Abstract
The authors examined the effects of mindfulness training on 2 aspects of mode of processing in depressed participants: degree of meta-awareness and specificity of memory. Each of these has been suggested as a maladaptive aspect of a mode of processing linked to persistence and recurrence of symptoms. Twenty-seven depressed participants, all of whom had experienced suicidal crises, described warning signs for their last crisis. These descriptions were blind-rated independently for meta-awareness and specificity. Participants were then randomly allocated to receive mindfulness-based cognitive therapy (MBCT) plus treatment as usual (TAU) or TAU alone, and retested after 3 months. Results showed that, although comparable at baseline, patients randomized to MBCT displayed significant posttreatment differences in meta-awareness and specificity compared with TAU patients. These results suggest that mindfulness training may enable patients to reflect on memories of previous crises in a detailed and decentered way, allowing them to relate to such experiences in a way that is likely to be helpful in preventing future relapses.
Keywords: suicidality, depression, relapse, meta-awareness, memory specificity, mindfulness
Cognition and emotion research in the 1970s and 1980s focused largely on emotional dysregulation arising from biases in information processing, for example, exploring the relationship between depressed mood and interpretive bias toward negative self-referential material (Williams, Watts, MacLeod, & Mathews, 1997). More recently, there has been an increased interest and research focus on the ways in which information is processed (e.g., image vs. verbal processing: Holmes, Brewin, & Hennessy, 2004; analytical vs. experiential processing: Watkins & Teasdale, 2004; or field vs. observer processing: Kuyken & Howell, 2006; for a review, see Watkins, 2008). Our research has been investigating emotional dysregulation that occurs when a person adopts a “discrepancy-based” mode of mind in which (a) negative ideas about the self are taken to represent reality, where (b) a “matching to standard” of the current state of affairs to ideals fuels both the striving for the ideal self and the avoidance of negative outcomes, and in which (c) ruminative or analytic attempts to solve emotional and self-related problems, as well as attempts to suppress or avoid negative thoughts and images, are used, but fail to address perceived discrepancies (Williams, 2008, p. 727). Such a mode of mind is likely to be most evident, and most toxic, when it is used to process extremely negative and personally relevant information. In this article, we consider two distinct aspects of this mode of mind as they relate to the ability of people with recurrent suicidal depression to recollect symptoms of a prior suicidal crisis, and examine how this ability alters with mindfulness training, an intervention that purports to teach people to see clearly which mode of processing they are using and, if they choose, to disengage from this mode and enter a more adaptive state.
Exploration of these issues is motivated by both theoretical and therapeutic interests. First, despite increasing evidence of the positive benefits of mindfulness training, there remains relatively little experimental work to demonstrate that it is actually able to bring about a shift in processing mode, particularly in relation to negative mental content. The current study provided a preliminary opportunity to examine this issue through the use of data from participants in a small randomized controlled trial of mindfulness-based cognitive therapy (MBCT) for chronic-recurrent depression. In this study, patients were asked to describe the symptoms they recollected experiencing in the period leading up to a prior suicidal crisis, such descriptions being elicited both before and after mindfulness treatment. To examine evidence for a shift in mode of processing, we operationalized the discrepancy-based mode in two ways: the extent to which people described their experience of prior symptoms in an overgeneral (as opposed to specific) way, and the extent to which there was evidence of a lack of meta-awareness in the descriptions of these same experiences.
Overgeneral memory has been linked to a discrepancy-based processing mode in a number of prior studies. For example, depressive rumination and overgeneral memory appear to be mutually reinforcing (e.g., Raes, Hermans, Williams, & Eelen, 2006; Watkins & Teasdale, 2001; Williams et al., 2007), and formerly depressed patients show higher levels of overgeneral memory when exposed to self-relevant material (Crane, Barnhofer, Mark, & Williams, 2007; Spinhoven, Bockting, Kremers, Schene, & Williams, 2007). Overgeneral memory is also closely associated with attempts to avoid unpleasant experiences, and may initially develop, in part, as a form of functional avoidance (e.g., Hermans et al., 2004; Raes et al., 2006; Williams, 1996).
Whereas overgeneral memory relates to the form that descriptions of mental content take, meta-awareness concerns a person’s relationship with that content, in particular the extent to which people adopt a cognitive set in which thoughts and emotions are experienced nonconceptually as transient mental events rather than as truths or as definitions of self. Low meta-awareness is characterized by an inability to distinguish the self from the content of negative thoughts and emotions (seeing the self as defined by or as synonymous with negative mental content) and is a central feature of discrepancy-based processing (Segal, Williams, & Teasdale, 2002).
There are also important therapeutic reasons for exploring how MBCT influences the mode with which patients describe signs and symptoms of a prior suicidal crisis. Treatment advances in the fields of schizophrenia (Birchwood & Spencer, 2001) and bipolar disorder (Lam & Wong, 2005) have demonstrated that increasing awareness of idiosyncratic prodromal symptoms (those that regularly occur before full-blown psychotic or manic symptoms are evident) is helpful in reducing relapse risk. It is likely that a similar approach may be beneficial for those experiencing recurrent suicidality in the context of major depression given that it appears that suicidality is easily reactivated once it has occurred during prior episodes (e.g., Williams et al., 2007). However, although identification of relapse warning symptoms (relapse signatures; Birchwood & Spencer, 2001) has the potential to be beneficial, the ability to detect and adaptively respond to signs of relapse is also likely to be challenging, in part because of cognitive deficits discussed above. For example, overgeneral memory is likely to make it more difficult for a person to recall the thoughts, feelings, and behavior associated with a previous suicidal episode, as well as the context within which these symptoms occurred. Previous research has demonstrated that overgeneral memory is associated with impaired interpersonal problem solving (Pollock & Williams, 2001; Sidley, Calam, Wells, Hughes, & Whitaker, 1999), and it is likely that it also makes it harder for a person to recognize and respond adaptively to the problem of their own suicidal crisis.
