Abstract
Campylobacter is the most common bacterial food-borne pathogen worldwide. Poultry and specifically chicken and raw chicken meat is the main source for human Campylobacter infection. Whilst being colonized by Campylobacter spp. chicken in contrast to human, do scarcely develop pathological lesions. The immune mechanisms controlling Campylobacter colonization and infection in chickens are still not clear. Previous studies and our investigations indicate that the ability to colonize the chicken varies significantly not only between Campylobacter strains but also depending on the original source of the infecting isolate.
The data provides circumstantial evidence that early immune mechanisms in the gut may play an important role in the fate of Campylobacter in the host.
Keywords: Campylobacter jejuni, chicken, colonization pattern, cytokines, T-cells
Introduction
Campylobacter spp. are curved or spiral shaped flagellated bacteria with a size of 0.2–0.5 μm length and a width of 0.2–0.9 μm. They are gram-negative, and so far 25 species and 8 sub-species have been described [1, 2]. Among these species, some show strict host specificity such as Campylobacter (C.) rectus for man or C. mucosalis for pig. Within the family Campylobacteriaceae, some species such as C. jejuni subsp. jejuni or C. coli are linked to more than one host and have zoonotic potential in avian species. C. jejuni is most commonly detected specifically in poultry, but C. coli and C. lari also occur regularly in birds. Particularly, C. coli shows a prevalence of almost 50% in turkeys [1, 3].
Thermophilic (37–42 °C) and non-thermophilic Campylobacter species (< 37 °C) can be differentiated. Different from other intestinal bacteria such as Salmonella, Campylobacter grows only under microaerophilic conditions in an atmosphere with 10% CO2, 5% O2 and 85% hydrogen [4, 5].
C. jejuni is the most frequent cause for human enteritis worldwide. It appears more frequently than other bacterial pathogens such as pathogenic Escherichia coli or Salmonella spp. [6, 7]. In Europe, C. jejuni is the most common food-borne pathogen with an incidence of 19.4 cases/100 people/year in England for example [6]. Campylobacter infection causes in humans acute gastrointestinal illness and is considered to be a predisposing factor for the Guil-lain-Barre syndrome [8, 9]. The disease is characterized by a watery or bloody diarrhoea, fever and abdominal cramps. In most cases it is self-limiting but may also sustain for several weeks [7].
Poultry and poultry meat is considered to be one of the major sources for human campylobacteriosis [1, 10, 11]. Beside poultry and raw poultry meat other sources for C. jejuni have been described such as livestock, including sheep and pigs, but also cats and dogs, water, humans and vehicles, raw milk, rodents and insects are known as possible vectors [12–16]. These different sources are not only involved in the horizontal transmission of Campylobacter to humans but also to poultry flocks.
Due to the fact that C. jejuni is found ubiquitous it is difficult to control spreading and the introduction of C. jejuni into poultry flocks. Campylobacter spp. colonized flocks are common and can be found in many countries worldwide [17]. However, Scandinavian countries show a lower prevalence than other European countries [18]. This difference may be due to improved hygiene barriers [19]. Although found ubiquitous, Campylobacter shows a low tenacity being highly sensitive to oxygen, desiccation, low pH and high temperature [20].
Campylobacter in poultry
Birds, and especially chickens are considered as the natural host of C. jejuni [21]. However, C. jejuni is regarded as a commensal of the intestinal flora of chickens, which leads to a predominantly asymptomatic colonisation of the gut, particularly the caecum [22–25]. Beside the lower intestine being the main reservoir, Campylobacter may be detected in several internal organs such as liver and spleen [26]. Both meat and laying type chickens are colonized. C. jejuni can be also found in other poultry species such as turkeys, Muscovy and Pekin ducks. Beside poultry, a vast variety of wild birds, such as gulls, corvids, waterfowl and passerines are also susceptible for Campylobacter and may act as vectors for transmission especially to poultry flocks [27–29]. The uptake of the pathogen by poultry species from the environment usually occurs between the age of two to four weeks [30, 31]. Maternal antibodies seem to have an influence on the onset of colonisation. But also birds younger then three weeks can be colonized successfully in the case of high environmental exposure [32].
