Abstract
Background
In the Netherlands about 50% of whole blood donors return to give blood after an invitation to donate. This study aimed to investigate the characteristics of donor return behaviour and to gain insight into the barriers to blood donation reported by the donors themselves.
Materials and methods
A total of 4,901 whole blood donors were invited to donate in week 39 of 2009. Barriers mentioned by donors who informed the blood bank for not donating were registered for 1 month. Logistic regression analyses assessed relevant characteristics of return behaviour, such as age and blood type, in men and women separately.
Results
Of the invited donors, 55% returned to give a donation, whereas 45% did not return. Male donors were more likely to return when they were older, had a higher previous return rate and had no past deferrals. The same pattern was found among women, but was less strong. The main barriers were: time constraints (35%), preference to postpone donation due to general physical problems although being eligible to donate (29%), and being ineligible to donate due to medical deferral criteria (9%).
Discussion
Specific donor characteristics are associated with return behaviour. Not donating due to time constraints could mean that donors do not feel the urgency of donating blood. Interventions targeted to increase commitment among specific donor groups should be tested further.
Keywords: blood donors, barriers, return behaviour, donor characteristics
Introduction
Ensuring a sufficient number of blood donors is of crucial importance for every blood bank. In western countries the percentage of eligible people who donate blood varies from 5% to 8%1–6. Because the supply of blood is provided by a small group of volunteers, it is essential for blood banks that they can rely on their donors when blood is needed. In Europe, for example, blood banks invite their donors in personalised and non-personalised ways7,8. Methods such as invitation letters, text messages, leaflets, advertisements, and radio commercials are common practice. The response rates to a personal invitation of whole blood donors vary considerably in Europe, ranging from 5% to 80% (DOMAINE Survey, unpublished results)9. In the Netherlands, whole blood donors are invited by a personal invitation card asking them to come in and donate within a 2-week walk-in period. Between 40% to 60% of invited whole blood donors visit the blood bank for a blood donation within the 2-week interval. Each invitation costs about € 1 and every year the Dutch blood bank sends more than 1,000,000 invitation cards. With a non-return rate of 50%, this results in an annual direct loss of roughly € 500,000. In order to reduce the non-return behaviour of blood donors it is necessary to know their characteristics. It is also important to know why donors choose not to donate. What are the barriers to donating blood?
Previous research revealed that several donor characteristics are associated with donor return behaviour. Factors such as a higher donation frequency in previous years10, a higher lifetime number of donations11, and a short interval between two donations12,13 positively affect donor return. The donation experience itself also affects return behaviour. Being deferred or experiencing a physical reaction has a deterrent effect on subsequent donations13–20.
Although research on donor characteristics provides useful information for understanding return behaviour, learning more about the motivations and barriers to donating blood mentioned by donors themselves is also important. The motivation of donors to donate blood has been well investigated21–25, but most research on barriers to donating blood has been performed among non-donors and lapsed donors26–32. Only few studies have looked into the barriers described by active blood donors5,27,33,34. In these studies, donors reported organisational-related barriers, such as long waiting times, an unpleasant physical environment, bad treatment by blood centre staff, and donation-related barriers such as medical problems, fear of giving blood and not feeling well after a donation5,27,34. Sojka et al. found that the most reported obstacle to overcome, in order to continue being an active donor, was laziness, followed by fear of needles, fainting, or discovering an illness33. In a study by McKeever et al. donors had to report at the blood bank which aspect of the donation process would discourage them from returning. The most discouraging aspect of the donation process was long waiting times5. Remarkably, the barrier “nothing (special)” was mentioned by, respectively, 34.1% and 65.4% of the blood donors in the two studies5,33. All these studies have in common that donors were asked to state possible future barriers to donate. The fact that, on the whole, donors were not able to mention a specific future barrier, could imply that donors are only able to state what hinders them at the moment they receive an appeal to donate blood. Until now, no research has been done that has identified which barriers blood donors mention for not donating at the specific moment they are invited.