Similarly, where meta-awareness is low, people’s ability to recognize symptoms of depression as symptoms will be reduced. Only one study to date has explored how the capacity to reflect on symptoms from a decentered perspective relates to risk of depressive relapse (Teasdale et al., 2002). This examined remitted depressed patients’ descriptions of past (mildly distressing) autobiographical events, and found that those patients who displayed higher levels of meta-awareness when describing events were less likely to experience a subsequent relapse. This indicates that adopting a meta-aware stance toward experience may be protective for those with a history of depression. However, it remains unclear whether the stance adopted toward experience can be modified in those at high risk of relapse. Indeed, although increased meta-awareness has been proposed to account for the beneficial effects of MBCT on depressive relapse (Segal et al., 2002), to the best of our knowledge, no studies to date have examined whether or not MBCT actually increases patients’ awareness of the relapse-related signs and symptoms or the meta-aware stance adopted toward these. Similarly, although prior research has indicated that MBCT can increase memory specificity overall (Williams, Teasdale, Segal, & Soulsby, 2000), it is unclear whether these effects extend to patients’ descriptions of their own prior symptoms in a way that might aid relapse prevention.
The current study, therefore, aimed to explore evidence for a shift in mode of processing in patients participating in a pilot randomized controlled trial of MBCT for chronic-recurrent suicidal depression. Two related hypotheses were tested: first, that treatment with MBCT would increase the specificity with which patients were able to describe the symptoms that occurred in the period leading up to a suicidal crisis; and second, that following MBCT, there would be evidence of higher levels of meta-awareness in patients’ descriptions of their relapse signatures.
Method
Participants
In total, 90 individuals from Oxfordshire contacted the research team in response to recruitment through online advertising, press releases, posters, and referrals from Oxfordshire physicians and therapists. Advertisements invited people aged 18–65 years who were currently feeling depressed, had felt depressed several times in the past, and also felt suicidal in the past to contact the research team. Following a prescreen phone interview, 43 individuals dropped out from either ineligibility or loss of interest on hearing further details of the study. The remaining 47 candidates were invited for an assessment interview at the Oxford Department of Psychiatry.
Inclusion criteria were (a) current depression in accordance with Diagnostic and Statistical Manual of Mental Disorders (4th ed.) criteria for depression or a history of chronic depression without full recovery, (b) a history of three or more previous episodes of depression, (c) a history of suicidal ideation or suicidal behavior, (d) written and spoken fluency in English, and (e) age between 18 and 65 years. Exclusion criteria were the presence of mania or hypomania, psychosis, alcohol dependence or substance abuse, obsessive–compulsive disorder, eating disorder, borderline personality disorder, pervasive developmental disorder, or ongoing habitual self-harming behavior. In addition, individuals were excluded if they were currently in psychotherapy or were currently practicing meditation.
The assessment interview found 13 individuals to be ineligible: Three did not meet criteria for depression, 4 engaged in habitual self-harming, 1 had Asperger syndrome, 2 were currently in the manic or hypomanic stages of bipolar disorder, 1 was dependent on alcohol, 1 had an eating disorder, and 1 was unavailable for MBCT class participation. Subsequently, 3 further participants were excluded. In one case, this was due to the participant displaying difficulties in orientation and attention; in another case, we were unable to obtain the required statement that the participant’s general practitioner was unaware of any contraindication; and in the final case, the participant voluntarily withdrew prior to randomization. Finally, 3 participants, 2 from the MBCT group and 1 from the treatment as usual (TAU) group, withdrew postrandomization and prior to completion of posttreatment assessments, and 1 participant only partially completed posttreatment assessments. Complete data were available for 27 participants (TAU: n = 13; MBCT: n = 14).
The study received ethical approval from the Mid and South Buckinghamshire Local Research Ethics Committee (Ref: 07/Q1607/2).
Procedure
Participants provided written consent prior to each assessment and test session. During the initial assessment session, a structured clinical interview was conducted and participants completed the Beck Depression Inventory II (BDI–II). During this session, those candidates meeting eligibility criteria were also interviewed, using the Relapse Signature of Suicidality Interview (ReSSI) described below, about the symptoms they recalled during days, weeks, or months preceding their most recent episode of suicidal ideation or behavior. A second test session was held during which the participants completed several self-report questionnaires as well as a number of cognitive tasks of which only those relevant to the current research questions are reported below.
All participants were to receive MBCT; however, they were randomized into immediate (MBCT) and delayed treatment (TAU) groups. Participants were encouraged to continue their current medication and keep appointments with mental health care practitioners as usual. Those in the TAU group were asked to refrain from starting any meditation practice during their waiting period. Participants in the MBCT group were individually briefed by the therapist who would be conducting the treatment.
