Abstract
Background
Women seem more willing to donate blood than men despite the limitations that affect their donation rate. The aim of our study was to determine the role of women in altruistic donation of blood in Huelva, a province in south-western Spain.
Materials and methods
We registered 87,601 offers to donate whole blood between January 1st, 2005 and December 31st, 2009. We statistically analysed variables such as sex, age, offers, deferrals and donations, problems in venous access, vasovagal reactions, weight and blood pressure to establish their significance according to donor gender.
Results
With regards to gender, 52.3% of donors were women and 47.7% men. Of the 87,601 offers to donate blood, 46.5% were from females and 53.5% from males. More females than males made their first donation during the study period. However, 43.9 % of donations were from women, whereas 56.1% were from men. Overall 8.7% of offers were deferred, 62.7% of which due to a low haemoglobin concentration, which was the most frequent cause of deferral in women. Difficulties in venous access and vasovagal reactions were also more frequent in female donors than in male donors. By the end of the study period, donor fidelity was 58.6% for men and 48.6% for women.
Discussion
In the province of Huelva, women are more altruistically inclined than men to give blood, with the percentages of donors and first-time donors being higher among females. However, there are restrictions to women giving blood, especially low haemoglobin concentration, which reduce the number of female blood donations. Women also have more difficulty when blood is withdrawn and are more susceptible to vasovagal reactions, which negatively affect their experience as donors. Measures should be taken to reduce these barriers to encourage women to continue to offer to donate blood, thereby ensuring that they become regular donors, which is a key factor in guaranteeing an adequate supply of blood within the region of Andalusia.
Keywords: female, blood donor, deferral, adverse reactions, fidelity
Introduction
In developed countries only 3 to 8% of subjects aged 18 to 65 years old are blood donors and almost half the units of blood collected come from regular donors1. A review by Ringwald et al. on keys to get donors to continue giving blood showed that there were fewer women than men among regular donors, especially young women under 45, although figures were similar for both sexes aged 45 and older. The main reason cited was pregnancy and the fact that only 42% of women returned to giving blood after childbirth.
Women seem more willing to give blood than men, which is a key factor in maintaining an adequate blood supply, according to Newman’s study2 of donors in south-eastern Michigan (United States of America). He observed that women were 31% more likely to offer to donate blood, a figure that gradually decreased between the ages of 30 and 50, when the numbers began to level off and fall below those for men in the fifth decade. Newman attributed this to the higher rate of temporary deferrals in women, 21% as opposed to 6% in men, mainly due to haemoglobin levels below acceptable limits, and the fact that any deferral itself, albeit for a short time, diminishes the likelihood of donor return, especially if the volunteer is a first-time donor. Slight variations in the accuracy of determining haemoglobin levels can have a marked effect on the temporary exclusion rate for women3 because haemoglobin levels more often do not fall within acceptable limits in females.
In 2009, Misje et al.4 published the results of a study of Norwegian donors, noting that women represented 56% and men 44% of new donors, while the opposite was true among regular donors (46% women, 54% men). They analysed donation patterns over a 6-year period and found that the percentage of donors who gave blood at least once a year was similar in both genders, but only 30% of new women donors had become regular donors by the end of the study period, compared to 41% of men. This difference was evident in donors who were younger than 45, rising to 36% in women compared to 28% of men above that age. Temporary deferrals of new donors were also higher in younger women than in men of a similar age (17% vs 10%) but were more or less equal after the age of 30 (13% of women, 12% of men).
Another factor contributing to the decline in offers from women is that they suffer the adverse effects of blood withdrawal more than men. In another study by Newman et al.5, 1,000 randomly selected donors were questioned about their experience 3 weeks after donating. Among women 9% reported vasovagal reactions, 11.1% fatigue and 12.5% arm discomfort after the procedure as opposed to 4.5%, 4% and 6.9%, respectively, in men. Women are typically lighter than men, and vasovagal reactions and post-donation fatigue appear inversely related to weight5,6.
A recent review by Bani and Giussani7 found that only 32% of women donate blood in Italy, compared to between 43 and 55% in other countries. The Authors analysed various female aspects of donation and noted that the reasons given for not donating included fear of certain components of the collection process such as needles, the sight of blood, possible errors and the feeling of discomfort8, which seem to be more prevalent in women. The tendency to repeat donations was similar in both sexes9, although satisfaction was inversely proportional to the perceived waiting time during the donation process, one variable that influences the return of donors10. Gender is also associated with other difficulties in giving blood, women citing medical reasons and vein issues as significant barriers11. Women more than men also tend to mention the negative effects of blood donation on their physical and emotional well-being12, with women more frequently than men complaining of the vasovagal-type reactions that may occur during or immediately after a donation6,13,14. Donor selection criteria vary at an international level15, but regardless of the location women always give a higher percentage of their blood volume than men, hence there could be a direct relationship between the volume withdrawn, the donor’s total blood volume and the incidence of adverse reactions.
Only in recent years has a gender perspective been applied to scientific studies on blood donation, although many publications have long described results that show clear differences between the sexes, from the willingness to donate to becoming regular donors, all of which unquestionably influences current and future blood supplies.
The aim of our study was to establish whether we could take the donor population at our centre and reproduce the findings of other Authors in terms of gender by classifying donation offers from women as a sample group and donation offers from men as the control group in order to specify the role of women in voluntary blood donations in the province of Huelva. We also aimed to draw attention to the potential barriers in our environment which might impede women from becoming regular donors, in order to implement measures to reduce or eliminate these obstacles.
Materials and methods
Blood and blood components are collected in Andalusia exclusively by a network of Transfusion Centres16,17 that are part of the Health Service of Andalusia. Offers to donate blood can be made at these centres or at special places designed for this purpose, collection points, where people register with the blood team, which usually consists of general practitioners, nurses and other personnel to assemble and transport these mobile installations. The mobile units belonging to the Huelva Transfusion Centre regularly visit different collection points in the capital and the province, and the blood obtained at these points represents 82% of the total blood collected, with the remaining 18% obtained at the Centre.
The study population comprised all people who offered to make a whole blood donation at the Huelva Transfusion Centre between January 2005 and the end of December 2009 who were registered in the PROGESA computer database (Mak System, Paris, France). Information regarding donations or deferrals was obtained by extracting Access format files for later analysis. Since the study used data that did not identify individual donors by name, there was no need to seek the approval of the Clinical Ethics Committee, although approval was asked of and granted by the Subcommittee on Health Research at the Hospital Juan Ramón Jiménez in Huelva. Testing for data was carried out on a random sample of 1% of the original records on paper.
