Abstract
Background
General practice is a common setting for the provision of weight-management advice, as well as the treatment of depression. While there is some evidence of a reciprocal relationship between obesity and depression, there are limited data about the rates of depression among general practice patients who are underweight, normal weight, overweight, and obese.
Aim
To explore the prevalence of depression among underweight, normal weight, overweight, and obese general practice patients.
Design and setting
A cross-sectional survey was conducted in 12 Australian general practices.
Method
Patients aged ≥18 years and older who were presenting for general practice care were eligible to participate. Consenting patients completed a touchscreen computer survey assessing self-reported weight and height. Depression was assessed by the Patient Health Questionnaire-9 (PHQ-9), with a score of ≥10 used to indicate possible depression.
Results
Data were obtained from 3361 participants. The prevalence of depression was 24% (95% confidence interval [CI] = 11.86 to 39.28) among underweight participants, 11% (95% CI = 8.5 to 14.0) among normal weight participants, 12% (95% CI = 0.9 to 15.2) among overweight participants, and 23% (95% CI = 17.8 to 29.0) among obese participants. The prevalence of depression was higher for women than for men across all weight categories except underweight.
Conclusion
Weight and depression demonstrated a U-shaped relationship, with higher prevalence of depression observed among underweight and obese general practice patients. These conditions may act as red flags for opportunistic screening of depression in the general practice setting.
Keywords: body weight, depression, general practice, obesity, primary care
INTRODUCTION
Depression and obesity are common, with an estimated 350 million and 500 million people globally with these respective conditions.1,2 Studies have consistently found a modest association between depression and obesity; however, the causal relationship is unclear. A meta-analysis of 17 community-based studies found that obese people were 1.18 times more likely to have depressive symptoms than those who were not obese, with this association more clearly present among women than men.3 Evidence of a reciprocal relationship between depression and excess weight was found in a meta-analysis of longitudinal studies.4 Overweight and obesity increased the odds of subsequent depression by 1.27 and 1.55 respectively, while depression increased the odds of obesity at follow-up by 1.58.4 This relationship has been suggested to be dose dependent, with a higher body mass index (BMI) being linked to a greater likelihood of clinical depression.4,5
Impact of comorbid depression and obesity
Depression and obesity are both associated with social stigma, low self-esteem, and chronic health conditions.6–9 When depression and obesity co-occur, the adverse health and social consequences are significant. Symptoms of depression in obese patients are strongly associated with poor quality of life, particularly social functioning, emotional roles, and mental health.10 Further, obesity coupled with depression has significant economic implications, owing to high service use11–13 and reduced participation in the labour force.14
GPs’ role in the detection and management of obesity and depression
In many countries, including Australia, the UK, and Canada, clinical practice guidelines recommend that GPs play a role in the management of both obesity and depression.15,16 Recent data from Australia’s Bettering the Evaluation and Care of Health (BEACH) study of GP encounters found that depression was the fifth most frequently managed problem, and weight and nutrition counselling was the most common preventative treatment administered.17 The frequency with which these conditions are encountered in primary care suggests that GPs may need to be equipped to recognise and provide comprehensive care to patients with comorbid depression and obesity.
Limited information of the prevalence of comorbid depression and obesity
While there are numerous community studies on depression and obesity,3,4 there are limited data on the prevalence of comorbid obesity and depression in the general practice setting. The frequency with which comorbid depression and obesity occur in general practice is important because of the implications for its detection and management. For example, some somatic criteria for the diagnosis of depression, such as sleep problems, fatigue, or changes in appetite, could be confounded with manifestations of obesity.6 While interventions for weight management, such as exercise, may also be helpful in managing depression, there are no protocols for providing integrated treatment of these health conditions. Therefore, if comorbid depression and obesity is a common presentation, the development and testing of models of care to facilitate GPs to recognise and treat these multiple conditions is likely to be indicated. This study aimed to examine the prevalence of depression among underweight, normal weight, overweight, and obese patients in general practice.