The MBCT treatment comprised eight weekly sessions of 2 hr in duration. The content and format followed the manual by Segal et al. (2002), with some minor alterations to address suicidality, that is, introduction of crisis plans and cognitive components addressing suicidal cognitions and hopelessness. The sessions were led by a fully qualified CBT therapist (Thorsten Barnhofer) who had trained in mindfulness-based stress reduction through an internship at the Center for Mindfulness in Medicine, Health Care and Society at the University of Massachusetts, Worcester, Medical Center, and who delivered the treatment under regular supervision of J. Mark G. Williams, one of the developers of the program, who monitored adherence to the treatment protocol. Following the first MBCT course, all participants were invited for another clinical interview and were asked to complete the same set of self-report questionnaires and cognitive tasks as they had done previously. Participants were also interviewed, using the ReSSI, and were specifically asked to recall the same incident of suicidal ideation or behavior as described in the first set of interviews. Interviewers were blind to the treatment status of the participants.
Materials
Structured Clinical Interview for DSM–IV–TR Axis I + SCID Borderline Personality Disorder Module (First, Gibbon, Spitzer, & Williams, 2002)
Current and past psychiatric diagnosis status was determined using the research version of the Structured Clinical Interview for DSM–IV–TR Axis I Disorders along with the Borderline Personality Disorder Module of the SCID for Axis II Disorders. The clinical assessments were used to determine eligibility of participants, and were administered by an experienced postdoctoral research psychologist trained in SCID methodology.
Beck Depression Inventory II (BDI–II; Beck, Steer, & Brown, 1996)
Current symptoms of depression were measured using the BDI–II self-report questionnaire. The BDI–II contains 21 groups of statements that assess the presence and severity of depressive symptoms occurring within the preceding 2 weeks. Each item is ranked on a 3-point scale, for a total score ranging from 0 to 63, with a score ≥20 typically used to indicate at least moderate depression (Beck et al., 1996). The BDI–II is a well-established measure with high internal consistency.
Relapse Signature of Suicidality Interview (ReSSI)
The ReSSI was developed specifically for this study.1 The ReSSI was designed as a semistructured, free-recall interview to investigate individuals’ ability to recall (a) changes in feelings, thoughts, body sensations, and behaviors preceding an episode of deliberate self-harm or a time they had thoughts of suicide or deliberate self-harm; (b) the sequence of the changes; (c) duration of the changes; and (d) whether they had experienced other episodes in the past and a brief assessment of the consistency of content, sequence, and duration of changes across episodes.
Participants were asked to recall the most recent time they felt suicidal or wanted to harm themselves, which was then referred to as their crisis day. Participants were asked to describe the symptoms they experienced prior to their crisis day using the following instructions:
Different feelings, thoughts, and behaviors will often precede a person’s crisis. For example, some people start having restless or unsettled sleep, while others can’t do anything but sleep. Some people have difficulty concentrating, become agitated, feel low, withdraw, stop caring about their appearance, or start feeling very dissatisfied with themselves. The same person may experience all of these changes at once or over time.
Consider your thoughts, feelings, body sensations, and behavior during the days, weeks, or months prior to your crisis day. Can you describe to me what happened? What changes did you notice in the run up to the crisis? If your crisis was triggered by an external event (like “my partner and I had a fight” or “I lost my job”), how did your body and mind react to it?
Relapse signature specificity measure
Transcripts were prepared by removing interviewer comments and by highlighting the symptoms described and confirmed by the participants during the course of the interview. Participants’ symptom descriptions were classified as specific, extended, or categoric according to the criteria shown in Table 1. These classifications match those employed in autobiographical memory research examining overgeneral memory and psychopathology (Williams & Broadbent, 1986; Williams et al., 2007). In this literature, memory retrieval processes are generally viewed as involving a form of hierarchical search, with semantic associations being retrieved at an initial stage, with increasing specification, culminating in the retrieval of a memory incorporating event-specific knowledge and relating to a discrete episode located in time and space. In the context of the relapse signature, it is hypothesized that participants move through a similar search strategy, first making associations to aid the search process (“semantic associates”), then recollecting the types of experiences they notice when feeling low or suicidal (“categoric”), moving on to identify the most recent period in which this occurred (“extended”), and finally recollecting specific details of their experience on this occasions (“specific”). Reflecting this hierarchical search process, specific memories were assigned a score of 4, extended memories a score of 3, categoric memories a score of 2, and associations a score of 1. No semantic associations were identified, resulting in all relapse signature elements being coded as specific (4), extended (3), or categoric (2). The primary researcher rated all of the transcripts, then two independent raters were provided with a representative sample of transcripts. Raters were instructed to consider the symptom descriptions within the context of the comments preceding and following the highlighted phrases to limit any potential bias that might have been introduced by the researcher’s selection of the specific set of words or phrases highlighted for the ratings. For example, the highlighted phrase “I was worried” could be rated as extended unless the raters considered the entire sentence, which read, “Somebody at work said it to me one day, they said I just had this look on my face like I was terribly worried, about something. And I was sort of thinking, I was worried.” In this context, the symptom description is a specific memory because of the fact that it happened on a specific day in a specific place.
Table 1. Definition of the Classification of Autobiographical Memory of Prodromal Symptoms of Suicidal Depression.
Classification Definition/description Example Extended Describes a particular thought, feeling, body sensation, or behavior lasting longer than a day. Similar to a specific memory but of longer duration. “I was starting to not do anything.” Categoric Summarizes a number or category of thoughts, feelings, body sensations, or behaviors. Describes what happens repeatedly or typically. “I often get images of a box of tablets.” Specific Describes a particular thought, feeling, body sensation, or behavior that lasted less than 1 day. “He was planting a bush in the garden, ordinarily I’d be planting it but the whole thing just exhausted me.”
