Abstract
Objectives
Sleep is critical for adolescent health and is influenced by the family environment. In our study, we examined if family structure defined as single- vs 2-parent households affected adolescent sleep.
Methods
Participants were 242 (57% black; 47% boys) healthy adolescents (mean age, 15.7 years). Sleep was measured using self-report and wrist actigraphy over 7 consecutive nights. Outcomes were actigraphy-assessed sleep duration and sleep efficiency (SE) for the full week and weekends and weekdays separately, as well as self-reported sleep-wake problems and variability in bedtimes. Linear regression examined the relationship between family structure and sleep, after adjusting for age, sex, race, body mass index, and depressive symptoms, parental education, family conflict, and financial strain. Race and sex were examined as potential moderators.
Results
After adjusting for covariates, adolescents from single-parent households had poorer SE across the week and shorter sleep duration on weekends. White adolescents from 2-parent households had the fewer sleep-wake problems and lower bedtime variability, whereas black adolescents from single-parent households had the lowest weekend SE. There were no significant differences in family structure*sex interactions.
Conclusion
Our findings are the first to demonstrate that single-parent family structure is an independent correlate of sleep problems in adolescents, and they highlight the moderating role of race.
Keywords: sleep, family structure, marital status, single parent, adolescence, children, actigraph
1. Introduction
Sleep disturbances are highly prevalent among children and adolescents and are associated with a wide variety of adverse health outcomes, including increased risk for the development of depression [1], anxiety [2], and substance abuse [3], as well as physical health problems, such as obesity [4] and cardiovascular outcomes [5–7]. Among adults, single or divorced marital status is associated with an increased risk for sleep symptoms and clinically notable sleep disorders such as insomnia [8,9]. In a similar vein, several decades of research have shown that family structure most often defined by parental marital status also has profound effects on children’s mental and physical health, with an almost exclusive emphasis on waking life [10,11].
With 2 notable exceptions, few studies have investigated the association between family structure and children’s sleep. Among preschool-aged children, single-parent status was associated with less consistent parent-reported bedtime routines [12] and a greater likelihood of parent-reported sleep problems among children ages 8 to 9 years [13]. Taken together, these studies are consistent with the hypothesis that single-parent status may confer risk for parent-reported child sleep problems, at least in childhood, by influencing the timing and regularity of sleep. It is unknown if similar associations would be observed in adolescents. It also is unknown if these findings would extend to behavioral measures of sleep such as actigraphy, which reduce reporting bias and provide objective estimates of sleep quantity and efficiency (an indicator of sleep disruption). Therefore, the primary aim of our study was to examine the association between family structure (defined as single vs 2-parent households) and subjective and objective indicators of sleep in a sample of healthy adolescents.
Examining the relationship between family structure and sleep is particularly salient during adolescence, as this is a developmental period characterized by increasing autonomy from parents and an increasing importance of extra-familial social relationships in the context of dramatic biologically determined changes in sleep timing, architecture, and quality [14]. In turn, these changes in sleep put adolescents at increased risk for a host of sleep problems, including reduced sleep duration, increased risk for insomnia-related symptoms, and circadian phase delay [14,15]. These sleep problems often times represent the nonclinical range of symptoms characterized by disrupted, delayed, or irregular sleep patterns; however, they may portend increased risk for clinically notable sleep problems for some adolescents.
Adolescents from single-parent homes may have higher rates of sleep problems, due to feelings of insecurity about the stability of the home environment. As articulated by Dahl [16], insecurity in the home environment may heighten vigilance, which is antithetical to the sleep state. A small but growing literature also has demonstrated that family processes which are associated with family structure including family or parental marital conflict, and parental marital stability [17–19] are critical for the development of healthy sleep behaviors in infants and school-aged children. For instance, Gregory et al [20] found a modest but significant longitudinal association between family conflict and self-reported insomnia symptoms at the age of 18 years.
It also is possible that single-parent status serves as a proxy for other known risk factors for sleep problems that are known to covary with family structure. The vast majority of single-parent households in the United States are led by mothers, and black children are considerably more likely to grow up in single parent homes than their white counterparts [21]. Studies of the economic impact of divorce demonstrated that girls experienced a dramatic and disproportionate drop in income following marital dissolution relative to boys [22,23]. Concurrent with the substantial income decline, custodial mothers experienced increased psychosocial stress and financial strain from heavy workloads, high rates of job instability, and relocation to less desirable neighborhoods, with high crime rates, poor schools, and inadequate services [24]. Black race, lower parental education, and higher levels of financial strain are each in turn associated with higher increased rates of sleep problems in children and adults, as measured through self-report [25–28]. Therefore, it is important to determine if there is an independent association between family structure and adolescent sleep problems or if family structure is merely a proxy for these known risk factors.
Previous research on single parenthood and child and adolescent outcomes suggests that not only are there race differences in the likelihood of growing up in a single-parent home [29], but there also are race differences in the magnitude of the effects of single parenthood on child and adolescent outcomes [30]. For instance, several studies have shown that differences in adjustment in children from divorced and nondivorced families are less marked in black families than in white families [24,30,31]. Researchers have suggested that single parenthood may be less detrimental for black families, as black families more often are embedded within extended family networks than white families [32], which provides access to a broader set of parenting resources beyond that provided by traditional marriage. Consistent with these findings, we hypothesized that observed associations between family structure and adolescent sleep measures would be more pronounced in white adolescents than in black adolescents.