During the study period, a total of 87,601 whole blood donation offers were registered from 20,998 donors, which represented 6.3% of the population aged between 18 and 65 years during that period. The criteria for acceptance or deferral of offers in Andalusia are regulated by national law18, following European Union guidelines19,20 and recommendations from the Council of Europe21. The basic criteria for blood donation with particular reference to gender differences are a weight ≥ 50 kg (≈110 lb), a haemoglobin level ≥7.8 mmol/L in women and ≥8.4 mmol/L in men, and 6 months having passed since a miscarriage, abortion or childbirth in women. All donations are preceded by an interview and health check including heart rate (donor deferred if >110 bpm or <50 bpm except in athletes) and blood pressure (donor deferred if systolic blood pressure >180 mmHg or <90 mmHg or diastolic blood pressure >100 mmHg or <50 mmHg) measured with an electronic tensiometer (OMRON Healthcare Europe, London, UK) which is validated and regularly checked. The recorded weight was expressed verbally by the donor at the time of the interview. Haemoglobin concentration was only determined in potential donors who successfully passed this interview.
During the study period the pre-donation haemoglobin concentration was determined from a sample of capillary blood obtained by pricking the fingertip, using portable haemoglobinometers (HemoCue® 201/301, Ängelhom, Sweden), validated against a Coulter analyzer® Ac. T 5 Diff AL (Beckman Coulter Inc., Miami, Florida, USA), calibrated regularly and periodically checked by external quality controls. The haemoglobinometers were tested weekly for accuracy of results according to the manufacturer’s instructions, with controls of known values and recalibrated if necessary.
The volume of blood withdrawn was set at 470 mL + 25 mL for testing; the minimum interval between withdrawals was 2 months with a maximum of three donations a year for women and four donations a year for men18,21.
Data retrieved from the database for analysis were related to sex, age, weight, systolic and diastolic blood pressure, number of offers, number of donations, offers deferred following medical interview, offers deferred due to haemoglobin levels less than legally established limits (low Hb), problems with venipuncture and vasovagal-type reactions during or after blood extraction, classified as mild (pallor, sweating, anxiety), moderate (plus loss of consciousness, hypotension) or severe (plus vomiting, seizures, incontinence). For the purposes of statistical analysis the donor’s age was classified into one of five groups: 10–30, 31–40, 41–50, 51–60 and >60 years. For donor fidelity a study group was formed of those who made a donation in 2005, differentiated by gender and whether they were new (first-time donor in 2005) or regular donors (any donation made before 2005).
The chi-square test was used to establish the significance of the different variables according to donor gender. ANOVA was used to determine whether there were significant differences between men and women in the variables, and the odds ratio (OR) was applied to measure differences in the probability of occurrence of events in either gender. Analyses were performed using the SPSS v13 IBM (IBM, Madrid, Spain) statistical package. The results were considered statistically significant when the p value was <0.05.
Results
Of the 20,998 donors 52.3% were female and 47.7% were male, who made a total of 87,601 donation offers during the study period. Only 19,916 effectively made a donation during the period, of whom 10,220 (51.3%) were female and 9,696 (48.7%) were male. Table I shows that the percentage of offers was higher by males than by females, except in the group of subjects aged 18 to 30 years old, in which a higher proportion of women offered to donate. The overall difference was statistically significant (P <0.001). Comparing the age distribution of the first offer by donors of both sexes (Table II) showed a higher overall frequency of women than men (4,333 to 3,651, P <0.05, OR=1.36), with the difference being statistically significant, except in donors between 31 and 40 years old, in whom there was a slight predominance of male donors. Table III presents the distribution of donations from both sexes, showing that there were significantly more donations from men (p <0.001) except in the 18 to 30 year old age group, in which more donations were made by women.
Table I.
Distribution of blood donation offers by age and sex of the potential donors.
| Age (years) | Women | % | Men | % | Total | % |
|---|---|---|---|---|---|---|
| 18–30 | 8,805 | 10.1 | 6,421 | 7.3 | 15,226 | 17.4 |
| 31–40 | 11,301 | 12.9 | 14,053 | 16.0 | 25,354 | 28.9 |
| 41–50 | 12,326 | 14.1 | 15,038 | 17.2 | 27,364 | 31.3 |
| 51–60 | 5,861 | 6.7 | 7,962 | 9.1 | 13,823 | 15.8 |
| >60 | 2,463 | 2.8 | 3,371 | 3.8 | 5,834 | 6.6 |
|
| ||||||
| Total | 40,756 | 46.5 | 46,845 | 53.5 | 87,601 | 100 |
Table II.
Distribution of first blood donation offers by age and sex of the potential donors.
| Age (years) | Women | % | Men | % | Total | % |
|---|---|---|---|---|---|---|
| 18–30 | 1,980 | 24.8 | 1,398 | 17.5 | 3,378 | 42.3 |
| 31–40 | 1,093 | 13.7 | 1,183 | 14.8 | 2,276 | 28.5 |
| 41–50 | 785 | 9.8 | 685 | 8.6 | 1,470 | 18.4 |
| 51–60 | 397 | 5.0 | 312 | 3.9 | 709 | 8.9 |
| >60 | 78 | 1.0 | 73 | 0.9 | 151 | 1.9 |
|
| ||||||
| Total | 4,333 | 54,3 | 3,651 | 45.7 | 7,984 | 100 |
Table III.
Distribution of donations by age and sex of the donors.
| Age (years) | Women | % | Men | % | Total | % |
|---|---|---|---|---|---|---|
| 18–30 | 7,639 | 9.5 | 6,213 | 7.8 | 13,852 | 17.3 |
| 31–40 | 9,759 | 12.2 | 13,565 | 17.0 | 23,324 | 29.2 |
| 41–50 | 10,458 | 13.1 | 14,428 | 18.1 | 24,886 | 31.2 |
| 51–60 | 5,187 | 6.5 | 7,523 | 9.4 | 12,710 | 15.9 |
| >60 | 2,119 | 2.6 | 3,084 | 3.8 | 5,203 | 6.4 |
|
| ||||||
| Total | 35,162 | 43.9 | 44,813 | 56,1 | 79,975 | 100 |
Overall, 7,626 offers to donate were deferred (8.7% of total offers): 2,844 (37.3% of deferrals) were decided during the medical interview and 4,782 (62.7% of deferrals) were due to low Hb. Women accounted for 73.3% of all deferrals and men for only 26.7%.