Classification of the memories as specific, categoric, or extended was based on comparison of category determinations by three independent raters of 30% of the sample. The agreement level among the three raters on the classification into memory specificity categories was 89%. The remaining 11% were resolved by a review of transcripts and subsequent consensus among the raters.
Relapse signature meta-awareness measure
Meta-awareness of the “relapse signature” was measured using an adapted version of the Measure of Awareness and Coping in Autobiographical Memory (MACAM; Teasdale et al., 2002). Meta-awareness scores were based on statements made during the participant interview during which the participant described symptoms experienced in the period preceding a suicidal crisis. Raters were extensively trained in rating the meta-awareness of relapse symptoms in accordance with the procedure described above for autobiographical memory ratings but using the meta-awareness categories modeled on those used by Teasdale et al. (2002) and described in Table 2. The numerical values used in the itemized list in Table 2 were used to rate the degree of meta-awareness (e.g., minimal discrimination was numerically scored as 1 and extended discrimination was numerically scored as 5). An average score across all rated statements was calculated corresponding to the mean meta-awareness rating.
Table 2. Definition of the Classification of Meta-Awareness of Prodromal Symptoms of Suicidal Depression.
Rating Definition/description Example 1. Minimal discrimination of different thoughts or feelings Inability to see condition as temporary or use of global descriptions. “I’m not ever going to be able to sleep again.” “I’m a failure.” 2. Discrimination of different thoughts or feelings Apparent immersion in thoughts or feelings with an ability to distinguish separate feelings and thoughts. “I was angry and got really emotional and tearful.” “I was anxious and tense and wound up and fidgety.” 3. Some discrimination of self and reactions to situation The first inkling of insight that shows some level of awareness or the ability to think of the impact on another. “I thought about how suicide would affect my wife.” “I thought, ’I don’t want to do this.’” 4. Discrimination of self from thoughts and feelings Indication that the self is not synonymous with thoughts or feelings. Possibly some evidence of self-compassion. “I get irritable in situations I am normally able to control.” “I felt life was getting difficult, but it was my own inability to cope.” 5. Persistent/extended discrimination of self from thoughts and feelings Thoughts and feelings are described as very distinct from the self and recognized as temporary aspects of the depression. “I kept thinking, ’What’s the point?’ but I knew that it was the depression talking and eventually it would pass.”
The primary researcher rated all of the data and then compared results on 28% of the data with two independent raters. The agreement level among the three raters was 85%. The remaining 15% were resolved by a review of transcripts and subsequent consensus among the raters.
Results
Participant Descriptives
Data were obtained for 27 participants (9 men and 18 women). The mean age of the participants was 41.89 years (SD = 10.47, range = 26–64), and mean level of education was 15.78 years (SD = 3.18, range = 11–22). The MBCT (n = 14) and TAU (n = 13) groups did not differ significantly in gender distribution, age, marital status, employment, and level of education. In addition, the MBCT and TAU groups were comparable in their levels of current depression prior to the treatment phase of the study (see Table 3).
Table 3. Characteristics of the Participants in the MBCT (n = 14) and TAU (n = 13) Groups at Pretreatment.
Status MBCT TAU Statistic p Note. MBCT = mindfulness-based cognitive therapy; TAU = treatment as usual; BDI–II = Beck Depression Inventory II. Gender (male/female), n 4/10 5/8 χ2(26) = 0.30 ns Mean (SD) age (years) 42.07 (11.34) 41.69 (9.90) t(25) = 0.09 ns Living situation (cohabitating/alone), n 7/7 7/6 χ2(26) = 0.04 ns Employment (full time/not full time), n 9/5 7/6 χ2(26) = 0.30 ns Mean (SD) education (years) 16.38 (3.04) 15.15 (3.31) t(24) = 1.14 ns Mean (SD) BDI–II score 30.35 (9.93) 32.37 (11.18) t(25) = −0.50 ns
BDI–II
The main clinical outcomes of this study have been reported elsewhere (Barnhofer et al., in press). However, to aid the interpretation of the analyses of interest in this article, we report the findings relating to BDI–II change below. Change in BDI–II score was analyzed in a 2 × 2 repeated measures analysis of variance (ANOVA) with time (pre, post) as the within-subject factor and group (MBCT, TAU) as the between-subjects factor. This analysis revealed a main effect of time, F(1, 25) = 13.58, p = .001, qualified by a significant Time × Group interaction, F(1, 25) = 7.13, p ≤ .001. Post hoc tests indicated that this interaction resulted from the fact that there was no significant difference in BDI–II scores between the groups at baseline, MI-J = 2.02, SE = 4.06, ns, whereas at follow-up, BDI–II scores were significantly lower in those allocated to MBCT, MI-J = 13.30, SE = 4.81, p = .01. This was the result of a significant decrease in BDI–II score in the MBCT group, MI-J = 13.41, SE = 2.93, p < .001, in the context of no change in those allocated to TAU.