In summary, the purpose of our study was to examine the association between family structures and sleep problems during adolescence. We examined sleep using objective (i.e., actigraphy) and subjective sleep parameters that have previously been linked with waking health and functioning in adolescents and may be differentially related to family structure. Specifically, given our interest in examining subjective sleep problems associated with disrupted or delayed sleep schedules, we utilized a well-validated self-report instrument, which has been extensively used in adolescents and has previously been associated with adolescent risk-taking behavior. We also included actigraphy-assessed sleep efficiency (SE), which provided an objective measure of sleep fragmentation and sleep duration, as these sleep outcomes are most reliably associated with diverse health outcomes [7,33–35]. These sleep measures were evaluated according to school nights and weekend nights, in addition to the overall week. Finally, we assessed night-to-night variability in bedtimes (using sleep diaries), given that family structure may influence adolescents’ sleep habits through the influence of the regularity of daily routines (e.g., bedtimes). Recent evidence further suggests that variability in sleep timing is associated with a host of negative adolescent outcomes including truancy and substance use [36]. To determine the independent association between family structure and adolescent sleep, we adjusted analyses for variables known to covary with family structure or sleep. In particular, we examined if observed associations between family structure and sleep persisted after adjusting for adolescent age, sex, depressive symptoms, and body mass index, as well as parental education, family conflict, and financial strain. Recognizing the considerable variability in the effects of family structure on adolescent outcomes [29], we examined the degree to which adolescent race moderated any observed associations. Given previous reports of sex differences in adolescent sleep, we also explored the moderating role of sex. However, we made no a priori hypotheses concerning the moderating role of sex, given that previous research on sex differences in the effects of family structure on child and adolescent outcomes have yielded inconsistent findings [37,38].
2. Methods
2.1. Participants
A sample of 250 adolescents between the ages of 14 and 19 years were recruited from a single public high school near Pittsburgh, PA to participate in a study of stress, sleep, and cardiovascular risk factors. Start time for the school day was approximately 7:30 AM, which is consistent with data showing that the majority of high schools in the United States begin between 7:30 and 8:00 AM [39]. Approval of the research project was obtained from the school district superintendent, school principal, and the University of Pittsburgh Institutional Review Board. Participants or parents/legal guardians for students under the age of 18 years provided written informed consent prior to any research procedures. Exclusionary criteria were treatment of cardiovascular disease or diabetes mellitus; and medication use for emotional or psychologic disorders, blood pressure, or any medication known to affect the cardiovascular system or sleep. Our study included 242 participants who had complete data available for sleep assessments, demographic characteristics, and covariates.
2.2. Measures
2.2.1. Sleep
Actigraphy data were collected over a period of 7 consecutive days and nights using the Mini-Mitter actiwatch model AW-16 (Phillips Respironics, McMurray, PA). Actigraphy has been extensively validated as a measure of sleep-wake behavior in samples ranging from infants to older adults [40,41]. Actigraphs were configured to collect data over a 1-minute epoch. Stored data were downloaded into the Actiware software program (version 5.57) for processing and analysis. The medium threshold (default) was selected to detect nocturnal sleep periods that occurred within the time interval reported in the diary of time attempted to go to sleep and time awake (see below). Sleep onset was defined as having at least 10 minutes of sleep at the beginning of the sleep period when there was at least 3 hours of sleep, and sleep offset was defined as having at least 10 minutes of no sleep at the end of the sleep period. In addition, sleep periods occurring within 30 minutes of the major nocturnal sleep interval (either 30 minutes before sleeping or after waking) that were ≥15 minutes in duration were combined with the major sleep interval (i.e., if a 6-hour sleep interval was detected from 00:00–06:00 hours, and if a 20-min sleep interval was detected beginning at 23:30 PM the 20-minute interval was combined with the major sleep interval; the new major rest interval would become 23:30–06:00). All derived sleep variables were calculated from data within these set rest periods. The nights prior to vacation days during the school week were considered to be weekends, and Sunday night was considered to be a school night. Actigraphy collection occurred during the school year; school holidays (e.g., for teacher training) were considered to be weekends.
On average participants had 7.07 (standard deviation [SD], .60) days of actigraphy data collection (minimum, 4 nights; maximum, 10 nights). Previous research suggests that a minimum of 4 days of actigraphy is necessary to derive reliable actigraphy outcomes [42]. However, given the considerable variability in adolescent sleep patterns during the school week and on the weekends [36], we included actigraphy outcomes calculated for the full week and separately for weekdays and weekends. Using the maximum number of nights with valid actigraphy data, Cronbach α values were as follows: sleep duration for full week, weekdays, and weekends, respectively (α=.39, α=.52, and α=.35); and SE for full week, weekdays, and weekends, respectively (α=.76, α=.73, and α=.50). These differing reliability estimates are expected given the considerable night-to-night variability in sleep in general, and particularly with respect to adolescent sleep patterns during the school week and on the weekends.