Horizontal transmission within the flock occurs predominantly via shedding birds and contaminated litter. Feed and water may be sources of recurring infections. There is no vertical transmission [33]. The C. jejuni-prevalence within a flock is almost 100% after introduction [31, 34]. Furthermore, multi-strain colonisation is possible within one flock. A recent study concerning a field trial with nineteen poultry flocks of four avian species revealed a large genetic diversity of Campylobacter within individual flocks and among different flocks using amplified fragment length polymorphism (AFLP) analysis [34]. Petersen et al. [35] also showed coexistence of different Camplyobacter clones in broiler flocks. These results raise the question of the colonisation potential of different Campylobacter strains of different origin not only for human but also for poultry.
In a recent study we tested C. jejuni isolates of human and avian origin for their ability to colonize chicken, replicate in different organs and induce lesions. So far, we compared a total of seven C. jejuni isolates, including four Campylobacter of human and three of avian origin.
Three weeks old specific-pathogen free pullets confirmed to be negative of Campylobacter at the day of inoculation, were inoculated orally with 104 colony-forming units of C. jejuni. Afterwards, the birds were monitored daily for clinical signs, and on selected days for weight gain and the number of colony forming units per gram caecal content and liver.
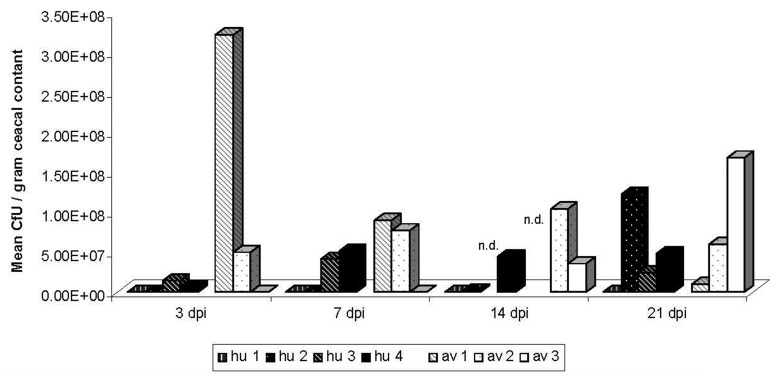
There was a clear difference in the ability of the strains to colonize the chicken gut and liver [34]. While one human isolate was not detectable by the applied cultivation method at any of the investigated time points up to two weeks post inoculation, all other strains colonized the chicken gut (Fig. 1). A possible reason for different Campylobacter colonisation patterns may be genetic diversity of C. jejuni isolates [36, 37]. Only one strain of avian origin showed the ability to also invade the liver (data not shown). This observation supports previous studies demonstrating low detection rates of Campylobacter in liver samples, too [26, 34, 38]. Furthermore, based on the comparison of the colonisation efficiency of C. jejuni and of C. coli Korolik et al. [37] suggests that Campylobacter strains of human origin may lack or lost the ability to colonize the chicken intestine.
Fig. 1.
Mean Colony forming Units (CfU) per gram caecal content in chickens after different days of inoculation with human (hu 1–hu 4) and avian (av 1–av 3) C. jejnui isolates. n = six animals/day and group in each of the four experiments. For determination, caecal content was serially diluted and plated on selective agar (CCDA) for 48 h at 38 °C under microaerophilic conditions [63]. dpi = days post inoculation. n.d. = not done
In our experiment, all inoculated birds independent of the inoculated Campylobacter strain were free of clinical signs, pathological or histopathological lesions such as crypt abscesses, epithelial cell ballooning, basal subnuclear vacuolation or villous tip disruption [24, 39, 40]. Their weight gain was comparable to the non-inoculated birds.
Host factors controlling C. jejuni in poultry
Differences in colonisation ability of Campylobacter may also be due to host factors. Possibly, the genetic background of the host may significantly affect Campylobacter colonisation and infection as it was shown for a variety of other avian pathogens [41–43].
Furthermore, an important limiting factor for bacterial diseases is the host immune response. For Salmonella it was demonstrated that infection induces an increase of T cell receptor (TCR) γδ, TCR αβ, CD4+ and CD8α+ T cells in chicken caecum. This increase coincides with cytokine upregulation such as IL-12, IL-18 and IL-2 indicating the stimulation of a T cell response [44].
