Abstract
Findings have been inconsistent regarding the association of obesity and sexual risk behaviors. The purpose of the current study was to assess the prospective nature of body mass index (BMI), depression, and their interaction in predicting condom use during anal intercourse among HIV-infected men who have sex with men (MSM). The sample (N = 490) was obtained from a large, HIV clinical cohort from four sites across the U.S. The following inclusion criteria were employed: identification as MSM and had completed at least one wave of patient-reported measures (e.g., depression, as measured by the PHQ-9) in the clinical cohort study. Longitudinal linear mixed-effects modeling revealed a significant BMI by depression interaction. Depressive symptoms were predictive of less frequent condom use for obese but not overweight men. Analogous results were found in regard to comparisons between normal weight and overweight men. Obesity, in the context of depression, is a risk factor for unprotected anal intercourse among HIV-infected MSM. Cognitive behavioral interventions to reduce HIV transmission risk behaviors among HIV-infected MSM should adopt an integrated perspective, combining sexual risk reduction with treatment for depression and body-related concerns.
Keywords: HIV/AIDS, Depression, Obesity, Sexual Risk, Body Mass Index, Condom Use
INTRODUCTION
Rates of obesity are high in the United States, with an estimated prevalence rate of 36% in 2009–2010 (Flegal, Carroll, Kit, & Ogden, 2012). Similarly, rates of obesity are on the rise among HIV-infected individuals, with 62% diagnosed during the anti-retroviral therapy (ART) era classified as overweight or obese (Crum-Cianflone et al., 2010; Tate et al., 2012). Further, recent estimates of overweight and obesity among men who have sex with men (MSM) are roughly 53% (Guadamuz et al., 2012). Obesity has been associated with numerous deleterious health outcomes, including depression, diabetes, and cardiovascular disease (Bray, 2004; Marti, Macros, & Martinez, 2001). However, the relationship between obesity and other salient public health outcomes (i.e., sexually transmitted infections) is less clear.
One such public health outcome is HIV sexual transmission risk behaviors. MSM with extreme weights may be less likely to engage in condom use during anal intercourse, as they may lack self-esteem and/or self-efficacy due to negative thoughts and feelings about their weight or shape. In other words, overweight or obese MSM may be concerned that asking a sexual partner to wear a condom (or wearing one themselves) may lead to rejection. Empirically, findings on the relationship between obesity and sexual risk behaviors among HIV-uninfected MSM have been mixed. Moskowitz and Seal (2010) found that those with a higher BMI had fewer sex partners but were also less likely to use condoms during anal intercourse. In contrast, Allensworth-Davies, Welles, Hellerstedt, and Ross (2008) found that obesity decreased the risk for unprotected anal intercourse; however, others have found non-significant differences between BMI groups on condom use among MSM (Guadamuz et al., 2012). Finally, Kraft, Robinson, Nordstrom, Bockting, and Rosser (2006) noted a non-linear relationship between BMI and condom use, with overweight men being at the highest risk for unprotected anal intercourse and normal weight and obese men being at lower risk. The confluence of these contradicting findings may suggest the role of unaccounted for moderator variables and the need for alternative analytic approaches to further define the relationship of obesity and HIV sexual risk transmission behaviors.
Another variable known to impact sexual risk behavior is depression. Individuals who experience depressive symptoms may seek out sexual risk behaviors in an attempt to modulate negative affect. In addition, core depressive symptoms, such as hopelessness or worthlessness, may promote decreased self-care activities, including less frequent condom use. In a meta-analysis, Crepaz and Marks (2001) found a non-significant association (r = .04) between depression and sexual risk behaviors; however, significant heterogeneity was noted in the effect size parameters. This suggested the presence of unaccounted for moderator variables. Furthermore, non-linear relations between depression and sexual risk behaviors were not examined. This is a limitation, given that curvilinear associations of depression and sexual risk behaviors have been found among HIV-uninfected (Koblin et al., 2006) and HIV-infected MSM (O’Cleirigh et al., 2013). These findings indicate that there is a complex relationship between depression and sexual risk behaviors and that non-linear and/or moderator variables should be further explored in future research.