Actigraphy outcomes were sleep duration calculated as the time spent asleep between initial sleep onset and final sleep offset, excluding periods of wakefulness throughout the night; and SE calculated as the percentage of total sleep time and time in bed. Bedtime variability defined as the standard deviation in diary-assessed time to try to sleep was collected over 7 days of daily diaries, in which participants reported bedtime for the previous night on their awakening.
The Sleep-Wake Behavior Problems subscale of the Sleep Habits Survey [43] was completed by adolescent self-report to address the participant’s tendency towards circadian phase delay and associated daytime consequences in the previous 2 weeks. This subscale consists of 10 items assessing the frequency of behaviors indicative of erratic or delayed sleep-wake patterns (e.g., arrived late to class due to oversleeping, stayed up later than 3:00 AM, had an extremely hard time falling asleep). The Sleep-Wake Behavior Problems subscale has demonstrated high internal reliability [43] and has previously been linked with health risk behaviors in adolescence [44].
2.2.2. Family structure and demographic information
Age, sex, and race were determined by adolescent report, whereas family structure was determined by interview of the parent or guardian. The majority of parent interviews were conducted by phone. Family structure was evaluated using a single item, which asked the parent or caregiver to indicate the marital or cohabitation status of the parents or caregivers in the child’s primary household. Response options included: single/never married, married, living as married, separated, widowed, or divorced. For our analyses, family structure was coded as a dichotomous variable (1=parents or guardians married or living together as married; 0=single-parent or guardian, which included single, divorced, separated, and widowed). Custodial parents’ years of education (higher of the 2 individuals, in case of 2-parent households) was provided by parents or guardians and were included as a covariate in all statistical models.
2.2.3 Body mass index
Height was measured using a stadiometer and weight was measured on a Tanita® digital scale. Body mass index (BMI) was calculated using the National Heart, Lung, and Blood Institute online calculator [45].
2.2.4. Family conflict
Three items from the Adolescent Life Events Scale [46] which assessed adolescents’ reports of arguments among adults in this house, many arguments with brothers and sisters, or many arguments with parents were used to assess family conflict. A summary score was computed of the sum of the family conflict items endorsed as somewhat unpleasant or very unpleasant.
2.2.5. Depressive symptoms
We used the Center for Epidemiologic Studies Depression Scale (CES-D) [47], which has been extensively validated as a measure of depressive symptoms. The sleep item from the CES-D was removed to avoid confounding with the sleep outcomes. Higher values are indicative of greater depressive symptoms.
2.2.6. Financial strain
The participants’ parent or guardian answered 2 questions evaluating the degree to which the family experienced difficulty not having enough money to make ends meet or worried about having enough money to pay for emergencies. These items were summed to create a financial strain measure. Based on the skewed distribution of the measure and as used in previous research [48], this measure was dichotomously coded, such that individuals endorsing financial strain of much of the time or always to either question were coded as 1, with those who reported financial strain never or once in a while in response to both questions coded as 0.
2.3. Analysis
Data were observed for normality and sleep measures were transformed as necessary using logarithmic or natural log transformations. We used t tests and χ2 tests to examine sample characteristics according to family structure. The primary analytic strategy employed hierarchical linear regression to examine the association between family structure on sleep outcomes, after adjusting for age, sex, race, BMI, depressive symptoms, highest level of parental education, family conflict, and financial strain. Next the race*family structure interaction term was entered into separate models for each sleep outcome with covariate adjustment to examine the degree to which family structure and sleep associations differed according to race. Preliminary analyses exploring if sex moderated any effects showed null effects and are not further discussed.
3. Results
Table 1 summarizes the sample characteristics for the total sample and analyzes according to family structure. The analytic sample was comprised of 242 adolescents (114 boys; 136 blacks). Of the total sample 60.7% were from single-parent households, with a significantly greater proportion of black adolescents from single-parent households than white adolescents. Consistent with previous reports [49] which have reported high rates of depressive symptoms in community-based samples of adolescents, depressive symptoms were in the moderate range of severity (mean CES-D, 15.4). On average adolescents were in the overweight range based on calculated BMI. There was no difference in family conflict or financial strain based on family structure. In unadjusted models adolescents from single-parent homes had significantly lower actigraphy-assessed SE (across the full week, weekdays, and weekends); shorter weekend sleep duration; and greater variability in bedtimes across the week (1 hour 24 minutes vs 1 hour 12 minutes on average across the week), as compared to adolescents from 2-parent households (Table 1). Mean SE (across the full week) was 83.7% for adolescents from 2-parent households and 82.1% for adolescents from single-parent families. There were no differences in sleep duration according to family structure across the 7 days of weekdays only (mean, 6 hours). However, sleep duration on weekends was significantly shorter for adolescents from single-parent households (mean, 7.2 [SD, 1.3]) compared to adolescents from 2-parent households (mean, 7.6 [SD, 1.2]).
Table 1.