In the Netherlands, blood banks have the possibility to register the barriers at the moment active donors inform the blood bank of their inability to donate. Aside from the added value of gaining more knowledge about barriers to donating blood among active donors, registration of these barriers at the moment donors inform the blood bank of their decision not to donate offers readily available information. This can lead to more effective interventions aimed at increasing return behaviour among specific donor groups. The aim of this study was, therefore, to identify relevant characteristics associated with return behaviour among Dutch whole blood donors. In addition, the barriers mentioned by donors themselves, when they inform the blood bank that they are not going to donate, were investigated.
Materials and methods
Study population
This study was conducted at Sanquin Blood Centre Nijmegen, the main blood centre in the southeast region of the Netherlands. All blood donors who received an invitation card in week 39 of 2009 (N =4,901) were included for this study. The invitation card encouraged these donors to donate within a 2-week period (week 40 and 41). Although it was officially communicated to the donors that they were invited to donate within these 2 weeks, blood banks also accepted the invitation card when donors donated 1 week before (week 39), or 1 week after the 2-week walk-in period (week 42). So, this study included all donors who received an invitation card in week 39 and were followed during weeks 39, 40, 41, and 42.
Data collection
After receiving the invitation card, whole blood donors could either visit the blood bank for a donation (return), or not visit the blood bank (non-return). The donor characteristics of return behaviour and non-return behaviour were extracted from a computerised blood bank donor database (eProgesa 5.02, Mak-system, Paris, France). Barriers to donating were registered at the donor call centre during a 1 month period: from the day donors received the invitation card until the last day that the card was valid (from week 39 to 42 of 2009). Donors could either call or send an e-mail to inform the blood bank about their inability to donate. During this period there were no holidays or other special occasions that could disturb a regular donation period. Barriers were coded into ten different categories (Table I). A unique code was assigned to every category in eProgesa. Before the study started, a staff member of the donor call centre tested the clarity and usability of the list of categories. Every staff member at the donor call centre received the list on a yellow overview chart that provided the type of donation barrier, a short definition of the barrier, and the accompanying code to be used for registration in eProgesa. During a staff meeting the whole procedure of registering the barriers was clarified to the administrative personnel. If a donor cancelled the donation without giving an explicit barrier, staff members were instructed to ask in a polite way with a pre-defined open-ended question what the barrier was. If a donor gave multiple barriers, then the first barrier was registered. If the barrier was unclear or not mentioned on the yellow barrier-chart, staff members filled in the option “other, namely”.
Table I.
Barriers to donating blood.
| Barrier | Definition | N.* (%) |
|---|---|---|
| Time constraints, not specified | Donor who could not donate and didn’t give an explicit barrier | 96 (35.3) |
| Eligible to donate but prefers to postpone donation due to general physical problems | Donor who is eligible to donate, but doesn’t want to because of physical problems (e.g. feeling nauseous) | 80 (29.4) |
| Ineligible to donate due to medical deferral criteria | Donor is ineligible to donate according to the medical criteria from the blood bank (eProgesa) | 23 (8.5) |
| Work / study | Donor who could not donate due to work or study | 17 (6.3) |
| Vacation / stay abroad | Donor who goes on vacation or stays abroad | 16 (5.9) |
| Personal circumstances | Donor who could not donate due to personal circumstances (e.g. having a funeral) | 15 (5.5) |
| Forgotten | Donor who forgot the invitation to donate | 12 (4.4) |
| Sport / hobby | Donor who could not donate because of a sport/hobby | 2 (0.7) |
| Expected deferral | Donor who expects to be deferred from donating blood (e.g. Hb too low) | 2 (0.7) |
| Previous donation experience | Donor who doesn’t want to donate because of negative donation experience(s) at previous visit | 2 (0.7) |
| Other, namely | Donor who gave a reason that could not be assigned to a category | 7 (2.6) |
Barriers as reported by the donors (N =272) who informed the blood bank by phone that they were going to donate.
