Abstract
Aim of the study
The Patient Assistance Program, a type of expanded access program, was initiated for compassionate purposes to provide ipilimumab to patients with unresectable stage III or IV melanoma with failed previous treatment. The aim of this analysis is to evaluate efficacy, safety, and tolerability of ipilimumab therapy in daily clinical practice.
Material and methods
We analyzed 50 patients (29 males, 21 females) aged 21 to 76 years (median: 49 years). An ipilimumab dose of 3 mg/kg was administered intravenously every 3 weeks for a total of 4 doses. Patients were assessed for response rate, progression-free survival and overall survival, and monitored for adverse events.
Results
The objective response (complete or partial response) rate was 12%. Median overall survival was 8 months and median progression-free survival was 3 months. In patients with ECOG-PS 0, the median overall survival was 16 months. Immune-related adverse events (irAEs) occurred in 48% of the patients, grade 3 or 4 irAEs were reported in 8% of the patients, and there were no toxic deaths.
Conclusions
Ipilimumab demonstrated clinical benefit in previously treated advanced melanoma patients. Although clinical benefit is limited to a minority of the patients, there is a benefit in terms of overall survival in this group of patients.
Keywords: melanoma, ipilimumab, CTLA-4, immunotherapy, outcome
Introduction
Ipilimumab, a human monoclonal antibody against cytotoxic T-lymphocyte-associated antigen-4 (CTLA-4), was the first agent in the history of melanoma that was registered on the basis of overall survival benefit [1, 2]. The mechanism of action of ipilimumab is indirect and non-cancer-specific. The CTLA-4 blockade results in the enhancement of the T-cell mediated antitumor immune response [3]. Outcomes of phase II and III clinical trials led to the registration of the drug in the United States in March 2011 and in Europe in July 2011. In the European Union, it has been approved for the treatment of advanced (unresectable or metastatic) melanoma in adults who have received prior therapy. Although the objective response rate to ipilimumab is only 10%, some patients (20–25%) have shown a significant improvement in overall survival. Due to unusual patterns of response that can occur after initial progression, immune-related response criteria (irRC) are recommended for evaluation of objective responses [4, 5]. Ipilimumab treatment has been associated with autoimmune side effects, called immune-related adverse events (irAEs). As they may be severe and potentially fatal, appropriate treatment algorithms for irAEs have been developed to ensure the safety of melanoma patients during ipilimumab therapy [6].
In Poland, access to ipilimumab therapy is still limited due to the high cost of therapy. The Patient Assistance Program (PAP) was designed for compassionate purposes to provide access to ipilimumab for patients with unresectable stage III and IV melanoma whose disease had progressed after systemic therapy and had no other treatment option. The aim of the study was to evaluate the efficacy and safety of ipilimumab therapy in daily clinical practice.
Material and methods
Between May 2011 and July 2012, 50 patients (29 males, 21 females) with unresectable stage III and IV melanoma were treated with ipilimumab in 5 Polish oncological centers that were involved in the analysis. The baseline characteristics of patients are presented in Table 1. Forty-one (82%) patients had cutaneous melanoma and 9 (18%) patients had primary ocular melanoma. The median age was 49 years (range: 21–76 years). Thirty-six (72%) patients had stage M1c disease, including 9 (18%) patients with brain metastases. The majority of the patients (82%) had a performance status (PS) ≤ 1 according to ECOG (Eastern Cooperative Oncology Group). An elevated lactate dehydrogenase (LDH) level at baseline was observed in more than half of the patients. All patients received prior therapy for metastatic disease. Thirty-two percent of the patients received more than one line of systemic therapy. All patients gave informed consent for therapy. Thirty-five (70%) patients received all four doses of ipilimumab. Four patients discontinued treatment due to adverse events, and 6 due to rapid disease progression (Table 2).
Table 1.
