Clinical Question
How effective is video capsule endoscopy in investigating the small bowel compared to traditional investigations?
ADVANTAGES OVER EXISTING TECHNOLOGY
Video capsule endoscopy (VCE) was first developed in 1999 and has been in widespread use since the late 2000s. It is primarily used for investigation of the small bowel and has the advantage of being able to accurately examine the small bowel which cannot be easily reached by standard endoscopy methods. The major advantages are that it is non-invasive, safe, and convenient for the patient, and involves no ionising radiation. Additionally, VCE can provide some information on the rest of the gastrointestinal (GI) tract as well as basic information on small bowel transit time.
Previously the small bowel could only be imaged by contrast small bowel studies (for example, barium/gastrograffin) and more recently by cross-sectional imaging such as computed tomography (CT) and Magnetic resonance imaging (MRI). CT and contrast small bowel meal are relatively insensitive for examining the small bowel. Small bowel ultrasound, CT enterography/enterocolysis and MRI enterography/enterocolysis are readily available and can be performed to visualise the small bowel, but requires a radiologist with specialist experience for interpretation of the results. CT has the limitation of exposure to ionising radiation.
Available examinations to investigate the small bowel mucosa are by anterograde, that is, per oral push enteroscopy, single/double balloon enteroscopy, and retrograde, that is, per rectum ileoscopy, however, these are not widely available, invasive, and are technically challenging. However, these investigations do allow therapy such as the treatment of angiodysplasia and small lesion removal where necessary. They are generally reserved for cases where non-invasive investigation has confirmed an abnormality.
Disadvantages of VCE are that therapeutic work cannot be performed and biopsies cannot be obtained.
New developments in VCE have led to new capsules which can be used to examine the oesophagus and colon. They may be used for patients who do not tolerate upper/and/or lower gastrointestinal endoscopy. Also, reader software used for analysis has improved and newer capsules have increased battery lives with excellent lens resolution thus providing high definition images.
DETAILS OF TECHNOLOGY
Following an overnight fast, the patient swallows a small capsule measuring 26 mm × 11 mm and weighing 3.4 g (PillCam). It consists of a camera, light source, and a wireless circuit for the transmission of signals. As the capsule moves via peristalsis through the GI tract, images are transmitted to an external data recorder worn by the patient. The study usually lasts about 8 hours which is the lifespan of the battery. The data recorder is then connected to a computer and the images uploaded. These are then reviewed and analysed by a trained endoscopy reader. There are currently five types of VCE available in the UK:
PillCam® (Given Imaging Ltd, Israel). This was the original VCE which was approved by the US Food and Drug Administration (FDA) in 2001. It is a forward-viewing VCE which takes 2 frames per second. It features a ‘suspected blood indicator’ which may identify bleeding sites. The third generation of the capsule is about to be released. Almost all the available literature on VCE relates to PillCam.
EndoCapsule System EC-1® (Olympus, Japan). This technology is similar to the PillCam.
MiroCam® (IntroMedic, Korea). This is a forward-viewing VCE which takes three pictures per second. It has the widest angulation view and thus may enable more mucosa to be viewed and pathology to be identified.
OMOM (Chongqing Jinshan Science and Technology Group, China). This technology is similar to the PillCam.
CapsoCam SV-1® (CapsoVision, Medical Innovations, US). This is a novel 360 degree side-viewing VCE. It differs from previous VCEs in that no data recorders or sensors are needed. The images are stored on the VCE itself therefore the patient must retrieve the VCE themselves from their stool. This VCE is then sent to the endoscopy reader who analyses the data. It has a longer battery life of between 18–24 hours.
Top: PillCam® (Given Imaging Ltd, Israel) Middle: MiroCam® (IntroMedic, Korea) Bottom: CapsoCam SV-1® (CapsoVision, Medical Inovations, US).
PATIENT GROUP AND USE
Use is indicated for:
persistent unexplained iron deficiency anaemia (IDA);
obscure GI bleeding with previously negative upper and lower endoscopies;
assessment of small bowel lesions in known or suspected Crohn’s disease;
diagnosing and assessment of the small bowel in suspected coeliac disease;
screening and surveillance in familial polyposis syndromes; and
assessment and localisation of small-bowel tumours.