Statistics
To look more closely into the characteristics of return behaviour, logistic regression analyses were performed on return vs non-return behaviour. Due to gender-related differences in the number of donations per year (men are allowed to give five times a year, women three times a year), the analyses were done separately for men and women. First, univariate logistic regression analyses were conducted, including each of the following variables separately: age, blood type, return rate in the previous 4 years, total lifetime number of donations and being deferred in the past. Second, multivariate logistic regression analyses were performed by including all these variables at once. Categorisation of the following variables was necessary due to non-linearity: age, return rate in the previous 4 years, and lifetime number of donations. Age was categorised into 18–29 years old, 30–49 years old, and 50 years or older; return rate was categorised into 0–25%, 26–50%, 51–75%, and 76–100%; and lifetime number of donations into 0–5 donations, 6–10 donations, 11–20 donations and 21 or more donations. Logistic regression analyses resulted in odds ratios (OR) and their 95% confidence intervals (CI).
Furthermore, barriers to donating were investigated and displayed descriptively as numbers and percentages.
Results
Demographics of invited blood donors
The characteristics of 4,901 invited active whole blood donors in week 39 of 2009 are shown in Table II. Men were older than women (P <0.01), with a mean age for men being 47.9 years (SD =13.4) and that of women being 41.9 years (SD =12.5). Men had also given a significantly higher number of donations in their lifetime (P <0.01; mean =37.8, SD =28.4) than women (mean =16.3, SD =15.4).
Table II.
Characteristics of invited whole blood donors*.
| Characteristic | Total invited (N =4,901; 100%) | |
|---|---|---|
| Men (n =2,565; 52.3%) | Women (n =2,336; 47.7%) | |
| Age, n (%) | ||
| 18–29 | 293 (11.4) | 558 (23.9) |
| 30–49 | 973 (37.9) | 1,020 (43.7) |
| ≥50 | 1,299 (50.6) | 758 (32.4) |
| Blood type, n (%) | ||
| O-negative | 346 (13.5) | 338 (14.5) |
| Not O-negative | 2,219 (86.5) | 1,998 (85.5) |
| Return rate in previous 4 years, n (%) | ||
| 0%–25% | 136 (5.3) | 192 (8.2) |
| 26%–50% | 536 (20.9) | 529 (22.7) |
| 51%–75% | 788 (30.7) | 710 (30.4) |
| 76%–100% | 1,105 (43.1) | 904 (38.7) |
| Lifetime donations, n (%) | ||
| 0–5 | 333 (13.0) | 722 (30.9) |
| 6–10 | 208 (8.1) | 382 (16.4) |
| 11–20 | 330 (12.9) | 479 (20.5) |
| ≥ 21 | 1,694 (66.0) | 753 (32.2) |
| Deferral, n (%) | ||
| No | 711 (30.4) | 1,002 (39.1) |
| Yes | 1,625 (69.6) | 1,563 (60.9) |
Numbers do not always count up to total due to rounding of percentages.
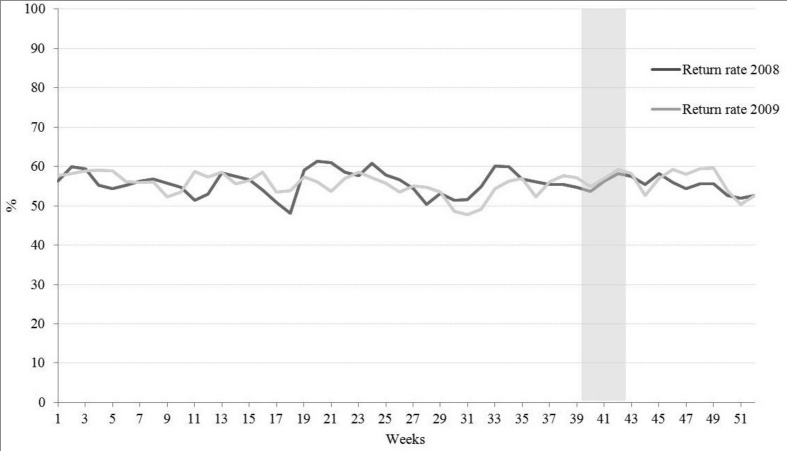
The return rates in 2008 and 2009 of Dutch whole blood donors in the southeast of the Netherlands ranged from 48% to 61% with an average return rate of 56% (Figure 1). The return rate of 55% in week 39 of 2009 (see grey bar in Figure 1) does not differ much from the average return rate in 2009 or 2008 (56% in both years), and is, therefore, considered representative of the other weeks in those years.
