Abstract
Objective
At the present time, there is a trend towards performing open heart surgery at a younger age. Myocardium of infants has been thought to be more vulnerable to cardiopulmonary bypass in comparison with adults. For this study, we evaluated the degree of myocardial injury by measurement of cardiac troponin levels in infants in comparison with older children for similar surgeries.
Methods
Serum was collected before bypass, after bypass, and daily after surgery and serum cardiac troponin I level (micrograms per litre). The demographic data, cardiac diagnoses, types of surgery performed, and peri-operative parameters were collected.
Results
Of the 21 children enrolled consecutively, five were infants. Among the 21 patients, four patients had post-operative peak troponin values greater than 100 (three were infants) and all four patients survived and had normal left ventricular systolic function upon discharge echocardiogram. The five infants had peak troponin levels of 222.3, 202, 129, 26.7, and 82.3. The post-operative peak troponin levels were significantly higher in infants (mean 132.5 with a standard deviation of 81.6) than in the older children (mean 40.3 with a standard deviation of 33.4), although there was no significant difference in bypass time, bypass temperature, cross-clamp time, or the length of stay in the intensive care unit between the two age groups.
Conclusions
Higher troponin release is seen in infants in comparison with older children after bypass for similar surgeries. A troponin level greater than 100 after bypass does not necessarily predict death or a severe cardiovascular event in the very young.
Keywords: Open heart surgery, congenital cardiac malformations, myocardial ischaemia, paediatric, congenital heart surgery, cyanosis
Open heart surgery on cardiopulmonary bypass is associated with cardiac injury and release of cardiac troponins I and T. Cardiac troponin I is a specific and sensitive marker for myocardial injury.1,2 Measurement of serum cardiac troponin I is preferable over cardiac troponin T because it has the advantage of being uninfluenced by renal failure.3 The post-operative cardiac troponin levels are being increasingly used to predict post-operative events and complications in children.4-7
At the present time, there is a trend towards performing open heart surgery at a younger age. However, it is thought that children undergoing surgical repair for congenital heart disease during the first few months of life exhibit more complications when compared with older children for a similar type of surgery. Myocardium of infants has also been thought to be more vulnerable to cardiopulmonary bypass in comparison with older children and adults.8,9 For this study, we evaluated the degree of myocardial injury by measurement of cardiac troponin I in infants in comparison with older children for the same lesions and during similar types of surgeries.
Materials and methods
Study design
The study was prospective and observational, involving children who underwent open heart surgeries at the New York Presbyterian Hospital. The protocol was approved by the Institutional Review Board. Informed written consent was required for enrolling.
Patients
Consecutive patients requiring elective open heart surgery under cardiopulmonary bypass for various congenital heart diseases were enrolled after obtaining written consent. The inclusion criteria included body weight 5 kilograms or greater – because of daily blood collection for the study. The exclusion criteria were any emergent surgery and presence of other systemic disease, such as diabetes or systemic lupus erythematosus or recent infections. The children were divided into two groups based on their age at surgery: either above or below 1 year. The following data were collected: demographic data, cardiac diagnoses, types of surgery performed, cardiopulmonary bypass time, cross-clamp time, post-operative parameters including blood pressure, and occurrence of cardiac arrest or death.
Surgery
The study patients underwent open heart surgery to correct their underlying congenital heart disease via sternotomy under cardiopulmonary bypass. The cardiopulmonary unit included the membrane oxygenator (Terumo, New Jersey, United States of America), roller pump (Cobe, Arvada, Colorado, United States of America), non-heparin-coated polyvinyl chloride circuit tubing (Cobe), with an arterial filter (Cobe) and hemoconcentrator (Minntech HP 400, Minnesota, United States of America). The cardiopulmonary unit was primed with an electrolyte solution with albumin, mannitol, and heparin, as well as with donor blood as needed. The flow rate was maintained at 2.2 litres per minute per square metre and the haematocrit was maintained at or greater than 25%. Myocardial protection was achieved with 15 millilitres per kilogram at 4°C of cardioplegia solution containing 5% dextrose water 500 cubic centimetres with 15 milli-equivalents of sodium bicarbonate, 25 millilitres of 25% mannitol, and 15 milliequivalents of potassium chloride. Hypothermia (19.9–35.7°C) was maintained in every patient. The post-operative days were defined as follows: post-operative day 0 was the day of surgery, post-operative day 1 was 1 day after the surgery, and so forth.