Little is known about immune reactions involved in the control of C. jejuni colonisation and infection in avian species. To investigate the local immune responses of chickens after colonisation with different C. jejuni isolates of human and avian origin, we analyzed intraepithelial lymphocytes (IELs) of the caecum and the jejunum for CD4+ and CD8α+ T cells by flow cytometric analysis [45–48].
Interestingly, Campylobacter colonisation of the chicken gut hardly induced any changes in the number of CD4+ and CD8α+ T cells in the group of IELs.
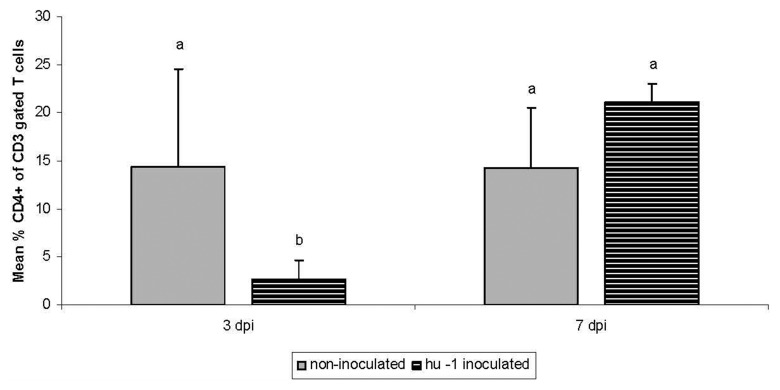
Only one human strain induced a reduction in the relative number of CD4+ T cells compared to the non-inoculated control group at 3 days post inoculation (dpi) in the jejunal IELs population (Fig. 2). This finding suggests that T cells may control Campylobacter colonisation in the early phase after inoculation because birds were negative of this C. jejuni strain at 3dpi and at later time points during the experiment. Further and earlier time points and further Campylobacter isolates of human origin have to be investigated to confirm this observation.
Fig. 2.
Comparison of the relative percent of CD4+ T cells of intraepithelial lymphocytes (IELs) of the jejunum of a non-inoculated and a group, inoculated with a human (hu) C. jejuni strain at 3 and 7 days post inoculation. n = six animals/day and group representative for the four conducted experiments. IELs were isolated and processed for flow cytometric analysis using monoclonal antibodies for CD3+ and CD4+ T cells (Southern Biotechn., USA). Presented are the %CD4+ T cells within the CD3+ IEL. Different letters indicate significant differences between groups at indicated time-points (p ≤ 0.05 Kruskal–Wallis test).
The investigation of pro-inflammatory cytokines revealed a role they play in Campylobacter infection in mammalian species and may allow to further understand the immune system in Campylobacter infected chickens, especially the innate mechanisms [49, 50]. We compared the expression pattern of IL-6 and interferon (IFN)-γ after infection of chickens with seven C. jejuni isolates of human and avian origin.
Being both pro-inflammatoric and anti-inflammatoric, IL-6 plays an important role in steering the switch from innate to acquired immunity [51]. It is secreted from a vast variety of cells including dendritic cells, monocytes, T cells, B cells and shows a wide range of biological activities [52, 53]. Friis et al. [54] could show an increase in levels of expression and secretion of IL-6 in human intestinal epithelial cells due to infection with several C. jejuni isolates. In a previous study Shaughnessy et al. [55] detected an increase of IL-6 in the intestine at 48 h post infection of four weeks old chickens, which indicates that innate immune reactions may possibly be important in the control of Campylobacter infection also in chicken. IFN-γ being the only type II class interferon secreted by a variety of cells such as T helper, cytotoxic T cells and Natural killer cells, acts as a regulatory and effector molecule for inflammatory responses [56].
Edwards et al. [57] showed with his studies that IFN-γ plays a critical role during the early acute phase of infection in human, detecting an increase of IFN-γ in human intestinal biopsies of both ileal and colonic tissue as well as in human dendritic cells after Campylobacter infection.
The cytokine expression pattern of IL-6 and IFN-γ in caecum and jejunum as well as in the spleen did not significantly differ between C. jejuni inoculated and non-in-oculated birds between 3 dpi to 14 dpi independent of the Campylobacter strain. In contrast Nyati et al. [58] could show an increase of both IFN-γ at 10 and 15 days and IL-6 at five and 10 days post inoculation with C. jejuni in the sciatic nerve in chickens.