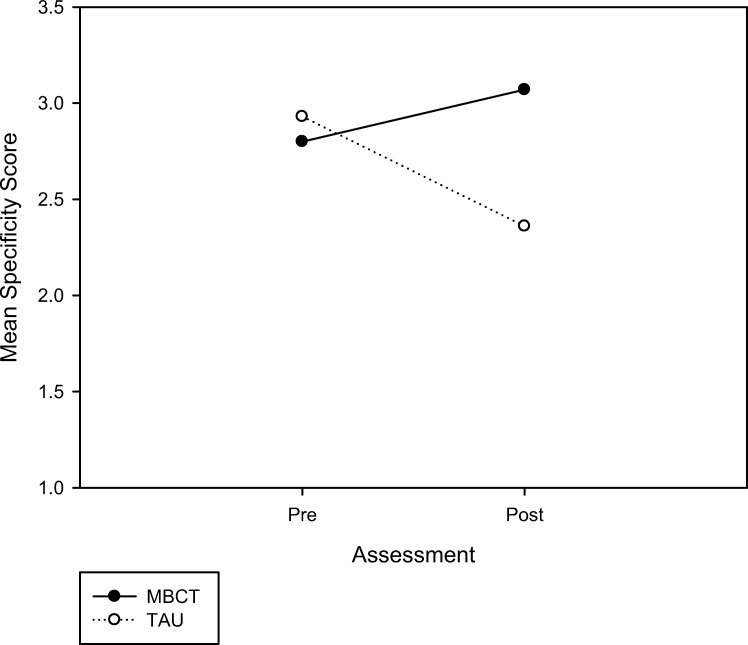
Relapse Signature Specificity Change
Relapse signature specificity scores were analyzed using a 2 × 2 repeated measures ANOVA with time (pre, post) as the within-subject factor and group (MBCT, TAU) as the between-subjects factor. There was a significant Time × Group interaction, F(1, 25) = 6.64, p = .16, η2 = .21, which is shown in Figure 1. Post hoc tests indicated that, whereas there was no significant difference between the MBCT and TAU groups in the specificity of relapse signatures at the baseline assessment (MI-J = 0.13, SE = 0.26, p > .50), recollection of the relapse signature became less specific over time in participants in the TAU group (MI-J = 0.57, SE = 0.23, p = .02), but did not change significantly in the MBCT group, leading to a significant difference between groups at the follow-up assessment, MI-J = −0.70, SE = 0.28, p = .018.
Figure 1.
Pre- and posttreatment changes in mean memory specificity scores between mindfulness-based cognitive therapy (MBCT; n = 14) and treatment as usual (TAU; n = 13) groups.
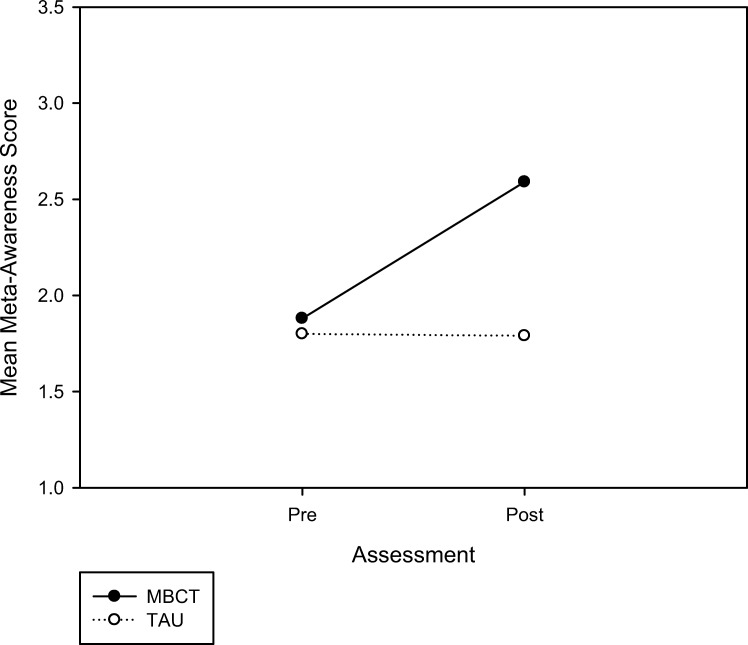
Relapse Signature Meta-Awareness Change
Meta-awareness scores were analyzed using 2 × 2 repeated measures ANOVA with time (pre, post) as the within-subject factor and group (MBCT, TAU) as the between-subjects factor. There was a significant main effect of time, F(1, 25) = 4.74, p = .03, η2 = .16, qualified by a significant Time × Group interaction, F(1, 25) = 4.9, p = .03, η2 = .16, shown in Figure 2. Follow-up post hoc analyses showed that, at the baseline assessment, the two participant groups did not differ significantly from one another on relapse signature meta-awareness, MI-J = −0.08, SE = 0.22, p = .72. However, at follow-up the participants allocated to MBCT reported significantly higher levels of meta-awareness in their relapse signature descriptions, MI-J = −0.81, SE = 0.22, p = .001. This was the result of a significant increase in meta-awareness in the patients allocated to immediate treatment with MBCT, MI-J = −0.72, SE = 0.23, p = .004, and no significant change in those allocated to TAU.
Figure 2.
Pre- and posttreatment changes in mean meta-awareness scores between mindfulness-based cognitive therapy (MBCT; n = 14) and treatment as usual (TAU; n = 13) groups.
Relationship Between BDI–II Scores and Measures of Relapse Signature Specificity and Meta-Awareness
Pearson correlation coefficients were computed between measures of relapse signature specificity and meta-awareness and BDI–II score at the baseline assessment. These indicated a significant negative correlation between BDI–II score and relapse signature specificity at baseline, r(27) = −.39, p = .04. There was no significant association between BDI–II score and relapse signature meta-awareness, r(27) = −.08, ns. Correlations between change scores again indicated a significant correlation between change in BDI–II score and change in relapse signature specificity, r(27) = .39, p = .046, but no significant correlation between change in BDI–II score and change in meta-awareness, r(27) = .19, ns.