Blood sampling and measurement of cardiac troponin I
Blood samples were collected using sterile technique from each patient before cardiopulmonary bypass, within 2 hours after chest closure, and early morning of each subsequent day hospitalised in the intensive care unit. The blood was centrifuged for 20 minutes and the serum separated and frozen at −70°C. Serum levels of cardiac troponin I were measured in a single batch by microparticle enzyme immunoassay with Abbott AxSYM system (Abbott laboratories, Abbott Park, Illinois, United States of America). Based on the 95 percentile, the expected values for apparently healthy individuals by this assay are serum levels of less than or equivalent to 0.4 micrograms per litre. At the cut-off value of 2.0 micrograms per litre, cardiac troponin I level is 94% sensitive and 93% specific for the diagnosis of myocardial infarction within the first 24 hours of presentation (package insert Abott AxSYM 69-3119/R3).
Statistical analysis
The Spearman rank correlations were calculated to demonstrate associations between numeric variables between subjects. The Mann–Whitney test was carried out to compare all continuous variables. The Fisher Exact test was carried out to determine the association between categorical variables. A p-value less than 0.05 was considered significant.
Results
The study cohort included 21 consecutive patients requiring elective open heart surgery under cardiopulmonary bypass for various congenital heart diseases (see Table 1). All infants had cardiac surgery for acyanotic lesions. All patients enrolled completed the study; none had post-operative renal failure or a severe cardiac event requiring resuscitation, and there were no deaths. All had normal ventricular systolic function before surgery and upon discharge per echocardiogram. All patients had significant increases in the cardiac troponin I level post-operatively within 24 hours, which were almost within the normal limits by the 1st week after surgery.
Table 1.
Clinical and laboratory data.
| Age >1, n = 16 | Age ≤ 1, n = 5 | p-value | |
|---|---|---|---|
| Age (years) | 6.9 (5.6) | 0.67 (0.23) | <0.05 |
| Males (%) | 56 | 40 | ns |
| CPB temperature (°C) | 30.3 (3.9) | 29.8 (3.8) | ns |
| CPB time (min) | 104 (62) | 99 (74) | ns |
| Cross-clamp time (min) | 51 (44) | 61 (54) | ns |
| Aspartate aminotransferase (units/l) | 174 (469) | 96 (47) | <0.05 |
| Lactate dehydrogenase (units/l) | 268 (70) | 331(147) | ns |
| Creatine kinase (units/l) | 427 (237) | 991 (640) | ns |
| Peak cardiac troponin I (μg/l) | 40.3 (33.4) | 132.5 (81.6) | <0.05 |
| Days intubated | 1.0 (0.4) | 1.4 (0.9) | ns |
| Days in ICU | 6.2 (4) | 7.8 (4.6) | ns |
| Days of inotropic support | 0.9 (1) | 2 (2.4) | ns |
| Surgeries (n) | Fontan (4) | ASD (2) | |
| Glenn (1) | AV canal (2) | ||
| ASD (2) | VSD (1) | ||
| AV canal (1) | |||
| VSD (3) | |||
| TOF (3) | |||
| SMSR (1) | |||
| TVR (1) |
ASD = atrial septal defect; AV canal = atrioventricular canal; CPB = cardiopulmonary bypass; ICU = intensive care unit; peak level (highest level of troponins on the multiple measurements after surgery) is the highest value; ns = not significant; SMSR = supra mitral stenosing ring; TOF = tetralogy of Fallot; TVR = tricuspid valve repair; VSD = ventricular septal defect All values are in mean (standard deviation) unless specified. p-values are between the two age groups compared