Baseline characteristics of patients
| Characteristic | Number of patients, N = 50 |
|---|---|
| Median age, years (range) | 49 (21–76) |
| Female/male | 21/29 |
| ECOG performance status | |
| 0 | 19 (38%) |
| 1 | 22 (44%) |
| 2 | 7 (14%) |
| 3 | 2 (4%) |
| Primary melanoma site, n (%) | |
| Cutaneous | 41 (82 %) |
| Uveal | 9 (18%) |
| M stage, n (%) | |
| M1a | 8 (16%) |
| M1b | 6 (12%) |
| M1c | 36 (72%) |
| M1c – brain | 9 (18 %)] |
| Number of previous lines of therapy, n (%) | |
| 1 | 34 (68%) |
| 2 | 10 (20%) |
| 3 | 6 (12%) |
| Median number of previous lines of therapy (range) | 1 (1–3) |
| LDH > ULN | 27 (54%) |
| Cancer Center, number of patients treated with ipilimumab | |
| Warsaw | 26 |
| Poznan | 11 |
| Lodz | 8 |
| Bialystok | 3 |
| Olsztyn | 2 |
ECOG – Eastern Cooperative Oncology Group; LDH – lactate dehydrogenase;ULN – upper limit of normal value
Table 2.
Overview of treatment
| Ipilimumab 3 mg/kg | Patients, n (%) |
|---|---|
| 1 dose | 6 (12%) |
| 2 doses | 3 (6%) |
| 3 doses | 6 (12%) |
| 4 doses | 35 (70%) |
Ipilimumab was available upon physician request in the PAP for patients with unresectable stage III and IV cutaneous or uveal melanoma whose previous treatments failed or were not tolerated. Patients with stable brain metastases after previous therapy were eligible. Exclusion criteria were as follows: concomitant autoimmune disease, HIV infection, hepatitis B or C, and prior treatment with anti-CTLA-4 antibody. Ipilimumab at 3 mg/kg was administered intravenously over 90 minutes every 3 weeks for a total of 4 doses. If mild or moderate adverse reactions occurred, the dose could be omitted.
In patients with severe toxicity, ipilimumab therapy was permanently discontinued. The re induction of therapy was not used in the case of possible disease progression after previous at least stabilization of disease gained due to ipilimumab treatment.
All patients were closely monitored for adverse drug reactions. Adverse events (AEs) were graded using the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0. Clinical response was assessed with CT or MR scans using immune-related response criteria (irRC) [4].
The first scheduled tumor assessment was at week 12, and complete responses (CR) and partial responses (PR), if applicable, were confirmed at least 4 weeks later. If disease progression occurred before week 12, treatment was continued in patients without intolerable toxicity or a worsening performance status.
Statistical analysis was performed with a licensed copy of MedCalc 12.4.0. For survival analysis, the Kaplan-Meier method was used with the log-rank tests for bivariate comparisons. Overall survival (OS) time was calculated from the date of the first administration of ipilimumab to the date of the most recent follow-up (censored data) or death (death due to any cause was set as the end point because no patients had died of causes other than melanoma). Progression-free survival (PFS) time was calculated from the date of the first administration of ipilimumab to the date of the most recent follow-up (censored data), documented disease progression, or death (whichever occurred earlier).
The differences were considered statistically significant if the p-values were < 0.05.
Results
Efficacy
Efficacy data are shown in Table 3. At week 12, 1 patient (2%) achieved confirmed irCR (immune-related complete response), 5 patients (10%) experienced irPR (immune-related partial response), and 9 patients (8%) had irSD (immune-related stable disease). Thirty-five patients (70%) experienced irPD (immune-related progressive disease). Responses were observed at all stages of metastatic disease and in patients with normal and elevated baseline LDH levels. The objective response rate (irCR and irPR) was 12%.
Table 3.
