Abstract
BACKGROUND AND OBJECTIVES:
Health care reform offers a new opportunity to address child health disparities. This study sought to characterize racial differences in pediatric asthma readmissions with a focus on the potential explanatory role of hardships that might be addressed in future patient care models.
METHODS:
We enrolled 774 children, aged 1 to 16 years, admitted for asthma or bronchodilator-responsive wheezing in a population-based prospective observational cohort. The outcome was time to readmission. Child race, socioeconomic status (measured by lower income and caregiver educational attainment), and hardship (caregivers looking for work, having no one to borrow money from, not owning a car or home, and being single/never married) were recorded. Analyses used Cox proportional hazards.
RESULTS:
The cohort was 57% African American, 33% white, and 10% multiracial/other; 19% were readmitted within 12 months. After adjustment for asthma severity classification, African Americans were twice as likely to be readmitted as whites (hazard ratio: 1.98; 95% confidence interval: 1.42 to 2.77). Compared with whites, African American caregivers were significantly more likely to report lower income and educational attainment, difficulty finding work, having no one to borrow money from, not owning a car or home, and being single/never married (all P ≤ .01). Hardships explained 41% of the observed racial disparity in readmission; jointly, socioeconomic status and hardship explained 49%.
CONCLUSIONS:
African American children were twice as likely to be readmitted as white children; hardships explained >40% of this disparity. Additional factors (eg, pollution, tobacco exposure, housing quality) may explain residual disparities. Targeted interventions could help achieve greater child health equity.
Keywords: childhood asthma, readmissions, racial disparities, pediatrics
What’s Known on This Subject:
Asthma morbidity disproportionately affects racial minorities and disadvantaged children. Differences in socioeconomic status and genetics have been offered as explanations but an in-depth understanding of differences in hardships may better explain disparities and also help to identify intervention targets.
What This Study Adds:
Among children admitted for asthma, African Americans were twice as likely to be readmitted as whites. Nearly half the disparity was explained by socioeconomic status and hardships. Community-based interventions targeting hardships may be more feasible given emerging health care payment reform.
Racial disparities are widespread and persistent.1,2 Asthma is the most common chronic physical health condition of childhood, and morbidity disproportionately affects racial minorities.3–10 Population-based studies that report racial disparities, however, rarely include patient-level details beyond traditional sociodemographic factors.9 Further characterization of the challenges families face may help identify risks amenable to both clinical and public health interventions that could prevent subsequent morbidity and reduce disparities.11 Such a focus on prevention could be especially relevant with emerging health care reform in which payment is based on outcomes and coordinated community-based care becomes more feasible.
Asthma-related disparities extend to children of socioeconomic disadvantage.12,13 Measurement of disadvantage, frequently conceptualized as socioeconomic status (SES), is often crude, failing to capture the varied challenges in patients’ lives.14–16 Failure to fully account for racial variability in disadvantage can lead to prematurely ascribing racial outcome differences to genetic factors,17–19 missing opportunities for socioeconomic risk identification and mitigation. Given that racial disparities likely operate, at least in part, through socioeconomic disadvantage,13 a more complete and effective understanding of this relationship is essential.20–24
Measures of financial and social hardship, or strain, can highlight challenges families confront in the setting of limited resources.25,26 African Americans are more likely to experience competing household priorities14 and hardships, even after adjustment for income and education.27–29 Personalizing and refining screening to more adequately identify drivers of disparities are increasingly relevant to clinical care in the era of accountable, coordinated care. Adding hardship to patient- and population-level assessments could determine where disparity-reducing investments could be targeted, elevating financial and social screening and interventions to the level of medical tests and treatments.30,31
Thus, we first sought to characterize racial differences in time to asthma-related readmission in a population-based pediatric cohort. Second, we aimed to assess the degree to which SES and markers of financial and social hardship explained expected racial disparities in readmissions.