How this fits in
Previous research suggests a reciprocal relationship between depression and obesity; however, there has been limited study of the relationship between weight and depression in the Australian general practice setting. The results of this study indicate a U-shaped relationship exists between depression and weight, with a higher prevalence of depression observed among both underweight and obese patients. The findings suggest that these conditions may act as red flags for opportunistic screening of depression in the general practice setting.
METHOD
Design and setting
A cross-sectional survey was conducted among primary care patients in 12 practices in Australia. Sampling of practices has been described elsewhere.18
Participants
Patients presenting for a primary care appointment, aged ≥18 years, and who had sufficient English to complete the survey independently, were eligible to participate. Those presenting for a nursing or allied health appointment, or who were unable to provide independent informed consent were excluded.
Procedure
A research assistant sought informed consent from patients to participate in the study when they presented to the practice reception for their appointment. The sex of non-consenters was recorded, to assess consent bias. Consenting patients completed a 15-minute touchscreen computer survey while waiting for their appointment. Patients called into their appointment were able to exit the survey. The survey assessed a range of health risk factors and behaviours; however, only results relating to depression and obesity are presented here. Feedback on health risk factors identified within the survey was not provided to GPs.
Measures
Sociodemographic characteristics
Self-report data were obtained for age category (18–24 years, then in 5-year age categories to ≥70 years), sex, postcode, education, health insurance, and possession of a government Health Care Card or Veterans’ Affairs Card.
Medical history
Participants were asked to indicate whether they had ever been told by a doctor or nurse that they had depression. The number of times the participant consulted their GP in the last 12 months was also sought.
Body mass index
Participants were asked to report their weight to the nearest kilogram and their height to the nearest centimetre. BMI was calculated and World Health Organization (WHO) definitions applied to categorise underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (>30 kg/m2).19 BMI derived from self-reported weight and height has been shown to have adequate reliability when compared to BMI derived from measured values.20
Depression
The Patient Health Questionnaire (PHQ-9) was used to assess depression. This brief tool has been used extensively in the primary care setting.21 It is scored on a 27-point scale.22 A total score of ≥10 to classify depression is considered to provide the best balance between sensitivity (88%) and specificity (88%) compared to mental health professional assessment, and this cut-off value was used for this study.22
Data analyses
The proportions and modified Clopper–Pearson (exact) 95% confidence intervals (CIs, to account for clustering by practice) were calculated for each BMI category (underweight, normal weight, overweight, obese) for both depressed and non-depressed patients. The prevalence of depression across BMI categories was also calculated separately for men and women. For those who were identified as depressed, a χ2 test was undertaken, to compare the proportion who consulted their GP three or more times and the proportion reporting a previous history of depression, by BMI category. A Rao–Scott χ2 test was used to test whether the distribution of depressed patients was equal across all BMI categories.
RESULTS
Practice consent rate and characteristics
Of 48 practices approached to participate in the study, 12 (25%) consented. Eight practices had a practice nurse. The mean number of GPs employed within participating practices was 5 (range 3 to 15).
Patient consent rate and characteristics
Of 5667 patients screened for eligibility, 4705 were eligible and, of these, 4058 (86%) consented to participate. Comparison of the percentage of males among non-consenting patients with that among consenting patients found no significant differences between the two groups (χ2 = 0.13; degrees of freedom [df] = 1; P = 0.253). Participants with self-reported height greater than 240 cm and less than 120 cm, and weight greater than 250 kg and less than 30 kg were excluded from the analyses, as these values were perceived to be errors in self-report. This left a total of 3361 participants. As shown in Table 1, the majority of participants were female (61%) and had attended the practice on a previous occasion (94%). Twenty-two per cent were aged 70 years or older, and 25% reported one or more chronic medical conditions.