Tumor response to therapy
| Response according to irRC | Patients, N = 50(%) | Melanoma diagnosi n (%) | Performance status n (%) | M stage n (%) | LDH level | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||
| cutaneous | uveal | ECOG 0–1 | ECOG ≥ 2 | M1a | M1b | M1c | M1c-brain | < ULN | ≥≥ ULN | ||
| irCR | 1 (2%) | 1 (2%) | 0 | 1 (2%) | 0 | 1 (2%) | 0 | 0 | 0 | 1 (2%) | 0 |
| irPR | 5 (10%) | 5 (10%) | 0 | 5 (10%) | 0 | 0 | 2 (4%) | 3 (6%) | 1 (2%) | 3 (6%) | 2 (4%) |
| irSD | 9 (18%) | 7 (14%) | 2 (4%) | 9 (18%) | 0 | 3 (6%) | 1 (2%) | 5 (12%) | 0 | 6 (12%) | 3 (6%) |
| irPD | 35 (70%) | 28 (56%) | 7 (14%) | 27 (54%) | 8 (16%) | 4 (8%) | 3 (6%) | 27 (54%) | 8 (16%) | 13 (26%) | 22 (44%) |
irCR – immune-related complete response; irPR – immune-related partial response; irSD – immune-related stable disease; irPD – immune-related progressive disease; LDH – lactate dehydrogenase; ULN – upper limit of normal
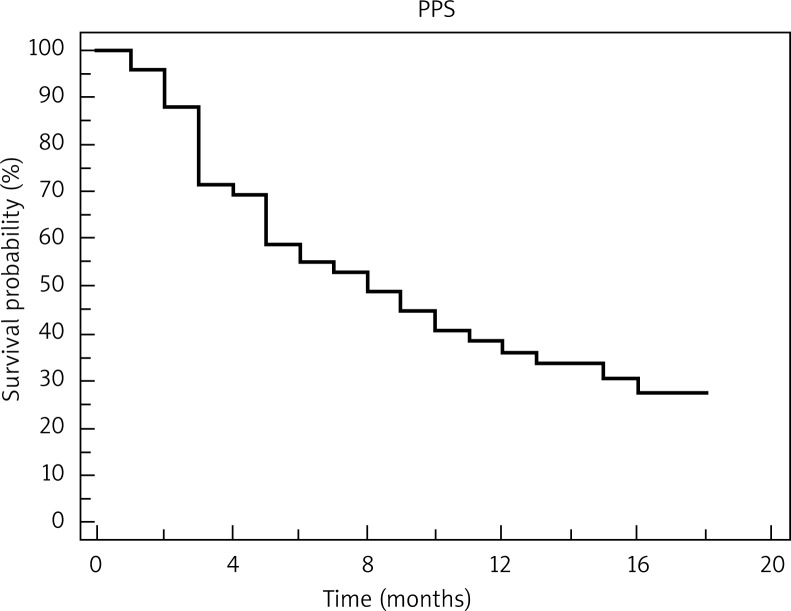
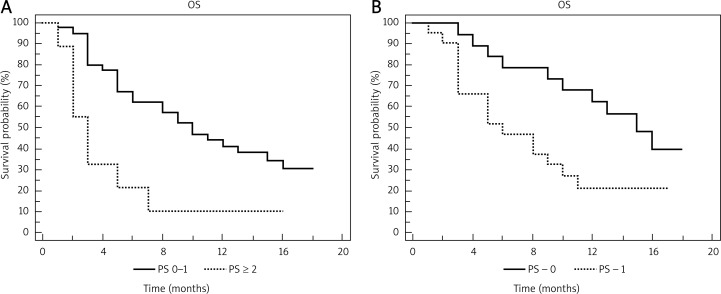
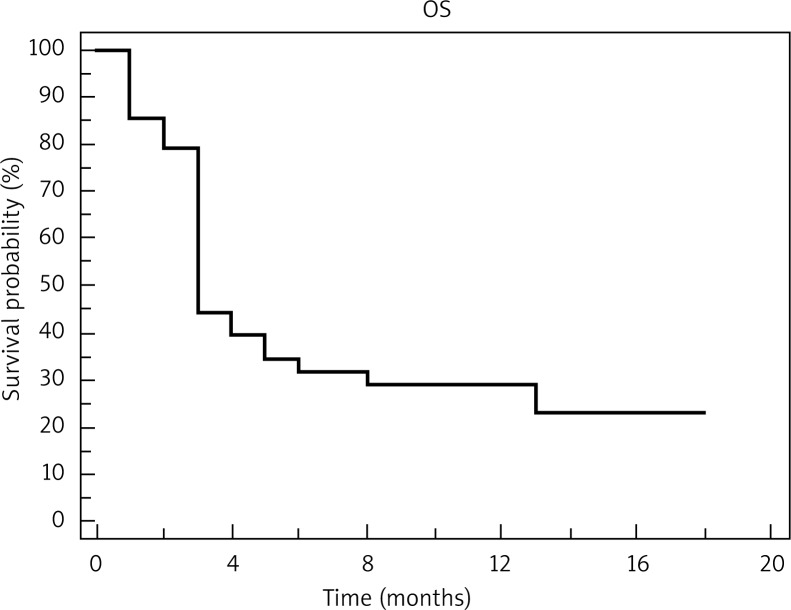
The median overall survival (assessed in 49 patients, 1 patient was lost to follow-up) was 8 months; the 1-year survival rate was 34.7% (Fig. 1). There was a significant difference in overall survival between patients in ECOG PS ≤ 1 and ≥ 2. The 1-year survival rate for patients with PS 0 or 1 was 40%, compared with 11.1% for those with PS ≥ 2 (p = 0.0047, hazard ratio 2.82, 95% CI: 0.91–8.71) (Fig. 2A). When comparing patients with ECOG PS 0 and 1, the 1-year survival was 63.2% and 19%, respectively (p = 0.0231, hazard ratio 2.33, 95% CI: 1.06–5.1) (Fig. 2B). The median progression-free survival (PFS) was 3 months; the 1-year PFS rate was 14% (Fig. 3).
Fig. 1.
Kaplan-Meier curve for overall survival (OS)
Fig. 2.
A) Kaplan-Meier plot of overall survival (OS) according to performance status (PS), PS 0-1 vs. PS ≥ 2; B) Kaplan-Meier plot of overall survival (OS) according to performance status (PS), PS 0-1 vs. PS 1