Few studies to date have explored the interactive effect of BMI and psychological distress variables, such as depression, in the context of sexual risk behaviors. Among HIV-uninfected post-partum women, Kershaw, Arnold, Lewis, Magriples, and Ickovics (2011) found that psychosocial distress interacted with BMI, such that stress and social conflict increased the likelihood of having a risky or casual partner for obese women. Blashill, O’Cleirigh, Mayer, Goshe, and Safren (2012) examined the interactive effect of BMI and depression in predicting condom use during anal intercourse among a sample of HIV-infected MSM. Results showed that depression was related to decreased condom use only for underweight men. Although Kershaw et al. (2011) and Blashill et al. (2012) examined nuanced models of BMI, psychological distress, and sexual risk behavior, limitations in these designs leave room for future research to build upon.
The limited data on the interaction of BMI and psychological distress in predicting sexual risk behavior require additional empirical endeavors to address previous methodological limitations. For instance, the Blashill et al. (2012) study was a cross-sectional design and thus temporal influence could not be determined. Additionally, Blashill et al. had a small n for underweight participants, suggesting the possibility of an unstable cell, thus limiting the generalizability of the results. While Kershaw et al. (2011) addressed one issue by employing a longitudinal design, predictor variables were time invariant, and their outcome variable included only two time points, which is considered inadequate to assess growth curves, as two wave studies cannot describe individual trajectories of change and confound true change with measurement error (Singer & Willett, 2003). The present study added to the literature by employing a prospective design with a large, nationally-distributed cohort sample of HIV-infected MSM, which assessed time variant BMI, depression, and condom use over three waves of data.
METHOD
Participants
Participants were 490 HIV-infected MSM, of whom 48% were normal weight, 40% were overweight, and 12% were obese (underweight men were not included in the current study due to a very small n across time points). The mean age of the sample was 41.2 years (SD = 9.5). Race included 78% White, 11% Black, 4% Asian, and 7% Other; ethnicity included 30% Hispanic and 70% non-Hispanic.
Procedure
The sample was selected from a large, national HIV clinical cohort (The Center for AIDS Research [CFAR]--Network of Integrated Clinical Systems [CNICS]) which has been previously described in detail (Kitahata et al., 2008). CNICS consists of 8 CFAR sites across the U.S. and includes more than 25,000 HIV-infected individuals, dating back to 1995. Approximately every two months, participating CNICS sites upload standardized patient data into the centralized CNICS Data Repository, which was the data source for this study. Repository data included patient-reported measures, such as depression and sexual risk behavior, collected as part of the CNICS assessment which was implemented as part of routine clinical care at four CNICS sites between 2005 and 2011. CNICS was approved by each site’s respective institutional review board.
The current study included patients who were MSM (i.e., those who reported their sex was male and had anal intercourse with another man within the past six months) and had completed the CNICS clinical assessment of patient-reported measures at one of the four participating sites. Data from September 2005 to July 2011 were included.
Measures
BMI
Objectively measured height and weight were extracted from participants’ medical records. BMI was operationally defined as: weight in pounds/(height in inches × height in inches) × 703, and the following categorical groups were created based on guidelines from the National Institutes of Health (NIH): BMI 18.5 to 24.9 (normal weight), BMI 25 to 29.9 (overweight), and BMI ≥ 30 (obese).
Depression
Symptoms of depression were measured using the continuous total score from the 9-item Depression Severity Scale of the Patient Health Questionnaire (PHQ) (Spitzer, Kroenke, & Williams, 1999), a self-report instrument designed to detect symptoms of major depressive disorder in primary care settings through diagnostic and symptom severity assessments. Participants reported the frequency in which they experienced each symptom with response options ranging from 1 (“not at all”) to 4 (“nearly every day”). For the current sample, internal consistency at baseline was α = .90.