Of the 2,844 donors deferred on the basis of the medical interview, 53% were women and 47% men. Table IV presents the distribution of these deferrals by age and sex, showing that they more frequent in women between 18 and 40 years, more or less equally common in men and women between 40 and 50 years old and less common in women than in men from the age of 50 onwards. The chi-square test (P =0.240) and ANOVA (P =0.529) showed no significant differences between men and women, although there was a slight predominance in females, with an OR=1.29.
Table IV.
Distribution of deferrals by age and sex of the potential donors based on the medical interview.
| Age (years) | Women | % | Men | % | Total | % |
|---|---|---|---|---|---|---|
| 18–30 | 353 | 12.4 | 168 | 5.9 | 521 | 18.3 |
| 31–40 | 395 | 13.9 | 336 | 11.8 | 731 | 25.7 |
| 41–50 | 368 | 12.9 | 364 | 12.8 | 732 | 25.7 |
| 51–60 | 238 | 8.4 | 279 | 9.8 | 517 | 18.2 |
| >60 | 152 | 5.4 | 191 | 6.7 | 343 | 12.1 |
|
| ||||||
| Total | 1,506 | 53.0 | 1,338 | 47.0 | 2,844 | 100 |
Table V shows the main causes of deferral at the medical interview stage; the listed causes constitute 72.8% of the total. The most frequent causes were minor infections, donor discomfort, endoscopies and skin piercing, drug treatment or hypertension at the time of exploration (together accounting for 51% of all deferrals determined by the medical interview, data not shown). Deficiency anaemias, having exceeded the maximum number of annual donations, hypotension and malaise were more common in females than in males (371 vs 163, respectively; OR =2.61). Furthermore, some causes of deferral, such as pregnancy and childbirth, were unique to the females. Among males the most frequent causes for deferral were surgery, risky sexual behaviour, drug or alcohol consumption and high blood pressure (268 vs 108 in females; OR =2.15), the last being a significantly more common cause in men than in women (149 vs 34, respectively; OR =3.81).
Table V.
Major medical reasons for deferral.
| Reason for deferral | Women | % | Men | % | Total | % |
|---|---|---|---|---|---|---|
| Deficiency anaemias | 70 | 2.5 | 14 | 0.5 | 84 | 3.0 |
| Major surgery | 46 | 1.6 | 56 | 2.0 | 102 | 3.6 |
| Minor surgery | 23 | 0.8 | 32 | 1.1 | 55 | 1.9 |
| High-risk behaviour | 5 | 0.2 | 22 | 0.8 | 27 | 1.0 |
| Drugs or alcohol consumer | 0 | 0.0 | 9 | 0.3 | 9 | 0.3 |
| >3 or >4 donations in a year | 89 | 3.1 | 10 | 0.4 | 99 | 3.5 |
| Pregnancy or lactation | 34 | 1.2 | NA* | 0.0 | 34 | 1.2 |
| Endoscopy, tattoo, piercing, etc. | 158 | 5.5 | 142 | 5.0 | 300 | 10.5 |
| Fever, mild infections | 217 | 7.6 | 221 | 7.8 | 438 | 15.4 |
| Hypotension | 30 | 1.1 | 7 | 0.2 | 37 | 1.3 |
| Malaise, unwell | 182 | 6.4 | 132 | 4.6 | 314 | 11.0 |
| Delivery, miscarriage | 63 | 2.2 | NA* | 0.0 | 63 | 2.2 |
| Unreliable answers | 2 | 0.1 | 10 | 0.4 | 12 | 0.5 |
| Tachycardia or bradycardia | 45 | 1.6 | 58 | 2.0 | 103 | 3.6 |
| Blood pressure >180 or >110 mmHg | 34 | 1.2 | 149 | 5.2 | 183 | 6.4 |
| Taking medication | 112 | 3.9 | 98 | 3.5 | 210 | 7.4 |
|
| ||||||
| Total | 1,110 | 39 | 960 | 33.8 | 2,070 | 72.8 |
Not applicable
Given the large difference between the sexes, we analysed deferrals for low Hb separately. Of the 4,782 offers deferred for this reason, 4,088 (85.5%) were from women, accounting for 73% of all causes of non-collection in women, and 694 (14.5%) were from men, representing only 34% of all causes of deferral in males. Table VI shows these deferrals divided by age and sex of the potential donors; the differences are quite striking up to 50 years old (3,460 vs 438; OR =9.07), and then decrease significantly after this age (628 vs 256, respectively; OR =2.81). The chi-square test (P <0.001) and ANOVA (P <0.001) showed that the overall difference was statistically significant, with a predominance of this type of deferral in women (OR =6.77).
Table VI.
Distribution of deferrals because of low Hb by age and sex of the potential donors.
| Age (years) | Women | % | Men | % | Total | % |
|---|---|---|---|---|---|---|
| 18–30 | 813 | 17.0 | 40 | 0.9 | 853 | 17.9 |
| 31–40 | 1,147 | 24.0 | 152 | 3.2 | 1,299 | 27.2 |
| 41–50 | 1,500 | 31.4 | 246 | 5.1 | 1,746 | 36.5 |
| 51–60 | 436 | 9.1 | 160 | 3.3 | 596 | 12.4 |
| >60 | 192 | 4.0 | 96 | 2.0 | 288 | 6.0 |
|
| ||||||
| Total | 4,088 | 85.5 | 694 | 14.5 | 4,782 | 100 |
Concerning the problem of venous access for blood collection, of 79,975 donations made during the study period, 1,200 (1.5%) were found to be underweight units as a result of venipuncture difficulties, according to data recorded by the nursing staff. Of these 1,200 units 813 (67.7%) were from women and 387 (32.3%) from men (OR =2.67). We also found a significant difference between women and men in vasovagal-type adverse reactions: 426 vasovagal reactions occurred in 79,916 donations (0.53%), of which 271 occurred in women and 155 in men (P <0.05; OR =2.23).
A comparative analysis of blood pressure in both genders was performed only for donors who made donations, excluding 66 empty records. There were significant differences between men and women in systolic blood pressure (12.95±1.33 mmHg in men vs 12.17±1.32 mmHg in women, P <0.05) and diastolic blood pressure (8.16±0.91 mmHg in men vs 7.58±0.89 mmHg in women, P <0.05), both of which were higher in men than in women. The weight recorded for donors, excluding 123 empty records, also revealed significant differences between the two genders (83.7±12.3 kg in men vs 67.1±11.4 kg in women, P <0.05), with men unsurprisingly being heavier than women.
