Abstract
Purpose
To determine the effect of induced monocular blur on stereoacuity measured using ‘real depth’ and ‘random dot’ tests.
Methods
Monocular visual acuity deficits (range 20/15 to 20/1600) were induced with 7 different Bangerter filters (<0.1, 0.1, 0.2, 0.3, 0.4, 0.8, and 1.0) in 15 visually normal adults. Stereoacuity was measured using Frisby and Frisby Davis Distance (FD2) ‘real depth’ tests and Preschool Randot (PSR) and Distance Randot (DR) ‘random dot’ tests. Stereoacuity results were grouped as either ‘fine’ (≤60 arcsec), ‘moderate’ (>60 and ≤200 arcsec), or ‘coarse/nil’ (>200 arcsec to nil) stereo.
Results
Across visual acuity deficits, stereoacuity was more severely degraded with random dot (PSR, DR) than with real depth (Frisby, FD2) tests. Degradation to ‘worse than fine’ stereoacuity consistently occurred at 0.7 logMAR (20/100) or worse for Frisby, 0.1 logMAR (20/25) or worse for PSR, 0.1 logMAR (20/25) or worse for FD2. There was no meaningful threshold for the DR since ‘worse than fine’ stereoacuity was associated with −0.1 logMAR (20/15). Course/nil stereoacuity was consistently associated with 1.2 logMAR (20/320) or worse for Frisby, 0.8 logMAR (20/125) or worse for PSR, 1.1 logMAR (20/250) or worse for FD2, and 0.5 logMAR (20/63) or worse for DR.
Conclusions
Stereoacuity thresholds are more easily degraded by reduced monocular visual acuity using random dot tests (PSR and DR) than real depth tests (Frisby and FD2). We have defined levels of monocular visual acuity degradation associated with ‘fine’ and ‘nil’ stereoacuity. These findings have important implications for testing stereoacuity in clinical populations.
Introduction
Reduced stereoacuity is commonly associated with either reduced visual acuity in one eye or with ocular misalignment. In patients with ocular misalignment, the severity of stereoacuity degradation appears to differ depending on which test of stereoacuity is used, as measured stereoacuity is more severely degraded when using random dot tests than when using real depth tests.1–4 There are few data on the effect of pure monocular blur on measured stereoacuity, particularly for more recent clinical tests. Based on differences in performance between random dot and real depth tests in strabismus patients,1–4 we hypothesized that there would be differences in performance on different stereoacuity tests at different levels of visual acuity deficit. The purpose of the present study was to determine the effect of induced monocular blur on stereoacuity measured using real depth and random dot tests and to define the levels of monocular blur associated with reduced stereoacuity.
Subjects and Methods
Institutional Review Board approval was obtained and each patient gave informed consent before participating. All procedures and data collection were conducted in a manner compliant with the Health Insurance Portability and Accountability Act.
Subjects
We previously reported the effect of blurring one eye with Bangerter filters on different modalities of visual function in 15 visually normal adults.5 In this present study we report the effect on stereoacuity in the same 15 subjects, measured using four different stereoacuity tests.
Participants, mainly volunteers from the local medical student population, were aged 22 to 35 years (median 24 years); ten (67%) of 15 were male and 8 (53%) were Caucasian. All subjects had best corrected visual acuity of 20/25 Snellen or better in each eye, stereoacuity of at least 40 arcsec using the Titmus as a screening test, and orthotropia at both near and distance by cover test. No subject had a history of strabismus or other eye disease.