Fig. 3.
Kaplan-Meier curve for progression-free survival (PFS)
Toxicity
Twenty-five (50%) patients experienced treatment-related adverse events (AEs) (Table 4). The most common AEs were those classified as immune-related adverse events (irAEs). They occurred mainly in the skin (11 patients) and gastrointestinal tract (6 patients). The majority of them were grade 1 or 2 and were generally manageable and reversible without any sequelae. There were no treatment-related deaths. In cases with irAEs, we followed treatment guidelines for irAEs [6, 7]. Adverse events of grade 3 or higher occurred in 8% of the patients. Two patients experienced grade 3 or 4 diarrhea that resolved within a few weeks after treatment with high-dose intravenous corticosteroids.
Table 4.
Treatment-related adverse events
| Treatment-related adverse events | Patients n (%) | |
|---|---|---|
|
| ||
| All grades | Grades 3–4 | |
| total | 25 (50%) | 4 (8%) |
| rash | 10 (20%) | 0 |
| pruritus | 4 (8%) | 0 |
| vitiligo | 2 (4%) | 0 |
| asthenia | 5 (10%) | 0 |
| diarrhea | 6 (12%) | 2 (4%) |
| hypophysitis | 1 (2%) | 1 (2%) |
| hepatitis | 1 (2%) | 1 (2%) |
| hypothyroidism | 1 (2%) | 0 |
| hyperthyroidism | 1 (2%) | 1 (2%) |
| ALT/AST elevation | 0 | 1 (2%) |
ALT – alanine aminotransferase, AST – asparagine aminotransferase
One patient experienced grade 4 mixed endocrinopathy. The patient was diagnosed with thyroid crisis due to autoimmune thyroiditis and lymphocytic hypophysitis. Grade 3 elevation in alanine aminotransferase and vitiligo were also observed in this patient. Toxicity occurred after the third dose of ipilimumab. The treatment was discontinued. The patient currently remains stable on glucocorticoid replacement therapy. At week 12, assessment of this patient found irCR, which is still ongoing (17 months).