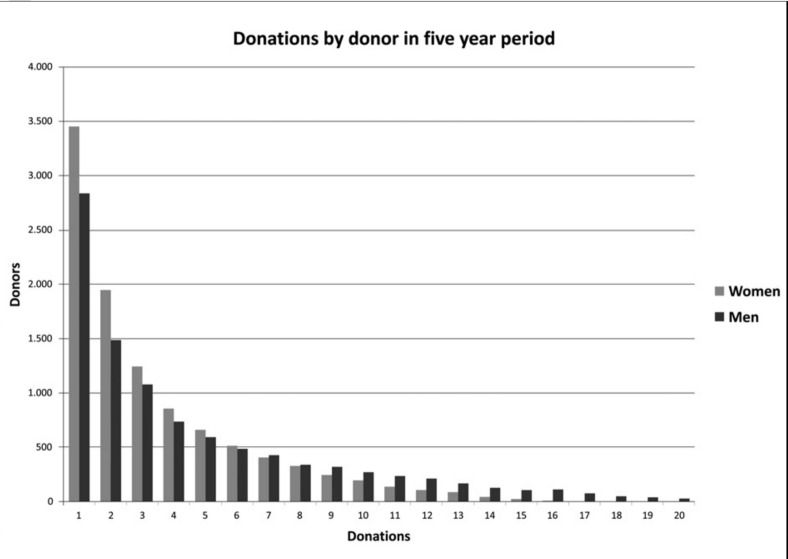
We also found differences between the genders in the commitment of donors to give blood. Of the 19,916 donors who donated during the study period, the average number of donations made by both sexes across all age ranges was higher for men (4.6 vs 3.4), especially after the age of 30 (Table VII). When analysing the total number of donations per donor during the study period (Figure 1) we found that women predominate up to the sixth donation while a higher number of men gave blood from the 7th to the 15th donations. Only 20 women made the maximum 15 allowable donations and only 27 men made the maximum allowable 20 donations during the study period.
Table VII.
Number of donations made during the study period divided according to age and sex of the donors.
| Age (years) | Women | Average | Men | Average | Total | Average |
|---|---|---|---|---|---|---|
| 18–30 | 7,639 | 2.6 | 6,213 | 3.1 | 13,852 | 2.8 |
| 31–40 | 9,759 | 3.3 | 13,565 | 4.4 | 23,324 | 3.8 |
| 41–50 | 10,458 | 4.1 | 14,428 | 5.5 | 24,886 | 4.8 |
| 51–60 | 5,187 | 4.1 | 7,523 | 5.3 | 12,710 | 4.7 |
| >60 | 2,119 | 4.2 | 3,084 | 5.7 | 5,203 | 5.0 |
|
| ||||||
| Total | 35,162 | 3.4 | 44,813 | 4.6 | 79,975 | 4.0 |
Figure 1.
Number of donations per donor in the 5-year study period.
The number of active donors decreased progressively during the study period, so that after 5 years only 52.9% of the initial donors from 2005 were still donating (Table VIII). Of the initial donors, 46.8% of the women continued to donate, compared to 58.6% of men. We found a significant difference in fidelity between first-time donors and donors who had made donations prior to the start of the study, since of the donors who made their first donation in 2005 only 34.7% remained active in 2009 (31.8% of women vs 38.1% of men, data not shown), this decrease being more marked in the 18 to 30 age group (26.3% fidelity, data not shown). On the other hand, of the donors who had made donations prior to 2005, 56.1% were still donating in 2009 (49.8% of women vs 61.9% of men, data not shown).
Table VIII.
Donor’s fidelity during the study period.
| 2005 | 2006 | 2007 | 2008 | 2009 | Fidelity (%) | |
|---|---|---|---|---|---|---|
| All | 8,617 | 5,545 | 5,013 | 4,600 | 4,555 | 52.9 |
| Women | 4,191 | 2,471 | 2,225 | 1,996 | 1,961 | 46.8 |
| Men | 4,426 | 3,074 | 2,788 | 2,604 | 2,594 | 58.6 |
| First donors | 1,313 | 685 | 572 | 482 | 456 | 34.7 |
| Repeated donors | 7,304 | 4,860 | 4,441 | 4,118 | 4,099 | 56.1 |
Discussion
The rate of whole blood donation in the province of Huelva in 2009 was 36.72 per thousand inhabitants per year, with regular donors representing 2.7% of the population aged 18 to 65 years; these figures are similar to those presented by Ringwald et al1. Of the 20,998 donors who donated during the study period, 52.3% were women and 47.7% were men. Studies vary in terms of donor distribution by sex, with a predominance of women2,4,22,23 in some while others show a prevalence of men9,24,25, although the differences were small except in one particular case7.
However, of the 87,601 donation offers 46.5% were from females and 53.5% were from males (Table I) although the proportion of men was lower than that of women in the 18 to 30 year-old age range (10,1% vs 7.3%). These findings are also consistent with those of other studies2,4,9, with a greater number of offers from women up to the age of 30, followed by a fall until offer levels are similar after the age of 50. When analysing the age at which the donors in our study made their first donation offer (Table II), we, like Misje et al.4, found an overall prevalence of women which was statistically significant (P <0.05).
Several studies have found that women have a stronger tendency to donate blood voluntarily2,4,26–30, with female donors seeming to be more altruistic in this sense and possess stronger moral norms and cognitive attitudes towards blood donation31. However, this predisposition of women to donate blood is not reflected in the number of donations that are actually made because, as shown in Table III, the total number of units collected is higher in men than in women (P <0.001), although women between 18 and 30 years old provided more units of whole blood than men during the study period, which again indicates that they are initially more predisposed to donate blood.
The lower number of annual donations by women in Spain represents a 25% reduction in their contribution to the nation’s blood supply in relation to men. Limitations on female blood donation aimed at protecting women’s health add to other obstacles related to gender factors or conditions more frequently associated with women, as we will review below.
There were 7,626 rejections of offered donations, representing 8.7% of total offers, of which 37.3% were due to deferrals arising from the medical interview and 62.7% because of low Hb. Deferrals resulting from the medical interview (Table IV) were more frequent in women than in men (53% vs 47%), confirming findings already reported by other Authors32–35, although the causes varied in the two sexes and according to age. In our case more women were deferred up to the age of 40 with the figures levelling out by the age of 50 and falling thereafter; these differences were not statistically significant, despite a slight overall female predominance.
