Abstract
Background
An adequate, safe supply of blood and blood components is a crucial part of blood transfusion services. Blood donors with reactive screening test results are informed of their results by letter and telephone call, and are requested to come for counselling either at the blood centre or the integrated counselling and testing centre. Many notified donors either do not respond at all or do not follow up their first visit to the blood bank. This study was undertaken to determine the response of voluntary blood donors after notification of their reactive status by telephone call or letter.
Material and methods
We considered reactive donations during a 2-year period (January 2010 to December 2011). Blood donors with reactive test results were notified and their response rates were evaluated at various levels.
Results
During the study period, 416 donors (0.87%) were found to be reactive for different markers. Of these 416 reactive donors, 249 (59.8%) responded positively to the notification calls and attended counselling. The response rate was highest among donors reactive for hepatitis B virus (HBV) (154/225 i.e. 68.4%). After their first visit, around 6% donors could not be contacted further and were lost to follow up. Fifty donors (22.3%) did not continue their treatment and two (both reported to be HBV reactive) were subsequently found to be negative. Therefore, at 6 months of follow-up, only 182 donors (43.7%) were continuing/had completed their treatment.
Discussion
The response rate of reactive blood donors in developing countries is quite low. These results suggest insufficient health care knowledge and a poor understanding of screening tests.
Keywords: donor notification, transfusion-transmissible infection, blood donor counselling
Introduction
Blood is a life-saving product and there is no substitute for this precious resource. However, like drugs, blood transfusions come with potentially fatal risks. Blood donor screening and testing for transfusion-transmissible infections have become stringent all over the world. Nevertheless, transfusing blood that is zero risk i.e. free from all transmissible infections, is still far from becoming reality. In developing countries, a major source of hepatitis C virus (HCV), hepatitis B virus (HBV) and human immunodeficiency virus (HIV) infections is transfusion of blood and blood products from unscreened or inadequately screened blood donors.
A fundamental part of preventing disease transmission by transfusion is to notify and counsel donors about the status of their seroreactivity. According to Objective 4.16 of the Indian Action Plan for Blood Safety, donors are counselled about transfusion-transmissible infections prior to donation and are offered the option of knowing their infective status provided they give consent to this1. Blood donors with reactive screening test results are informed by letter and telephone call, and are requested to come for counselling and repeat testing either at a blood centre or at an integrated counselling and testing centre (ICTC). While technological advancements have led to the development of more sensitive methods to detect markers of transfusion-transmissible infections, the prevalence of false-positive cases (positive tests in people who are not really infected) has increased simultaneously. This leads to unnecessary anxiety in donors who are notified about their reactive results either by letter or telephonically.
On the other hand, it has been realised that most donors who are notified of their results either do not respond at all or do not follow up their first visit to the blood centre. Some donors with deferrable risk behaviours continue to donate blood (at other blood donation centres) despite being notified about the infectious disease test results on their blood samples. This study was undertaken to determine the response of voluntary blood donors after they were notified of their reactive status by telephone calls or letters.
Materials and methods
The IMA blood bank is the largest blood bank in the region of Uttarakhand (India) and collects 100% voluntary blood donations. We evaluated reactive donations in a 2-year (January 2010 to December 2011). Most of the donors were from an urban background and had received at least primary school education. Blood donors whose samples gave a reactive test result in a fully automated enzyme-linked immunosorbent assay (Evolis, Bio-Rad, Hercules, California, United States of America) were tested again with a fully automated, random access, enhanced chemiluminescence immunoassay (ECI, Ortho, New York, United States of America). Only donors reactive on both tests were notified about their results by letter and personal calls. The response rate of these donors was evaluated at the time of notification and at various follow-up visits at the blood bank, ICTC (for HIV) or physician of choice for other infections. They were also referred to their physicians if they were unaware of the infections.