Consequentially, time points earlier than 3 dpi should be investigated more carefully to elucidate the mechanisms controlling Campylobacter infection in chicken.
Conclusion
Our investigations clearly show that human and avian isolates may differ in their ability to colonize chickens, which is supported by previous investigations of other groups [36, 37, 59, 60].
Possible reasons may be genetic diversity between strains which may also affect the innate and eventually also the acquired immune response in the very early phase of colonisation.
Our data, as well as Shaughnessy et al. [55] provide circumstantial evidence that the immune response in the first three days may significantly affect the outcome of Campylobacter colonisation and infection.
Overall it may be suggested that C. jejuni is non pathogenic for healthy chickens.
Other predisposing factors may contribute to the systemic spread of Campylobacter in birds and the induction of lesions as observed under field conditions and described in the literature in the past [61, 62].
Further studies are needed to further understand important host factors responsible for the control of Campylobacter in chickens. This may allow the implementation of better control strategies of this important and zoonotic pathogen in poultry.
Acknowledgments
The authors would like to thank Sonja Bernhardt, Sabrina Techel and Katja Stolpe for their excellent support during the animal experiments. Further we would like thank Lydia Teske and Christine Haase for their technical assistance in the laboratory. The project was funded by the German Research Foundation (DFG, RA 767/4-1).
Contributor Information
C. Pielsticker, Clinic for Poultry, University of Veterinary Medicine Hannover, Hannover, Germany
G. Glünder, Clinic for Poultry, University of Veterinary Medicine Hannover, Hannover, Germany
S. Rautenschlein, Clinic for Poultry, University of Veterinary Medicine Hannover, Hannover, Germany.
References
- 1.Humphrey T, O'Brien S, Madsen M. Campylobacters as zoonotic pathogens: a food production perspective. Int J Food Microbiol. 2007 Jul 15;117(3):237–257. doi: 10.1016/j.ijfoodmicro.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Man SM. The clinical importance of emerging Campylobacter species. Nat Rev Gastroenterol Hepatol. 2011 Oct 25;8(12):669–685. doi: 10.1038/nrgastro.2011.191. [DOI] [PubMed] [Google Scholar]
- 3.Weber R, Alter T, et al. Campylobacter in different poultry species: Prevalence and spread between flocks. In: Wieliczko A, editor. Proceedings “Aktualne Problemy W Patologii Drobiu Ze Szczegolnym Uwzglednieniem Parazytoz”. Wroclaw, Poland: 2011. pp. 60–64. [Google Scholar]
- 4.Skirrow MB. Campylobacter enteritis: a "new" disease. Br Med J. 1977 Jul 2;2(6078):9–11. doi: 10.1136/bmj.2.6078.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bolton FJ, Hutchinson DN, Coates D. Blood-free selective medium for isolation of Campylobacter jejuni from feces. J Clin Microbiol. 1984 Feb;19(2):169–171. doi: 10.1128/jcm.19.2.169-171.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wheeler JG, Sethi D, Cowden JM, Wall PG, Rodrigues LC, Tompkins DS, Hudson MJ, Roderick PJ. Study of infectious intestinal disease in England: rates in the community, presenting to general practice, and reported to national surveillance. The Infectious Intestinal Disease Study Executive. BMJ. 1999 Apr 17;318(7190):1046–1050. doi: 10.1136/bmj.318.7190.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allos BM. Campylobacter jejuni Infections: update on emerging issues and trends. Clin Infect Dis. 2001 Apr 15;32(8):1201–1206. doi: 10.1086/319760. [DOI] [PubMed] [Google Scholar]