Methods
As described in our previous report,5 Bangerter filters (Fresnel Prism and Lens Co., LLC, Eden Prairie, MN) were applied to the inner surface of plano trial lenses. Seven filter densities were selected: <0.1, 0.1, 0.2, 0.3, 0.4, 0.8, and 1.0 (from most to least dense), the same filters being used for all subjects. Mounted filters were placed over one eye, either in trial frames or using Halberg clips over the subject’s spectacles. Filter testing order progressed step-wise from the most dense (<0.1) to the least dense (1.0) filter. For each subject, acuity and stereoacuity tests were performed with each of the seven filters over one eye and then repeated, on a separate occasion, with each of the seven filters over the other eye. Each Bangerter filter induced a range of visual acuity deficits.5 For each eye baseline (without filter) measures were performed at the end of testing, creating a total of 240 trials for each stereotest. Eye testing order was randomized by dominant or non-dominant eye, determined using the distance hole-in-the-card test.6
Distance optotype visual acuity assessment
At each filter density, distance optotype acuity was assessed monocularly using a standardized protocol on the electronic M&S Smart System II PC Plus (M&S Technologies, Inc. Park Ridge, Illinois). Single letters, with crowding bars, were displayed in a random sequence, first in a screening phase, one letter per logMAR level until failed, then in a threshold determination phase7 in which three of five correct responses were required to pass. If the subject could not identify the largest optotype (20/400), they were moved to a quarter of the testing distance so that the 20/400 letter subtended 20/1600 (1.9 logMAR), from which point testing progressed by decreasing 0.1 logMAR steps. Testing was performed at a distance of 3 m, and at 0.75 m if needed. The range tested was 20/12 to 20/1600 (−0.2 to 1.9 logMAR).
Near optotype acuity
The Near Visual Acuity Test (Lighthouse International, New York, NY) was used to assess optotype visual acuity at a distance of 40 cm. Near acuity measurements were converted to logMAR values based on the test distance and the M value. The range tested was −0.1 to 1.3 logMAR. Near optotype acuity was only measured in 10 of 15 subjects (13 of 20 eyes) because it was added to the protocol after commencement of the study.
Vernier acuity
As described previously,5 vernier acuity was also assessed at each filter level, using vernier offset patterns mounted on cards8 (measuring 56 × 24 cm) with square wave gratings of 0.5 cycles/degree and offsets of 3.72 mm, 0.93 mm, and 0.23 mm. There were two gratings on each card, one with an offset, and one without. The presentation of the grating with the offset was randomized by rotating the card. Through varied testing distances (38 cm to 8 m), testing levels ranged from 6 arcsec to 1920 arcsec in logMAR steps (−1.0 to 1.5 logMAR). Four of four correct responses were required to pass each logMAR level.
Contrast Sensitivity
Contrast sensitivity was measured using Pelli-Robson optotype based contrast sensitivity charts (Clement Clarke International, Harlow, UK), as described in our previous report.5 Testing was performed in recommended lighting conditions at the standard 1 m distance. The two testing charts were alternated each time the filter was changed. Two of three correct responses were required to pass each contrast level and thresholds were recorded in log units, ranging from 0.0 to 2.1 log units.
Stereoacuity
At each Bangerter filter level, stereoacuity was assessed using four stereotests: two real depth tests (Frisby at near; Frisby Davis Distance (FD2) at distance) and two random dot tests (Preschool Randot (PSR) at near; Distance Randot (DR) at distance). At each filter level, stereoacuity was assessed in the following order: Frisby, FD2, PSR, DR. Once testing had been completed with the final (1.0) filter, baseline (no filter) Frisby, FD2, PSR and DR stereoacuity was assessed.
Real depth stereoacuity tests
The three plates of the near Frisby test were presented at a range of distances (38 cm, 48 cm, 57 cm, 60 cm) to yield disparities of 400, 200, 100, 60 and 40 arcsec. At each disparity level, two of two correct responses were required to pass. Threshold was recorded as the finest disparity at which two of two presentations were correctly identified. Patients unable to pass the 400 arcsec level were recorded as having ‘nil’ stereo.
FD2 stereoacuity was assessed at 3 meters, testing disparities of 200, 160, 80, 40 and 20 arcsec, as described previously.9, 10 At each disparity level, two of two correct responses were required to pass. Threshold was recorded as the finest disparity at which two of two shapes were correctly identified. A monocular testing phase9 was performed the first time a subject obtained a threshold of 200 to 80 arcsec to ensure that such threshold scores reflected binocular, rather than monocular, responses. None of our subjects could pass 80, 160 or 200 arcsec using monocular cues. Patients unable to pass the 200 arcsec level were recorded as having ‘nil’ stereo.
Random dot stereoacuity tests
The PSR test, a Polaroid vectograph, was performed at 40 cm, testing fixed disparities of 800, 400, 200, 100, 60 and 40 arcsec.11, 12 Polarizing glasses were placed over the trial frames or the subjects spectacles. Two correct responses were required to pass each level, and threshold was determined by the finest disparity at which two shapes were correctly identified. Patients unable to identify shapes at the 800 arcsec level were recorded as having ‘nil’ stereo.