Sample characteristics for the total sample and according to family structure.
| Family structure | ||||
|---|---|---|---|---|
| Variable | Total sample N=242 | Single-parent (n=147; 60.7%) | 2-parent (n=95; 39.3%) | |
| Mean±SD | P value for group difference | |||
| Age (y) | 15.7±1.3 | 15.8±1.3 | 15.7±1.3 | .55 |
| Depressive symptoms¥ | 15.4±8.7 | 15.4±8.6 | 15.4±9.0 | .80 |
| Family conflict | 1.4±1.4 | 1.3±1.1 | 1.5±1.1 | .20 |
| Body mass index | 26.2±5.9 | 26.0±5.8 | 26.6±6.1 | .46 |
| Sleep-wake problems | 23.2±6.1 | 23.7±6.5 | 22.4±5.4 | .09 |
| Variability in bedtimes (h) Actigraphy |
1.3±0.6 | 1.4±0.6 | 1.2±0.6 | .04 |
| 7-day sleep efficiency (%) | 82.7±4.9 | 82.1±5.0 | 83.7±4.5 | .01 |
| Weekday sleep efficiency (%) | 83.1±6.2 | 82.0±5.3 | 83.5±4.6 | .04 |
| Weekend sleep efficiency (%) | 82.6±5.1 | 82.4±6.5 | 84.1±5.5 | .03 |
| 7-day sleep duration (h) | 6.4±.8 | 6.4±.8 | 6.6±.8 | .06 |
| Weekday sleep duration (h) | 5.9±.9 | 5.9±.9 | 6.0±.9 | .58 |
| Weekend sleep duration (h) | 7.4±1.2 | 7.2±1.3 | 7.6±1.2 | .02 |
| N (%) | ||||
| Race | ||||
| Black | 136 (56.2%) | 94 (63.9%) | 42 (44.2%) | .003 |
| White | 106 (43.8%) | 53 (36.1%) | 53 (55.8%) | |
| Gender | ||||
| Girls | 128 (52.9%) | 82 (55.8%) | 46 (48.4%) | .29 |
| Boys | 114 (47.1%) | 65 (44.2%) | 49 (51.6%) | |
| Parents’ education‡ | ||||
| Higher than high school education | 34 (14.0%) | 26 (17.7%) | 8 (8.4%) | .12 |
| High school diploma | 110 (45.5%) | 65 (44.2%) | 45 (47.4%) | |
| Higher than high school education | 98 (40.5%) | 56 (38.1%) | 42 (44.2%) | |
| Financial strain | ||||
| Yes | 116 (48.1%) | 76 (65.5%) | 55 (44.0%) | .13 |
| No | 126 (51.9%) | 70 (56.0%) | 40 (34.5%) | |
Abbreviations: SD, standard deviation; y, years; h, hours.
Custodial parent’s education (higher of the 2 in 2-parent households).
Center for Epidemiologic Studies for Depression with sleep item was removed. For ease of interpretation, means and SDs for sleep outcomes are nontransformed values.
As shown in Table 2, there remained a significant association between family structure and SE persisted measured across the full week (β=1.48; ΔR2=.02; P<.05) after adjusting for age, sex, race, depressive symptoms, BMI, parental education, family conflict, and financial strain; and there was a marginal relationship between family structure and SE for weekdays only (β=1.33; ΔR2=.015; P=.05) and weekends only (β=1.6; ΔR2=.015; P=.05). There was a significant association between family structure and weekend sleep duration in the adjusted model (β=.37; ΔR2=.02; P<.05). There were no main effects of family structure on 7-day or weekday sleep duration, variability in bedtimes, or sleep-wake problems.
Table 2.
Hierarchical linear regression analyses of sleep outcomes on family structure and family structure by race interactions with covariate adjustment.
| 7-day sleep duration | WD sleep duration | WE sleep duration | 7-day sleep efficiency† | WD Sleep efficiency† | WE Sleep efficiency† | Bedtime variability† | Sleep- wake problems | |
|---|---|---|---|---|---|---|---|---|
| β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | |
| Model 1: | ||||||||
| Family structure | .14 (.10) | −.02 (.12) | .37* (.17) | 1.5* (.64) | 1.3 (.68) | 1.6 (.84) | −.06 (.04) | −1.4 (.79) |
| Model 2: | ||||||||
| Family structure | .14 (.10) | −.04 (.12) | .37* (.17) | 1.5* (.65) | 1.3 (.68) | 1.6 (.84) | −.06 (.03) | −1.5 (.77) |
| Family structure * race | .03 (.10) | .04 (.12) | .07 (.17) | −.51 (.65) | .16 (.68) | −1.8* (.83) | −07 (.03)* | −2.5*** (.78) |
Abbreviations: WD, weekday; WE, weekend; SE, standard error.
All models include the following covariates: adolescent age, sex, body mass index, depressive symptoms, financial strain, family conflict, and parental education.
Variables are transformed using logarithmic or natural logarithmic transformations prior to analysis.
P<.05;
P≤.01
P≤.001.