- 8.Blaser MJ. Epidemiologic and clinical features of Campylobacter jejuni infections. J Infect Dis. 1997 Dec;176(Suppl 2):S103–S105. doi: 10.1086/513780. [DOI] [PubMed] [Google Scholar]
- 9.Takahashi M, Koga M, Yokoyama K, Yuki N. Epidemiology of Campylobacter jejuni isolated from patients with Guillain-Barré and Fisher syndromes in Japan. J Clin Microbiol. 2005 Jan;43(1):335–339. doi: 10.1128/JCM.43.1.335-339.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corry JE, Atabay HI. Poultry as a source of Campylobacter and related organisms. Symp Ser Soc Appl Microbiol. 2001;2001(30):96S–114S. doi: 10.1046/j.1365-2672.2001.01358.x. [DOI] [PubMed] [Google Scholar]
- 11.Grant IH, Richardson NJ, Bokkenheuser VD. Broiler chickens as potential source of Campylobacter infections in humans. J Clin Microbiol. 1980 May;11(5):508–510. doi: 10.1128/jcm.11.5.508-510.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hald B, Skovgård H, Bang DD, Pedersen K, Dybdahl J, Jespersen JB, Madsen M. Flies and Campylobacter infection of broiler flocks. Emerg Infect Dis. 2004 Aug;10(8):1490–1492. doi: 10.3201/eid1008.040129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guerin MT, Martin W, Reiersen J, Berke O, McEwen SA, Bisaillon JR, Lowman R. A farm-level study of risk factors associated with the colonization of broiler flocks with Campylobacter spp. in Iceland, 2001-2004. Acta Vet Scand. 2007 Jul 10;49:18. doi: 10.1186/1751-0147-49-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bates C, Hiett KL, Stern NJ. Relationship of Campylobacter isolated from poultry and from darkling beetles in New Zealand. Avian Dis. 2004 Jan-Mar;48(1):138–147. doi: 10.1637/7082. [DOI] [PubMed] [Google Scholar]
- 15.Hastings R, Colles FM, McCarthy ND, Maiden MC, Sheppard SK. Campylobacter genotypes from poultry transportation crates indicate a source of contamination and transmission. J Appl Microbiol. 2011 Jan;110(1):266–276. doi: 10.1111/j.1365-2672.2010.04883.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sahin O, Morishita TY, Zhang Q. Campylobacter colonization in poultry: sources of infection and modes of transmission. Anim Health Res Rev. 2002 Dec;3(2):95–105. doi: 10.1079/ahrr200244. [DOI] [PubMed] [Google Scholar]
- 17.Hald B, Wedderkopp A, Madsen M. Thermophilic Campylobacter spp. in Danish broiler production: a cross-sectional survey and a retrospective analysis of risk factors for occurrence in broiler flocks. Avian Pathol. 2000 Apr;29(2):123–131. doi: 10.1080/03079450094153. [DOI] [PubMed] [Google Scholar]
- 18.Newell DG, Fearnley C. Sources of Campylobacter colonization in broiler chickens. Appl Environ Microbiol. 2003 Aug;69(8):4343–4351. doi: 10.1128/AEM.69.8.4343-4351.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Engvall A. COST Action 97. Lelystad, The Netherlands: Commission of the European Unions; 1999. Surveillance and control of Salmonella and Campylobacter in Swedish commercial poultry. [Google Scholar]
- 20.Park SF. The physiology of Campylobacter species and its relevance to their role as foodborne pathogens. Int J Food Microbiol. 2002 Apr 5;74(3):177–188. doi: 10.1016/s0168-1605(01)00678-x. [DOI] [PubMed] [Google Scholar]
- 21.Yogasundram K, Shane SM, Harrington KS. Prevalence of Campylobacter jejuni in selected domestic and wild birds in Louisiana. Avian Dis. 1989 Oct-Dec;33(4):664–667. [PubMed] [Google Scholar]
- 22.Hermans D, Pasmans F, Heyndrickx M, Van Immerseel F, Martel A, Van Deun K, Haesebrouck F. A tolerogenic mucosal immune response leads to persistent Campylobacter jejuni colonization in the chicken gut. Crit Rev Microbiol. 2012 Feb;38(1):17–29. doi: 10.3109/1040841X.2011.615298. [DOI] [PubMed] [Google Scholar]