IMPORTANCE
Obscure GI bleeding accounts for approximately 5% of all overt GI bleeding cases1 and the source is commonly from the small bowel. It is the most frequent indication for small bowel VCE2 and can result in IDA. VCE should be performed after bidirectional endoscopy and after a repeat ‘second-look’ gastroscopy has failed to identify the source of bleeding.3
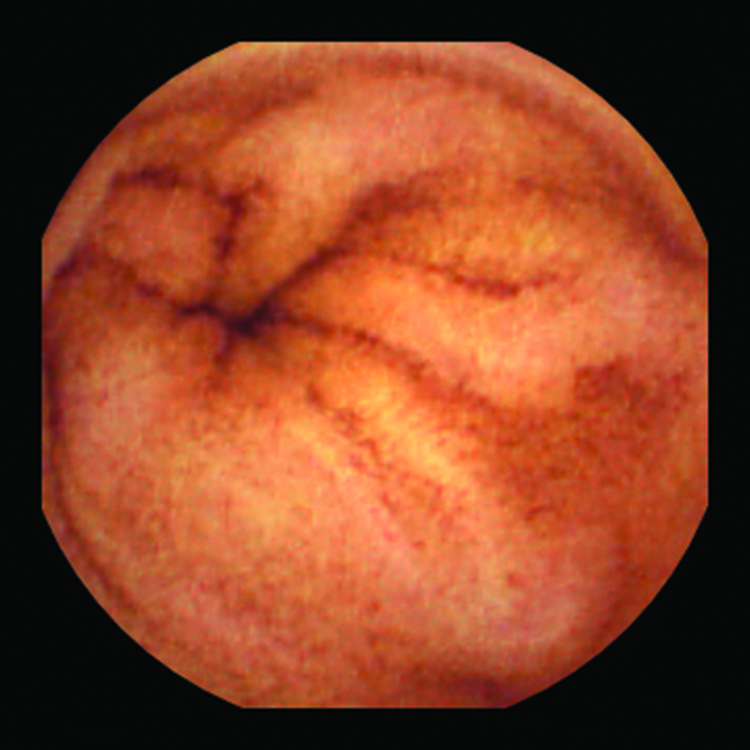
View of normal small bowel from video capsule.
Approximately 15% of the world’s population suffer from IDA.4 In the developed world, IDA occurs in 2–5% of adult men and postmenopausal women5 and this accounts for 4–13% of referrals to gastroenterology.6 The commonest cause is from menstrual losses in young women, however, blood loss from the GI tract is an important cause and current guidelines suggest that all men and postmenopausal women with IDA should undergo urgent endoscopic investigation.5 VCE is indicated when bidirectional endoscopy is negative and IDA persists despite adequate iron replenishment.5 Undetected and untreated, severe IDA can lead to fatigue, presyncope, and dyspnoea.
There are many possible causes of IDA or occult GI bleeding from the small bowel including: angiodysplasias, NSAID-associated ulceration, tumours, gastrointestinal stromal tumours, carcinoids, lymphoma, and Crohn’s disease.
PREVIOUS RESEARCH
Accuracy compared to existing technology
A meta-analysis has shown that complete imaging of the small bowel is achieved in 80% of VCE studies.7 Limitations include poor bowel preparation, slow gut transit, and undiagnosed strictures. The completion rate is almost 100% in second-look studies and once strictures have been excluded.
In the investigation of obscure GI bleeding, another meta-analysis has shown that VCE has a significantly greater diagnostic yield (63%) compared with push enteroscopy (23%).8 A study has also shown that VCE detected a bleeding source in 72% of patients, compared to 24% by CT angiography and 56% by standard angiography.9 Intraoperative enteroscopy is currently the gold standard for investigating obscure GI bleeding from the small bowel. In comparison, VCE has been shown to have a sensitivity, specificity, positive and negative predictive values of 95%, 75%, 95% and 86%, respectively.10
Impact compared to existing technology
VCE is now considered to be the first line test for investigating the small bowel. It is easy to perform, minimally invasive, and unlike previous radiological investigations, does not involve ionising radiation. Prior to the advent of VCE, investigation of the small bowel was incredibly challenging. Compared to other small bowel investigations, VCE remains the safest investigation of the small bowel.
The limitations and risks associated with VCE are small. The risk of VCE retention is under 1.5% but is higher in patients with Crohn’s disease (5–13%).11 Most retained capsules eventually pass spontaneously with no sequelae, but balloon enteroscopy or surgery may be necessary for VCEs persistently retained after 2 weeks.
The contraindications of VCE are:
presence of known intestinal strictures, fistulas, or obstruction;
small and/or young children;
patients with swallowing disorders (but VCEs can be easily placed with a gastroscope and biopsy forceps if necessary);
pregnancy (relatively contraindicated); and
concurrent MRI examination.
The limitations of VCE are:
missed lesions due to reader error or technical malfunction;
unable to obtain biopsies or perform therapeutic interventions;
the position of the capsule cannot be accurately controlled;
potentially obstructed views from inadequate bowel preparation; and
subjectivity of interpretation of images by the observer.
The ease of performing VCE in an ambulatory outpatient setting makes it an attractive investigation to be performed in primary care. Nurse endoscopists and GPs with a special interest in endoscopy may wish to provide a VCE service in primary care.