3.1. Moderating influence of race
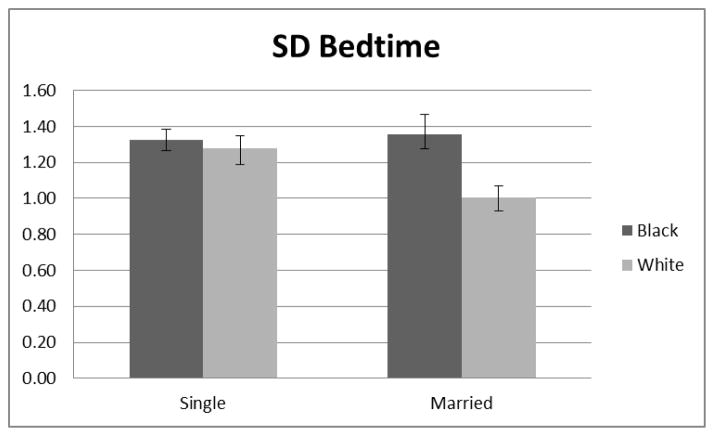
Analyses using the race*family structure interaction term revealed significant race differences in the effect of family structure on weekend sleep efficiency, bedtime variability, and sleep-wake problems (Table 2; model 2). Specifically, black adolescents from single-parent homes had the lowest weekend SE compared to all other groups (β=−1.8; ΔR2=.03; P<.05 [Fig. 1]). White adolescents from 2-parent households had lower bedtime variability compared to white adolescents from single-parent households, whereas there was no effect of family structure on bedtime variability for black adolescents (β=−.07; ΔR2=.03; P<.05 [Fig. 2]). In addition, white adolescents from 2-parent households had fewer sleep-wake problems than white adolescents from single-parent households; however, there were no differences in sleep-wake problems for black adolescents based on family structure (β=−2.5; ΔR2=.05; P<.001 [Fig. 3]).
Fig. 1.
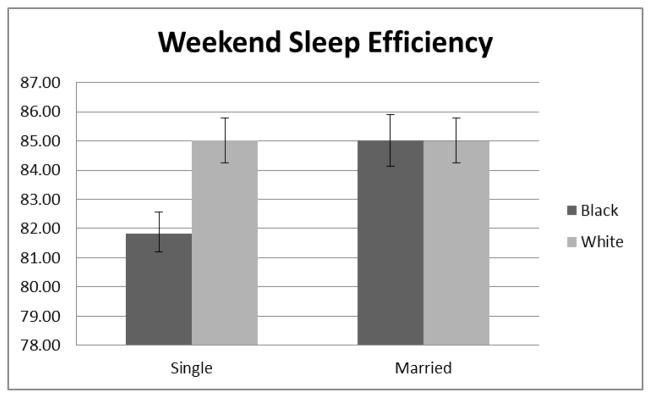
Family structure*race interaction on weekend sleep efficiency.
Fig. 2.
Family structure*race interaction on adolescent bedtime variability.
Fig. 3.
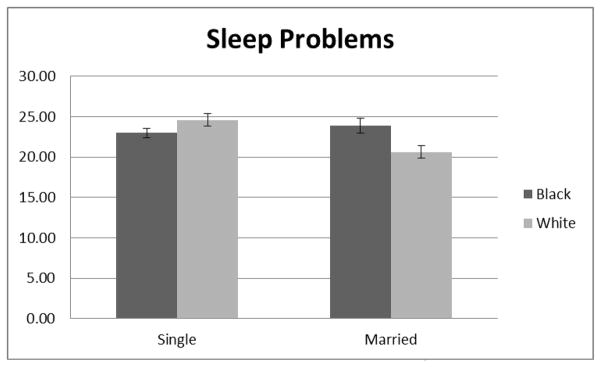
Family structure*race interaction on adolescent subjective sleep-wake problems.
4. Discussion
Family structure is a robust predictor of diverse mental and physical health outcomes across child development; however, previous literature has almost exclusively focused on waking behaviors. To our knowledge, our study is the first to examine family structure as a correlate of sleep problems in a community sample of black and white adolescents. In unadjusted models adolescents from single-parent households had lower actigraphy-assessed SE, greater variability in bedtimes, and shorter sleep duration on the weekends only compared to adolescents from 2-parent households. Follow-up models tested if family structure was merely a proxy for other known correlates of both family structure and sleep problems, including sociodemographic factors, depressive symptoms, family conflict, and financial strain. In the adjusted models, there remained a significant association between family structure and SE across the full week and weekend sleep duration. Findings for weekday and weekend SE were in the expected direction but attenuated to a trend-level finding (P=.06). These findings suggest that other unmeasured family characteristics or processes within single-parent households may contribute to observed associations. For instance, adolescents from single-parent households may be at greater risk for sleep problems due to decreased parental supervision or inconsistent family routines. Although our study did not measure these constructs, one previous study [50] found that adolescents from family environments characterized as being disorganized had higher rates of subjective sleep problems (e.g., prolonged sleep latency and daytime sleepiness); further, these effects were fully mediated by poor sleep hygiene practices including consistency of sleep-wake routines.