The DR, a Polaroid vectograph, was tested at 3 meters, testing fixed disparities of 400, 200, 100 and 60 arcsec.2, 10, 13 Two correct responses were required to pass each disparity level, and threshold was recorded as the finest disparity at which two shapes were correctly identified. Patients unable to pass the 400 arcsec level were recorded as having ‘nil’ stereo.
Statistical analysis
To account for potential bias of comparing stereotests with different measurable levels, stereoacuity results were grouped as either ‘fine’ (≤60 arcsec), ‘moderate’ (>60 and ≤200 arcsec) or ‘coarse/nil’ (>200 arcsec to nil) stereo. Also, because we found no systematic differences when comparing data from the blurring of dominant versus non-dominant eyes, data were combined for analysis and generalized linear models utilizing generalized estimating equation (GEE) methods were used to account for correlation between the eyes.
Median stereoacuity values were calculated for each stereotest and compared between stereoacuity tests using GEE methods with contrasting statements. The degradation of stereoacuity across all filters was calculated for each stereotest, by absolute threshold and by the three tiers of stereoacuity. For each stereotest, the worst level of monocular distance optotype acuity consistently associated with ‘worse than fine’ stereoacuity was derived.
To examine the relationship between distance optotype acuity and the other modalities of visual function, scatter plots were created to compare distance optotype acuity versus near optotype acuity, distance optotype acuity versus vernier acuity and distance optotype acuity versus contrast sensitivity. Spearman rank correlation coefficients were calculated for each relationship.
Results
Baseline stereoacuity
As expected in this cohort of normal adults, the median stereoacuity values without Bangerter filters were excellent: Frisby 40 arcsec (all 40 arcsec), FD2 20 arcsec (range 20 to 60 arcsec), PSR 40 arcsec (range 40 to 60 arcsec), and DR 60 arcsec (range 60 to nil; 5 of 15 patients demonstrated less than 60 arcsec stereoacuity without filters on both trials).
Overall effect of monocular blur across the range of filters
Median stereoacuity values across all filter levels were: Frisby 40 arcsec; FD2 60 arcsec; PSR 100 arcsec, and DR >400 arcsec. Analyzed by categories of ‘fine,’ ‘moderate,’ or ‘course/nil,’ the median stereoacuity across filters was: Frisby ‘fine,’ FD2 ‘fine,’ PSR ‘moderate,’ DR ‘course/nil.’ Stereoacuity was more severely degraded with random dot (PSR, DR) tests compared with real depth (Frisby, FD2) tests (P<0.0001 for each comparison).
Stereoacuity degradation as a function of distance optotype acuity
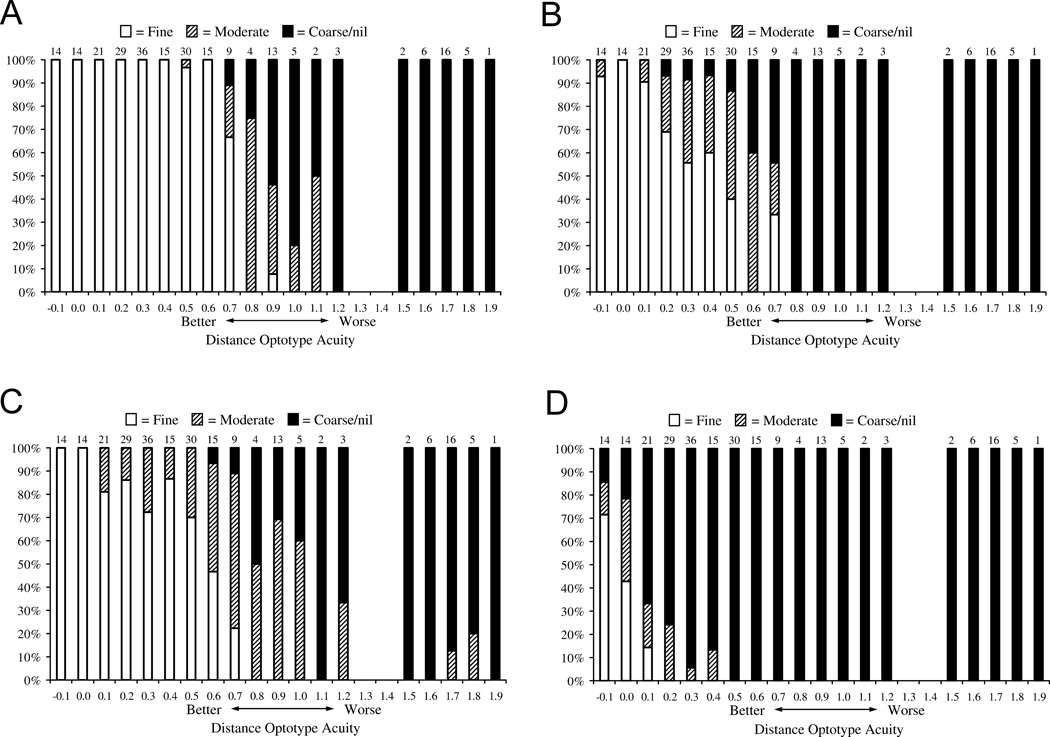
To provide practical thresholds at which degradation of optotype visual acuity was associated with degradation of stereoacuity, we report the distance optotype acuity at which further degradation resulted in failure of some subjects to pass ‘fine’ levels (60 arcsec or better).