Cost-effectiveness and economic impact
The current cost of a single use capsule is in the region of £300.12
A cost-effectiveness analysis study was performed to explore the optimal strategy for investigating obscure GI bleeding. Five small bowel investigations were compared to a no therapy reference and the authors found that an initial double-balloon enteroscopy was the most cost-effective approach. However, due to the significant resources required and potential complications involved, it was concluded that VCE should be performed to guide subsequent treatment before invasive endoscopy.13
Another retrospective cost-effectiveness study found VCE to be a cost-saving approach in the evaluation of patients with obscure GI bleeding. The VCE diagnostic yield was compared to other imaging modalities and evaluated as a measure of efficacy. The mean cost of a positive diagnosis with VCE was €2091 compared with €3829 for other procedures. Therefore, one positive diagnosis by VCE provided a mean cost saving of €1738.14
Provenance
Freely submitted; externally peer reviewed.
Discuss this article
Contribute and read comments about this article: www.bjgp.org/letters
REFERENCES
- 1.Rockey DC. Occult and obscure gastrointestinal bleeding: causes and clinical management. Nat Rev Gastroenterol Hepatol. 2010;7(5):265–279. doi: 10.1038/nrgastro.2010.42. [DOI] [PubMed] [Google Scholar]
- 2.Ladas SD, Triantafylou K, Spada C, et al. European Society of Gastrointestinal Endoscopy (ESGE): recommendations (2009) on clinical use of video capsule endoscopy to investigate the small-bowel, esophageal and colonic disease. Endoscopy. 2010;42:220–227. doi: 10.1055/s-0029-1243968. [DOI] [PubMed] [Google Scholar]
- 3.Sidhu R, Sanders DS, Morris AJ, et al. Guidelines on small bowel enteroscopy and capsule endoscopy in adults. Gut. 2008;57:125–136. doi: 10.1136/gut.2007.129999. [DOI] [PubMed] [Google Scholar]
- 4.Pasricha SR, Drakesmith H, Black J, et al. Control of iron deficiency anaemia in low- and middle-income countries. Blood. 2013;121(14):2607–2617. doi: 10.1182/blood-2012-09-453522. [DOI] [PubMed] [Google Scholar]
- 5.Goddard A, James MW, McIntyre AS, et al. Guidelines for the management of iron deficiency anaemia. Gut. 2011;60:1309–1316. doi: 10.1136/gut.2010.228874. [DOI] [PubMed] [Google Scholar]
- 6.McIntyre AS, Long RG. Prospective survey of investigations in outpatients referred with iron deficiency anaemia. Gut. 1993;34:1102–1107. doi: 10.1136/gut.34.8.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rokkas T, Papaxoinis K, Triantafyllou K, et al. Does purgative preparation increase the diagnostic yield of small bowel video capsule endoscopy? A meta-analysis. Am J Gastroenterol. 2009;69:418–425. doi: 10.1038/ajg.2008.63. [DOI] [PubMed] [Google Scholar]
- 8.Triester SL, Leighton JA, Leontiadis GI, et al. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2005;100:2407–2418. doi: 10.1111/j.1572-0241.2005.00274.x. [DOI] [PubMed] [Google Scholar]
- 9.Saperas E, Dot J, Videla S, et al. Capsule endoscopy versus computed tomographic or standard angiography for the diagnosis of obscure gastrointestinal bleeding. Am J Gastroenterol. 2007;102:731–737. doi: 10.1111/j.1572-0241.2007.01058.x. [DOI] [PubMed] [Google Scholar]
- 10.Hartmann D, Schmidt H, Bolz G, et al. A prospective two-centre study comparing wireless capsule endoscopy with intraoperative enteroscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;61:826–832. doi: 10.1016/s0016-5107(05)00372-x. [DOI] [PubMed] [Google Scholar]
- 11.Chiefetz AS, Korenbluth AA, Legnani P, et al. The risk of retention of the capsule endoscope in patients with known or suspected Crohn’s disease. Am J Gastroenterol. 2006;101:954–964. doi: 10.1111/j.1572-0241.2006.00761.x. [DOI] [PubMed] [Google Scholar]
- 12.Sidhu R, Sanders DS, McAlindon ME. Gastrointestinal capsule endoscopy: from tertiary centres to primary care. BMJ. 2006;332:528–531. doi: 10.1136/bmj.332.7540.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerson L, Kamal A. Cost-effectiveness analysis of management strategies for obscure GI bleeding. Gastrointest Endosc. 2008;68(5):920–936. doi: 10.1016/j.gie.2008.01.035. [DOI] [PubMed] [Google Scholar]
- 14.Marmo R, Rotondano G, Rondonotti E, et al. Capsule enteroscopy vs. other diagnostic procedures in diagnosing obscure gastrointestinal bleeding: a cost-effectiveness study. Eur J Gastroenterol Hepatol. 2007;19(7):535–542. doi: 10.1097/MEG.0b013e32812144dd. [DOI] [PubMed] [Google Scholar]