Table 1:
Demographic and medical characteristics of participants (n = 3361)
| Characteristic | n (%) |
|---|---|
| Sex (n = 3361) | |
| Male | 1305 (39) |
|
| |
| Age, years (n = 3361) | |
| 18–29 | 439 (13) |
| 30–39 | 464 (14) |
| 40–49 | 570 (17) |
| 50–59 | 587 (17) |
| 60–69 | 577 (17) |
| ≥70 | 724 (22) |
|
| |
| Education (n = 3120)a | |
| Primary | 49 (1.6) |
| Some high school | 239 (7.7) |
| Year 10 | 456 (15) |
| Completed high school | 533 (17) |
| Technical and further education/diploma | 535 (17) |
| University | 1003 (32) |
| Postgraduate | 220 (7.1) |
| Other | 85 (2.7) |
|
| |
| Visited clinic before? (n = 3151)a | |
| Yes | 2969 (94) |
|
| |
| Veterans’ Affairs Card (n = 3361) | 86 (2.6) |
|
| |
| Health Care Card (n = 3361) | 742 (22) |
|
| |
| Private healthcare insurance (n = 3361) | 1953 (58) |
|
| |
| Number of chronic conditions (n = 3361) | |
| None | 2534 (75) |
| 1–2 | 792 (24) |
| ≥3 | 35 (1.0) |
Number less than total participants, owing to missing data.
Prevalence of depression among underweight, normal weight, overweight, and obese participants
As shown in Table 2, the distribution of the prevalence of depression by weight category was U-shaped, with the highest rates observed among underweight and obese participants (24% and 23% respectively). The prevalence of depression was also remarkably similar among those of normal weight and those who were overweight (11% and 12% respectively). The rates of depression varied significantly by weight category (χ2 = 109.5; df = 3; P<0.0001).
Table 2:
Percentage of patients classified as depressed (PHQ-9≥10) by weight category
| Weight category | Not depressed (PHQ-9<10) n (%) [95% CI] | Depressed (PHQ-9 ≥10) n (%) [95% CI] | Total |
|---|---|---|---|
| Underweight | 68 (76) [60.72 to 88.14] | 21 (24) [11.86 to 39.28] | 89 |
| Normal weight | 1265 (89) [86.0 to 91.5] | 157 (11) [8.5 to 14.0] | 1422 |
| Overweight | 1035 (88) [84.8 to 91.1] | 138 (12) [8.9 to 15.2] | 1173 |
| Obese | 521 (77) [71.0 to 82.2] | 156 (23) [17.8 to 29.0] | 677 |
PHQ-9 = Patient Health Questionnaire.
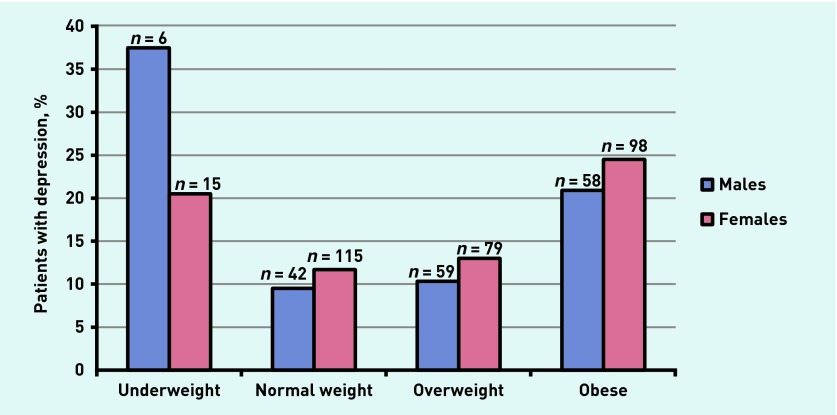
Depression among males and females, by BMI category
As shown in Figure 1, there was a higher percentage of females than males with depression in all BMI categories except for the underweight category. However, the prevalence of underweight among males was very low (n = 6, 1.2% of males).
Figure 1.
Percentage of males and females with depression, by BMI category.