Methods
Study Design and Population
We analyzed data from a population-based, prospective observational cohort at Cincinnati Children’s Hospital Medical Center (CCHMC), a large, urban academic pediatric facility. Data were available for 774 patients, aged 1 to 16 years, enrolled in the Greater Cincinnati Asthma Risk Study (GCARS) cohort between August 11, 2010, and October 20, 2011. GCARS also included children admitted to a nearby satellite inpatient facility beginning November 1, 2010. Because Ohio Hospital Association data indicate that ∼85% of all asthma admissions for children aged 1 to 16 years within our 8-county primary service area occur at CCHMC facilities, the accrued admission sample was considered population-based.32,33
Patients were identified by the admitting physician’s use of the evidence-based clinical pathway for acute asthma or bronchodilator-responsive wheezing. Children who were removed from the pathway before discharge, who had significant respiratory or cardiovascular comorbidities (eg, cystic fibrosis, congenital heart disease), who resided outside of the 8-county service area, or whose primary caregiver did not understand written or spoken English (∼2% of those otherwise eligible) were excluded. Study recruitment took place, on average, 7 days per week and 12 hours per day. The CCHMC Institutional Review Board approved this study.
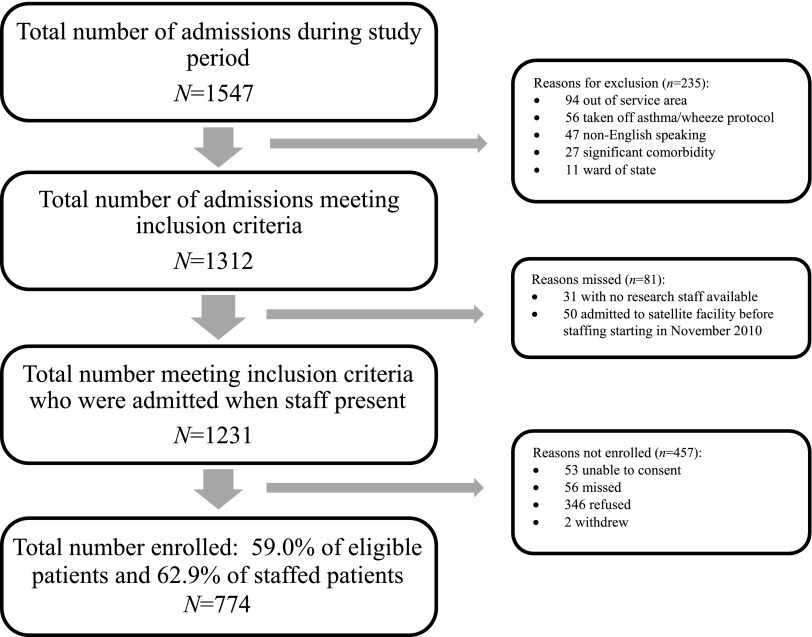
During the enrollment period, 1312 patients met inclusion criteria (Fig 1). Of the 1312 eligible, 81 (6.2%) were admitted when research personnel were unavailable. Research personnel were unable to obtain consent for 53 (4.0%) patients who had no parent or guardian available. Fifty-six (4.3%) patients were missed as a result of difficulty completing the consent process because of high patient census or competing patient care priorities. Finally, 346 (26.4%) refused to participate, and 2 withdrew after consent but before completion of any study procedures. Altogether, research personnel enrolled 59.0% of those eligible and 62.9% of those eligible with staff available to recruit.
FIGURE 1.
Recruitment diagram for patients enrolled in the GCARS between August 2010 and October 2011.
A 25% subsample of all those enrolled were contacted by telephone ∼12 months after index admission to assess potential loss to follow-up or admission to non-CCHMC sites. The subsample was selected by using block randomization (blocking was used due to the seasonality of asthma morbidity). The 774 enrolled patients were divided into groups of 20 with 5 randomly chosen subjects in each block then selected for follow-up. If staff were unable to complete the call, the subject’s current home address was identified by using the electronic medical record and/or public records; 95.9% of those in this subsample were confirmed as having maintained residence in CCHMC’s primary service area. Of those reached by telephone (n = 164, 84% of possible participants), none reported an admission to a hospital other than CCHMC during the follow-up period.