Consistent with previous literature suggesting considerable variability in the effects of family structure on adolescent adjustment, we found that race moderated the impact of family structure on several sleep problems. Specifically white adolescents from single-parent households had more sleep-wake problems than white adolescents from 2-parent households. However, there were no differences in sleep-wake problems according to family structure among black adolescents. These findings are consistent with previous data [51] suggesting weaker effects of family structure on black and Hispanic adolescents as compared to white adolescents. In contrast, black adolescents from single-parent homes had the lowest weekend SE compared to all other groups. However, these findings must be interpreted with caution, given that weekend estimates of sleep parameters are less reliable than estimates based on longer recording periods. Nevertheless, the results suggest the possibility that black adolescents from single-parent homes may have less of an opportunity to catch up on sleep on weekends, perhaps due to other competing obligations (e.g., household responsibilities, paid work outside of the home). Finally white adolescents from 2-parent households had lower bedtime variability compared to all other groups. These findings are consistent with previous work showing that black adolescents had shorter sleep on the weekends and later bedtimes compared to white adolescents [36]. Given that stable bedtime routines are a critical component of healthy sleep hygiene, stable bedtimes and bedtime routines may contribute to lower risk for sleep problems among white adolescents from 2-parent households. Importantly significant associations were observed after adjusting for known risk factors for adolescent sleep problems. In particular, previous evidence [1] revealed strong potentially bidirectional associations between sleep problems and depressive symptoms; that is, sleep problems can be both a cause and a correlate of depressive symptoms. The fact that reported associations were independent of depressive symptoms and demographic characteristics and were evidenced for both objective and subjective sleep outcomes suggests that the relationship between family structure and adolescent sleep problems is not solely attributable to depression or other known covariates. Importantly, however, the magnitude of the associations between family structure and sleep outcomes were small (approximately 2%–5% of variance), but they were comparable in magnitude to other known risk factors such as race, with an effect size of 4% in our sample.
Although our adjusted models provide a robust test of the independent association between family structure and adolescent sleep problems, several limitations of our covariate assessment, study design, and sample characteristics must be noted. Regarding measurement limitations, we characterized family structure according to single vs 2-parent households due to low statistical power to examine differences among specific subgroups of married/cohabiting or divorced/widowed/separated. Moreover, our study neither collected information on other relationship characteristics which may be relevant to adolescent sleep including the length or quality of the parents’ marital or cohabiting relationships, nor did it assess noncohabiting parental relationships. Similarly our assessment of family conflict was limited to a 3-item measure, which may have reduced the reliability of this construct.
Further research is needed using more comprehensive assessments of other family factors in more socioeconomically diverse populations to identify if single-parent status is itself a risk factor for sleep problems or if it is a proxy for other risk factors that covary with single-parent households. In particular, stable social rhythms for the regularity and predictability of daily routines known to influence sleep have been shown to act as a protective factor for adolescent outcomes from high-risk families (e.g., alcoholic parent) [41] and may be a critical pathway through which family structure influences the variability in adolescent bedtimes and the quality of sleep. However, the cross-sectional design of our study limits our ability to examine potential mediating pathways in a causal framework. Longitudinal studies better suited to identify the processes underlying links between family structure and adolescent sleep may elucidate novel intervention efforts to reduce the risk for adolescent sleep problems and improve adolescent health and well-being.
Several characteristics of our sample also must be considered when interpreting the results. Although our sample was comprised of healthy adolescents without any known psychiatric, sleep, or metabolic disorders, who were free of medications that might have influenced sleep-wake function, the sample was drawn from a single high school comprised of predominantly low to middle income families Thus these results may not generalize to all adolescents. Across the sample, sleep duration was considerably lower than the optimal 9 hours of sleep recommended for adolescents, and rates of depressive symptoms also were high. However, these findings are consistent with other recent studies documenting high rates of insufficient sleep among adolescents [52] and high rates of depressive symptoms in community-based samples of adolescents [53]. Finally rates of overweight and obese adolescents were higher in our sample than in the national average; however, they are consistent with national data in predominantly black populations [54]. As in all novel findings, replication of our results is needed reflecting diverse adolescent populations.
Strengths of our study include the relatively large community-based sample of black and white adolescents; the comprehensive assessment of sleep-wake problems using actigraphy and a well-validated adolescent sleep instrument; and the conservative analytic approach, which examined the independent association between family structure and adolescent sleep problems after adjusting for relevant covariates. Focus on a single high school has the advantage of a similar school culture across a range of racial and socioeconomic groups.
5. Conclusion
Our findings provide preliminary evidence which highlights the importance of considering family structure and family functioning as potential risk factors for sleep problems in adolescence. Moreover, our findings extend the previous literature examining race as a moderator of the effects of family structure on key adolescent outcomes. Understanding the links between family factors and sleep may elucidate a key underinvestigated pathway through which family environments influence adolescent health and well-being, during both day and night.
Highlights.
Sleep problems are highly prevalent in adolescence.
Family factors are important for child and adolescent sleep.
Adolescents from single-parent households had poorer sleep efficiency.
Race moderated the effects of family structure on sleep.
Acknowledgments
Funding sources
Support for our study was provided by the National Heart Lung Blood Institute (HL25767; PI: Matthews). Support for the first author (WMT) was provided by an Early Career Award from NHLBI (HL093220). The National Institutes of Health and NHLBI specifically disclaim responsibility for any analyses, interpretations, or conclusions. Dr. Karen A. Matthews had full access to the data and takes responsibility for the integrity of the data and accuracy of the analysis.