Figure 1.
Return rates for whole blood donors* in the southeast region of the Netherlands in 2008 and 2009.
*Return rates for whole blood donors were calculated as follows: Return rate = (number of whole blood donors visiting the blood bank within 4 weeks / number of invitations in 1 week) × 100.
Characteristics of the invited donors who returned to donate and those who did not
Of the invited donors (N =4,901), 55% (n =2,679) returned to give blood at the blood bank and 45% (n =2,222) of the donors did not. Univariate logistic regression analyses were performed on the characteristics associated with return or non-return behaviour (Table III). For both men and women, increasing age, having a higher return rate in the previous 4 years and a higher lifetime number of donations increased the odds of return, while having type O-negative blood and having been deferred in the past decreased the odds of return.
Table III.
Univariate and multivariate logistic regression analyses on return donors vs non-return donors.
| Characteristic | Men | Women | ||
|---|---|---|---|---|
|
| ||||
| Unadjusted OR (95% CI) | Adjusted OR* (95% CI) | Unadjusted OR (95% CI) | Adjusted OR* (95% CI) | |
| Age | ||||
| 18–29 | 1.0 | 1.0 | 1.0 | 1.0 |
| 30–49 | 1.81 (1.39–2.35) | 1.64 (1.20–2.25) | 1.36 (1.10–1.68) | 1.36 (1.07–1.73) |
| ≥50 | 2.60 (2.01–3.37) | 1.85 (1.31–2.59) | 2.63 (2.10–3.30) | 2.09 (1.57–2.78) |
| Blood type | ||||
| Not O-negative | 1.00 | 1.0 | 1.0 | 1.0 |
| O-negative | 0.74 (0.59–0.93) | 0.82 (0.64–1.05) | 0.78 (0.62–0.98) | 0.83 (0.65–1.07) |
| Return rate in previous 4 years | ||||
| 0%–25% | 1.0 | 1.0 | 1.0 | 1.0 |
| 26%–50% | 1.01 (0.68–1.49) | 0.92 (0.62–1.39) | 0.53 (0.37–0.74) | 0.49 (0.34–0.70) |
| 51%–75% | 1.91 (1.31–2.79) | 1.71 (1.15–2.54) | 1.22 (0.89–1.69) | 1.10 (0.78–1.54) |
| 76%–100% | 6.34 (4.34–9.26) | 5.39 (3.63–8.01) | 2.98 (2.16–4.09) | 2.48 (1.78–3.47) |
| Lifetime donations | ||||
| 0–5 | 1.0 | 1.0 | 1.0 | 1.0 |
| 6–10 | 1.12 (0.79–1.59) | 1.11 (0.76–1.62) | 1.12 (0.87–1.44) | 1.08 (0.82–1.42) |
| 11–20 | 1.24 (0.91–1.68) | 1.06 (0.75–1.51) | 1.04 (0.82–1.31) | 0.90 (0.69–1.19) |
| ≥21 | 2.07 (1.64–2.63) | 1.35 (0.98–1.85) | 1.96 (1.59–2.41) | 1.29 (0.98–1.68) |
| Deferral | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 0.84 (0.72–0.99) | 0.73 (0.61–0.88) | 0.76 (0.64–0.90) | 0.78 (0.64–0.95) |
Adjusted for all other variables included in the model.
Subsequently, all factors were included into a multivariate model to disentangle the independent associations with return behaviour for men and women separately. For men, increasing age enhanced the odds of return, compared to the reference group aged 18–29 years (OR30–49 =1.64, 95% CI =1.20–2.25; OR ≥50 =1.85, 95% CI =1.31–2.59). For male donors, having a return rate above 50% in the previous 4 years increased the odds of return, compared to male donors with a return rate lower than 25% in the previous 4 years (OR51%–75% =1.71, 95% CI =1.15–2.54; OR76%–100% =5.39, 95% CI =3.63–8.01). On the other hand, male donors with past deferral(s) were less likely to return than male donors with no past deferrals (OR deferral =0.84, 95% CI =0.72–0.99). In the multivariate analysis, the effects of life-time number of donations and having type O-negative blood were no longer associated with return behaviour.
