Although it is widely accepted that the doctor should allow the patient to speak freely at the start of the consultation, many doctors find it difficult not to interrupt, and tend to medicalise the patient’s presentation prematurely. To help overcome these tendencies we use a simple description of the consultation as consisting of three parts, according to who should be leading the dialogue at the time (Figure 1).1–3 The consultation begins with the ‘Patient’s part’, during which the patient has the freedom to express their pre-consultation experience (symptoms, problems) and thoughts (ideas, concerns, and expectations [ICE]). Next comes the ‘Doctor’s part’, when the doctor selectively gathers information relevant to the task of translating the patient’s narrative from ‘lay’ language into ‘medical’ constructs. Finally, in the ‘Shared part’, doctor and patient cooperate to arrive at plans and decisions acceptable to both of them.
Figure 1.
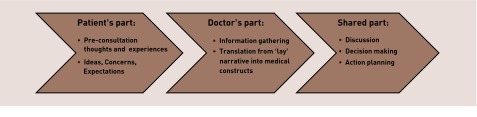
The three parts of the consultation.
The patient will usually open with a condensed account of what the consultation is about, often including cues to associated feelings and latent agenda. However, because of time pressure and our wish to find a medically solvable problem as quickly as possible, we are tempted to interrupt with questions about, for example, symptoms and duration: questions that belong in the Doctor’s part. This disrupts and distorts the prepared story, to which the patient will try to return having dealt with the interruption. Moreover, asking about the patient’s own thoughts and anxieties is often reduced to a few cursory and formulaic questions.
In studying nearly 3000 GPs’ video-recorded consultations in residential workshops over 20 years (www.kalymnos-kurser.dk), we have noticed that two patterns of behaviour frequently recur:
When the doctor clearly acknowledges what the patient has said by giving a verbal ‘receipt’, the patient listens and is prepared to let the doctor take the initiative; for example, ask the next question or steer the dialogue in a new direction.
When the doctor summarises some or all of the patient’s narrative, the patient again listens and, if the summary is accurate, will allow the doctor to take control of the consultation process.
The following is a simple guide, based on these observations, to help the doctor avoid closing down the Patient’s part prematurely. It confirms the truth of the apparent paradox that, by asking less at the start of the consultation, the doctor in fact discovers more.
FIVE CARDS
During the patient’s opening narrative it is best for you, the doctor, to concentrate on how the patient has interpreted the presenting problem and its implications, and not so much on the detail of symptoms. Imagine that the patient holds three kinds of ‘thoughts’ cards, that is, ICE cards (corresponding to that oft-cited triad), all of which need to be played during the telling of the story. Your task is to help the patient play all three ‘thoughts’ cards. To achieve this, you have two kinds of ‘response’ cards of your own in your hand: ‘receipt’ and ‘summary’ cards.
Each time you play a receipt or summary card, you create the opportunity to invite the patient to play a ‘thoughts’ card. In this way you can ensure that none of the patient’s cards is overlooked. If, for example, the patient does not play the ‘concerns’ card, and you do not ask, the burden of unshared anxiety will increase. If the ‘expectations’ card is not played, you may misinterpret what the patient wants from the consultation. If not all ‘ideas’ cards are played, it may later prove difficult genuinely to involve the patient in the Shared part of the consultation. When all three ‘thoughts’ cards have been played, you will have a good understanding of the patient’s illness experience, and a natural empathy will develop. During the Patient’s part, you will inevitably also be monitoring the narrative for medically-relevant information; but you should try to put this aside for now, to return to during the Doctor’s part.
THE ‘RECEIPT’ CARD
We cannot be sure we have been understood until the other person has replied. Giving the patient a receipt means showing, verbally and non-verbally, that you have recognised the importance of what you have heard. Receipts are remarks that indicate you are listening attentively and appreciatively, signal your acceptance, and encourage the telling of the patient’s prepared narrative: for example, ‘Thank you for telling me that — tell me more’; ‘That’s helpful, I’m glad you mentioned it’; ‘That must have been really upsetting’; ‘I can see that’s very worrying for you.’
Each time the patient discloses a significant aspect of the story, you should give a receipt in confirmation. You can then follow it up with a response which will prompt the playing of one of the patient’s ‘thoughts’ cards: for example, ‘What did you think was causing this?’ (ideas); ‘Was there anything in particular that worried you?’ (concerns); ‘How would you like me to help?’ (expectations).