Outcome and Predictors
The primary outcome was asthma-related readmission, assessed as both time to first readmission and any readmission within 12 months. Readmission data were captured by International Classification of Diseases, Ninth Revision, Clinical Modification, classification codes of primary or secondary discharge diagnoses (493.XX or 786.07 for asthma or wheeze, respectively)34 recorded in hospital billing data. Outcome accuracy was verified by electronic medical record review to ensure that readmissions met the same inclusion and exclusion criteria as index admissions. Time to readmission was calculated as the interval between the discharge date of the index admission and the date of the first readmission for asthma or wheezing. Censoring occurred at the end of the follow-up period (October 2012) for those not readmitted.
We obtained demographic variables, asthma severity classification,35 and measures of household SES and hardship from a face-to-face survey completed with each patient’s caregiver during the index admission. Severity was classified by using survey responses assessing symptoms and control in the 4 weeks preceding the exacerbation; specific therapeutic steps could not be verified. Patient race was defined according to caregiver report. Caregivers could choose ≥1 of the following US Census categories: white/Caucasian, black/African American, Asian/Oriental or Pacific Islander, American Indian or Alaskan Native, or other.36 Ethnicity was characterized as Hispanic/non-Hispanic. For this study, racial categories were collapsed to African American, white, and multiracial/other. Children identified as Hispanic were included in the multiracial/other category. Given the study aims and small numbers in the multiracial/other category, primary analyses were conducted in African Americans and whites.
SES was measured by using income, adjusted for household size, and primary caregiver educational attainment. Annual household income, household size, and educational attainment were collected as ordinal variables. Annual income per household person was calculated by dividing the midpoint of the reported income category by the number of persons reported to be in the household. Dichotomization of this income variable and educational attainment improved model fit when relationships with readmission were assessed; there were natural breakpoints in observed associations without evidence of dose response. For annual income per household person, dichotomization occurred at $15 000, an approximation of the federal poverty line.37 Those with incomes of <$15 000 per household person were considered “at risk.” Caregivers who had completed high school or had less than a high school education were considered at risk.
Financial and social hardship was characterized by using previously validated questions.25,38,39 Ten candidate survey questions were included. Financial hardship was assessed via difficulty making ends meet, looking for work but being unable to find it, being unable to pay rent or utilities for financial reasons, having to move in with others for financial reasons, and having had property repossessed. Social hardship was assessed via a household’s inability to borrow money during times of need. Those answering “yes” to any of these questions were considered at risk. Wealth was assessed via home and car ownership, with car ownership also allowing for an assessment of transportation access. Those not owning a home or car were considered at risk. Finally, those who were single and never married were conceptualized as having less help with their child’s health care and more child care challenges than those in other categories of marital status40 and were therefore considered at risk.
Statistical Analyses
Bivariate associations compared African American and white children with respect to demographic characteristics, asthma severity classification, SES, and hardship by using χ2 statistics. Kaplan-Meier curves and log-rank statistics compared African Americans and whites with respect to time to readmission. Bivariate associations between key predictors and time to readmission were assessed by using Cox proportional hazards regression.
To evaluate the extent to which SES and hardship explained the increased risk of readmission in African American children, we focused on variables at least marginally associated (P < .2) with both race and time to readmission. We then used inverse probability weighting (IPW) to calculate an African American’s risk of readmission should he or she have the same distribution of SES and hardship risks as his or her white counterparts. Similar methods have been previously used to investigate health disparities related to race.15,41
By using IPW, we constructed a series of Cox proportional hazards models, adjusted for asthma severity, with the outcome being time to readmission. Model 1 included race as a predictor, model 2 included race and SES variables (income and educational attainment), and model 3 included race and hardship variables that met our significance criteria (looking for work, ability to borrow money, home ownership, car ownership, and marital status). Model 4 included race alongside SES and hardship measures included in models 2 and 3. The extent to which SES and hardship explained the relationship between race and time to readmission was assessed by the percentage change in the parameter estimated for race. This reduction was interpreted as quantification of the degree to which SES and hardship explained the racial disparity in readmission hazard. Bootstrapping was used to obtain confidence intervals (CIs) around this quantification. All analyses used SAS statistical software (version 9.3; SAS Institute, Cary, NC).