Consulting behaviour and history of depression among people with depression, by BMI category
The number and proportion of patients with depression who reported a history of depression was calculated for the categories underweight (n = 10, 48%), normal weight (n = 92, 59%), overweight (n = 79, 57%), and obese (n = 109, 70%). There were no significant differences by weight category (χ2 = 6.97; df = 3; P = 0.0729). Similarly, there were no significant differences across weight categories for the proportion of depressed patients who reported three or more GP consultations within the past 12 months (χ2 = 2.02; df = 3; P = 0.5679). The number and proportion of responders with depression who had three more consultations within the past 12 months were: underweight (n = 13, 62%), normal weight (n = 108, 69%), overweight (n = 98, 71%), and obese (n = 112, 72%).
DISCUSSION
Summary
To the authors’ knowledge, this is one of the first studies to examine the prevalence of depression across all BMI categories in the Australian general practice setting. Depression and weight demonstrated a U-shaped relationship, with rates of depression higher among those who were underweight and among those who were obese. Depression was more prevalent among women across all BMI categories except underweight.
Strengths and limitations
The multi-site nature of the current study is a strength; however, the low practice consent rate raises the possibility that participating practices were not representative of the general practice setting. This is mitigated by a high participant consent rate, indicating that the sample was representative of participating practices.
The use of self-reported data on height and weight to calculate BMI may have resulted in an underestimation of BMI. However, the reliability of self-reported weight and height data collected for the current study were assessed with measured data collected for a subset of participants, and substantial agreement was found between self-report and measured categorisation of BMI.20 Given the low number of people reporting both underweight and depression in the current study, the results pertaining to this group must be treated with caution. The PHQ-9 has been shown to have high sensitivity and specificity in the general practice setting. However, it is a screening tool, and does not provide a clinical diagnosis of depression. Therefore, there is likely to be some degree of measurement error in the rates of depression reported for each BMI category.
Comparison with existing literature
While there are limited studies in the general practice setting, two large community-based studies conducted in the US and the Netherlands, involving 40 086 and 43 534 participants respectively, reported similar U-shaped associations between BMI and depression.23,24 Consistent with the current study, both studies used self-reported measures to collect data on height, weight, and depressive symptoms.
The point prevalence of depression among obese patients in the current study was 23% and is higher than the 14% reported in a previous study from one family practice clinic in the US.25 In the latter study, depression rates were based on a documented diagnosis of depression in the electronic medical record. The strong evidence that depression is under-detected in primary care26 is likely to account for the difference in prevalence reported. Past research sheds some light on the possible reasons for the high prevalence of depression among obese people. Factors associated with obesity, such as stigmatisation; discrimination in health care, education, and employment;27,28 low self-esteem; and body dissatisfaction,4,6 can contribute to or exacerbate depressive illness in an obese person.4 Conversely, features of depression may also cause or exacerbate weight problems and obesity. This includes prominent symptoms of depression, such as physical inactivity and weight gain, as well as weight gain attributed to antidepressant medication, major depressive episodes, or endocrine disturbance.4,8,29
Previous studies that have assessed the association between underweight and depression have focused specifically on individuals with eating disorders, which may not accurately reflect the general population of underweight individuals.30 Therefore, there are limited data with which to compare the present finding of a 24% prevalence rate for depression among underweight individuals. The few community studies that have examined the association between depression and underweight report inconsistent results.24,30 Depressive disorders are characterised by changes in eating behaviour, both overeating and under-eating, and weight changes, both significant weight gain and loss, and this is listed as a core diagnostic criterion according to the Diagnostic and statistical manual of mental disorders (DSM-5).31 While a decrease in food intake might be less common than an increase in food intake, these behaviours could partially explain the U-shaped association between depression and body weight.24
Rates of depression were higher among women than men across all BMI categories, except for the underweight category. However, it should be noted that only a small number of men were underweight (n = 6, 1.2%); therefore, these data must be interpreted with caution. An association between psychopathology and underweight among men has also been reported in community samples,23 suggesting that the current finding warrants further investigation.