The most common medical causes for deferral, excluding low Hb (Table V), were mild infection, donor feeling unwell, endoscopy and skin piercing, drug treatment and hypertension registered when taking the donor’s blood pressure. A deficiency anaemia, having exceeded the maximum number of annual donations, hypotension and malaise were almost three times more common in women, in addition to factors unique to the female gender such as pregnancy and childbirth. Among men the most frequent reasons for deferral were recent surgery, risky sexual behaviour, drug-taking or alcohol consumption and high blood pressure at the time of the examination, this last factor being almost four times more frequent in men than in women.
It should, however, be noted that we cannot accurately establish the number of women who did not offer to make donations due to pregnancy or after childbirth and during breastfeeding, either because they were not summoned to the collection points for these reasons (in the case of regular donors) or because many women already knew they could not donate for the duration of these ante- and post-natal processes. Moreover, as a result of our information campaigns, other conditions, such as weight below 50 kg (≈110 lb), are widely known by the general public to lead to deferral, making it impossible to specify the number of people (mostly women) who might not have offered to give blood for this reason.
As found in many studies, deferrals due to haemoglobin levels below the established limits are much more common in women, although the figures vary depending on the donors’ demographic characteristics32–38. In our study the leading cause of deferral was low Hb, which was more prevalent in women than in men (85.5% vs 14.5%, respectively; P <0.001, OR =6.77), although less than reported in some recent studies36,37.
We observed that offers deferred due to low Hb in women increased progressively with age, from 17% among 18 to 30 year olds to 31.4% among 41 to 50 years old, and then decreased to 9.1% in the 51 to 60 age group and to 4% in women older than 60 years of age. These results can be compared with those of a study published in 2010 by Mast et al.36, who considered some 715,000 donation and found that the frequency of deferrals because of low Hb was similar in women of all age groups between 18 and 50 (18.2–21.7%), while also noting that the number of deferrals as a result of low Hb in young women was approximately 25% higher than in postmenopausal women between 51 and 60 years old, although the deferral rate because of low Hb was still five times higher in this group of women than in men of the same age. In our case, the rate of deferral due to low Hb was nearly three times higher in women between 51 and 60 years old than in men of the same age, and only twice as high as that in men from 60 years onwards.
In their study of 116,165 donation offers, Custer et al.35 also observed a higher frequency of deferrals because of low Hb among women aged 16 to 54, with nearly twice as many cases in this group as in young women in the narrower age group of 16 to 24 year-olds, and then a decline after 55 years old. These Authors also found that deferrals for low Hb were twice as frequent in regular donors as in new donors, mainly because of an increased incidence of deferrals for this reason among regular female donors over 25 years old compared to among new donors of the same age (a ratio of 2.4 to 1). In our study we also found that deferrals for low Hb were almost twice as frequent in regular female donors than in new donors, especially between 18 and 40 year-olds (data not shown).
Given these results, we believe that short-term measures should be implemented to prevent and/or correct the iron deficiency in women induced by whole blood donations, in order that they maintain their levels of voluntary blood donations without impairing their health39–44.
The problem of venous access in blood donation, described as being more common in women32, may result in units that are underweight and unsuitable for component separation. We found that 1.5% of collections were underweight, of which about two-thirds (67.7%) were from female donors and one-third (32.3%) from male donors. Custer et al.35 found that 3.7% of 100,141 whole blood donations were underweight, and that this problem was more common for units from young donors, female donors and first-time donors.
There is also the problem of adverse reactions, especially of the vasovagal type, to blood donation. During the study period 0.53% of the donors had vasovagal reactions to blood collection: almost two-thirds of these reactions occurred in female donors and about one-third in males (P <0.05, OR =2.23). In a study of 554,534 whole blood donations at 15 US centres, Bravo et al.45 found an overall incidence of loss of consciousness during or after the donation of 0.27%, with 72.7% of cases occurring in women. A study by Kamel et al.46 of some 800,000 donations of whole blood and apheresis found a 0.41% incidence of moderate and severe vasovagal reactions, with women accounting for 75% of cases and men for the other 25%.
Other studies also corroborate the higher frequency of vasovagal reactions and other adverse effects of blood donation in women, with the rate being two or three times higher in women than in men5,6,12–14,45–49. That said, the difference in vasovagal reactions in one study was almost negligible when donors of both sexes weighting less than 150 lb were excluded, because the Authors considered that low weight was the main reason for the higher incidence of reactions in women14. In our study we found a significant difference in donor weight, which was lower in females; 67.8% of women who had a vasovagal reaction weighted less than 68 kg (≈150 lb), compared to only 12.2% of men who had this type of adverse effect (data not shown).
This higher rate of the adverse effects of blood donation in female donors appears to be related to factors that are more common in women, such as lower weight and blood pressure. Low systolic or diastolic blood pressure is associated with potential vasovagal reactions47, which adds to differences in the regulatory mechanisms of blood pressure between men and women50,51, which may explain at least in part the higher incidence of vasovagal reactions in women, along with other more complex physiological and emotional aspects46,52. In our study we also found significant differences in systolic and diastolic blood pressure values between the sexes, which were lower in women than men.
We plan to incorporate measures to reduce the frequency of vasovagal reactions in susceptible donors, selecting those measures that are compatible with our work system and with the studies that scored the best results in this subject matter53–58, such as water intake prior to collection of the blood and/or applying muscle tension during the collection59–65.
The consequences of the barriers that women face in relation to whole blood donation are reflected in the typical female donor career recorded throughout our 5-year study. The percentage of whole blood donations made by women in this period (Table III) was 12.2% lower than that made by men, and although there were almost 5% more female donors than male donors, the mean number of donations from males during the period was higher than the mean number from women (4.6 vs 3.4, Table VII) in all age groups, especially after 40 years old.
The greater predisposition of women to donate blood was, however, confirmed because up to the sixth donation women were more numerous than men (Figure 1), with the number of men donating blood only become superior after the seventh donation. These results are similar to those of Misje et al.4. The maximum number of possible donations over the 5 years, representing full donor fidelity, was made by only 20 women (15 donations) and 27 men (20 donations).