Condom Use Behavior
Participants responded to the item “In the past 6 months, how often did you use condoms when you had anal sex?” Responses options ranged from 1 (“Never”) to 4 (“Always”).
Statistical Analyses
The main analyses of the study, examining BMI, depression, and their interaction term as longitudinal predictors of condom use, were conducted via linear mixed-effects modeling in SPSS 20 (MIXED Procedure). One of the advantages of mixed-effects modeling is that it allows participants to be included in analyses with missing data—a common occurrence in longitudinal clinical cohort data. The time variable provided the structure to the model with three waves of data (baseline, 11, and 14 months post-baseline), and was entered as both a fixed and random effect. Random intercepts and slopes were also entered, which allow different participants to have unique growth trajectories. Time variant values (i.e., data were assessed at each of the three times points) of depression and BMI (and their interaction term) were entered into the model, as fixed effects, to predict condom use during anal intercourse over time. The restricted maximum likelihood (REML) estimation method was chosen in lieu of maximum likelihood (ML) estimation, as the former approach tends to result in unbiased estimates of the variances and covariances (West, 2009). The scaled identity covariance structure was chosen based on the best goodness-of-fit (as evaluated by the Akaike Information Criterion [AIC]), compared to competing covariance structures. The AIC was also used to evaluate the fit of linear vs. quadratic models, with linear models fitting the data better. Finally, to assess the incremental fit of adding the interaction term into the model, the AIC was compared to a model with only main effects. The model with a lower AIC is considered to fit the data better (Singer & Willett, 2003).
RESULTS
Demographic characteristics (along with depression symptoms) were examined by BMI group membership. A trend (p = .06) indicated that age differed by BMI groups, with overweight men being older than normal weight men. White participants were disproportionally represented (p = .04) in the overweight (84%) and normal weight (79%) groups compared to the obese (73%) group. Therefore, age and race were covaried; however, it should be noted that results did not significantly differ between adjusted and unadjusted models.
An initial unconstrained model of condom use over time indicated that condom use during anal intercourse did not significantly change over the course of the study, γ = −.01, SE = .009, 95% CI [−.03, .007], t(78) = −1.1. There was significant individual variance in the slope, γ = .006, SE = .002, 95% CI [.003, .01], Wald z = 2.6, p = .008, and intercept, γ = 1.5, SE = .10, 95% CI [1.3, 1.7], Wald z = 15.3, p < .0001. These findings indicate that participants varied in their initial condom use score at baseline, as well as the rate of change over time, suggesting the utility of modeling time and participants’ slopes and intercepts as random effects. Finally, the estimated covariance of the two random effects emerged as significant, γ = −.05, SE = .01, 95% CI [−.08, −.03], Wald z = −4.2, p < .0001, indicating that the higher a participant’s intercept on condom use, the smaller the rate of change. Given that condom use did not significantly change over time, the results presented below collapse across all time points.
Next, a model predicting condom use over time was tested with depression as the predictor variable. Results revealed a significant effect of depression, F(1, 405) = 16.6, p < .0001, γ = −.033, SE = .008, 95% CI [−.05, −.018], t(405) = −4.1, p < .0001, indicating that a one unit increase in depression was prospectively associated with a .033 decrease in condom use.
An analogous model was tested with BMI category as the only predictor variable. Results revealed a significant effect of BMI category, F(2, 547) = 5.2, p = .006. Normal weight men used condoms significantly less frequently than overweight men, γ = .29, SE = .11, 95% CI [.07, .51], t(546) = 2.52, p = .001, and obese men, γ = .47, SE = .17, 95% CI [.13, .80], t(528) = 2.71, p = .007, with the latter two groups not differing significantly, γ = .18, SE = .17, 95% CI [−.15, .51], t(552) = 1.05.