Implications for research and practice
Given the paucity of prior research examining the prevalence of depression by BMI categories among general practice attendees, further research is needed to confirm the current findings and to determine the extent to which they can be generalised within the primary care setting in Australia and overseas. The data from this study indicated that rates of depression history among people with elevated PHQ-9 scores were similar across BMI categories. Similarly, there were no differences in the rate of depressed people who consulted their GP on three or more occasions in the past 12 months. Therefore, it would be useful for future research to investigate whether other factors may discriminate between those who are underweight and depressed and those who are obese and depressed. This may provide some insights into the impact of depression when associated with underweight or obesity, and assist in developing intervention approaches in this setting.
Both underweight and obesity may act a potential red flag for opportunistic screening for depression. The relatively high rates of depression among both underweight and obese participants in the present study suggest that these conditions may need to be addressed in combination. Given that both conditions are associated with stigma,27,28,32 GPs may be reluctant to raise issues of weight and/or depression with patients for whom this is not the primary reason for presenting for care.33 Therefore, exploration into the most effective ways of discussing the potential comorbidity of obesity and depression is needed.
In addition to aiding weight management,34 there is some evidence suggesting that exercise may improve mood.35 Therefore, exercise interventions integrated into depression treatment may be valuable among depressed patients who are underweight or obese. Similarly, depression screening and treatment may be beneficial alongside health-behaviour interventions for obesity. Despite their co-occurrence, there are no models for providing combined treatment for depression and obesity, and this is an important area for research. One of the key questions that remain unanswered is whether it is more effective to target these conditions simultaneously or sequentially. The importance of developing evidence-based approaches for tackling these two major health problems in an integrated way is highlighted by the present finding that almost one-quarter of those who were obese or underweight reported depression.
Funding
This work was supported by a grant from beyondblue and the National Heart Foundation of Australia Strategic Research Partnership [G 08S 4042].
Ethics approval
The study was approved by the Human Research Ethics Committees of the University of Newcastle, University of New South Wales, and Monash University (H-2009-0341).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: www.bjgp.org/letters
REFERENCES
- 1.World Health Organization . Depression. Fact sheet No. 369. Geneva: WHO; 2012. http://www.who.int/mediacentre/factsheets/fs369/en/index.html (accessed 9 January 2014). [Google Scholar]
- 2.World Health Organization . Obesity and overweight. Fact sheet No. 311. Geneva: WHO; 2013. http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed 9 January 2014). [Google Scholar]
- 3.de Wit L, Luppino F, van Straten A, et al. Depression and obesity: a meta-analysis of community-based studies. Psychiatry Res. 2010;178(2):230–235. doi: 10.1016/j.psychres.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 5.Onyike CU, Crum RM, Lee HB, et al. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158(12):1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 6.Markowitz S, Friedman MA, Arent SM. Understanding the relation between obesity and depression: causal mechanisms and implications for treatment. Clin Psychol (New York) 2008;15(1):1–20. [Google Scholar]
- 7.McNair BG, Highet NJ, Hickie IB, Davenport TA. Exploring the perspectives of people whose lives have been affected by depression. Med J Aust. 2002;176(10):S69. doi: 10.5694/j.1326-5377.2002.tb04507.x. [DOI] [PubMed] [Google Scholar]
- 8.Patten SB, Williams JV, Lavorato DH, et al. Major depression as a risk factor for chronic disease incidence: longitudinal analyses in a general population cohort. Gen Hosp Psychiatry. 2008;30(5):407–413. doi: 10.1016/j.genhosppsych.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009;190(7):S54. doi: 10.5694/j.1326-5377.2009.tb02471.x. [DOI] [PubMed] [Google Scholar]
- 10.Dixon JB, Dixon ME, O’Brien PE. Depression in association with severe obesity: changes with weight loss. Arch Intern Med. 2003;163(17):2058. doi: 10.1001/archinte.163.17.2058. [DOI] [PubMed] [Google Scholar]
- 11.Finkelstein EA, Ruhm CJ, Kosa KM. Economic causes and consequences of obesity. Annu Rev Public Health. 2005;26:239–257. doi: 10.1146/annurev.publhealth.26.021304.144628. [DOI] [PubMed] [Google Scholar]
- 12.Druss BG, Rosenheck RA. Patterns of health care costs associated with depression and substance abuse in a national sample. Psychiatr Serv. 1999;50:214–218. doi: 10.1176/ps.50.2.214. [DOI] [PubMed] [Google Scholar]
- 13.Baumeister H, Härter M. Mental disorders in patients with obesity in comparison with healthy probands. Int J Obes. 2007;31(7):1155–1164. doi: 10.1038/sj.ijo.0803556. [DOI] [PubMed] [Google Scholar]
- 14.Karakus MC, Okunade AA. Obesity with comorbid depression and early retirement. 2007. Jun, iHEA 2007 6th World Congress: Explorations in Health Economics Paper. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=992241 (accessed 22 January 2014).