There was no significant difference in the baseline pre-operative cardiac troponin I levels between the children with cyanotic congenital heart disease (seven patients, mean 0.13 with a standard deviation of 0.16 micrograms per litre) and those with acyanotic congenital heart disease (14 patients, mean 0.2 with a standard deviation of 0.21 micrograms per litre). The enrolled children in the two age groups underwent elective surgeries that were of similar Risk Adjustment in Congenital Heart Surgery-1 risk category (category 1 to 3).10 None of the infants underwent a surgery requiring ventriculotomy or surgery for a cyanotic heart defect. The older children underwent surgeries for similar acyanotic heart defects to infants, but also had surgeries that included a ventriculotomy and surgeries for cyanotic heart defects such as tetralogy of Fallot and cavopulmonary shunts for single ventricles. Among the 21 patients, four patients, including three infants, had peak cardiac troponin I values greater than 100 micrograms per litre. The five infants had peak cardiac troponin I (micrograms per litre) levels of 222.3, 202, 129, 82.3, and 26.7 after surgeries for acyanotic heart defects. The post-operative peak cardiac troponin I levels in infants were significantly higher than those in the older children (see Table 1), and the peak cardiac troponin I correlated with age (see Fig 1).
Figure 1.
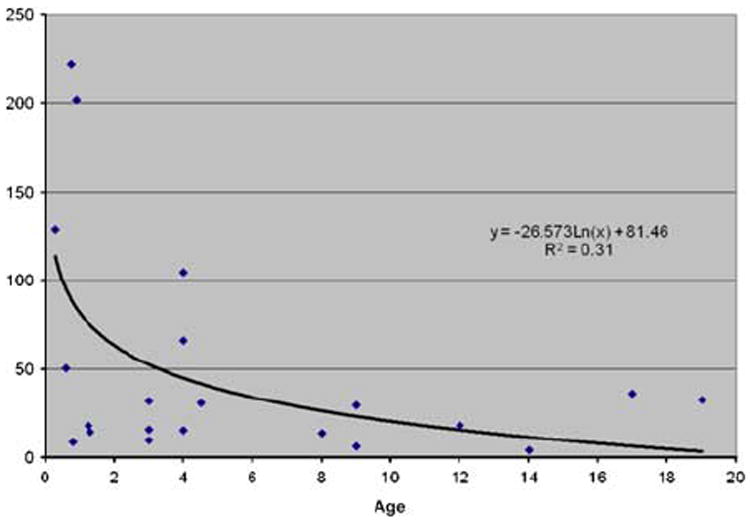
Peak post-operative serum levels of cardiac troponin I in micrograms per litre (y-axis) by age in years.
Discussion
We found that cardiac troponin I level before surgery was similar in cyanotic children compared with the acyanotic children, similar to previous reports6 indicating that cyanosis alone may not contribute to cardiac troponin I release. In our study, the cardiac troponin I release after a variety of paediatric cardiopulmonary bypass procedures was seen to peak within the first 24 hours of the event and decline over the next several days, similar to previous reports.6,11
Recently, the trend has been towards early repair in infancy of many of the congenital heart diseases including the most complicated repairs.12 Investigations have shown that children had five times higher cardiac troponin T release compared with the adults8 and that the younger age correlates significantly with higher amount of cardiac troponin I release.6,13 We demonstrated similar results, and our findings in this study are strengthened by the various parameters compared between the two age groups for similar types of surgeries. All infants had similar surgeries to the older children (age greater than 1 year). However, the children in the older group also had surgeries for more complex cardiac lesions including surgery on cyanotic heart defects and surgeries with ventriculotomy that should have caused a higher release of cardiac troponin I. Despite this, we found that in infants the post-operative peak cardiac troponin I was significantly higher than the older children, although there was no significant difference in cardiopulmonary bypass time, cardiopulmonary bypass temperature, cross-clamp time, or the number of days in the intensive care unit between the two age groups.