To explore how far changes in BDI–II scores could potentially account for treatment effects on relapse signature specificity, we recomputed the 2 (time: pre, post) × 2 (group: MBCT, TAU) repeated measures ANOVA of specificity scores with BDI–II change scores as a covariate. BDI change scores were normally distributed, Kolmogorov–Smirnov test, p > .20. The crucial Time × Group interaction was reduced but remained marginally significant, F(1, 24) = 3.01, p = .09, suggesting that changes in BDI–II score could have had some, albeit minor, effect. The actual effect is likely to be smaller, given that, because of their overlap with treatment group, BDI change scores are likely to also take out part of the variance due to genuine treatment effects (for a discussion of issues surrounding independence of covariates, see Miller & Chapman, 2001). In line with this reasoning, within-group correlations did not show any substantial associations between BDI–II change scores and pretreatment to posttreatment change in specificity (MBCT: r = −.23, p = .43; TAU: r = −.21, p = .47).
Discussion
The way in which people process information about themselves is a critical determinant of their reaction to their own patterns of thinking. The aim of this research was to investigate these processes by examining people’s ability to recognize warning signs of impending suicidal crisis. Our motivation for doing so was that, first, many patients with depression have overgeneral memory, and so find it hard to recollect the specific details of experience, which might otherwise provide clues to the idiosyncratic features of their relapse signature. Second, a low level of meta-awareness is potentially dangerous because it results in an inability to distinguish the self from the content of negative thoughts and emotions (e.g., to decenter from mental content) so that people’s ability to recognize symptoms of depression as symptoms is reduced.
The present study found that MBCT, a treatment explicitly designed to increase attention to the details of experience and to foster a meta-aware stance toward these, improved patients’ ability to delineate the prodromal signs and symptoms related to a past suicidal crisis. The pattern of results differed for the two measures. Specifically, individuals receiving immediate MBCT described relapse signatures of equivalent specificity at the baseline and follow-up assessments, whereas those allocated to delayed treatment reported more overgeneral relapse signatures at follow-up. Therefore, although MBCT did not lead to increased specificity of symptom descriptions, it did appear to aid retention of the details of relapse signatures, whereas those who did not undergo treatment were more likely to forget the details. One possibility is that MBCT allowed people to reflect on details of their prior suicidal crises, promoting greater maintenance of episodic details of the memory. By contrast, those not receiving treatment may have continued attempts to suppress memories of past suicidal crises, resulting in poorer retrieval for the details of experience over time.
For the meta-awareness measure, the results were exactly as predicted, with those receiving TAU showing no change and those receiving MBCT showing increased meta-awareness (ability to decenter). This is important because low meta-awareness has been reported to be associated with subsequent recurrence in major depression (Teasdale et al., 2002), but to date, no studies have explored whether it is possible to increase the capacity to decenter from self-related symptoms in patients with major depression. The fact that these effects were unrelated to, or, in the case of relapse signature specificity, only marginally affected by change in depressive symptoms suggests that they are not simply an epiphenomenon of symptomatic improvements but a more particular result of the mindfulness-based training. Again, this is in line with previous research that has found that a considerable number of patients who have recovered from the most severe phase of their episode without having received cognitive therapy or mindfulness treatment continue to show deficits in memory specificity (Brittlebank, Scott, Williams, & Ferrier, 1993; Peeters, Wessel, Merckelbach, & Boon-Vermeeren, 2003) or low meta-awareness (Teasdale et al., 2002), both of which have been found to predict either persistence of residual symptoms or subsequent recurrence.
Remembering suicidal crises and the prodromal states preceding them is important. Patients need to access these experiences to learn from them so that, in the future, they can recognize them clearly at an early stage and initiate skillful actions to prevent relapse. However, they can be highly emotional and aversive, and the suicidal thinking and hopelessness characteristic of these states have been found to be easy to trigger and reinstantiate, particularly in those with a history of repeated episodes (Williams, Van der Does, Barnhofer, Crane, & Segal, 2008). Because of their aversiveness, patients often react to such memories either (a) by trying to suppress or avoid them—a reaction that is likely to produce paradoxical effects—or (b) by ruminating about them in ways that make mood worse, resulting in further attempts to avoid (Wenzlaff & Luxton, 2003). These reactions constitute a particular challenge in dealing with memories of past suicidal ideation and behavior. Patients need to relate openly to the experience of such memories while at the same time being able to abstain from engagement in habitual maladaptive patterns of reacting to them.
Recent experimental research has shown that such distanced engagement is an adaptive way of dealing with negative experiences that can help reconstrual and buffer individuals against future depressed affect (Kross & Ayduk, 2008). The findings of the current study provide preliminary evidence that MBCT can foster the skills that are centrally involved in both aspects of this form of relating to negative experience. Positive effects on the specificity with which suicidal patients are able to describe past crises and prodromal states suggest that the training helped them continue to recall such experiences in detail. Increases in meta-awareness are indicative of an ability to see these experiences as mental events and to relate to them in a more decentered way.