The donor fidelity recorded at the end of the study period was also different. The number of men and women who were active donors fell progressively (Table VIII) to 52.9% of registered donors in the first year. Of these active donors, 58.6% were men and 46.8% were women, again indicating the difficultly that women have in remaining regular donors. The cessation of donations was higher in those who donated for the first time in 2005 than in those who had donated before (34.7% vs 56.1%), with the percentage of women who continued donating being lower in both groups (31.8% and 49.8% for first-time female donors vs repeat female donors, and 38.1% and 61.9% for first-time male donors and repeat male donors, respectively; data not shown). Results similar to ours were published by Misje et al.4, who found, in a study of 17,812 registered donors in Oslo (Norway) in 1999, that donor fidelity over 6 years was higher in men, and fidelity among regular donors was higher than that of first-time donors. In this study, 35% of first-time donors went on to become regular donors.
Conclusions
The first conclusion of our study is that in the province of Huelva women are more willing than men to donate blood as an act of altruism, as evidenced by the fact that there were more women than men among the group of donors analysed; a greater number of women made their first donation during this same period, the donations by women between 18 and 30 years old exceeded those of men, and more women than men gave blood up to the sixth donation during the 5 years analysed.
Secondly, it is important to incorporate more women in the group of regular donors by reducing the obstacles that prevent them from donating: this can be done by preventing iron deficiency induced by whole blood donations in women and curtailing the adverse reactions to donation by introducing measures to offset these reactions.
These actions will undoubtedly result in a greater contribution to the blood supply by women, which according to the data from the study period could boost the number of whole blood units by as much as 5%, but most importantly would allow more women to become regular donors, consistent with their greater predisposition to voluntarily giving blood, and would also improve their wellbeing as donors.
Footnotes
The Authors declare no conflicts of interest.
References
- 1.Ringwald J, Zimmermann R, Eckstein R. Keys to open the door for blood donors to return. Transfus Med Rev. 2010;24:295–304. doi: 10.1016/j.tmrv.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Newman BH. Adjusting our management of female blood donors: the key to an adequate blood supply. Transfusion. 2004;44:591–6. doi: 10.1111/j.0041-1132.2004.04014.x. [DOI] [PubMed] [Google Scholar]
- 3.Eder A, Goldman M, Rossmann S, et al. Selection criteria to protect the blood donor in North America and Europe: past (dogma), present (evidence), and future (hemovigilance) Transfus Med Rev. 2009;23:205–20. doi: 10.1016/j.tmrv.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Misje AH, Bosnes V, Heier HE. Gender differences in presentation rates, deferrals and return behaviour among Norwegian blood donors. Vox Sang. 2010;98:e241–8. doi: 10.1111/j.1423-0410.2009.01267.x. [DOI] [PubMed] [Google Scholar]
- 5.Newman BH, Pichette S, Pichette D, Dzaka E. Adverse effects in blood donors after whole-blood donation: a study of 1000 blood donors interviewed 3 weeks after whole-blood donation. Transfusion. 2003;43:598–603. doi: 10.1046/j.1537-2995.2003.00368.x. [DOI] [PubMed] [Google Scholar]
- 6.Trouern-Trend JJ, Cable RG, Badon SJ, et al. A case-controlled multicenter study of vasovagal reactions in blood donors: influence of sex, age, donation status, weight, blood pressure, and pulse. Transfusion. 1999;39:316–20. doi: 10.1046/j.1537-2995.1999.39399219291.x. [DOI] [PubMed] [Google Scholar]
- 7.Bani M, Giussani B. Gender differences in giving blood: a review of the literature. Blood Transfus. 2010;8:278–87. doi: 10.2450/2010.0156-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bednall TC, Bove LL. Donating blood: a meta-analytic review of self-reported motivators and deterrents. Transfus Med Rev. 2011;25:317–34. doi: 10.1016/j.tmrv.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Schreiber GB, Sharma UK, Wright DJ, et al. for the Retrovirus Epidemiology Donor Study. First year donation patterns predict long term commitment for first time donors. Vox Sang. 2005;88:114–21. doi: 10.1111/j.1423-0410.2005.00593.x. [DOI] [PubMed] [Google Scholar]
- 10.McKeever T, Sweeney MR, Staines A. An investigation of the impact of prolonged waiting times on blood donors in Ireland. Vox Sang. 2006;90:113–8. doi: 10.1111/j.1423-0410.2006.00734.x. [DOI] [PubMed] [Google Scholar]
- 11.Schreiber GB, Schlumpf KS, Glynn SA, et al. Convenience, the bane of our existence, and other barriers to donating. Transfusion. 2006;46:545–53. doi: 10.1111/j.1537-2995.2006.00757.x. [DOI] [PubMed] [Google Scholar]
- 12.Hinrichs A, Picker SM, Schneider A, et al. Effect of blood donation on well-being of blood donors. Transfus Med. 2008;18:40–8. doi: 10.1111/j.1365-3148.2007.00805.x. [DOI] [PubMed] [Google Scholar]
- 13.Newman BH, Satz SL, Janowicz NM, Siegfried BA. Donor reactions in high-school donors: the effects of sex, weight, and collection volume. Transfusion. 2006;46:284–8. doi: 10.1111/j.1537-2995.2006.00713.x. [DOI] [PubMed] [Google Scholar]
- 14.Newman BH. Vasovagal reactions in high school students: findings relative to race, risk factor synergism, female sex, and non-high school participants. Transfusion. 2002;42:1557–60. doi: 10.1046/j.1537-2995.2002.00238.x. [DOI] [PubMed] [Google Scholar]
- 15.Karp JK, King KE. International variation in volunteer whole blood donor eligibility criteria. Transfusion. 2010;50:507–13. doi: 10.1111/j.1537-2995.2009.02392.x. [DOI] [PubMed] [Google Scholar]