Another patient developed febrile neutropenia after the third cycle of ipilimumab, displaying a lack of all granulocyte lines in a blood smear test. The grade 4 neutropenia lasted for 16 days. The autoimmune character of this SAE (serious adverse event) was not confirmed, although neutropenia due to the administration of concomitant medications or metastases to the bone marrow was ruled out. The patient died a few weeks later due to progression of the neutropenia.
Discussion
The prognosis of patients with stage IV melanoma is very poor, with 1-year survival rates for those with M1a, M1b, and M1c being 62%, 53%, and 33%, respectively [8]. Despite many efforts over the past 40 years to improve outcomes, no significant impact on survival has been made. In contrast, in 2011, the treatment landscape for metastatic melanoma underwent dramatic changes. In March, the U.S. Food and Drug Administration registered ipilimumab, and just 5 months later, the molecularly targeted agent vemurafenib. Although the mechanism of action of these drugs is different, they have both been shown to improve survival of patients. Until their registrations, the standard treatment of advanced melanoma was dacarbazine (DTIC), a chemotherapy agent with a response rate of 10–20% [9].
The approval of ipilimumab was based on the results from a phase III randomized (3 : 1 : 1) double-blind study (MDX010-20) of patients with unresectable or metastatic melanoma who had received at least one prior systemic treatment for melanoma. The study group consisted of 55%, 43%, and 1% of patients with ECOG performance status 0, 1, and 2, respectively. Most patients (70%) were in stage M1c and 11% had brain metastases at study entry. The median OS among patients receiving ipilimumab alone was 10.1 months, the 1-year OS was 46%, and the 2-year survival rate was 24% [10]. That means that in some percentage of patients, ipilimumab can induce a durable response lasting 2 to 5 years [11].
We report here the survival of non-selected patients treated in routine clinical practice, where the median OS was 8 months (range: 1–18) and the 1-year survival rate was 34.7%. At the time of data analysis, 15 (30%) patients remained alive and the median follow-up time for the survivors was 16 months (range: 9–18). These results are slightly worse than expected, but we have to stress that in the analyzed group, one third of the patients received more than one line of previous systemic therapy due to metastatic disease and almost 20% of the patients had a PS of at least 2 (those patients did not benefit from ipilimumab therapy). Furthermore, 18% of patients presented brain metastases before starting ipilimumab treatment.
In phase II and III studies, objective response rates ranged from 5.8% to 15.8% [10, 12–15]. In the present study, the objective response rate was similar, with 12% of patients achieving irCR and irPR. The disease control rate (DCR) was 30%, with 8 patients (16%) without disease progression to date. The effect of ipilimumab on DCR was independent of the stage of metastatic disease (M1a-M1c). Subgroup analysis showed that only patients with a good performance status (ECOG 0–1) experienced clinical benefit (Fig. 3). The survival rate is particularly high in the PS 0 group of patients. No clinical benefits of ipilimumab treatment have been observed in patients with PS > 1. In the group of patients with metastases to the central nervous system, clinical benefits were observed in only 1 patient, although previous documented cases indicate the possibility of clinical benefits for patients with asymptomatic metastases to the CNS [16]. Since no reliable factors for predicting clinical benefits of treatment with ipilimumab have been determined, the patient's overall condition (optimal PS value – 0) seems to be the most important factor in assessing the patient's suitability for ipilimumab treatment after previous, unsuccessful systemic treatment (as per European Union registration terms). This also shows the need for thorough testing among patients for melanomas with a high risk of relapse using various imaging techniques. This way, potential metastases can be detected sooner, when the patient is in a good performance status, leaving enough time to develop an immunological response through treatment with ipilimumab. The results are yet to be confirmed in pending research on biological markers, such as changes in the absolute lymphocyte count and ICOS + T cells (inducible costimulator involved in autoimmunity mechanisms and Treg function) during treatment [17–19].