- 23.Conlan AJ, Coward C, Grant AJ, Maskell DJ, Gog JR. Campylobacter jejuni colonization and transmission in broiler chickens: a modelling perspective. J R Soc Interface. 2007 Oct 22;4(16):819–829. doi: 10.1098/rsif.2007.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beery JT, Hugdahl MB, Doyle MP. Colonization of gastrointestinal tracts of chicks by Campylobacter jejuni. Appl Environ Microbiol. 1988 Oct;54(10):2365–2370. doi: 10.1128/aem.54.10.2365-2370.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee MD, Newell DG. Campylobacter in poultry: filling an ecological niche. Avian Dis. 2006 Mar;50(1):1–9. doi: 10.1637/7474-111605R.1. [DOI] [PubMed] [Google Scholar]
- 26.Knudsen KN, Bang DD, Andresen LO, Madsen M. Campylobacter jejuni strains of human and chicken origin are invasive in chickens after oral challenge. Avian Dis. 2006 Mar;50(1):10–14. doi: 10.1637/7376-051005R.1. [DOI] [PubMed] [Google Scholar]
- 27.Glünder G, Hinz K-H, et al. Zum Vorkommen von Bakterien der Gattung Campylobacter bei Vögeln. Tierärztl Umschau. 1988;43:694–699. [Google Scholar]
- 28.Craven SE, Stern NJ, Line E, Bailey JS, Cox NA, Fedorka-Cray P. Determination of the incidence of Salmonella spp., Campylobacter jejuni, and Clostridium perfringens in wild birds near broiler chicken houses by sampling intestinal droppings. Avian Dis. 2000 Jul-Sep;44(3):715–720. [PubMed] [Google Scholar]
- 29.Keller JI, Shriver WG, Waldenström J, Griekspoor P, Olsen B. Prevalence of Campylobacter in wild birds of the mid-Atlantic region, USA. J Wildl Dis. 2011 Jul;47(3):750–754. doi: 10.7589/0090-3558-47.3.750. [DOI] [PubMed] [Google Scholar]
- 30.Nauta M, Hill A, Rosenquist H, Brynestad S, Fetsch A, van der Logt P, Fazil A, Christensen B, Katsma E, Borck B, Havelaar A. A comparison of risk assessments on Campylobacter in broiler meat. Int J Food Microbiol. 2009 Feb 15;129(2):107–123. doi: 10.1016/j.ijfoodmicro.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 31.van Gerwe T, Miflin JK, Templeton JM, Bouma A, Wagenaar JA, Jacobs-Reitsma WF, Stegeman A, Klinkenberg D. Quantifying transmission of Campylobacter jejuni in commercial broiler flocks. Appl Environ Microbiol. 2009 Feb;75(3):625–628. doi: 10.1128/AEM.01912-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cawthraw SA, Newell DG. Investigation of the presence and protective effects of maternal antibodies against Campylobacter jejuni in chickens. Avian Dis. 2010 Mar;54(1):86–93. doi: 10.1637/9004-072709-Reg.1. [DOI] [PubMed] [Google Scholar]
- 33.Callicott KA, Friethriksdóttir V, Reiersen J, Lowman R, Bisaillon JR, Gunnarsson E, Berndtson E, Hiett KL, Needleman DS, Stern NJ. Lack of evidence for vertical transmission of Campylobacter spp. in chickens. Appl Environ Microbiol. 2006 Sep;72(9):5794–5798. doi: 10.1128/AEM.02991-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alter T, Weber RM, Hamedy A, Glünder G. Carry-over of thermophilic Campylobacter spp. between sequential and adjacent poultry flocks. Vet Microbiol. 2011 Jan 10;147(1-2):90–95. doi: 10.1016/j.vetmic.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 35.Petersen L, Nielsen EM, On SL. Serotype and genotype diversity and hatchery transmission of Campylobacter jejuni in commercial poultry flocks. Vet Microbiol. 2001 Sep 20;82(2):141–154. doi: 10.1016/s0378-1135(01)00382-0. [DOI] [PubMed] [Google Scholar]
- 36.Ringoir DD, Korolik V. Colonisation phenotype and colonisation potential differences in Campylobacter jejuni strains in chickens before and after passage in vivo. Vet Microbiol. 2003 Apr 2;92(3):225–235. doi: 10.1016/s0378-1135(02)00378-4. [DOI] [PubMed] [Google Scholar]