Troponin levels have been used as a predicator of post-operative death after cardiopulmonary bypass.14,15 Cardiac troponin T has been found to correlate with the severity score of cardiac surgery in children.16 In adults, the thresholds of cardiac troponin I predicting severe cardiac event and/or death have been found to be 11.8 nanograms per litre (11.5–14.8 nanograms per litre) and an elevated cardiac troponin I above the threshold was significantly associated with a severe cardiac event and/or death (odds ratio, 4.33).15 In a retrospective study of children, a level of cardiac troponin T greater than 5.9 micrograms per litre on the first post-operative day was found to predict death (odds ratio, 10.7).17 In children, a very high post-operative cardiac troponin I release (especially at or greater than 100 micrograms per litre) has been found to be associated with mortality after cardiopulmonary bypass.4,5,13,18-20 In a study of 54 children who underwent cardiopulmonary bypass, only two children died, both with levels of cardiac troponin I greater than 100 micrograms per litre5. However, in our prospective study, four patients, including three were infants, had a post-operative cardiac troponin I level greater than 100 micrograms per litre, and none had a severe cardiac event or death and demonstrated a normal ventricular systolic function before discharge. Hence, in children, a threshold level of cardiac troponin I in predicting severe cardiac event and/or death remains to be determined and the threshold may differ in the younger and the older children. Further, it appears that infant myocardium, although more vulnerable than an adult myocardium8 with a higher release of cardiac troponin I, may also be more resilient with a recovery to normal contractility despite the excessive injury. The limitation of our study includes the small sample size of the patient population.
In conclusion, a higher cardiac troponin I is seen in infants in comparison with older children after cardiopulmonary bypass for similar surgeries. Very high cardiac troponin I levels greater than 100 micrograms per litre after surgery does not necessarily predict death or a severe cardiovascular event after cardiopulmonary bypass in the very young.
Acknowledgments
Funding resources: The project described was partially supported by Grant number 5K23HL089301-03 (PI Monesha Gupta, MD) from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
References
- 1.Bhavsar PK, Dhoot GK, Cumming DV, Butler-Browne GS, Yacoub MH, Barton PJ. Developmental expression of troponin I isoforms in fetal human heart. FEBS Lett. 1991;292:5–8. doi: 10.1016/0014-5793(91)80820-s. [DOI] [PubMed] [Google Scholar]
- 2.Bodor GS, Porterfield D, Voss EM, Smith S, Apple FS. Cardiac troponin-I is not expressed in fetal and healthy or diseased adult human skeletal muscle tissue. Clin Chem. 1995;41:1710–1715. [PubMed] [Google Scholar]
- 3.Immer FF, Stocker FP, Seiler AM, Pfammatter JP, Printzen G, Carrel TP. Comparison of troponin-I and troponin-T after pediatric cardiovascular operation. Ann Thorac Surg. 1998;66:2073–2077. doi: 10.1016/s0003-4975(98)00795-4. [DOI] [PubMed] [Google Scholar]
- 4.Bottio T, Vida V, Padalino M, Gerosa G, Stellin G. Early and long-term prognostic value of troponin-I after cardiac surgery in newborns and children. Eur J Cardiothorac Surg. 2006;30:250–255. doi: 10.1016/j.ejcts.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Immer FF, Stocker F, Seiler AM, et al. Troponin-I for prediction of early postoperative course after pediatric cardiac surgery. J Am Coll Cardiol. 1999;33:1719–1723. doi: 10.1016/s0735-1097(99)00061-3. [DOI] [PubMed] [Google Scholar]