Degradation below ‘fine’ stereoacuity occurred from 0.7 logMAR (20/100) or worse for Frisby (Figure 1A), 0.1 logMAR (20/25) or worse for PSR (Figure 1B) and 0.1 logMAR (20/25) or worse for FD2 (Figure 1C). For the DR test some subjects showed below ‘fine’ stereoacuity at −0.1 (20/15) (Figure 1D). Since optotype visual acuity was not measured at levels finer than −0.1 (20/15) there was no meaningful threshold for the DR test.
Figure 1.
Comparison of distance optotype acuity to corresponding stereoacuity values across all subjects, using the Frisby (A), Pre-school Randot (B), Frisby Davis Distance (C) and Distance Randot (D) tests. Bars show percentage of subjects achieving ‘fine’ (≤60 arcsec), ‘moderate’ (>60 and ≤200 arcsec) or ‘coarse/nil’ (>200 arcsec to nil) stereoacuity at each level of distance optotype acuity. Numbers at the top of each bar represent the number of measures of stereoacuity for each level of visual acuity, totalling 240 observations..
Coarse/nil stereoacuity was associated with 1.2 logMAR (20/320) or worse for Frisby (Figure 1A), 0.8 logMAR (20/125) or worse for PSR (Figure 1B) 1.1 logMAR (20/250) or worse for FD2 (Figure 1C), and 0.5 logMAR (20/63) or worse for DR (Figure 1D).
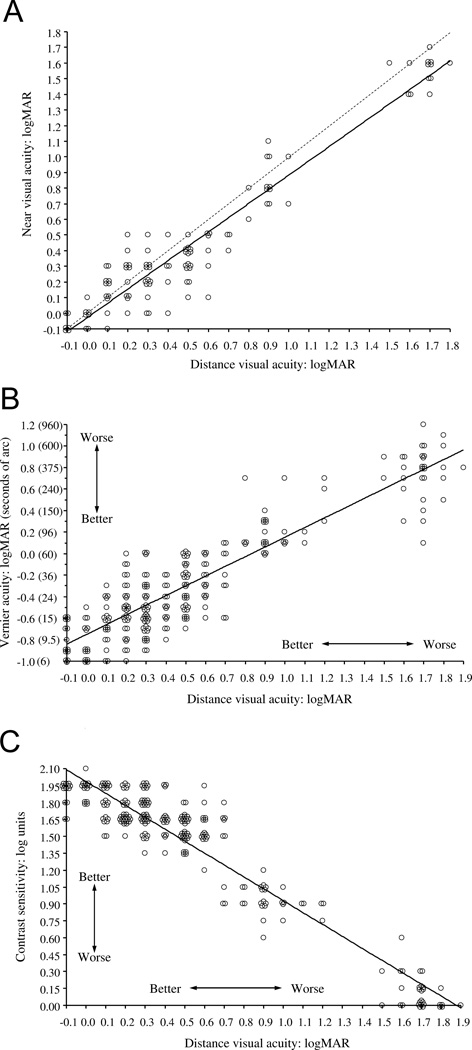
Distance optotype and near optotype acuity
Comparison of distance optotype and near optotype acuity showed overall good agreement (r=0.88, P<0.0001 Figure 2A). There was a small systematic bias towards better optotype acuity at near: mean difference = 0.075 +/− 0.19 logMAR (GEE adjusted), P<0.0001.