After the reports had been sent, the donors were followed telephonically to make sure that they had received the report, consulted a doctor and undergone a confirmatory test, as required. The first follow-up call was made on the 10th day after sending the letter. If the donor did not respond to this first call, second and third follow-up calls were made 20 and 30 days after dispatching the letter. The case was closed only if the donor did not respond to any of the three telephone calls.
Results
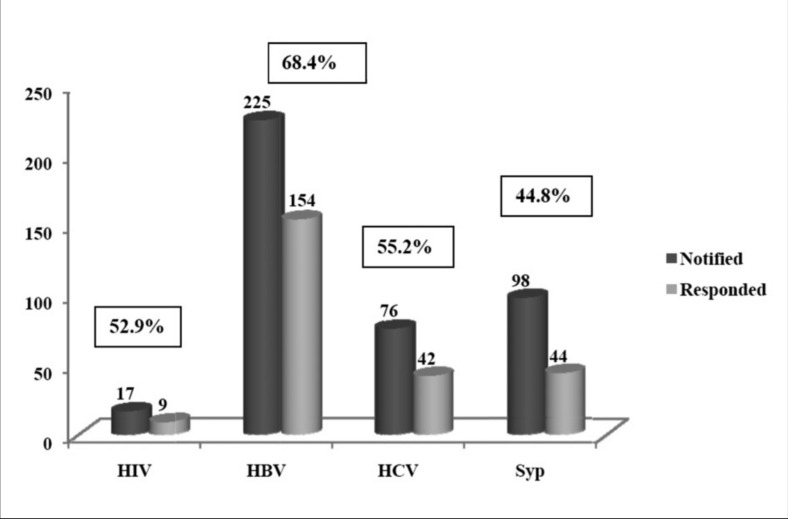
Out of 48,386 whole blood donations, 416 donors (0.87%) were found to be reactive for different markers (225 for HBV, 76 for HCV, 98 for syphilis and 17 for HIV). Among the 416 reactive donors, 249 (59.8%) responded positively to the notification calls and attended counselling either at the blood bank or with the physician they were told to consult. The response rate was highest for HBV-reactive donors (154/225; 68.4%) (Figure 1). After their first visit, about 6% of donors could not be contacted further and were lost to follow-up. Out of 234 donors, two donors (both reactive for HBV) were shown to be negative by confirmatory tests and 52 donors (21.3%) did not continue their treatment without disclosing any concrete reasons. Thirty-three of these donors were HBV-reactive, 11 were HCV-reactive, seven were reactive for syphilis while only one was HIV-reactive. In summary, at 6 months of follow-up, only 182 (43.7%) of the donors were continuing or had completed their treatment.
Figure 1.
Response rate of donors notified.
Discussion
Over the years, the demand for blood transfusions has been increasing world over. Various critical disease conditions, road traffic accidents and emergency and routine surgical operations require safe blood transfusions. However, safe blood still remains out of reach of millions who require it.
The rate of all markers of transfusion-transmissible infections at our centre was found to be quite low (0.87%) as compared to rates in other studies in India and other developing countries2,3. One possible explanation for this is that all our donations are from voluntary blood donors, whereas in other centres replacement donors still comprise a large proportion of the blood donors4. Most of the HIV-reactive people in India and other developing countries are unaware about their HIV status and remain asymptomatic for a long time. It is a great benefit to both society and blood donors that the donors are informed about their reactive status so that they can confirm their status and get prompt treatment. On the other hand, the information becomes a great source of anxiety and stigma for a person who was otherwise asymptomatic and came to make a donation with an altruistic intent.
Although the rate of response by the reactive donors after notification of screening test results on their blood samples was low (59.8%) in our study, it was higher than that in the few other studies in other centers5,6. This may be because of the detailed pre-donation counselling given by our dedicated team. All our donors are made aware about the various problems that they and the recipients of their blood could encounter if they conceal their risk behaviours and the donors are motivated to exclude themselves if they think they may have an infection.
