Introduction
Radiation proctitis is very difficult to manage and remains an unresolved therapeutic challenge1. It has been reported that following pelvic radiotherapy, 50% of patients develop intestinal symptoms which negatively affect quality of life2. The optimal therapy for this clinical condition has not yet been established1. Despite positive effects in some randomised clinical trials, treatment options such as anti-inflammatory agents, sucralfate, antibiotics, hyperbaric oxygen and argon plasma coagulation are not resolutive in many patients. Tissue regenerative medicine using platelet-derived growth factors (PDGF) exploits the ability of these factors to accelerate normal tissue repair mechanisms via a receptor-mediated pathway, and has been shown to be effective in several cutaneous and mucosal conditions3. We tested a platelet lysate muco-adhesive compound acting as a “drug delivery system” for prolonged in situ release of PDGF4. We report the case of a transfusion-dependent patient in whom we used this possible novel treatment option for post-actinic proctitis.
Case report
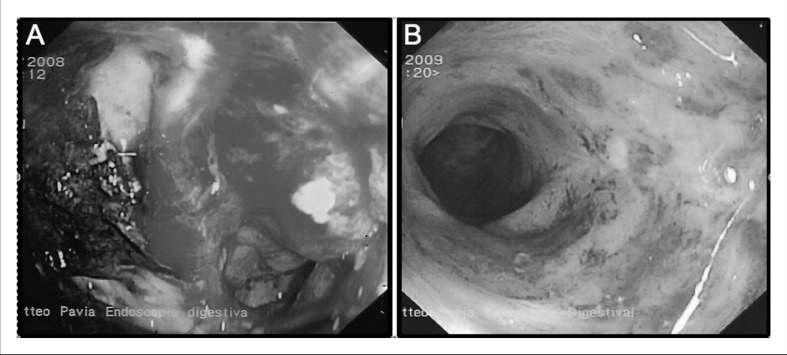
A 69-year old woman was admitted to our hospital in December 2008 with rectal haemorrhage, haematochezia, severe anaemia (Hb 5.7 g/dL) and thrombocytopenia (platelet count 62×109/L). The patient’s medical history included metabolic liver cirrhosis, pulmonary embolism with a caval filter positioned and treatment with sodium enoxaparin (4,000 U/die). The patient had previously undergone radiation therapy (60 Gy) to the pelvis for carcinoma of the uterus followed by intrauterine low-dose rate brachytherapy with 137Cs given the impossibility of performing curative surgery in this woman with a very poor performance status. Rectal haemorrhage was observed 40 days after the end of the radiotherapy. Colonoscopy revealed actinic proctitis (Figure 1A).
Figure 1.
Figure 1A - Spontaneous bleeding of the mucosa in the rectal ampulla, which is completely occupied by coalescent angiodysplasia as from actinic proctitis.
At 10 cm from the anal sphincter there is a giant ulcer with an irregular border. The ulcer is about 5 mm deep in the mucosa and extends about 50% of the circumference of the lumen. The ulcer is almost completely covered by tightly adherent coagulum, and therapeutic endoscopic treatment is impossible. It was not considered prudent to perform biopsies.
Figure 1B - Minimal residual angiodysplasia, with no ulcers.
The heparin was withdrawn and the patient started systemic therapy with mesalazine, octreotide, tranexamic acid, red blood cell (RBC) transfusions (3 units) and local therapy with steroid and mesalazine, with no benefit. Techniques to reduce or stop bleeding, such as argon plasma coagulation and endoscopic thermal treatment were not applicable to this patient because of her poor clinical condition. Since the rectal bleeding continued, despite having suspended heparin treatment, the woman became transfusion-dependent, requiring one RBC unit fortnightly.
We devised a local treatment with a PDGF gel. The gel formulation was chosen to achieve a constant release of growth factors.
Since the patient’s platelet count was very low (because of the liver cirrhosis), it was planned that platelets would be obtained from the peripheral blood of her two sons, provided that their platelet counts were >150×109/L. Informed consent was obtained from both the patient and the potential donors; the latter underwent routine blood donor screening and were found to be suitable.