- 16.Consejería de Salud y Consumo. Orden de 27 de julio de 1984, de creación del programa sectorial de hemoterapia en Andalucía. Boletín Oficial de la Junta de Andalucía. 1984;84:1783. [Google Scholar]
- 17.Consejería de Salud y Consumo. Orden de 6 de junio de 1986, por la que se regula la red transfusional de Andalucía. Boletín Oficial de la Junta de Andalucía. 1986;58:2102–4. [Google Scholar]
- 18.Ministerio de Sanidad y Consumo. Spain. Real Decreto 1088/2005, de 16 de septiembre, por el que se establecen los requisitos técnicos y condiciones mínimas de la hemodonación y de los centros y servicios de transfusión. Boletín Oficial del Estado. 2005;225:31288–304. [Google Scholar]
- 19.Consejo de Europa. Directiva 2002/98/CE del Parlamento Europeo y del Consejo de 27 de enero de 2003 por la que se establecen normas de calidad y de seguridad para la extracción, verificación, tratamiento, almacenamiento y distribución de sangre humana y sus componentes. Diario Oficial de la Unión Europea. 2003;L 33:30–8. [Google Scholar]
- 20.Consejo de Europa. Directiva 2004/33/CE de la Comisión de 22 de marzo de 2004 por la que se aplica la Directiva 2002/98/CE del Parlamento Europeo y del Consejo en lo que se refiere a determinados requisitos técnicos de la sangre y los componentes sanguíneos. Diario Oficial de la Unión Europea. 2004;L 91:25–39. [Google Scholar]
- 21.Council of Europe. Guide to the preparation, use and quality assurance of blood components. European Directorate for the Quality of Medicine & HealthCare. 2008:71. [Google Scholar]
- 22.Gillespie TW, Hillyer CD. Blood donors and factors impacting the blood donation decision. Transfus Med Rev. 2002;2:115–30. doi: 10.1053/tmrv.2002.31461. [DOI] [PubMed] [Google Scholar]
- 23.Alessandrini M. Community volunteerism and blood donation: altruism as a lifestyle choice. Transfus Med Rev. 2007;21:307–16. doi: 10.1016/j.tmrv.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Veldhuizen IJ, Doggen CJ, Atsma F, De Kort WL. Donor profiles: demographic factors and their influence on the donor career. Vox Sang. 2009;97:129–38. doi: 10.1111/j.1423-0410.2009.01201.x. [DOI] [PubMed] [Google Scholar]
- 25.Schlumpf KS, Glynn SA, Schreiber GB, et al. for the National Heart, Lung, and Blood Institute Retrovirus Epidemiology Donor Study. Factors influencing donor return. Transfusion. 2008;48:264–72. [Google Scholar]
- 26.Glyn SA, Kleinman SH, Schreiber GA, et al. Motivations to donate blood: demographics comparison. Transfusion. 2002;42:216–25. doi: 10.1046/j.1537-2995.2002.00008.x. [DOI] [PubMed] [Google Scholar]
- 27.Hupfer ME, Taylor DW, Letwin JA. Understanding Canadian students motivations and beliefs about giving blood. Transfusion. 2005;45:149–61. doi: 10.1111/j.1537-2995.2004.03374.x. [DOI] [PubMed] [Google Scholar]
- 28.Hupfer ME. Helping me, helping you - self-referencing and gender roles in donor advertising. Transfusion. 2006;46:996–1005. doi: 10.1111/j.1537-2995.2006.00834.x. [DOI] [PubMed] [Google Scholar]
- 29.Steele WR, Schreiber GB, Guiltinan A, et al. for the Retrovirus Epidemiology Donor Study. The role of altruistic behavior, empathetic concern, and social responsibility motivation in blood donation behavior. Transfusion. 2008;48:43–54. doi: 10.1111/j.1537-2995.2007.01481.x. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen DD, DeVita DA, Hirschler NV, Murphy EL. Blood donor satisfaction and intention of future donation. Transfusion. 2008;48:742–8. doi: 10.1111/j.1537-2995.2007.01600.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferguson E, Atsma F, de Kort W, Veldhuizen I. Exploring the pattern of blood donor beliefs in first-time, novice, and experienced donors: differentiating reluctant altruism, pure altruism, impure altruism, and warm glow. Transfusion. 2012;52:343–355. doi: 10.1111/j.1537-2995.2011.03279.x. [DOI] [PubMed] [Google Scholar]
- 32.Shaz BH, James AB, Hillyer KL, et al. Demographic variations in blood donor deferrals in a major metropolitan area. Transfusion. 2010;50:881–7. doi: 10.1111/j.1537-2995.2009.02501.x. [DOI] [PubMed] [Google Scholar]
- 33.Custer B, Schlumpf K, Simon TL, et al. for the NHLBI Retrovirus Epidemiology Donor Study-II (REDS-II) Demographics of successful, unsuccessful and deferral visits at six blood centers over a 4-year period. Transfusion. 2012;52:712–21. doi: 10.1111/j.1537-2995.2011.03353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.James AB, Hillyer CD, Shaz BH. Demographic differences in estimated blood donor eligibility prevalence in the United States. Transfusion. 2012;52:1050–61. doi: 10.1111/j.1537-2995.2011.03416.x. [DOI] [PubMed] [Google Scholar]
- 35.Custer B, Johnson ES, Sullivan SD, et al. Quantifying losses to the donated blood supply due to donor deferral and miscollection. Transfusion. 2004;44:1417–26. doi: 10.1111/j.1537-2995.2004.04160.x. [DOI] [PubMed] [Google Scholar]
- 36.Mast AE, Schlumpf KS, Wright DJ, et al. for the NHLBI Retrovirus Epidemiology Donor Study-II. Demographic correlates of low hemoglobin deferral among prospective whole blood donors. Tranfusion. 2010;50:1794–802. doi: 10.1111/j.1537-2995.2010.02649.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oliveira CdL, Martins G, Custer B, et al. Hierarchical analysis of anaemia deferral in blood donor candidates: the individual in the population perspective. Transfus Med. 2011;21:371–7. doi: 10.1111/j.1365-3148.2011.01110.x. [DOI] [PubMed] [Google Scholar]
- 38.Cable RG, Glynn SA, Kiss JE, et al. for the NHLBI Retrovirus Epidemiology Donor Study-II (REDS-II) Iron deficiency in blood donors: analysis of enrollment data from the REDS-II Donor Iron Status Evaluation (RISE) study. Transfusion. 2011;51:511–22. doi: 10.1111/j.1537-2995.2010.02865.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bianco C, Brittenham G, Gilcher RO, et al. Maintaining iron balance in women blood donors of childbearing age: summary of a workshop. Transfusion. 2002;42:798–805. doi: 10.1046/j.1537-2995.2002.00103.x. [DOI] [PubMed] [Google Scholar]