Results
A total of 774 children were enrolled in GCARS. Our sample was 57% African American, 33% white, and 64% male with a mean age of 6.2 years (Table 1). A total of 83% reported annual income per household person as <$15 000; 43% of caregivers had a high school education or less. Additionally, 45% of caregivers reported that they were looking but unable to find work, and just 22% of caregivers reported that they owned their home. More than 60% of caregivers were single, having never married. Compared with whites, African American caregivers were significantly more likely to be at risk of each SES and hardship variable: they were more likely to report lower income per household person and educational attainment, difficulty finding work, having no one to borrow money from, not owning a car or home, and being single/never married (all P ≤ .01).
TABLE 1.
Demographic, Socioeconomic, and Hardship Characteristics and Distribution by Race for Patients Enrolled in the GCARS Between August 2010 and October 2011
| Characteristic | n | % | African American (n = 441), %a | White (n = 254), %a | Multiracial/Other (n = 76), %a | Pb |
|---|---|---|---|---|---|---|
| Age | ||||||
| <4 years | 294 | 38 | 34 | 41 | 53 | .14 |
| 4–11 years | 396 | 51 | 55 | 49 | 37 | |
| ≥12 years | 81 | 11 | 11 | 9 | 11 | |
| Gender | ||||||
| Male | 503 | 65 | 63 | 67 | 66 | .35 |
| Female | 271 | 35 | 37 | 33 | 34 | |
| Asthma severity classification | .03 | |||||
| Mild intermittent | 261 | 34 | 32 | 36 | 38 | |
| Mild persistent | 318 | 41 | 40 | 44 | 45 | |
| Moderate persistent | 145 | 19 | 22 | 16 | 12 | |
| Severe persistent | 44 | 6 | 7 | 4 | 5 | |
| Health insurance | ||||||
| Public | 562 | 73 | 89 | 50 | 67 | <.01 |
| Private | 171 | 22 | 10 | 44 | 28 | |
| Self-pay | 27 | 4 | 2 | 7 | 5 | |
| SES | ||||||
| Annual household income | ||||||
| <$15 000 | 261 | 34 | 46 | 14 | 30 | <.01 |
| $15 000–$29 999 | 212 | 28 | 29 | 24 | 29 | |
| $30 000–$44 999 | 108 | 14 | 12 | 17 | 17 | |
| $45 000–$59 999 | 46 | 6 | 5 | 9 | 3 | |
| $60 000–$89 999 | 78 | 10 | 5 | 19 | 9 | |
| ≥$90 000 | 55 | 8 | 2 | 15 | 12 | |
| Annual income per household person | .16 | |||||
| <$15 000 | 627 | 83 | 91 | 68 | 83 | |
| ≥$15 000 | 132 | 17 | 9 | 32 | 17 | |
| Caregiver educational attainment | ||||||
| Less than high school graduate | 121 | 16 | 19 | 10 | 16 | <.01 |
| High school or GED but not more | 204 | 27 | 28 | 27 | 18 | |
| Some college | 220 | 30 | 30 | 23 | 37 | |
| Two-year college or technical school graduate | 83 | 11 | 11 | 10 | 13 | |
| Four-year college graduate | 82 | 11 | 7 | 17 | 9 | |
| Any postgraduate work | 34 | 5 | 2 | 9 | 5 | |
| Financial and social hardship | ||||||
| Looking for work, unable to find | ||||||
| Yes | 342 | 45 | 55 | 27 | 42 | <.01 |
| No | 426 | 55 | 45 | 72 | 58 | |
| Unable to borrow money in time of need | ||||||
| Yes | 412 | 54 | 58 | 46 | 54 | <.01 |
| No | 358 | 46 | 42 | 54 | 46 | |
| Owns home | ||||||
| No | 599 | 78 | 90 | 58 | 75 | <.01 |
| Yes | 170 | 22 | 10 | 42 | 25 | |
| Owns car | ||||||
| No | 215 | 28 | 39 | 9 | 26 | <.01 |
| Yes | 553 | 72 | 61 | 91 | 74 | |
| Marital status | ||||||
| Single, never married | 484 | 63 | 82 | 37 | 39 | <.01 |
| Divorced/widowed/separated | 77 | 10 | 7 | 13 | 16 | |
| Married | 209 | 27 | 11 | 50 | 45 | |
GED, General Educational Development.