A 30 mL peripheral blood sample was obtained every 3 days alternately from the two related donors. In parallel, a 3 mL sample was collected to check the blood cells counts which showed that the platelet counts ranged from 200×109/L to 256×109/L in both donors.
The 30 mL blood sample was centrifuged at 1,000 rpm for 10 min and the platelet-rich plasma (PRP) was collected in a syringe under sterile conditions. At the same time, in another syringe, 2 mL of an activator (Plateltex act, Plateltex S.R.O, Praha, CZ), consisting of baxotrobin plus Ca2+ gluconate, was aspirated. To induce local formation of a platelet gel, the PRP and activator were united in a single syringe and manually agitated for 3 minutes (the average time for gel formation is 3–6 minutes). Finally, the syringe was connected to a catheter (10 cm length) with two lateral ports. Afterwards the patient was insufflated in the rectal ampulla lying on a bed and maintaining the same position for 30 minutes to enable adequate adherence of the platelet gel to the rectal mucosa. Starting in March 2009, the gel was applied every 3 days for 2 weeks, and then in alternate weeks thereafter.
The procedures were tolerated extremely well, with no pain or bleeding.
From the third application, bleeding was greatly reduced and the patient did not require additional RBC transfusions (Hb constantly around 9 g/dL). After 12 applications, the clinical picture was completely resolved, Hb stabilised at 11 g/dL and a follow-up colonoscopy (4 months after treatment) documented complete healing of the lesions (Figure 1B). At the 2-year follow-up, the patient was clinically stable, Hb levels were stable and no further transfusions had been required.
Discussion
The optimal therapy of post-radiation proctitis has not yet been established1. Tissue regenerative medicine using PDGF exploits the ability of the growth factors to accelerate normal tissue repair mechanisms via a receptor-mediated pathway, and has been shown to be effective in particular in several cutaneous and mucosal conditions3. We tested a platelet lysate muco-adhesive compound that acts as a “drug delivery system” for prolonged in situ release of PDGF4.
Our original therapeutic approach is encouraging, in view of the excellent compliance to PDGF gel, the rapid and dramatic response (with complete “restitutio ad integrum” and no additional transfusion requirements), safety (particularly if autologous platelets can be used) and low cost. Obviously, these results need to be confirmed in properly designed clinical trials. Finally, we suggest that patients with other conditions could benefit from this approach, for instance patients experiencing severe radiation-induced bladder bleeding because of the need to include the bladder neck in the so-called “high-dose region” or patients with oral mucositis after high-dose chemo/radiotherapy or Graft-versus-Host-disease. PDGF gel has the potential to be a simple and economic option for healing mucosal lesions that are otherwise very difficult to treat5.
Footnotes
The Authors declares no conflicts of interest.
References
- 1.Andreyev HJ, Davidson SE, Gillespie C, et al. Practice guidance on the management of acute and chronic gastrointestinal problems arising as a result of treatment for cancer. Gut. 2012;61:179–92. doi: 10.1136/gutjnl-2011-300563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henson C. Chronic radiation proctitis: issues surrounding delayed bowel dysfunction post-pelvic radiotherapy and an update on medical treatment. Therap Adv Gastroenterol. 2010;3:359–65. doi: 10.1177/1756283X10371558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martinez-Zapata MJ, Marti-Carvajal A, Sola I, et al. Efficacy and safety of the use of autologous plasma rich in platelets for tissue regeneration: a systematic review. Transfusion. 2009;49:44–56. doi: 10.1111/j.1537-2995.2008.01945.x. [DOI] [PubMed] [Google Scholar]
- 4.Sandri G, Bonferoni MC, Ferrari F, et al. An in situ gelling buccal spray containing platelet lysate for the treatment of oral mucositis. Curr Drug Discov Technol. 2011;8:277–85. doi: 10.2174/157016311796799017. [DOI] [PubMed] [Google Scholar]
- 5.Del Fante C, Perotti C, Bonferoni MC, et al. Platelet lysate mucoadhesive formulation to treat oral mucositis in graft versus host disease patients: a new therapeutic approach. AAPS PharmSciTech. 2011;12:893–9. doi: 10.1208/s12249-011-9649-3. [DOI] [PMC free article] [PubMed] [Google Scholar]