A similar pattern was found for women. Multivariate analyses also showed that increased age enhanced the odds of return, compared to that of the reference group younger than 29 years (OR30–49 =1.36, 95% CI =1.07–1.73; OR≥50 =2.09, 95% CI =1.57–2.78). Furthermore, women with a return rate above 50% in the previous 4 years were more likely to return (OR76%–100% =2.48, 95% CI =1.78–3.47) than women with a return rate lower than 25%. On the other hand, women who had a previous return rate between 26–50% were less likely to return (OR26%-25% =0.49, 95% CI =0.34–0.70) than women with a return rate lower than 25%. For women, being deferred once or more often decreased the odds of return (OR deferral =0.78, 95% CI =0.64–0.95) compared to women with no past deferrals. Also for women, the effects of lifetime number of donations and having type O-negative blood were no longer associated with return behaviour.
Barriers to donating blood
Of the donors who did not return to the blood bank (n =2,222), only 407 donors (18%) informed the blood bank that they were not going to donate. Far more donors cancelled their invitation by telephone (n =272, 67%) than by e-mail (n =135, 33%). Donors who cancelled their donation by e-mail were not required to provide an explicit reason for not donating. Donors who cancelled their donation by phone, were explicitly asked about barriers to donating (Table I). The three main barriers for not donating were time constraints (35.3%), preference to postpone donation due to general physical problems, despite being eligible to donate (29.4%), and ineligibility to donate because of medical deferral criteria (8.5%). Barriers that were less often mentioned were work/study (6.3%), vacation/stay abroad (5.9%), personal circumstances (5.5%), and forgotten (4.4%). Reasons assigned to the category “other namely” (2.6%) included, for example, moving to another city.
Discussion
This study revealed that 55% of invited donors returned for their donation, whereas 45% did not return. The first aim was to investigate the characteristics of the donors who decided to return and those who did not return. Male donors were more likely to return for their donation when they were older, had a higher return rate in the previos 4 years and had no past deferrals. Having made more donations and having type O-negative blood did not influence return behaviour. The same pattern was found among women, but was less strong. The second aim was to investigate the barriers mentioned by donors who informed the blood bank that they were not going to donate. Donors reported time constraints, eligibility to donate but preference to postpone donation due to general physical problems, and ineligibility to donate due to medical deferral criteria as the three main barriers.
Taken together, our results confirm previous research on donor characteristics13–16,35, which also found that donors with a higher age, a higher return behaviour and donors with no past deferral(s) are more likely to return for a donation. Importantly, this is the first study that has registered the barriers to donating at the time the donors informed the blood bank about their decision, whereas previous studies had primarily investigated future barriers to donation. Time constraints was the most important reason given for not donating, while organisational barriers, such as waiting time, were not mentioned at all. In addition, most donors who preferred not to donate because of physical problems, such as having a headache, would not have been officially deferred for donating according to medical exclusion criteria from the blood bank. This means that, formally, they were eligible to donate, but chose not to. It might be that these donors mentioned medical barriers as a “fake” reason, which is more socially acceptable than stating that they don’t have time.
Results from the present study have implications for the daily practice of blood banks. In order to improve return behaviour, blood banks should focus more on specific donor groups, such as younger donors, donors who have had a low return rate in previous years and donors who have been deferred once or more. In addition, the most frequently mentioned barrier, not having enough time to donate, seems to fit in the psychological concept of “social inertia”36. Social inertia refers to the situation in which a person has a positive attitude towards a request, but doesn’t take the corresponding action because of a lack of urgency or motivation. In general, most donors have the intention to give blood, but it might be that some donors do miss the urgency and priority in their life that makes them return to give a subsequent donation.