- 37.Korolik V, Alderton MR, Smith SC, Chang J, Coloe PJ. Isolation and molecular analysis of colonising and non-colonising strains of Campylobacter jejuni and Campylobacter coli following experimental infection of young chickens. Vet Microbiol. 1998 Feb 28;60(2-4):239–249. doi: 10.1016/s0378-1135(98)00145-x. [DOI] [PubMed] [Google Scholar]
- 38.Glünder G, Hinz K-H, et al. Campylobacter-Infektionen in Legehennenherden und Antikörperstatus. In: Neumann U, editor. Proceedings “53. Bi-annual Meeting Poultry Branch of the German Vet.-Med. Society Fachgruppe Geflügelkrankheiten DVG”. Hannover, Germany: 1997. pp. 151–165. [Google Scholar]
- 39.Morales W, Pimentel M, Hwang L, Kunkel D, Pokkunuri V, Basseri B, Low K, Wang H, Conklin JL, Chang C. Acute and chronic histological changes of the small bowel secondary to C. jejuni infection in a rat model for post-infectious IBS. Dig Dis Sci. 2011 Sep;56(9):2575–2584. doi: 10.1007/s10620-011-1662-6. [DOI] [PubMed] [Google Scholar]
- 40.Murphy H, Cogan T, Humphrey T. Direction of neutrophil movements by Campylobacter-infected intestinal epithelium. Microbes Infect. 2011 Jan;13(1):42–48. doi: 10.1016/j.micinf.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 41.Aricibasi M, Jung A, Heller ED, Rautenschlein S. Differences in genetic background influence the induction of innate and acquired immune responses in chickens depending on the virulence of the infecting infectious bursal disease virus (IBDV) strain. Vet Immunol Immunopathol. 2010 May 15;135(1-2):79–92. doi: 10.1016/j.vetimm.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 42.Berchieri A, Jr., Murphy CK, Marston K, Barrow PA. Observations on the persistence and vertical transmission of Salmonella enterica serovars Pullorum and Gallinarum in chickens: effect of bacterial and host genetic background. Avian Pathol. 2001 Jun;30(3):221–231. doi: 10.1080/03079450120054631. [DOI] [PubMed] [Google Scholar]
- 43.Sarson AJ, Parvizi P, Lepp D, Quinton M, Sharif S. Transcriptional analysis of host responses to Marek's disease virus infection in genetically resistant and susceptible chickens. Anim Genet. 2008 Jun;39(3):232–240. doi: 10.1111/j.1365-2052.2008.01710.x. [DOI] [PubMed] [Google Scholar]
- 44.Berndt A, Wilhelm A, Jugert C, Pieper J, Sachse K, Methner U. Chicken cecum immune response to Salmonella enterica serovars of different levels of invasiveness. Infect Immun. 2007 Dec;75(12):5993–6007. doi: 10.1128/IAI.00695-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen CL, Ager LL, Gartland GL, Cooper MD. Identification of a T3/T cell receptor complex in chickens. J Exp Med. 1986 Jul 1;164(1):375–380. doi: 10.1084/jem.164.1.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Göbel TW. Isolation and analysis of natural killer cells in chickens. Methods Mol Biol. 2000;121:337–345. doi: 10.1385/1-59259-044-6:337. [DOI] [PubMed] [Google Scholar]
- 47.Liman M, Rautenschlein S. Induction of local and systemic immune reactions following infection of turkeys with avian Metapneumovirus (aMPV) subtypes A and B. Vet Immunol Immunopathol. 2007 Feb 15;115(3-4):273–285. doi: 10.1016/j.vetimm.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 48.Schwarz A, Gauly M, Abel H, Daş G, Humburg J, Rohn K, Breves G, Rautenschlein S. Immunopathogenesis of Ascaridia galli infection in layer chicken. Dev Comp Immunol. 2011 Jul;35(7):774–784. doi: 10.1016/j.dci.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 49.Bahrami B, Macfarlane S, Macfarlane GT. Induction of cytokine formation by human intestinal bacteria in gut epithelial cell lines. J Appl Microbiol. 2011 Jan;110(1):353–363. doi: 10.1111/j.1365-2672.2010.04889.x. [DOI] [PubMed] [Google Scholar]