Figure 2.
Comparison of distance optotype acuity to near optotype acuity (A), vernier acuity (B), and contrast sensitivity (C). For a given degradation of distance optotype acuity there is a similar degradation of near optotype acuity (A; r=0.88, P<0.0001) with a small mean difference of 0.075 +/− 0.19 logMAR towards better near optotype acuity. There is an overall association between degradation of distance optotype acuity and degradation of both vernier acuity (B; r=0.83, P<0.0001) and contrast sensitivity (C; r=−0.83, P<0.0001).
Since two of the tests of stereoacuity are performed at near (Frisby and PSR) the effect of degradation of near optotype visual acuity on stereoacuity was examined in analogous histograms to those shown for distance optotype visual acuity in Figure 1. A pattern similar to distance optotype visual acuity was seen, where stereoacuity was degraded to ‘worse than fine’ when the near optotype visual acuity was 0.6 logMAR or worse for Frisby and 0.0 logMAR or worse for PSR.
Distance optotype versus vernier acuity and contrast sensitivity
Since Bangerter foils simultaneously degrade vernier acuity and contrast sensitivity, in addition to optotype visual acuity,5 we examined the relationships between distance optotype acuity and vernier acuity (Figure 2B) and between distance optotype acuity and contrast sensitivity (Figure 2C), under conditions of blur with Bangerter filters. Overall, there was an association between degradation of distance optotype acuity and vernier acuity (r=0.83, P<0.0001 Figure 2B), and between degradation of distance optotype acuity and contrast sensitivity (r=−0.83, P<0.0001 Figure 2C).
Discussion
Measurable stereoacuity thresholds progressively degraded as optotype visual acuity was degraded in one eye. The level of degradation was found to vary depending on the specific stereotest used. Measurable stereoacuity was more easily degraded by monocular blur when tested using random dot tests (PSR and DR) compared with real depth tests (Frisby and FD2).
Previous studies examining the effects of induced optotype acuity deficits on stereoacuity have used methods of either optical blur14–18 or diffusing filters.19, 20 Our study using Bangerter filters is most similar to the latter studies. While some previous studies report a correlation between decreasing optotype acuity and decreasing stereoacuity,14, 16–18 others15, 19 report a great deal of variability in response. Our study confirms that for a given level of reduction of monocular optotype visual acuity, there may be a range of effects on stereoacuity across subjects, even with the same stereoacuity tests.
Few previous studies have examined the influence of type of stereotest. Our findings appear similar to those of Nakagawa et al,20 who also found that random dot tests degraded more rapidly with decreasing optotype visual acuity than ‘solid pattern’ or real depth tests. Our results also parallel previous studies by our research group, reporting a differential effect of strabismus on measured stereoacuity depending on the type of stereotest used. Real depth tests such as the near Frisby and the FD2 yielded finer thresholds than random dot tests such as the Preschool Randot and the Distance Randot.1, 3 In particular, the near Frisby test seems much more resistant to degradation by monocular blur than the other tests we studied.
The reasons for our findings remain speculative. It would seem possible that in free space, the contours of real depth tests allow greater use of motor fusion mechanisms and therefore improved ability to detect binocular disparity even when optotype visual acuity is degraded. Nevertheless, Archer et al21 studied the effect of monocularly detectable contours on motor fusion amplitudes and found that, using stereo targets in the amblyoscope, the presence or absence of contours made no appreciable difference to motor fusion amplitudes. It is possible that our condition of testing stereoacuity in free space, and our use of fine disparities, might have been the cause of the apparent inconsistency between our results and that of Archer et al.21
The relatively poor performance of the Distance Randot stereotest in our study is noteworthy. Several of our normal adult subjects could not pass the 60 arcsec level. This is in contrast to the first report of normal adults evaluated with this test.2 If a proportion of normal adults cannot achieve ‘fine’ stereoacuity levels, then failure on the Distance Randot test may not be a clinically useful finding, unless the patient previously passed that level.