Interventions aimed at increasing commitment to return to donate should be developed to overcome social inertia. One of the possibilities is creating commitment at the start of the donor career, for example, by formalising “blood donorship” in the form of a “social contract”. With this contract, a blood donor confirms and agrees with the blood bank policy. As a consequence, blood donors would be more aware of the expectations of the blood bank, which might enhance the urgency to donate blood. Another option to improve return behaviour is to use “implementation intentions”, previously mentioned by Ferguson et al.37. Implementation intentions are “if-then” plans to facilitate the conversion of intentions into behaviour (e.g. donating blood) and have the following structure: “When it is situation X, I will perform Y”.38 The purpose of implementation intentions is that, when the specific situation arises, a person feels committed to act according to a well-defined plan to reach the goal behaviour. For the blood bank situation, donors can be asked to specify “where”, “when” and “how” they will donate blood after an invitation to donate. For example, the blood bank can ask the donor to plan in his or her agenda a specific day and time to donate blood at the blood centre: “When I receive the invitation card, I will give blood on Tuesday at 8.00 pm at the blood centre in Amsterdam”.
Although it is valuable to identify the barriers to donating at the moment donors inform the blood bank about their inability, we are aware that this procedure is not common practice in every country. In this study only a small number of donors informed the blood bank that they were not able to donate, which might indicate that most donors are not aware of the possibility of cancelling their donation or do not feel obliged to do so. In addition, donors who do cancel their invitation to donate might be more inclined to give social desirable responses to the blood bank. It is, therefore, possible that the barriers for donors who inform the blood bank about not donating differ from those donors who did not inform the blood bank for not donating. To overcome this lack of information we also interviewed 30 donors who did not return and did not inform the blood bank about their inability to donate (data not reported in this article). The most common barrier mentioned by these donors was also “time constraints”, and does not differ from the barrier mentioned by donors who informed the blood bank that they would not donate. However, it should be noted that the limitations of this method are that these interviews were held in retrospect, and that donors had to mention their barriers by phone to a member of staff. Furthermore, the analyses performed in this study are correlational by nature and causal inferences should, therefore, be made with care.
In conclusion, donors who returned to donate were older, had a higher return rate in the previous 4 years and had no past deferrals. These findings signal that interventions aimed at increasing return behaviour need to be better targeted at specific donor groups. A “one size fits all” approach does not seem feasible. The current study is the first study to investigate donation barriers mentioned by donors at the moment they choose not to donate, instead of asking them to reflect upon barriers in retrospect. The fact that time constraints formed the most reported barrier, suggests that donors do not feel the urgency of donating blood, which can be explained by social inertia. This provides valuable information that can be used to set up better targeted interventions aimed at creating commitment by overcoming social inertia.
Footnotes
The Authors declare no conflicts of interest.
References
- 1.Linden JV, Gregorio DI, Kalish RI. An estimate of blood donor eligibility in the general population. Vox Sang. 1988;54:96–100. doi: 10.1111/j.1423-0410.1988.tb01624.x. [DOI] [PubMed] [Google Scholar]
- 2.Neal RD, Hussain-Gambles M, Allgar VL, et al. Reasons for and consequences of missed appointments in general practice in the UK: questionnaire survey and prospective review of medical records. BMC Fam Pract. 2005;6:47. doi: 10.1186/1471-2296-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.America’s Blood Center News Release. Urgent appeal for blood donation in New York: advertising community pledges massive weeklong blood donation campaign. [Accessed on 25/11/2012]. Available at: http://www.americasblood.org/download/releases/pr_060925_adweek.pdf.