- 15.National Institute for Health and Clinical Excellence . CG90 Depression in adults: the treatment and management of depression in adults. London: NICE; 2009. [Google Scholar]
- 16.The US Preventative Services Task Force Screening for depression in adults: US Preventive Service Task Force recommendation statement. USAHRQ Publication No. 10-05143-EF-05142US, December 2009. http://www.uspreventiveservicestaskforce.org/uspstf09/adultdepression/addeprrs.htm (accessed 9 January 2013).
- 17.Britt H, Miller GC, Henderson J, et al. General practice activity in Australia 2011–12. Sydney: University of Sydney; 2012. http://ses.library.usyd.edu.au/bitstream/2123/8675/4/9781743320198_ONLINE.pdf (accessed 9 January 2014). [Google Scholar]
- 18.Yoong SL, Carey ML, Sanson-Fisher RW, et al. Touch screen computer health assessment in Australian general practice patients: a cross-sectional study protocol. BMJ Open. 2012;2(4):pii: e001405. doi: 10.1136/bmjopen-2012-001405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization . BMI classification. Geneva: WHO; 2006. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html (accessed 9 January 2014). [Google Scholar]
- 20.Yoong SL, Carey ML, D’Este C, Sanson-Fisher RW. Agreement between self-reported and measured weight and height collected in general practice patients: a prospective study. BMC Med Res Methodol. 2013;13(1):38. doi: 10.1186/1471-2288-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22(11):1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90(2):251. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Wit LM, van Straten A, van Herten M, Penninx BW, Cuijpers P. Depression and body mass index, a U-shaped association. BMC Public Health. 2009;9(1):14. doi: 10.1186/1471-2458-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stecker T, Sparks S. Prevalence of obese patients in a primary care setting. Obesity. 2006;14(3):373–376. doi: 10.1038/oby.2006.49. [DOI] [PubMed] [Google Scholar]
- 26.Cepoiu M, McCusker J, Cole MG, et al. Recognition of depression by non-psychiatric physicians--a systematic literature review and meta-analysis. J Gen Intern Med. 2008;23(1):25–36. doi: 10.1007/s11606-007-0428-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav. 2005;46(3):244–259. doi: 10.1177/002214650504600303. [DOI] [PubMed] [Google Scholar]
- 28.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 29.Björntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2(2):73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 30.Kelly S, Daniel M, Dal Grande E, Taylor A. Mental ill-health across the continuum of body mass index. BMC Public Health. 2011;11(1):765. doi: 10.1186/1471-2458-11-765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: APA; 2013. Depressive disorders. [Google Scholar]
- 32.Griffiths KM, Christensen H, Jorm AF. Predictors of depression stigma. BMC Psychiatry. 2008;8(1):25. doi: 10.1186/1471-244X-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tham M, Young D. The role of the general practitioner in weight management in primary care – a cross sectional study in General Practice. BMC Fam Pract. 2008;9(1):66. doi: 10.1186/1471-2296-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shaw K, Gennat H, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006;4(4):CD003817. doi: 10.1002/14651858.CD003817.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cooney GM, Dwan K, Greig CA, et al. Exercise for depression. Cochrane Database Syst Rev. 2013;12(9):CD004366. doi: 10.1002/14651858.CD004366.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]