Pre-donation screening of donors’ health history is an integral part of blood safety and there is a need to optimise this aspect. Counsellors and interviewers should be well trained and competent, the written material given to the donor should be clear and comprehensible and most importantly, privacy and confidentiality should be maintained at every step. In a study by Doll et al. it was found that 31% of HIV-positive donors felt a lack of privacy during their health interview, while 20% stated that they would have given different answers if they had been in a more private situation7.
The response of donors to notifications depends largely on the donors’ understanding about the transmission of infections and the results of screening tests that are done on blood samples to detect transfusion-transmissible infections. Donors have different perceptions about these tests. In a study by Sharma et al8, it was found that very few of the donors had information about the “window period”. The donors with “high risk behaviour” continued to donate blood thinking it would be tested for infections and discarded if it was shown to be reactive for any of the infections. This study also found that approximately 23% of donors thought it was reasonable to donate blood for the purpose of being tested for HIV virus.
Donors who come for counselling are benefitted in various ways over those who do not turn up after notification. During counselling, donors are encouraged to ask questions about their status and their myths and anxieties are taken care of. The responsibilities of these donors towards society and their partners and the various treatment options available for the disease in question are also discussed in detail. In comparison, donors who do not seek counselling continue to be a threat to the public, their families and blood transfusion services.
One more finding of this study that should be a serious concern for blood transfusion authorities is that around 28% of donors who responded to the first call did not follow up their first attendance at the ICTC or with the physicians they were asked to meet. This raises a few questions about the way donors are counselled and made aware of the consequences of not taking proper treatment. It is also alarming that only 43% of all the reactive donors were either taking treatment or had completed it 6 months after having received notification of their infectious status.
In conclusion, it is very evident that the response rate of donors after notification about the reactive status of their donations is very low. These results suggest poor health care knowledge and stigma associated with transfusion-transmissible infections among the population and a poor understanding of the screening tests. Blood donors need to be educated and motivated about the various transfusion-transmissible infections, about the importance of confirming results suggestive of an infection and about treatment if the infection is indeed confirmed.
Footnotes
The Author declares no conflicts of interest.
References
- 1.An Action Plan for Blood Safety. National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India; 2003. pp. 35–7. [Google Scholar]
- 2.Singh B, Kataria SP, Gupta R. Infectious markers in blood donors of East Delhi: prevalence and trends. Indian J Pathol Microbiol. 2004;47:477–9. [PubMed] [Google Scholar]
- 3.Fessehaye N, Naik D, Fessehaye T. Transfusion transmitted infections - A retrospective analysis from the National Blood Transfusion Service in Eritrea. Pan Afr Med J. 2011;9:40. doi: 10.4314/pamj.v9i1.71219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nanda A, Tyagi S, Basu S, Marwaha N. Prevalence of transfusion transmitted infections among voluntary and replacement donors. Indian J Hemat Blood Transf. 2001;19:104–5. [Google Scholar]
- 5.Roshan TM, Rosline H, Ahmed SA, et al. Response rate of malaysian blood donors with reactive screening test to transfusion medicine unit calls. Southeast Asian J Trop Med Public Health. 2009;40:1315–21. [PubMed] [Google Scholar]
- 6.Kleinman S, Wang B, Wu Y, et al. The donor notification process from the donor’s perspective. Transfusion. 2004;44:658–66. doi: 10.1111/j.1537-2995.2004.03347.x. [DOI] [PubMed] [Google Scholar]
- 7.Doll LS, Peterson LR, White CR, et al. Human immunodeficiency virus type-1 infected blood donors: behavioral characteristics and reasons for donation. Transfusion. 1991;31:704. doi: 10.1046/j.1537-2995.1991.31892023494.x. [DOI] [PubMed] [Google Scholar]
- 8.Sharma UK, Schreiber GB, Glynn SA, et al. Knowledge of HIV/AIDS transmission and screening in United States blood donors. Transfusion. 2001;41:1341–50. doi: 10.1046/j.1537-2995.2001.41111341.x. [DOI] [PubMed] [Google Scholar]