The main limitation of our study is that we were unable to separate the effects of degrading optotype acuity, vernier acuity, and contrast sensitivity. Bangerter filters simultaneously reduce all three modalities of visual acuity, although contrast sensitivity was less reduced until the very densest of the filters.5 It is well known that reduction of contrast sensitivity alone has an effect on measured stereoacuity thresholds.22–26 Although clinical conditions may affect these modalities differentially, contrast and vernier acuity are often reduced when optotype acuity is reduced, and so Bangerter filters may mimic some clinical conditions. Another potential limitation of this study is that standardizing stereoacuity testing order may have induced bias. Nevertheless, previous studies in adults by our group have shown no apparent fatigue or learning effect when testing stereoacuity.10, 27
The thresholds that we describe for degradation to ‘worse than fine’ stereoacuity will be useful for clinicians (i.e., 0.7 logMAR (20/100) or worse for Frisby, 0.1 logMAR (20/25) or worse for PSR, 0.1 logMAR (20/25) or worse for FD2. If a patient has visual acuity at these levels, such reduction may be enough in itself to explain any stereoacuity ‘worse than fine’ (worse than 60 arcsec). These data may prove useful in the assessment of possible factitious visual loss. Our data also suggest that if the visual acuity in one eye is modestly reduced (e.g. 20/25 to 20/80), it would be reasonable to use the near Frisby test preferentially, since the other tests are frequently affected by monocular blur.
Additional analogous work on the effect of monocular blur on stereoacuity is needed in the pediatric population, since the normal baseline visual acuity in younger children is not 20/20.28 Nevertheless, it is most likely that the same pattern of effects will be seen, where small interocular differences have a more profound effect on measurable stereoacuity when using Randot tests, compared with real depth tests such as the FD2 and Frisby, with the Frisby test being most likely to resist monocular blur.
Acknowledgments
Financial support: Supported by National Institutes of Health Grants EY015799 (JMH), Research to Prevent Blindness, Inc., New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN.
Footnotes
Presented in part as a poster at the Association for Research in Vision and Ophthalmology meeting, April 29th 2008
No conflicting relationships exist.
References
- 1.Leske DA, Birch EE, Holmes JM. Real depth vs randot stereotests. Am J Ophthalmol. 2006;142:699–701. doi: 10.1016/j.ajo.2006.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fu VL, Birch EE, Holmes JM. Assessment of a new distance Randot stereoacuity test. J AAPOS. 2006;10:419–423. doi: 10.1016/j.jaapos.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 3.Holmes JM, Birch EE, Leske DA, Fu VL, Mohney BG. New tests of distance stereoacuity and their role in evaluating intermittent exotropia. Ophthalmology. 2007;114:1215–1220. doi: 10.1016/j.ophtha.2006.06.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rutstein RP, Eskridge JB. Stereopsis in small-angle strabismus. Am J Optom Physiol Opt. 1984;61:491–498. doi: 10.1097/00006324-198408000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Odell NV, Leske DA, Hatt SR, Adams WE, Holmes JM. The Effect of Bangerter Filters on Optotype Acuity, Vernier Acuity, and Contrast Sensitivity. J AAPOS. 2008 doi: 10.1016/j.jaapos.2008.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rice ML, Leske DA, Smestad CE, Holmes JM. Results of ocular dominance testing depend on assessment method. J AAPOS. 2008;12:365–369. doi: 10.1016/j.jaapos.2008.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Camparini M, Cassinari P, Ferrigno L, Macaluso C. ETDRS-Fast: Implementing psychophysical adaptive methods to standardized visual acuity measurement with ETDRS charts. Invest Ophthalmol Vis Sci. 2001;42:1226–1231. [PubMed] [Google Scholar]
- 8.Holmes JM, Archer SM. Vernier acuity cards: a practical method for measuring vernier acuity in infants. J Pediatr Ophthalmol Strabismus. 1993;30:312–314. doi: 10.3928/0191-3913-19930901-10. [DOI] [PubMed] [Google Scholar]