- 40.Newman B. Iron depletion by whole-blood donation harms menstruating females: the current whole-blood-collection paradigm needs to be changed. Transfusion. 2006;46:1667–81. doi: 10.1111/j.1537-2995.2006.00969.x. [DOI] [PubMed] [Google Scholar]
- 41.Boulton F. Evidence-based criteria for the care and selection of blood donors, with some comments on the relationship to blood supply, and emphasis on the management of donation-induced iron depletion. Transfus Med. 2008;18:13–27. doi: 10.1111/j.1365-3148.2007.00818.x. [DOI] [PubMed] [Google Scholar]
- 42.Pasricha S-R, McQuilten ZK, Keller AJ, Wood EM. Hemoglobin and iron indices in nonanemic premenopausal blood donors predict future deferral from whole blood donation. Transfusion. 2011;51:2709–13. doi: 10.1111/j.1537-2995.2011.03173.x. [DOI] [PubMed] [Google Scholar]
- 43.Newman B. Improving the US blood supply and blood donation safety for both women and men. Transfusion. 2008;48:1032–5. doi: 10.1111/j.1537-2995.2008.01664.x. [DOI] [PubMed] [Google Scholar]
- 44.Davey RJ. Recruiting blood donors: challenges and opportunities. Transfusion. 2004;44:597–600. doi: 10.1111/j.0041-1132.2004.04402.x. [DOI] [PubMed] [Google Scholar]
- 45.Bravo M, Kamel H, Custer B, Tomasulo P. Factors associated with fainting - before, during and after whole blood donation. Vox Sang. 2011;101:303–12. doi: 10.1111/j.1423-0410.2011.01494.x. [DOI] [PubMed] [Google Scholar]
- 46.Kamel H, Tomasulo P, Bravo M, et al. Delayed adverse reactions to blood donation. Transfusion. 2010;50:556–65. doi: 10.1111/j.1537-2995.2009.02397.x. [DOI] [PubMed] [Google Scholar]
- 47.Wiltbank TB, Giordano GF, Kamel H, et al. Faint and prefaint reactions in whole-blood donors: an analysis of predonation measurements and their predictive value. Transfusion. 2008;48:1799–808. doi: 10.1111/j.1537-2995.2008.01745.x. [DOI] [PubMed] [Google Scholar]
- 48.Newman BH, Roth AJ. Estimating the probability of a blood donation adverse event based on 1000 interviewed whole-blood donors. Transfusion. 2005;45:1715–21. doi: 10.1111/j.1537-2995.2005.00595.x. [DOI] [PubMed] [Google Scholar]
- 49.Sojka BN, Sojka P. The blood-donation experience: perceived physical, psychological and social impact of blood donation on the donor. Vox Sang. 2003;84:120–8. doi: 10.1046/j.1423-0410.2003.00271.x. [DOI] [PubMed] [Google Scholar]
- 50.Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension. 2001;37:1199–208. doi: 10.1161/01.hyp.37.5.1199. [DOI] [PubMed] [Google Scholar]
- 51.Laitinen T, Hartikainen J, Vanninen E, et al. Age and gender dependency of baroreflex sensitivity in healthy subjects. J Appl Physiol. 1998;84:576–83. doi: 10.1152/jappl.1998.84.2.576. [DOI] [PubMed] [Google Scholar]
- 52.Fu Q, Levine BD. Why do young women (donors) faint? Transfusion. 2010;50:522–5. doi: 10.1111/j.1537-2995.2010.02593.x. [DOI] [PubMed] [Google Scholar]
- 53.Eder AF. Improving safety for young blood donors. Transfus Med Rev. 2012;26:14–26. doi: 10.1016/j.tmrv.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 54.Wieling W, France CR, van Dijk N, et al. Physiologic strategies to prevent fainting responses during or after whole blood donation. Transfusion. 2011;51:2727–38. doi: 10.1111/j.1537-2995.2011.03202.x. [DOI] [PubMed] [Google Scholar]
- 55.Newman BH, Siegfried BA. The quest to reduce vasovagal reactions in young blood donors. Transfusion. 2011;51:2061–3. doi: 10.1111/j.1537-2995.2011.03306.x. [DOI] [PubMed] [Google Scholar]
- 56.Tomasulo P, Kamel H, Bravo M, et al. Interventions to reduce the vasovagal reaction rate in young whole blood donors. Transfusion. 2011;51:1511–21. doi: 10.1111/j.1537-2995.2011.03074.x. [DOI] [PubMed] [Google Scholar]
- 57.Hanson SA, France CR. Social support attenuates presyncopal reactions to blood donation. Transfusion. 2009;49:843–50. doi: 10.1111/j.1537-2995.2008.02057.x. [DOI] [PubMed] [Google Scholar]
- 58.France CR, Menitove JE. Mitigating adverse reactions in youthful donors. Transfusion. 2008;48:1774–6. doi: 10.1111/j.1537-2995.2008.01882.x. [DOI] [PubMed] [Google Scholar]
- 59.Newman B, Tommolino E, Andreozzi C, et al. The effect of a 473-mL (16-oz) water drink on vasovagal donor reaction rates in high-school students. Transfusion. 2007;47:1524–33. doi: 10.1111/j.1537-2995.2007.01293.x. [DOI] [PubMed] [Google Scholar]
- 60.Hanson SA, France CR. Predonation water ingestion attenuates negative reactions to blood donation. Transfusion. 2004;44:924–8. doi: 10.1111/j.1537-2995.2004.03426.x. [DOI] [PubMed] [Google Scholar]
- 61.Krediet OTP, van Dijk N, Linzer M, et al. Management of vasovagal syncope. Controlling or aborting faints by leg crossing and muscle tensing. Circulation. 2002;106:1684–9. doi: 10.1161/01.cir.0000030939.12646.8f. [DOI] [PubMed] [Google Scholar]
- 62.Kowalsky JM, France JL, Wissel ME, France CR. Effect of applied muscle tension on cerebral oxygenation in female blood donors. Transfusion. 2011;51:1802–8. doi: 10.1111/j.1537-2995.2011.03075.x. [DOI] [PubMed] [Google Scholar]
- 63.Ditto B, France CR, Albert M, Byrne N. Dismantling applied tension: mechanisms of a treatment to reduce blood donation-related symptoms. Transfusion. 2007;47:2217–22. doi: 10.1111/j.1537-2995.2007.01449.x. [DOI] [PubMed] [Google Scholar]
- 64.France CR, Ditto B, Wissel ME, et al. Predonation hydration and applied muscle tension combine to reduce presyncopal reactions to blood donation. Transfusion. 2010;50:1257–64. doi: 10.1111/j.1537-2995.2009.02574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kowalsky JM, France JL, Wissel ME, France CR. Effect of applied muscle tension on cerebral oxygenation in female blood donors. Transfusion. 2011;51:1802–8. doi: 10.1111/j.1537-2995.2011.03075.x. [DOI] [PubMed] [Google Scholar]