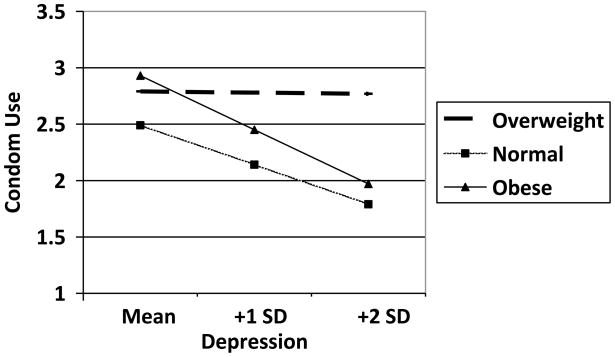
The main analyses of the study revealed a significant BMI by depression interaction, F(2, 554) = 6.4, p = .002. Probing this interaction revealed that depressive symptoms had a stronger inverse effect on condom use for obese MSM, compared to overweight men, γ = .07, SE = .03, 95% CI [.01, .13], t(578) = 2.3, p = .02, in that depressive symptoms were predictive of less frequent condom use for obese but not overweight men. Analogous results were found in regard to comparisons between normal weight and overweight men, γ = .05, SE = .016, 95% CI [.02, .08], t(514) = 3.2, p = .002. The relationship between depression and condom use slope did not differ statistically between obese and normal weight men, γ = −.017, SE = .03, 95% CI [−.07, .04], t(574) < 1. Thus, the relationships between depression and change in condom use for the respective BMI categories were: obese, γ = −.075, SE = .027, 95% CI [−.13, −.02], t(59) = −2.8, p = .007; normal weight, γ = −.057, SE = .011, 95% CI [−.08, −.035], t(249) = −5.2, p < .0001; and overweight, γ = .001, SE = .012, 95% CI [−.02, .03], t(226) = .09. The BMI by depression interaction also displayed a better fit of the data (AIC = 1915.61) compared to a model with only main effects (AIC = 1917.23), suggesting that the interaction incrementally added to the model.
DISCUSSION
The current study represents the first known longitudinal investigation of BMI, depression, and condom use among HIV-infected MSM. The confluence of contradicting results in the existing literature suggests the presence of unaccounted for moderator variables impacting the reported associations of BMI, depression, and sexual risk behavior in this unique population. To date, only two known studies have assessed the interactive effect of psychological distress variables and BMI in predicting sexual risk behaviors (Blashill et al., 2012; Kershaw et al., 2011) and only one (Blashill et al., 2012) sampled MSM and was cross-sectional in nature.
The main finding from the current study revealed a significant BMI by depression interaction in predicting condom use during anal intercourse. Specifically, over time, depression was associated with decreased condom use for normal weight and obese HIV-infected MSM. These results partially mirror those of Kershaw et al. (2011), who found that stress and social conflict interacted with BMI in predicting having a risky sexual partner, in that obese women were more likely to engage in risky sex with partners when they reported elevated levels of distress. The findings from the current study suggest that negative affect also impacts condom use for obese HIV-infected MSM. This finding qualifies some existing research which concluded that obesity was associated with increased condom use. Main effects from the current study also highlighted this fact; however, given the comorbidity of depression and obesity (e.g., Luppino et al., 2010; Simon et al., 2006), it would seem that not assessing both depression and obesity concurrently represents a limitation in the literature to date and should be considered as standard for future studies in this area.
The results from the current study are also, to our knowledge, the first cohort study to examine prevalence rates of overweight and obesity amongst an exclusively HIV-infected MSM sample. Findings revealed prevalence rates of overweight (40%) and obesity (12%) at 52%. These results largely mirror findings by Crum-Cianflone (2010), who reported rates of overweight (41.5%) and obesity (14.4%) at 56% among a sample of HIV-infected men and women. Further, Guadamuz et al. (2012) reported rates of overweight (43.5%) and obesity (9.4%) at 53% for HIV-uninfected MSM. Thus, it appears that MSM, regardless of their HIV status have similar overall levels of overweight and obesity, with HIV-infected MSM possibly having elevated obesity (12% vs. 9.4%).