- 9.Holmes JM, Fawcett SL. Testing distance stereoacuity with the Frisby-Davis 2 (FD2) test. Am J Ophthalmol. 2005;139:193–195. doi: 10.1016/j.ajo.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Laird PW, Hatt SR, Leske DA, Holmes JM. Stereoacuity and binocular visual acuity in prism-induced exodeviation. J AAPOS. 2007;11:362–366. doi: 10.1016/j.jaapos.2007.01.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leske DA, Holmes JM. Maximum angle of horizontal strabismus consistent with true stereopsis. J AAPOS. 2004;8:28–34. doi: 10.1016/j.jaapos.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Fawcett SL, Birch EE. Interobserver test-retest reliability of the Randot preschool stereoacuity test. J AAPOS. 2000;4:354–358. doi: 10.1067/mpa.2000.110340. [DOI] [PubMed] [Google Scholar]
- 13.Hatt SR, Mohney BG, Leske DA, Holmes JM. Variability of stereoacuity in intermittent exotropia. Am J Ophthalmol. 2008;145:556–561. doi: 10.1016/j.ajo.2007.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy NS, Glick EB. Stereoscopic perception and Snellen visual acuity. Am J Ophthalmol. 1974;78:722–724. doi: 10.1016/s0002-9394(14)76312-3. [DOI] [PubMed] [Google Scholar]
- 15.Donzis PB, Rappazzo JA, Burde RM, Gordon M. Effect of binocular variations of Snellen's visual acuity on Titmus stereoacuity. Arch Ophthalmol. 1983;101:930–932. doi: 10.1001/archopht.1983.01040010930016. [DOI] [PubMed] [Google Scholar]
- 16.Goodwin RT, Romano PE. Stereoacuity degradation by experimental and real monocular and binocular amblyopia. Invest Ophthalmol Vis Sci. 1985;26:917–923. [PubMed] [Google Scholar]
- 17.Schmidt PP. Sensitivity of random dot stereoacuity and Snellen acuity to optical blur. Optometry & Vision Science. 1994;71:466–471. doi: 10.1097/00006324-199407000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Menon V, Bansal A, Prakash P. Randot stereoacuity at various binocular combinations of Snellen acuity. Indian J Ophthalmol. 1997;45:169–171. [PubMed] [Google Scholar]
- 19.Larson WL, Bolduc M. Effect of induced blur on visual acuity and stereoacuity. Optometry & Vision Science. 1991;68:294–298. doi: 10.1097/00006324-199104000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Nakagawa E, Ikebuchi J, Kusube T. Studies on the relationship between stereoscopic near vision and near vision by the use of Ryser's stepwise increasing occlusion filters. Japanese Orthoptic Journal. 1999;27:247–254. [Google Scholar]
- 21.Archer SM, Miller KK, Helveston EM, Ellis FD. Vergence amplitudes with random-dot stereograms. Br J Ophthalmol. 1986;70:718–723. doi: 10.1136/bjo.70.10.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simons K. Effects on stereopsis of monocular versus binocular degradation of image contrast. Invest Ophthalmol Vis Sci. 1984;25:987–989. [PubMed] [Google Scholar]
- 23.Halpern DL, Blake RR. How contrast affects stereoacuity. Perception. 1988;17:483–495. doi: 10.1068/p170483. [DOI] [PubMed] [Google Scholar]
- 24.Legge GE, Gu YC. Stereopsis and contrast. Vision Res. 1989;29:989–1004. doi: 10.1016/0042-6989(89)90114-4. [DOI] [PubMed] [Google Scholar]
- 25.Westheimer G, Pettet MW. Contrast and duration of exposure differentially affect vernier and stereoscopic acuity. Proceedings of the Royal Society of London - Series B: Biological Sciences. 1990;241:42–46. doi: 10.1098/rspb.1990.0063. [DOI] [PubMed] [Google Scholar]
- 26.Rohaly AM, Wilson HR. The effects of contrast on perceived depth and depth discrimination. Vision Res. 1999;39:9–18. doi: 10.1016/s0042-6989(98)00034-0. [DOI] [PubMed] [Google Scholar]
- 27.Laird PW, Hatt SR, Leske DA, Holmes JM. Distance stereoacuity in prism-induced convergence stress. J AAPOS. 2008;12:370–374. doi: 10.1016/j.jaapos.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drover JR, Felius J, Cheng CS, Morale SE, Wyatt L, Birch EE. Normative pediatric visual acuity using single surrounded HOTV optotypes on the electronic visual acuity tester following the amblyopia treatment study protocol. J AAPOS. 2007 doi: 10.1016/j.jaapos.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]