Interpretation of our findings has to take into account several limitations. First, the study is based on a small sample and, therefore, is vulnerable to spurious effects. Although exploratory analyses showed that our results were not due to outliers, replication among a larger, more statistically powerful, sample would definitely be desirable. That said, however, statistical significance within a small sample is promising. Second, the dependent measures of the study were derived from a semistructured interview that was specifically developed for the current study. Although such an approach avoids common problems associated with self-report through questionnaires and dependent measures were based on well-established tests, there is currently only limited information available with regard to the reliability and validity of this procedure. Third, it is possible that the coding procedure used to assess level of meta-awareness in participant’s symptom descriptions may tap other aspects of cognition in addition to pure meta-awareness (e.g., cognitive reappraisal). The procedure for assessing level of meta-awareness was based very closely on a measure used in a prior study (MACAM; Teasdale et al., 2002) and, although concurrent or discriminant validity checks were absent from this study, previous research has demonstrated that meta-awareness scores derived from the coding scheme used by Teasdale et al. (2002) were able to reliably distinguish depressed patients from healthy controls and predict subsequent depressive symptoms while being generally unrelated to depression severity within a depressed sample. Thus, although there is certainly a need for further investigation and more thorough assessments of concurrent and discriminant validity of the relapse signature meta-awareness measure, we would argue that its use of blind ratings of participants’ spontaneous descriptions of their experiences is closer to the processes of interest than existing self-report questionnaires and is, therefore, of value.
Fourth, this study examined the immediate effects, rather than long-term effects, of MBCT. Our findings are therefore preliminary in the sense that we do not know whether the effects observed are of a lasting nature. This would have been of particular interest given that the patients in the current study all suffered from a chronic or highly recurrent course of depression. However, at the current state of knowledge, and given that the application of MBCT in currently depressed patients is only at an exploratory stage, we reasoned that a first necessary step was to investigate immediate effects and the viability of getting reliable measures.
Fifth, although we assume that the effects reported are a consequence of training in mindfulness meditation, this study alone does not let us know which aspect of MBCT made the difference and what mediated the observed effects. In particular, our data cannot conclusively answer the question of whether the observed changes in memory specificity and meta-awareness occurred simply as consequence of changes in mood or whether any changes in mood were preceded by changes in cognitive functioning that occurred as a direct consequence of the meditation training. Ideally, such analyses would be based on repeated assessment of the variables in questions in order to allow analyses of the temporal order in changes (Murphy, Cooper, Hollon, & Fairburn, 2009), which were not included in our design. However, when analyses controlled for change in BDI scores, differences in pretreatment to posttreatment changes in meta-awareness remained significant, and differences in pretreatment to posttreatment changes in memory specificity were reduced to trend levels, suggesting that there were no or only small effects of changes in depressive symptoms on meta-awareness and memory specificity. This is in line with previous research that has shown that, although predictive of the future course of the disorder, both memory specificity and meta-awareness vary relatively independently of current symptoms and mood (Teasdale et al., 2002; Williams et al., 2007). Although this is generally consistent with a direct effect of the treatment on the variables of interest, more research is needed to clearly demonstrate mediation. Similar questions remain with regard to the active ingredient of the treatment. MBCT encompasses a number of nonspecific and specific therapeutic factors, including a number of different forms of meditation, and further research will have to investigate in more detail in how far the current effects are due to this component and how far individual meditation techniques may differ in their effects.
Despite the above limitations, if the results can be replicated, they will have important clinical implications. Memories of suicidal crises can easily trigger the very mode of processing that was involved in the escalation of negative mood into crisis. Previously suicidal patients are, therefore, faced with the challenge of having to use and learn from a highly aversive past experience without entering the related maladaptive mode of processing. The current study provides preliminary evidence that MBCT can be particularly useful in this situation in that it helps patients adopt a style of processing in which they remain able to experience memories in a specific and detailed way while retaining a decentered (meta-aware) perspective that keeps them from being drawn into automatic maladaptive patterns of processing. Further longitudinal research will have to investigate how far such changes can protect suicidal patients from future occurrences of suicidal crises.
Footnotes
The ReSSI is available from J. Mark G. Williams on request.