Despite the novel findings from the current study, it is not without limitations. Of note, additional variables, such as body dissatisfaction, were not included. Given that there are significant relationships between both body dissatisfaction and obesity (e.g., Schwartz & Brownell, 2004) and body dissatisfaction and sexual risk behaviors (e.g., Wilton, 2009), future research should incorporate BMI, body image, as well as psychological distress variables, such as depression in the context of sexual risk. Additionally, the nature of the sample may limit generalizability of the results, as the sample exclusively included MSM, who were primarily White. Translating the results to women and/or non-White races should be done cautiously. Furthermore, CNICS represents patients in clinical care and may not be generalizable to HIV-infected patients who have not yet been diagnosed or are not engaged in clinical care. The metric of BMI also has limitations, most notable is the possible conflation of muscularity and adiposity. For instance, participants grouped into the “overweight” category may have been incorrectly labeled due to possession of a highly mesomorphic physique. We also chose to analyze BMI as a function of groups in lieu of a continuous measure. Although this approach has limitations, these NIH established cutoffs correspond to important health outcomes, and we wished to model this approach is assessing an oft overlooked area related to BMI and health—HIV sexual transmission risk. The measurement of condom use was also limited in that it consisted of a single item and did not discriminate between the HIV status of sexual partners. This is one of the disadvantages of large, clinical cohort studies; however, the failure to identify the HIV status of partners does not preclude the implications of the study’s findings. For instance, unprotected anal intercourse is a sexual risk behavior regardless of HIV status, as HIV-infected individuals may also acquire (and transmit) a variety of sexually transmitted infections. The possibility of this co-infection can significantly affect the disease progression of HIV and the overall health of HIV-infected individuals (e.g., Greub et al., 2000; Law et al., 2004; Lynn & Lightman, 2004). Finally, we were unable to include underweight participants in the analyses due to the small number of these patients who completed multiple waves of data. Given that there is cross-sectional data that indicate depression particularly influences sexual risk for underweight HIV-infected MSM (Blashill et al., 2012), future prospective studies are needed to confirm this finding. In may be that extreme BMIs (underweight and obese) represent a specific vulnerability to sexual risk in the context of depression.
Although the current study highlighted the role of moderators in the relationship between BMI and HIV sexual transmission risk behaviors, the mechanisms that drive this relationship remain unclear. Future research may benefit from exploring mediational models, in which plausible pathways of BMI to sexual risk behaviors are tested. One candidate for study is condom self-efficacy. Pervious research with HIV-uninfected African-American adolescent girls revealed that dissatisfaction with weight/shape was associated with decreased self-efficacy related to condom use and fear of rejection by sexual partners (Wingood, DiClemente, Harrington, & Davies, 2002). Other researchers have noted significant relationships between elevated BMI and intoxication during intercourse (Eisenberg, Neumark-Sztainer, & Lust, 2005). Although these constructs have not been examined among HIV-infected MSM, it is possible that they may be salient factors to consider in designing future research with this population.
The results from the current study have the potential to inform clinical interventions. Given that elevated levels of depression predicted decreased condom use during anal intercourse for obese HIV-infected MSM, integrated secondary prevention interventions are needed. Traditional prevention interventions for HIV-infected individuals yield modest effects (e.g., Crepaz et al., 2006). As has been recently recommended (e.g., Safren, Blashill, & O’Cleirigh, 2011; Sikkema et al., 2010), incorporating the treatment of psychosocial problems (e.g., depression) into traditional behavioral prevention efforts may likely improve the effectiveness of these interventions. It is unlikely that obesity in and of itself is a facilitator of depression in the context of sexual risk, but rather, obesity may be a marker of elevated body dissatisfaction (e.g., Peplau et al., 2009; Schwartz & Brownell, 2004). Perhaps an integrated sexual risk reduction/depression intervention could be combined with treatment for body dissatisfaction. Addressing sexual risk, depression, and body image in an integrated manner may represent an efficient, cost-effective approach to improving multiple health behaviors (Blashill, Perry, & Safren, 2011). Although to date no known interventions exist that have addressed body image and depression among HIV-infected individuals, recent evidence suggests that an integrative HIV prevention intervention that also targets mental health concerns may be particularly helpful for HIV-infected MSM with depression (Safren, O’Cleirigh, Skeer, Elsesser, & Mayer, 2013). Future research is needed in testing an integrative treatment that includes body-related concerns.