- 4.Heinrich J. Availability of Blood. Washington DC: United States General Accounting Office; 1999. [Google Scholar]
- 5.McKeever T, Sweeney MR, Staines A. An investigation of the impact of prolonged waiting times on blood donors in Ireland. Vox Sang. 2006;90:113–8. doi: 10.1111/j.1423-0410.2006.00734.x. [DOI] [PubMed] [Google Scholar]
- 6.Schoenborn CA, Marsh SL, Hardy AM. AIDS knowledge and attitudes for 1992. Data from the National Health Interview Survey. Adv Data. 1994;243:1–16. doi: 10.1037/e608982007-001. [DOI] [PubMed] [Google Scholar]
- 7.Veldhuizen I, Folléa G, Degiorgio A, et al. Donor recruitment. In: de Kort W, Veldhuizen I, editors. Donor Management Manual. 1st ed. Nijmegen: Domaine; 2010. pp. 84–102. [Google Scholar]
- 8.Folléa G, Veldhuizen IJT, Redpath G, et al. Donor retention. In: De Kort W, Veldhuizen I, editors. Donor Management Manual. 1st ed. Nijmegen: Domaine; 2010. pp. 103–22. [Google Scholar]
- 9.DOMAINE: Donor Management in Europe. [Accessed on 25/11/2012]. http://www.domaine-europe.eu/ Available from 2008.
- 10.Schlumpf KS, Glynn SA, Schreiber GB, et al. Factors influencing donor return. Transfusion. 2008;48:264–72. doi: 10.1111/j.1537-2995.2007.01519.x. [DOI] [PubMed] [Google Scholar]
- 11.Schreiber GB, Sharma UK, Wright DJ, et al. First year donation patterns predict long-term commitment for first-time donors. Vox Sang. 2005;88:114–21. doi: 10.1111/j.1423-0410.2005.00593.x. [DOI] [PubMed] [Google Scholar]
- 12.Ownby HE, Kong F, Watanabe K, et al. Analysis of donor return behavior. Retrovirus Epidemiology Donor Study. Transfusion. 1999;39:1128–35. doi: 10.1046/j.1537-2995.1999.39101128.x. [DOI] [PubMed] [Google Scholar]
- 13.Bosnes V, Aldrin M, Heier HE. Predicting blood donor arrival. Transfusion. 2005;45:162–70. doi: 10.1111/j.1537-2995.2004.04167.x. [DOI] [PubMed] [Google Scholar]
- 14.Piliavin JA. Temporary deferral and donor return. Transfusion. 1987;27:199–200. doi: 10.1046/j.1537-2995.1987.27287150200.x. [DOI] [PubMed] [Google Scholar]
- 15.Halperin D, Baetens J, Newman B. The effect of short-term, temporary deferral on future blood donation. Transfusion. 1998;38:181–3. doi: 10.1046/j.1537-2995.1998.38298193102.x. [DOI] [PubMed] [Google Scholar]
- 16.Custer B, Chinn A, Hirschler NV, et al. The consequences of temporary deferral on future whole blood donation. Transfusion. 2007;47:1514–23. doi: 10.1111/j.1537-2995.2007.01292.x. [DOI] [PubMed] [Google Scholar]
- 17.Veldhuizen I, Atsma F, van Dongen A, Kort de W. Adverse reactions, psychological factors, and their effect on donor retention in men and women. Transfusion. 2012;52:1871–9. doi: 10.1111/j.1537-2995.2011.03551.x. [DOI] [PubMed] [Google Scholar]
- 18.Newman BH, Newman DT, Ahmad R, Roth AJ. The effect of whole-blood donor adverse events on blood donor return rates. Transfusion. 2006;46:1374–9. doi: 10.1111/j.1537-2995.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- 19.France CR, Rader A, Carlson B. Donors who react may not come back: analysis of repeat donation as a function of phlebotomist ratings of vasovagal reactions. Transfus Apher Sci. 2005;33:99–106. doi: 10.1016/j.transci.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 20.France CR, France JL, Roussos M, Ditto B. Mild reactions to blood donation predict a decreased likelihood of donor return. Transfus Apher Sci. 2004;30:17–22. doi: 10.1016/j.transci.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 21.Ferguson E, Atsma F, de KW, Veldhuizen I. Exploring the pattern of blood donor beliefs in first-time, novice, and experienced donors: differentiating reluctant altruism, pure altruism, impure altruism, and warm glow. Transfusion. 2012;52:343–55. doi: 10.1111/j.1537-2995.2011.03279.x. [DOI] [PubMed] [Google Scholar]