Footnotes
Conflict of interest
The authors report no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ivanenko A, McLaughlin Crabtree V, et al. Sleep and depression in children and adolescents. Sleep Med Rev. 2005;9:115–29. doi: 10.1016/j.smrv.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Alfano CA, Zakem AH, Costa NM, et al. Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depress Anxiety. 2009;26:503–12. doi: 10.1002/da.20443. [DOI] [PubMed] [Google Scholar]
- 3.Gromov L, Gromov D. Sleep and substance use and abuse in adolescents. Child Adolesc Psychiatr Clin N Am. 2009;18:929–46. doi: 10.1016/j.chc.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell JA, Rodriguez D, Schmitz KH, et al. Sleep duration and adolescent obesity. Pediatrics. 2013;131:e1428–34. doi: 10.1542/peds.2012-2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Javaheri S, Storfer-Isser A, Rosen CL, et al. Sleep quality and elevated blood pressure in adolescents. Circulation. 2008;118:1034–40. doi: 10.1161/CIRCULATIONAHA.108.766410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Javaheri S, Storfer-Isser A, Rosen CL, et al. Association of short and long sleep durations with insulin sensitivity in adolescents. J Pediatr. 2011;158:617–23. doi: 10.1016/j.jpeds.2010.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mezick EJ, Hall M, Matthews KA. Sleep duration and ambulatory blood pressure in black and white adolescents. Hypertension. 2012;59:747–52. doi: 10.1161/HYPERTENSIONAHA.111.184770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11:470–8. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Troxel WM, Buysse DJ, Matthews KA, et al. Marital/cohabitation status and history in relation to sleep in midlife women. Sleep. 2010;33:973–81. doi: 10.1093/sleep/33.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amato PR. Children of divorce in the 1990s: An update of the Amato and Keith (1991) meta-analysis. J Fam Psychol. 2001;15:355–70. doi: 10.1037//0893-3200.15.3.355. [DOI] [PubMed] [Google Scholar]
- 11.Troxel WM, Matthews KA. What are the costs of marital conflict and dissolution to children’s physical health? Clin Child Fam Psychol Rev. 2004;7:29–57. doi: 10.1023/b:ccfp.0000020191.73542.b0. [DOI] [PubMed] [Google Scholar]
- 12.Hale L, Berger LM, LeBourgeois MK, et al. Social and demographic predictors of preschoolers’ bedtime routines. J Dev Behav Pediatr. 2009;30:394–402. doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paavonen EJ, Aronen ET, Moilanen I, et al. Sleep problems of school-aged children: A complementary view. Acta Paediatr. 2000;89:223–8. doi: 10.1080/080352500750028870. [DOI] [PubMed] [Google Scholar]
- 14.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31:175–84. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 15.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the national comorbidity survey replication—adolescent supplement (ncs-a) J Am Acad Child Adolesc Psychiatry. 2010;49:980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahl RE. The regulation of sleep and arousal: development and psychopathology. Dev Psychopathol. 1996;8:3–27. [Google Scholar]
- 17.Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: A pilot study. J Fam Psychol. 2007;21:67–73. doi: 10.1037/0893-3200.21.1.67. [DOI] [PubMed] [Google Scholar]
- 18.Kelly RJ, El-Sheikh M. Marital conflict and children’s sleep: reciprocal relations and socioeconomic effects. J Fam Psychol. 2011;25:412–22. doi: 10.1037/a0023789. [DOI] [PubMed] [Google Scholar]
- 19.Mannering AM, Harold GT, Leve LD, et al. Longitudinal associations between marital instability and child sleep problems across infancy and toddlerhood in adoptive families. Child Dev. 2011;82:1252–66. doi: 10.1111/j.1467-8624.2011.01594.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gregory AM, Caspi A, Moffitt TE, et al. Family conflict in childhood: a predictor of later insomnia. Sleep. 2006;29:1063–7. doi: 10.1093/sleep/29.8.1063. [DOI] [PubMed] [Google Scholar]
- 21.Vespa J, Lewis JM, Kreider RM US Department of Commerce. [Accessed December 16, 2013];United states census: American Families and Living Arrangements. 2012 http://www.census.gov/prod/2013pubs/p20-570.pdf. Published August 2013.