Figure 1. Depression predicting condom use by BMI category.
Note. Mean = PHQ-9 score of 15.4, +1 SD = PHQ-9 score of 21.8, +2 SD = PHQ-9 score of 28.2; higher score denote increased depressive symptoms. Condom use scores range between 1 (“Never”) and 4 (“Always”), with lower scores denoting less frequent condom use.
Acknowledgments
This work was supported in part by the CNICS grant (R24AI067039, Saag). Patient Reported Outcome (PRO) collection in CNICS is also supported in part by the PROMIS HIV grant (U01AR057954, Crane). Some investigator time is supported by K23MH096647 (Blashill) and K24MH094214 (Safren). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Allensworth-Davies D, Welles SL, Hellerstedt WL, Ross MW. Body image, body satisfaction, and unsafe anal intercourse among men who have sex with men. Journal of Sex Research. 2008;45:49–56. doi: 10.1080/00224490701808142. [DOI] [PubMed] [Google Scholar]
- Blashill AJ, O’Cleirigh C, Mayer KH, Goshe BM, Safren SA. Body mass index, depression, and sexual transmission risk behaviors among HIV-positive MSM. AIDS and Behavior. 2012;16:2251–2256. doi: 10.1007/s10461-011-0056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blashill AJ, Perry N, Safren SA. Mental health: A focus on stress, coping, and mental illness as it relates to treatment retention, adherence, and other health outcomes. Current HIV/AIDS Reports. 2011;8:215–222. doi: 10.1007/s11904-011-0089-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray GA. Medical consequences of obesity. Journal of Clinical Endocrinology and Metabolism. 2004;89:2583–2589. doi: 10.1210/jc.2004-0535. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Lyles CM, Wolitski RJ, Passin WF, Rama SM, Herbst JH, Stall R. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20:143–157. doi: 10.1097/01.aids.0000196166.48518.a0. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychology. 2001;20:291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- Crum-Cianflone N, Roediger MP, Eberly L, Headd M, Marconi V, Ganesan A, Agan BK. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PLoS ONE. 2010;5:e10106. doi: 10.1371/journal.pone.0010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg ME, Neumark-Sztainer D, Lust KD. Weight-related issues and high-risk sexual behaviors among college students. Journal of American College Health. 2005;54:95–101. doi: 10.3200/JACH.54.2.95-101. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index in obesity among U.S. adults, 1999–2010. Journal of the American Medical Association. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Greub G, Ledergerber B, Battegay M, Grob P, Perrin L, Furrer H, Telenti A. Clinical progression, survival, and immune recovery during antiretroviral therapy in patients with HIV-1 and hepatitis C virus coinfection: The Swiss HIV Cohort Study. Lancet. 2000;356:1800–1805. doi: 10.1016/s0140-6736(00)03232-3. [DOI] [PubMed] [Google Scholar]
- Guadamuz TE, Lim SH, Marshal MP, Friedman MS, Stall RD, Silvestre AJ. Sexual, behavioral, and quality of life characteristics of healthy weight, overweight, and obese gay and bisexual men: Findings from a prospective cohort study. Archives of Sexual Behavior. 2012;41:385–389. doi: 10.1007/s10508-011-9859-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw TS, Arnold A, Lewis JB, Magriples U, Ickovics JR. The skinny on sexual risk: The effects of BMI on STI incidence and risk. AIDS and Behavior. 2011;15:1527–1538. doi: 10.1007/s10461-010-9842-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitahata MM, Rodriguez B, Haubrich R, Boswell S, Matthews WC, Lederman MM, Saag MS. Cohort profile: The Centers for AIDS Research Network of Integrated Clinical Systems. International Journal of Epidemiology. 2008;37:948–955. doi: 10.1093/ije/dym231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Buchbinder S. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Kraft C, Robinson BB, Nordstrom DL, Bockting WO, Rosser BR. Obesity, body image, and unsafe sex in men who have sex with men. Archives of Sexual Behavior. 2006;35:587–595. doi: 10.1007/s10508-006-9059-x. [DOI] [PubMed] [Google Scholar]