In the present study, we treated 9 patients with metastatic uveal melanoma (UM), which comprised almost 20% of the analyzed group. Patients with primary ocular melanoma were usually excluded from phase II and III studies. Thus, the current treatment options for these patients are limited by the lack of data on the efficacy of novel therapies. Smaller studies indicate that UM is a potential indication for ipilimumab treatment. Danielli et al. evaluated the activity and safety of ipilimumab in patients with uveal melanoma. In 13 patients with stage IV UM, no objective responses were observed; however, 2 patients had stable disease (SD), with a third patient achieving SD after initial progressive disease [20]. A recently published analysis reports the outcomes of ipilimumab therapy in 5 patients with advanced UM. Two patients had durable stable disease and 3 developed progressive disease [21]. None of these patients responded to ipilimumab therapy. The clinical responses observed in our patients were similar: 2 patients had SD and 7 patients experienced progression of disease. These results suggest that ipilimumab therapy of patients with UM cannot be considered as a standard approach and should be further investigated in clinical trials.
Due to its mechanism of action, ipilimumab has a unique toxicity profile. The most common adverse events were immune-related [22]. IrAEs include mainly dermatitis, colitis, diarrhea, hepatitis, endocrinopathies, episcleritis/uveitis, and neuropathies [23]. These adverse effects have a characteristic pattern of onset. Adverse events affecting the skin were seen after 3 to 4 weeks, side effects involving the gastrointestinal tract and liver appeared after 6 to 7 weeks, and endocrine effects were apparent after approximately 9 weeks [24].
At a dosage of 3 mg/kg, as compared with 10 mg/kg, there was no significant difference in the frequency of immune-related adverse events [15]. However, the incidence of serious immune-related adverse events, especially those affecting the gastrointestinal tract, was higher in patients receiving a dose of 10 mg/kg. The frequency of grade 3 or 4 irAEs among patients treated with 3 mg/kg ipilimumab in phase II or III studies ranges from 7 to 14.5% [10, 15]. In the present study, irAEs were observed in 48% of the patients. IrAEs of grade 3 or higher occurred in 8% of the patients. In most cases, when the appropriate treatment was administered, the symptoms subsided quickly, proving the efficacy of the procedures developed in case of occurrence of any side effects of ipilimumab.
Data derived from several smaller studies suggested that there was a correlation of autoimmunity with objective cancer regression. In 56 patients with stage IV melanoma treated with ipilimumab, 36% of the patients with grade 3 or 4 autoimmunity toxicity showed a clinical response, compared with only 5% of responders in a group with no autoimmunity [25].
In analysis of 3 phase II studies published during the ASCO Annual Meeting of 2009, the rate of disease control in patients with grade 0 or 1 irAEs was 20–24%, and in patients with grade s≥ 2, irAEs was 34–43%. However, this difference was not statistically significant [26]. In our patient population, clinical benefit was observed among patients who developed an irAE and among patients who did not develop an irAE. However, the only patient who achieved irCR experienced the most serious adverse events (grade 4 endocrinopathy).