References
- Barnhofer T., Crane C., Hargus E., Amarasinghe M., Winder R., & Williams J. M. G. (2009). Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study. Behaviour Research and Therapy, 47, 366–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A. T., Steer R. A., & Brown G. K. (1996). Beck Depression Inventory manual (2nd ed.). San Antonio, TX: The Psychological Corporation [Google Scholar]
- Birchwood M., & Spencer E. (2001). Early intervention in psychotic relapse. Clinical Psychology Review, 21, 1211–1226 [DOI] [PubMed] [Google Scholar]
- Brittlebank A. D., Scott J., Williams J. M. G., & Ferrier I. M. (1993). Autobiographical memory in depression: State or trait marker? British Journal of Psychiatry, 162, 118–121 [DOI] [PubMed] [Google Scholar]
- Crane C., Barnhofer T., Mark J., & Williams J. M. G. (2007). Cue self-relevance affects autobiographical memory specificity in individuals with a history of major depression. Memory, 15, 312–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane C., Barnhofer T., Visser C., Nightingale H., & Williams J. M. G. (2007). The effects of analytical and experiential rumination on autobiographical memory specificity in individuals with a history of major depression. Behaviour Research and Therapy, 45, 3077–3087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M. B., Gibbon M., Spitzer R. L., & Williams J. B. W. (2002). User’s guide for the Structured Clinical Interview for DSM–IV–TR Axis I Disorders—Research Version (SCID-I for DSM–IV–TR, November 2002 Revision). Washington, DC: American Psychiatric Press [Google Scholar]
- Hermans D., Van den Broeck K., Belis G., Raes F., Pieters G., & Eelen P. (2004). Trauma and autobiographical memory specificity in depressed inpatients. Behaviour Research and Therapy, 42, 775–789 [DOI] [PubMed] [Google Scholar]
- Holmes E. A., Brewin C. R., & Hennessy R. G. (2004). Trauma films, information processing, and intrusive memory development. Journal of Experimental Psychology, 133, 3–22 [DOI] [PubMed] [Google Scholar]
- Kross E., & Ayduk O. (2008). Facilitating adaptive emotional analysis: Distinguishing distanced-analysis of depressive experiences from immersed-analysis and distraction. Personality and Social Psychology Bulletin, 34, 924–938 [DOI] [PubMed] [Google Scholar]
- Kuyken W., & Howell R. (2006). Facets of autobiographical memory in adolescents with major depressive disorder and never-depressed controls. Cognition & Emotion, 20, 466–487 [DOI] [PubMed] [Google Scholar]
- Lam D., & Wong G. (2005). Prodromes, coping strategies and psychological interventions in bipolar disorders. Clinical Psychology Review, 25, 1028–1042 [DOI] [PubMed] [Google Scholar]
- Miller G. A., & Chapman J. P. (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110, 40–48 [DOI] [PubMed] [Google Scholar]
- Murphy R., Cooper Z., Hollon S. D., & Fairburn C. G. (2009). How do psychological treatments work? Investigating mediators of change. Behaviour Research and Therapy, 47, 1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters F., Wessel I., Merckelbach H., & Boon-Vermeeren M. (2003). Autobiographical memory specificity and the course of major depressive disorder. Comprehensive Psychiatry, 43, 344–350 [DOI] [PubMed] [Google Scholar]
- Pollock L. R., & Williams J. M. G. (2001). Effective problem solving in suicide attempters depends on specific autobiographical recall. Suicide and Life-Threatening Behavior, 31, 386–396 [DOI] [PubMed] [Google Scholar]
- Raes F., Hermans D., de Decker A., Williams J. M. G., & Eelen P. (2003). Autobiographical memory specificity and affect regulation: An experimental approach. Emotion, 3, 201–206 [DOI] [PubMed] [Google Scholar]
- Segal Z. V., Williams J. M. G., & Teasdale J. D. (2002). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford Press [Google Scholar]
- Sidley G. L., Calam R., Wells A., Hughes T., & Whitaker K. (1999). The prediction of parasuicide repetition in a high-risk group. British Journal of Clinical Psychology, 38, 375–386 [DOI] [PubMed] [Google Scholar]
- Spinhoven P., Bockting C. L. H., Kremers I. P., Schene A. H., & Williams J. M. G. (2007). The endorsement of dysfunctional attitudes is associated with an impaired retrieval of specific autobiographical memories in response to matching cues. Memory, 15, 324–338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale J. D., Moore R. G., Hayhurst H., Pope M., Williams S., & Segal Z. V. (2002). Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology, 70, 275–287 [DOI] [PubMed] [Google Scholar]
- Watkins E. R. (2008). Constructive and unconstructive repetitive thought. Psychological Bulletin, 134, 163–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins E., & Teasdale J. D. (2001). Rumination and overgeneral memory in depression: Effects of self-focus and analytic thinking. Journal of Abnormal Psychology, 110, 353–357 [DOI] [PubMed] [Google Scholar]
- Watkins E., & Teasdale J. D. (2004). Adaptive and maladaptive self-focus in depression. Journal of Affective Disorders, 82, 1–8 [DOI] [PubMed] [Google Scholar]
- Wenzlaff R. M., & Luxton D. D. (2003). The role of thought suppression in depressive rumination. Cognitive Therapy and Research, 27, 293–308 [Google Scholar]
- Williams J. M. G. (1996). Depression and the specificity of autobiographical memory In Rubin D. C. (Ed.), Remembering our past: Studies in autobiographical memory (pp. 244–267). New York: Cambridge University Press [Google Scholar]
- Williams J. M. G. (2008). Mindfulness, depression and modes of mind. Cognitive Therapy and Research, 721–733
- Williams J. M. G., Barnhofer T., Crane C., Hermans D., Raes F., Watkins E., et al. (2007). Autobiographical memory specificity and emotional disorder. Psychological Bulletin, 133, 122–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J. M. G., & Broadbent K. (1986). Autobiographical memory in suicide attempters. Journal of Abnormal Psychology, 95, 144–149 [DOI] [PubMed] [Google Scholar]
- Williams J. M. G., Teasdale J. D., Segal Z. V., & Soulsby J. (2000). Mindfulness-based cognitive therapy reduces overgeneral memory in formerly depressed patients. Journal of Abnormal Psychology, 109, 150–155 [DOI] [PubMed] [Google Scholar]
- Williams J. M. G., Van der Does A. J. W., Barnhofer T., Crane C., & Segal Z. S. (2008). Cognitive reactivity, suicidal ideation and future fluency: Preliminary investigation of a differential activation theory of hopelessness/suicidality. Cognitive Therapy and Research, 32, 83–104 [Google Scholar]
- Williams J. M. G., Watts F. N., MacLeod C., & Mathews A. (1997). Cognitive psychology and emotional disorders. Chichester, UK: Wiley [Google Scholar]