment for hypertension, diabetes, and hypercholesterolemia was more common in the presence of CKD, although the proportion achieving optimal risk factor control overall and among those under treatment was low. There is room for substantial improvement in cardiovascular risk factor control among U.S. adults with CKD.
Supplementary Material
Acknowledgments
Funding Acknowledgement: This study was supported by the National Kidney Foundation (grant to Johns Hopkins) and Merck Sharp and Dohme Corp., a subsidiary of Merck & Co., Inc., Whitehouse Station, NJ (professional service agreement to the National Kidney Foundation). DN and EM are employees of Merck and own stock in the company. MCF is supported by a NIH/NHLBI T32HL007024 Cardiovascular Epidemiology Training Grant. The National Health and Nutrition Examination Survey is funded by the National Center for Health Statistics, Centers for Disease Control and Prevention, Department of Health and Human Services.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 2.Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108(17):2154–2169. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 3.Coresh J, Astor B, Sarnak MJ. Evidence for increased cardiovascular disease risk in patients with chronic kidney disease. Curr Opin Nephrol Hypertens. 2004;13(1):73–81. doi: 10.1097/00041552-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Astor BC, Hallan SI, Miller ER, 3rd, et al. Glomerular filtration rate, albuminuria, and risk of cardiovascular and all-cause mortality in the US population. Am J Epidemiol. 2008;167(10):1226–34. doi: 10.1093/aje/kwn033. [DOI] [PubMed] [Google Scholar]
- 5.Matsushita K, van der Velde M, Astor BC, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375(9731):2073–81. doi: 10.1016/S0140-6736(10)60674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 7.Keith DS, Nichols GA, Gullion CM, et al. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med. 2004;164(6):659–663. doi: 10.1001/archinte.164.6.659. [DOI] [PubMed] [Google Scholar]
- 8.K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2):S1–266. [PubMed] [Google Scholar]
- 9.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 10.Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. [PubMed] [Google Scholar]
- 11.Fox CS, Muntner P. Trends in diabetes, high cholesterol, and hypertension in chronic kidney disease among U.S. adults: 1988-1994 to 1999-2004. Diabetes Care. 2008;31(7):1337–42. doi: 10.2337/dc07-2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Plantinga LC, Miller ER, 3rd, Stevens LA, et al. Blood pressure control among persons without and with chronic kidney disease: US trends and risk factors 1999-2006. Hypertension. 2009;54(1):47–56. doi: 10.1161/HYPERTENSIONAHA.109.129841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parikh NI, Hwang SJ, Larson MG, et al. Cardiovascular disease risk factors in chronic kidney disease: overall burden and rates of treatment and control. Arch Intern Med. 2006;166(17):1884–1891. doi: 10.1001/archinte.166.17.1884. [DOI] [PubMed] [Google Scholar]
- 14.Foster MC, Hwang SJ, Larson MG, et al. Cross-classification of microalbuminuria and reduced glomerular filtration rate: associations between cardiovascular disease risk factors and clinical outcomes. Arch Intern Med. 2007;167(13):1386–1392. doi: 10.1001/archinte.167.13.1386. [DOI] [PubMed] [Google Scholar]
- 15.NHANES - Questionnaires Datasets and Related Documentation. [accessed 01/15/2013]; http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 16.Standards of medical care in diabetes--2013. Diabetes care. 2013;36(Suppl 1):S11–66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Continuous NHANES Web Tutorial: Specifying Weighting Parameters. [Accessed 01/15/2013]; URL: http://www.cdc.gov/nchs/tutorials/NHANES/SurveyDesign/Weighting/OverviewKey.htm.
- 19.McNutt LA, Wu C, Xue X, et al. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157(10):940–3. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 20.NHANES – NCHS Research Ethics Review Board Approval. [Accessed January 11, 2013]; URL: http://www.cdc.gov/nchs/nhanes/irba98.htm.
- 21.NHANES – NHANES 2007-2008 – General Release File Documentation. [Accessed January 11, 2013]; URL http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/generaldoc_e.htm.
- 22.NHANES – NHANES 2009-2010 – General Release File Documentation. [Accessed January 11, 2013]; URL http://www.cdc.gov/nchs/nhanes/nhanes2009-2010/generaldoc_f.htm.
- 23.Tsimihodimos V, Dounousi E, Siamopoulos KC. Dyslipidemia in chronic kidney disease: an approach to pathogenesis and treatment. Am J Nephrol. 2008;28(6):958–73. doi: 10.1159/000144024. [DOI] [PubMed] [Google Scholar]
- 24.Plantinga LC, Boulware LE, Coresh J, et al. Patient awareness of chronic kidney disease: trends and predictors. Arch Intern Med. 2008;168(20):2268–75. doi: 10.1001/archinte.168.20.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tuot DS, Plantinga LC, Hsu CY, et al. Chronic kidney disease awareness among individuals with clinical markers of kidney dysfunction. Clin J Am Soc Nephrol. 2011;6(8):1838–44. doi: 10.2215/CJN.00730111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Go AS, Mozaffarian D, Roger VL, et al. Heart Disease and Stroke Statistics--2013 Update: A Report From the American Heart Association. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. Heart Disease and Stroke Statistics--2013 Update: A Report From the American Heart Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