- 50.Young KT, Davis LM, Dirita VJ. Campylobacter jejuni: molecular biology and pathogenesis. Nat Rev Microbiol. 2007 Sep;5(9):665–679. doi: 10.1038/nrmicro1718. [DOI] [PubMed] [Google Scholar]
- 51.McLoughlin RM, Jenkins BJ, Grail D, Williams AS, Fielding CA, Parker CR, Ernst M, Topley N, Jones SA. IL-6 trans-signaling via STAT3 directs T cell infiltration in acute inflammation. Proc Natl Acad Sci U S A. 2005 Jul 5;102(27):9589–9594. doi: 10.1073/pnas.0501794102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Naka T, Nishimoto N, Kishimoto T. The paradigm of IL-6: from basic science to medicine. Arthritis Res. 2002;4(Suppl 3):S233–S242. doi: 10.1186/ar565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kishimoto T, Akira S, Narazaki M, Taga T. Interleukin-6 family of cytokines and gp130. Blood. 1995 Aug 15;86(4):1243–1254. [PubMed] [Google Scholar]
- 54.Friis LM, Keelan M, Taylor DE. Campylobacter jejuni drives MyD88-independent interleukin-6 secretion via Toll-like receptor 2. Infect Immun. 2009 Apr;77(4):1553–1560. doi: 10.1128/IAI.00707-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shaughnessy RG, Meade KG, Cahalane S, Allan B, Reiman C, Callanan JJ, O'Farrelly C. Innate immune gene expression differentiates the early avian intestinal response between Salmonella and Campylobacter. Vet Immunol Immunopathol. 2009 Dec 15;132(2-4):191–198. doi: 10.1016/j.vetimm.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 56.Hackney K, Cavanagh D, Kaiser P, Britton P. In vitro and in ovo expression of chicken gamma interferon by a defective RNA of avian coronavirus infectious bronchitis virus. J Virol. 2003 May;77(10):5694–5702. doi: 10.1128/JVI.77.10.5694-5702.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Edwards LA, Nistala K, Mills DC, Stephenson HN, Zilbauer M, Wren BW, Dorrell N, Lindley KJ, Wedderburn LR, Bajaj-Elliott M. Delineation of the innate and adaptive T-cell immune outcome in the human host in response to Campylobacter jejuni infection. PLoS One. 2010 Nov 9;5(11):e15398. doi: 10.1371/journal.pone.0015398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nyati KK, Prasad KN, Kharwar NK, Soni P, Husain N, Agrawal V, Jain AK. Immunopathology and Th1/Th2 immune response of Campylobacter jejuni-induced paralysis resembling Guillain-Barré syndrome in chicken. Med Microbiol Immunol. 2012 May;201(2):177–187. doi: 10.1007/s00430-011-0220-3. [DOI] [PubMed] [Google Scholar]
- 59.Hänel I, Borrmann E, Müller J, Müller W, Pauly B, Liebler-Tenorio EM, Schulze F. Genomic and phenotypic changes of Campylobacter jejuni strains after passage of the chicken gut. Vet Microbiol. 2009 Apr 14;136(1-2):121–129. doi: 10.1016/j.vetmic.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 60.Stern NJ, Bailey JS, Blankenship LC, Cox NA, McHan F. Colonization characteristics of Campylobacter jejuni in chick ceca. Avian Dis. 1988 Apr-Jun;32(2):330–334. [PubMed] [Google Scholar]
- 61.Burch D. Avian vibrionic hepatitis in laying hens. Vet Rec. 2005 Oct 22;157(17):528. doi: 10.1136/vr.157.17.528-a. [DOI] [PubMed] [Google Scholar]
- 62.Neill SD, Campbell JN, Greene JA. Campylobacter species in broiler chickens. Avian Pathol. 1984 Oct;13(4):777–785. doi: 10.1080/03079458408418574. [DOI] [PubMed] [Google Scholar]
- 63.Smith CK, Abuoun M, Cawthraw SA, Humphrey TJ, Rothwell L, Kaiser P, Barrow PA, Jones MA. Campylobacter colonization of the chicken induces a proinflammatory response in mucosal tissues. FEMS Immunol Med Microbiol. 2008 Oct;54(1):114–121. doi: 10.1111/j.1574-695X.2008.00458.x. [DOI] [PubMed] [Google Scholar]