In the present study, ipilimumab demonstrated clinical activity and benefit in pretreated patients with advanced melanoma, although the enrolled patients had remarkably worse prognostic factors than in previously conducted clinical trials (poor performance status, presence of central nervous system metastases, and metastatic uveal melanoma). Only one report on the results of treatment with ipilimumab in clinical practice has been published to date (apart from a study on a group of patients treated as part of a controlled clinical trial) [27], which increases the importance of the results obtained in this study. Proper selection of patients for ipilimumab therapy (especially proper performance status) seems to be crucial. Patients with a poor performance status (ECOG ≥ 2) are likely to have rapidly progressive disease and will not benefit from ipilimumab therapy. The adverse events of immunotherapy with ipilimumab can be serious and potentially life-threatening. Therefore, patients should be closely monitored for any adverse events, as only immediate initiation of appropriate treatment may prevent uncontrolled activation of an autoreactive immune response.
Acknowledgments
We would like to thank Bristol-Myers Squibb for providing financial support for medical writing and drug supply for patient treatment.
References
- 1.O'Day SJ, Hamid O, Urba WJ. Targeting cytotoxic T-lymphocyte antigen-4 (CTLA4): a novel strategy for the treatment of melanoma and other malignancies. Cancer. 2007;110:2614–27. doi: 10.1002/cncr.23086. [DOI] [PubMed] [Google Scholar]
- 2.Eggermont AM, Robert C. New drugs in melanoma: It's a whole new world. Eur J Cancer. 2011;47:2150–7. doi: 10.1016/j.ejca.2011.06.052. [DOI] [PubMed] [Google Scholar]
- 3.Leach DR, Krummel MF, Allison JP. Enhancement of antitumor immunity by CTLA-4 blockade. Science. 1996;271:1734–6. doi: 10.1126/science.271.5256.1734. [DOI] [PubMed] [Google Scholar]
- 4.Wolchok JD, Hoos A, O'Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15:7412–0. doi: 10.1158/1078-0432.CCR-09-1624. [DOI] [PubMed] [Google Scholar]
- 5.Switaj T, Wysocki P, Wojtukiewicz M, et al. Ipilimumab- Progress in therapy of advanced melanoma. Onkol Prakt Klin. 2011;7:231–45. [Google Scholar]
- 6.Kähler KC, Hauschild A. Treatment and side effect management of CTLA-4 antibody therapy in metastatic melanoma. J Dtsch Dermatol Ges. 2011;9:277–85. doi: 10.1111/j.1610-0387.2010.07568.x. [DOI] [PubMed] [Google Scholar]
- 7.Kaehler KC, Piel S, Livingstone E, Schilling B, Hauschild A, Schadendorf D. Update on immunologic therapy with anti-CTLA-4 antibodies in melanoma: identification of clinical and biological response patterns, immune-related adverse events, and their management. Semin Oncol. 2010;37:485–98. doi: 10.1053/j.seminoncol.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27:6199–206. doi: 10.1200/JCO.2009.23.4799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serrone L, Zeuli M, Sega FM, Cognetti F. Dacarbazine-based chemotherapy for metastatic melanoma: thirty-year experience overview. J Exp Clin Cancer Res. 2000;19:21–34. [PubMed] [Google Scholar]
- 10.Hodi FS, O'Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prieto PA, Yang JC, Sherry RM, et al. CTLA-4 blockade with ipilimumab: long-term follow-up of 177 patients with metastatic melanoma. Clin Cancer Res. 2012;18:2039–47. doi: 10.1158/1078-0432.CCR-11-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–26. doi: 10.1056/NEJMoa1104621. [DOI] [PubMed] [Google Scholar]
- 13.O'Day SJ, Maio M, Chiarion-Sileni V, et al. Efficacy and safety of ipilimumab monotherapy in patients with pretreated advanced melanoma: a multicenter single-arm phase II study. Ann Oncol. 2010;21:1712–7. doi: 10.1093/annonc/mdq013. [DOI] [PubMed] [Google Scholar]