- 6.Modi P, Imura H, Angelini GD, et al. Pathology-related troponin I release and clinical outcome after pediatric open heart surgery. J Card Surg. 2003;18:295–300. doi: 10.1046/j.1540-8191.2003.02031.x. [DOI] [PubMed] [Google Scholar]
- 7.Hammer S, Loeff M, Reichenspurner H, et al. Effect of cardiopulmonary bypass on myocardial function, damage and inflammation after cardiac surgery in newborns and children. Thorac Cardiovasc Surg. 2001;49:349–354. doi: 10.1055/s-2001-19011. [DOI] [PubMed] [Google Scholar]
- 8.Taggart DP, Hadjinikolas L, Wong K, et al. Vulnerability of paediatric myocardium to cardiac surgery. Heart. 1996;76:214–217. doi: 10.1136/hrt.76.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Imura H, Caputo M, Parry A, Pawade A, Angelini GD, Suleiman MS. Age-dependent and hypoxia-related differences in myocardial protection during pediatric open heart surgery. Circulation. 2001;103:1551–1556. doi: 10.1161/01.cir.103.11.1551. [DOI] [PubMed] [Google Scholar]
- 10.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123:110–118. doi: 10.1067/mtc.2002.119064. [DOI] [PubMed] [Google Scholar]
- 11.Saraiya NR, Sun LS, Jonassen AE, Pesce MA, Queagebeur JM. Serum cardiac troponin-I elevation in neonatal cardiac surgery is lesion-dependent. J Cardiothorac Vasc Anesth. 2005;19:620–625. doi: 10.1053/j.jvca.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Drinkwater DC, Laks H. Pediatric cardioplegic techniques. Semin Thorac Cardiovasc Surg. 1993;5:168–175. [PubMed] [Google Scholar]
- 13.Taggart DP, Hadjinikolas L, Hooper J, et al. Effects of age and ischemic times on biochemical evidence of myocardial injury after pediatric cardiac operations. J Thorac Cardiovasc Surg. 1997;113:728–735. doi: 10.1016/S0022-5223(97)70231-9. [DOI] [PubMed] [Google Scholar]
- 14.Lasocki S, Provenchere S, Benessiano J, et al. Cardiac troponin I is an independent predictor of in-hospital death after adult cardiac surgery. Anesthesiology. 2002;97:405–411. doi: 10.1097/00000542-200208000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Fellahi JL, Hedoire F, Le Manach Y, Monier E, Guillou L, Riou B. Determination of the threshold of cardiac troponin I associated with an adverse postoperative outcome after cardiac surgery: a comparative study between coronary artery bypass graft, valve surgery, and combined cardiac surgery. Crit Care. 2007;11:R106. doi: 10.1186/cc6126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lipshultz SE, Rifai N, Sallan SE, et al. Predictive value of cardiac troponin T in pediatric patients at risk for myocardial injury. Circulation. 1997;96:2641–2648. doi: 10.1161/01.cir.96.8.2641. [DOI] [PubMed] [Google Scholar]
- 17.Mildh LH, Pettila V, Sairanen HI, Rautiainen PH. Cardiac troponin T levels for risk stratification in pediatric open heart surgery. Ann Thorac Surg. 2006;82:1643–1648. doi: 10.1016/j.athoracsur.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Montgomery VL, Sullivan JE, Buchino JJ. Prognostic value of pre- and postoperative cardiac troponin I measurement in children having cardiac surgery. Pediatr Dev Pathol. 2000;3:53–60. doi: 10.1007/s100240050007. [DOI] [PubMed] [Google Scholar]
- 19.Kirklin JK, Blackstone EH, Kirklin JW, McKay R, Pacifico AD, Bargeron LM., Jr Intracardiac surgery in infants under age 3 months: incremental risk factors for hospital mortality. Am J Cardiol. 1981;48:500–506. doi: 10.1016/0002-9149(81)90079-5. [DOI] [PubMed] [Google Scholar]
- 20.Carmona F, Manso PH, Vicente WV, Castro M, Carlotti AP. Risk stratification in neonates and infants submitted to cardiac surgery with cardiopulmonary bypass: a multimarker approach combining inflammatory mediators, N-terminal pro-B-type natriuretic peptide and troponin I. Cytokine. 2008;42:317–324. doi: 10.1016/j.cyto.2008.03.005. [DOI] [PubMed] [Google Scholar]