- Law WP, Duncombe CJ, Mahanontharit A, Boyd MA, Ruxrungtham K, Lange JM, Dore GJ. Impact of viral hepatitis co-infection on response to antiretroviral therapy and HIV disease progression in the HIV-NAT cohort. AIDS. 2004;18:1169–1177. doi: 10.1097/00002030-200405210-00010. [DOI] [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: A systematic review and meta analysis of longitudinal studies. Archives of General Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Lynn WA, Lightman S. Syphilis and HIV: A dangerous combination. Lancet Infectious Diseases. 2004;4:456–466. doi: 10.1016/S1473-3099(04)01061-8. [DOI] [PubMed] [Google Scholar]
- Marti A, Macros A, Martinez JA. Obesity and immune function relationships. Obesity Reviews. 2001;2:131–140. doi: 10.1046/j.1467-789x.2001.00025.x. [DOI] [PubMed] [Google Scholar]
- Moskowitz DA, Seal DW. Revisiting obesity and condom use in men who have sex with men. Archives of Sexual Behavior. 2010;39:761–765. doi: 10.1007/s10508-009-9478-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, Safren SA. Moderate levels of depression predict sexual transmission risk in HIV-infected MSM: A longitudinal analysis of data from six sites involved in a “Prevention for Positives” study. AIDS and Behavior. 2013;17:1764–1769. doi: 10.1007/s10461-013-0462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peplau LA, Frederick DA, Yee C, Maisel N, Lever J, Ghavami N. Body image satisfaction in heterosexual, gay, and lesbian adults. Archives of Sexual Behavior. 2009;38:713–725. doi: 10.1007/s10508-008-9378-1. [DOI] [PubMed] [Google Scholar]
- Safren SA, Blashill AJ, O’Cleirigh CM. Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS and Behavior. 2011;15:30–34. doi: 10.1007/s10461-011-9898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, O’Cleirigh CM, Skeer M, Elsesser SA, Mayer KH. Project Enhance: A randomized controlled trial of an individualized HIV prevention intervention for HIV–infected men who have sex with men conducted in a primary care setting. Health Psychology. 2013;32:171–179. doi: 10.1037/a0028581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1:43–56. doi: 10.1016/S1740-1445(03)00007-X. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Watt MH, Drabkin AS, Meade CS, Hansen NB, Pence BW. Mental health treatment to reduce HIV transmission risk behavior: A positive prevention model. AIDS and Behavior. 2010;14:252–262. doi: 10.1007/s10461-009-9650-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC. Association between obesity and psychiatric disorders in the US adult population. Archives of General Psychiatry. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Tate T, Willig AL, Willig JH, Raper JL, Moneyham L, Kempf M, Mugavero MJ. HIV infection and obesity: Where did all the wasting go? Antiviral Therapy. 2012;17:1281–1289. doi: 10.3851/IMP2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West BT. Analyzing longitudinal data with linear mixed models procedures in SPSS. Evaluation & The Health Professions. 2009;32:207–228. doi: 10.1177/0163278709338554. [DOI] [PubMed] [Google Scholar]
- Wilton L. A preliminary study of body image and HIV sexual risk behavior in black gay and bisexual men: Implications for HIV prevention. Journal of Gay & Lesbian Social Sciences. 2009;21:309–325. [Google Scholar]
- Wingood GM, DiClemente RJ, Harrington K, Davies SL. Body image and African American females’ sexual health. Journal of Women’s Health & Gender-Based Medicine. 2002;11:433–439. doi: 10.1089/15246090260137608. [DOI] [PubMed] [Google Scholar]