- 22.Ferguson E, Farrell K, Lawrence C. Blood donation is an act of benevolence rather than altruism. Health Psychol. 2008;27:327–36. doi: 10.1037/0278-6133.27.3.327. [DOI] [PubMed] [Google Scholar]
- 23.Glynn SA, Kleinman SH, Schreiber GB, et al. Motivations to donate blood: demographic comparisons. Transfusion. 2002;42:216–25. doi: 10.1046/j.1537-2995.2002.00008.x. [DOI] [PubMed] [Google Scholar]
- 24.Misje AH, Bosnes V, Gasdal O, Heier HE. Motivation, recruitment and retention of voluntary non-remunerated blood donors: a survey-based questionnaire study. Vox Sang. 2005;89:236–44. doi: 10.1111/j.1423-0410.2005.00706.x. [DOI] [PubMed] [Google Scholar]
- 25.Kasraian L, Maghsudlu M. Blood donors’ attitudes towards incentives: influence on motivation to donate. Blood Trans. 2012;10:186–90. doi: 10.2450/2011.0039-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duboz P, Cuneo B. How barriers to blood donation differ between lapsed donors and non-donors in France. Transfus Med. 2010;20:227–36. doi: 10.1111/j.1365-3148.2010.00998.x. [DOI] [PubMed] [Google Scholar]
- 27.Marantidou O, Loukopoulou L, Zervou E, et al. Factors that motivate and hinder blood donation in Greece. Transfus Med. 2007;17:443–50. doi: 10.1111/j.1365-3148.2007.00797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harrington M, Sweeney MR, Bailie K, et al. What would encourage blood donation in Ireland? Vox Sang. 2007;92:361–7. doi: 10.1111/j.1423-0410.2007.00893.x. [DOI] [PubMed] [Google Scholar]
- 29.Boulware LE, Ratner LE, Ness PM, et al. The contribution of sociodemographic, medical, and attitudinal factors to blood donation among the general public. Transfusion. 2002;42:669–78. doi: 10.1046/j.1537-2995.2002.00120.x. [DOI] [PubMed] [Google Scholar]
- 30.Piliavin JA. Why do they give the gift of life? A review of research on blood donors since 1977. Transfusion. 1990;30:444–59. doi: 10.1046/j.1537-2995.1990.30590296381.x. [DOI] [PubMed] [Google Scholar]
- 31.Mathew SM, King M, Glynn SA, et al. Opinions about donating blood among those who never gave and those who stopped: a focus group assessment. Transfusion. 2007;47:729–35. doi: 10.1111/j.1537-2995.2007.01177.x. [DOI] [PubMed] [Google Scholar]
- 32.Gillespie TW, Hillyer CD. Blood donors and factors impacting the blood donation decision. Transfus Med Rev. 2002;16:115–30. doi: 10.1053/tmrv.2002.31461. [DOI] [PubMed] [Google Scholar]
- 33.Sojka BN, Sojka P. The blood donation experience: self-reported motives and obstacles for donating blood. Vox Sang. 2008;94:56–63. doi: 10.1111/j.1423-0410.2007.00990.x. [DOI] [PubMed] [Google Scholar]
- 34.Thomson RA, Bethel J, Lo AY, et al. Retention of “safe” blood donors. The Retrovirus Epidemiology Donor Study. Transfusion. 1998;38:359–67. doi: 10.1046/j.1537-2995.1998.38498257374.x. [DOI] [PubMed] [Google Scholar]
- 35.Whyte G. Quantitating donor behaviour to model the effect of changes in donor management on sufficiency in the blood service. Vox Sang. 1999;76:209–15. doi: 10.1159/000031053. [DOI] [PubMed] [Google Scholar]
- 36.Knowles ES, Linn JA. Resistance and persuasion. Mahwah, NJ: Erlbaum; 2004. [Google Scholar]
- 37.Ferguson E, France CR, Abraham C, et al. Improving blood donor recruitment and retention: integrating theoretical advances from social and behavioral science research agendas. Transfusion. 2007;47:1999–2010. doi: 10.1111/j.1537-2995.2007.01423.x. [DOI] [PubMed] [Google Scholar]
- 38.Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol. 2006;38:249–68. [Google Scholar]