- 22.Gadalla TM. Impact of marital dissolution on men’s and women’s incomes: a longitudinal study. J Divorce Remarriage. 2008;50:55–65. [Google Scholar]
- 23.Bianchi SM, Subaiya L, Kahn JR. The gender gap in the economic well-being of nonresident fathers and custodial mothers. Demography. 1999;36:195–203. [PubMed] [Google Scholar]
- 24.McLanahan S, Sandefur G. Growing up With a Single Parent: What Hurts, What Helps. Cambridge, MA: Harvard University Press; 1994. [Google Scholar]
- 25.Boe T, Hysing M, Stormark KM, et al. Sleep problems as a mediator of the association between parental education levels, perceived family economy and poor mental health in children. J Psychosom Res. 2012;73:430–6. doi: 10.1016/j.jpsychores.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 26.Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents [published online ahead of print June 3, 2013] Health Psychol. 2013 doi: 10.1037/a0032924. No Pagination Specified. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: the Swan Sleep Study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- 28.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amato PR. Research on divorce: continuing trends and new developments. J Marriage Fam. 2010;72:650–66. [Google Scholar]
- 30.Dunifon R, Kowaleski-Jones L. Who’s in the house? race differences in cohabitation, single parenthood, and child development. Child Dev. 2002;73:1249–64. doi: 10.1111/1467-8624.00470. [DOI] [PubMed] [Google Scholar]
- 31.Shaw DS, Winslow EB, Flanagan C. A prospective study of the effects of marital status and family relations on young children’s adjustment among African American and European American families. Child Dev. 1999;70:742–55. doi: 10.1111/1467-8624.00053. [DOI] [PubMed] [Google Scholar]
- 32.McLoyd VC, Harper CI, Copeland NL. Ethnic Minority Status, Interparental Conflict, and Child Adjustment. Cambridge, MA: Cambridge University Press; 2001. [Google Scholar]
- 33.American Academy of Pediatrics. Council on Child and Adolescent Health. The role of home-visitation programs in improving health outcomes for children and families. Pediatrics. 1998;101:486–9. doi: 10.1542/peds.101.3.486. [DOI] [PubMed] [Google Scholar]
- 34.Gupta NK, Mueller WH, Chan W, et al. Is obesity associated with poor sleep quality in adolescents? Am J of Hum Biol. 2002;14:762–8. doi: 10.1002/ajhb.10093. [DOI] [PubMed] [Google Scholar]
- 35.de Jonge L, Zhao X, Mattingly MS, et al. Poor sleep quality and sleep apnea are associated with higher resting energy expenditure in obese individuals with short sleep duration [published online ahead of print June 11, 2012] J Clin Endocrinol Metab. 2012;97:2881–9. doi: 10.1210/jc.2011-2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pasch KE, Laska MN, Lytle LA, et al. Adolescent sleep, risk behaviors, and depressive symptoms: Are they linked? Am J Health Behav. 2010;34:237–48. doi: 10.5993/ajhb.34.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aro HM, Palosaari UK. Parental divorce, adolescence and transition to adulthood. Am J Orthopsychiat. 1992;62:421–9. doi: 10.1037/h0079342. [DOI] [PubMed] [Google Scholar]
- 38.de Goede M, Spruijt E. Effects of parental divorce and youth unemployment on adolescent health. Patient Educ Couns. 1996;29:269–76. doi: 10.1016/s0738-3991(96)00924-x. [DOI] [PubMed] [Google Scholar]
- 39.Wolfson AR, Carskadon MA. A survey of factors influencing high school start times. NASSP Bull. 2005;89:47–66. [Google Scholar]
- 40.Ancoli-Israel S, Cole R, Alessi C, et al. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–92. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- 41.Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011;15:259–67. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 42.Acebo C, Sadeh A, Seifer R, et al. Estimating sleep patterns with activity monitoring in children and adolescents: how many nights are necessary for reliable measures? Sleep. 1999;22:95–103. doi: 10.1093/sleep/22.1.95. [DOI] [PubMed] [Google Scholar]
- 43.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 44.O’Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behav Sleep Med. 2005;3:113–33. doi: 10.1207/s15402010bsm0303_1. [DOI] [PubMed] [Google Scholar]
- 45.National Heart, Lung, and Blood Institute. Calculate Your Body Mass Index. http://www.nhlbi.nih.gov/guidelines/obesity/BMI/bmicalc.htm. Published 2013.
- 46.Masten AS, Neemann J, Andenas S. Life events and adjustment in adolescents: the significance of event independence, desirability, and chronicity. J Res Adolesc. 1994;4:71–97. [Google Scholar]
- 47.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psych Meas. 1977;1:385–401. [Google Scholar]
- 48.Puterman E, Adler N, Matthews KA, et al. Financial strain and impaired fasting glucose: the moderating role of physical activity in the coronary artery risk development in young adults study. Psychosom Med. 2012;74:187–92. doi: 10.1097/PSY.0b013e3182448d74. [DOI] [PubMed] [Google Scholar]
- 49.Roberts RE, Lewinsohn PM, Seeley JR. Symptoms of DSM-III-R major depression in adolescence: evidence from an epidemiological survey. J Am Acad Child Adolesc Psychiatry. 1995;34:1608–17. doi: 10.1097/00004583-199512000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Billows M, Gradisar M, Dohnt H, et al. Family disorganization, sleep hygiene, and adolescent sleep disturbance. J Clin Child Adolesc. 2009;38:745–52. doi: 10.1080/15374410903103635. [DOI] [PubMed] [Google Scholar]
- 51.Heard HE. The family structure trajectory and adolescent school performance: differential effects by race and ethnicity. J Fam Issues. 2007;28:319–54. [Google Scholar]
- 52.Fredriksen K, Rhodes J, Reddy R, et al. Sleepless in Chicago: tracking the effects of adolescent sleep loss during the middle school years. Child Dev. 2004;75:84–95. doi: 10.1111/j.1467-8624.2004.00655.x. [DOI] [PubMed] [Google Scholar]
- 53.Roberts RE, Andrews JA, Lewinsohn PM, et al. Assessment of depression in adolescents using the center for epidemiologic studies depression scale. Psychol Assess. 1990;2:122–8. [Google Scholar]
- 54.Ogden CL, Flegal KM, Carroll MD, et al. Prevalence and trends in overweight among us children and adolescents. JAMA. 2002;288:1728–32. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]