A receipt needs to be clear and unambiguous. It is not enough merely to nod, or mumble ‘Mmm, right, OK’. The patient needs to be sure you are taking a real interest in the story. Acknowledgements such as ‘That was quite understandable’, or ‘I’m wondering what happened next’ help build a secure and trusting relationship. Even with a patient who starts out by asking for a sick note, prescription, or referral, you can give your receipt a positive twist: ‘It’s good you told me right away, so that I know what you came for.’
If the patient over-emphasises or exaggerates some aspect of the story, it is likely that you have not confirmed receipt in sufficiently explicit terms, or have failed to give a clear enough commitment to help. You might try with, ‘I’m glad you’ve come to see me about this’ or ‘I completely accept what you’re saying’, perhaps adding ‘... and I’ll certainly try to help you with this.’
If you find yourself becoming frustrated with a rambling or repetitious narrative, you have probably not given enough or sufficiently clear receipts to allow the patient to move on to the next significant feature. In this case a receipt such as ‘Yes, I quite understand that, and I will really try to help you’ will usually move things on and restore calm. It is not possible to play too many receipt cards! Giving receipts like this may at first feel somewhat forced; but with practice they become more elegant, and the benefits receipts bring to the consultation process will quickly come to outweigh their initial artificiality.
Sometimes when you give a receipt you may see that the patient, instead of looking expectantly for you to make the next move, turns his or her attention inwards into private and as yet unexpressed thoughts. This is a time for you to remain silent, or to ask ‘Would you like to tell me what you’re thinking?’
THE ‘SUMMARY’ CARD
Summarising is the ultimate evidence that you have understood what you have been told. Moreover, when you summarise, the patient switches from narrative to listening mode. Thus, when you conclude your summary with a question of your own or by signalling a change of topic, the patient will be ready to allow you to lead the dialogue at this point. Summarising gives you a chance to take the initiative.
Sometimes the patient’s story goes off on a tangent, or round in circles. When you start to feel overwhelmed or irritated, it is particularly helpful to play a summary card, and perhaps follow it up with an invitation to the patient to play the expectations card: ‘You’ve explained that your knee has been troublesome for several months. I’ll certainly try to help you and I wonder what help you would like.’ Such a response gets the patient’s attention and focuses discussion where you want it to be. Summarising also gives you the chance to ask, ‘Have I got the whole story now?’ or ‘Is there anything else you would like us to discuss today?’ Using a summary to secure the patient’s agreement of the agenda makes it easier for you to prioritise your time and plan the remainder of the consultation.
Each time you give a receipt or a summary it provides an opportunity for you to invite the patient to play another ‘thoughts’ card. It is important to develop a repertoire of follow-up questions which sound fresh and ‘tailored’ to the particular patient, rather than formulaic phrases like ‘What are your concerns?’ or ‘What do you expect me to do about it?’ Helping the patient to play these cards should be integral to an effective patient-centred consultation, not just a politically-correct ritual ICE-ing of the patient! Well-turned remarks such as ‘You have probably been thinking what it could be’; ‘Was there anything you were especially worried about?’ or ‘Were you hoping for any particular thing from coming to see me?’ are more likely to elicit what you need to know.
CONCLUDING THE PATIENT’S PART
Once you sense that the Patient’s part is almost done, it is a good idea to sum up what the patient has said and what you understand to be the goal of the consultation. You might, for instance, say, ‘So you’ve been worried about your periods becoming heavier, and you’d like to know if you’re reaching the menopause?’ When you hear (and see) the patient’s ‘Yes’, you know it is safe to move on to the Doctor’s part by continuing, ‘There are various questions I need to ask about your symptoms, and then I should like to examine you, please.’ The patient, reassured that you have understood the key features of the problem, will now be as helpful as possible to you in the Doctor’s part, and you will both be well prepared for the Shared part which will bring the consultation to a successful close.
Provenance
Freely submitted; externally peer reviewed.
REFERENCES
- 1.Larsen J-H, Risør O. The consultation process in general practice. Månedsskr Prakt Lægegern. 1994;72:319–330. [In Danish] [Google Scholar]
- 2.Larsen J-H, Risør O, Putnam S. P-R-A-C-T-I-C-A-L: a step-by-step model for conducting the consultation in general practice. Fam Pract. 1997;14:295–301. doi: 10.1093/fampra/14.4.295. [DOI] [PubMed] [Google Scholar]
- 3.Nystrup J, Larsen J-H, Risør O. Developing communication skills for the general practice consultation process. SQU Med J. 2010;10(3):318–325. [PMC free article] [PubMed] [Google Scholar]