- 14.Weber J, Thompson JA, Hamid O, et al. A randomized, double-blind, placebo-controlled, phase II study comparing the tolerability and efficacy of ipilimumab administered with or without prophylactic budesonide in patients with unresectable stage III or IV melanoma. Clin Cancer Res. 2009;15:5591–8. doi: 10.1158/1078-0432.CCR-09-1024. [DOI] [PubMed] [Google Scholar]
- 15.Wolchok JD, Neyns B, Linette G, et al. Ipilimumab monotherapy in patients with pretreated advanced melanoma: a randomised, double-blind, multicentre, phase 2, dose-ranging study. Lancet Oncol. 2010;11:155–64. doi: 10.1016/S1470-2045(09)70334-1. [DOI] [PubMed] [Google Scholar]
- 16.Margolin K, Ernstoff MS, Hamid O, et al. Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol. 2012;13:459–65. doi: 10.1016/S1470-2045(12)70090-6. [DOI] [PubMed] [Google Scholar]
- 17.Ku GY, Yuan J, Page DB, et al. Single-institution experience with ipilimumab in advanced melanoma patients in the compassionate use setting: lymphocyte count after 2 doses correlates with survival. Cancer. 2010;116:1767–75. doi: 10.1002/cncr.24951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carthon BC, Wolchok JD, Yuan J, et al. Preoperative CTLA-4 blockade: tolerability and immune monitoring in the setting of a presurgical clinical trial. Clin Cancer Res. 2010;16:2861–71. doi: 10.1158/1078-0432.CCR-10-0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fu T, He Q, Sharma P. The ICOS/ICOSL pathway is required for optimal antitumor responses mediated by anti-CTLA-4 therapy. Cancer Res. 2011;71:5445–54. doi: 10.1158/0008-5472.CAN-11-1138. [DOI] [PubMed] [Google Scholar]
- 20.Danielli R, Ridolfi R, Chiarion-Sileni V, et al. Ipilimumab in pretreated patients with metastatic uveal melanoma: safety and clinical efficacy. Cancer Immunol Immunother. 2012;61:41–8. doi: 10.1007/s00262-011-1089-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khattak MA, Fisher R, Hughes P, Gore M, Larkin J. Ipilimumab activity in advanced uveal melanoma. Melanoma Res. 2013;23:79–81. doi: 10.1097/CMR.0b013e32835b554f. [DOI] [PubMed] [Google Scholar]
- 22.Weber J. Review: anti-CTLA-4 antibody ipilimumab: case studies of clinical response and immune-related adverse events. Oncologist. 2007;12:864–72. doi: 10.1634/theoncologist.12-7-864. [DOI] [PubMed] [Google Scholar]
- 23.Di Giacomo AM, Biagoli M, Maio M. The emerging toxicity profiles of anti-CTLA-4 antibodies across clinical indications. Semin Oncol. 2010;37:499–507. doi: 10.1053/j.seminoncol.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Lebbe C, O'Day S, Chiarion-Sileni V, et al. Analysis of the onset and resolution of immune-related adverse events during treatment with ipilimumab in patients with metastatic melanoma. Perspectives in Melanoma XII. 2008 abstr. O-015. [Google Scholar]
- 25.Attia P, Phan GQ, Maker AV, et al. Autoimmunity correlates with tumor regression in patients with metastatic melanoma treated with anti-cytotoxic T-lymphocyte Antigen-4. J Clin Oncol. 2005;23:6043–53. doi: 10.1200/JCO.2005.06.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lutzky J, Wolchok J, Hamid O, et al. Association between immune-related adverse events (irAEs) and disease control or overall survival in patients (pts) with advanced melanoma treated with 10 mg/kg ipilimumab in three phase II clinical trials. J Clin Oncol. 2009;27:15s. (suppl; abstr 9034) [Google Scholar]
- 27.Di Giacomo AM, Danielli R, Calabrò L, et al. Ipilimumab experience in heavily pretreated patients with melanoma in an expanded access program at the University Hospital of Siena (Italy) Cancer Immunol Immunother. 2011;60:467–77. doi: 10.1007/s00262-010-0958-2. [DOI] [PMC free article] [PubMed] [Google Scholar]