Percentages were rounded and thus may add up to more or less than 100.
P value compares African American children and white children using χ2 statistics, and Cochran-Mantel-Haenszel statistics for asthma severity, income, and education.
Compared with enrolled children, those who were eligible but not enrolled did not differ with respect to age, gender, or readmission rate at 12 months. Enrolled children were, however, more likely to be African American and publicly insured. There were no significant differences between children receiving and those not receiving the follow-up phone call.
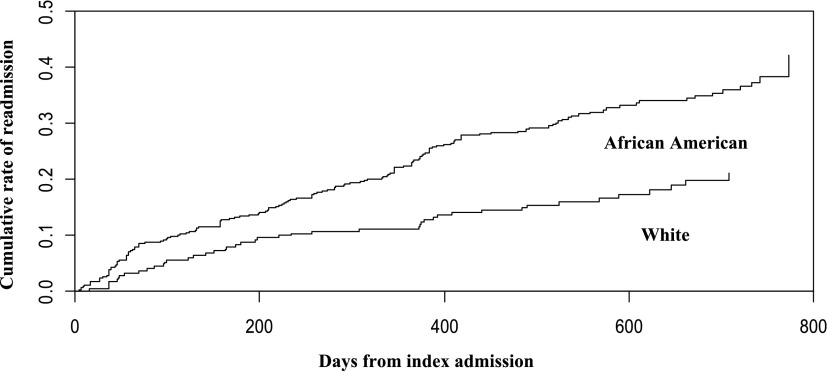
Overall, 18.6% of enrolled children were readmitted for asthma or bronchodilator-responsive wheezing within 12 months. African Americans were more than twice as likely to be readmitted as whites (23% vs 11%) and had a significantly shorter time to readmission: it took 114 days for 10% of African Americans to be readmitted compared with 234 days for whites (P < .01) (Fig 2). Bivariate analyses indicated that time to readmission was marginally associated with both annual income per household person (P = .1) and caregiver educational attainment (P = .17) (Table 2). For the included hardship variables, time to readmission was at least marginally associated with the caregiver actively looking for work but being unable to find it, having no one to borrow money from in a time of need, not owning a home, not owning a car, and being single/never married (all P < .1).
FIGURE 2.
Survival curve showing African American–white differences in hospital readmission for patients enrolled in the GCARS between August 2010 and October 2011 and followed through October 2012. Cumulative rates of readmission after index admission were estimated by using a 1–Kaplan-Meier survival curve (P < .01, log-rank test).
TABLE 2.
Bivariate Relationships Between Race and Demographic, Socioeconomic, and Hardship Characteristics Using Hazard of Readmission for Patients Enrolled in the GCARS between August 2010 and October 2011 and Followed Through October 2012
| Hazard of Readmissiona | 95% CI | |
|---|---|---|
| Race | ||
| African American | 2.07 | 1.48 to 2.89 |
| White | Reference | |
| Asthma severity classification | ||
| Severe persistent | 1.83 | 1.07 to 3.14 |
| Moderate persistent | 1.70 | 1.18 to 2.46 |
| Mild persistent | 1.12 | 0.80 to 1.56 |
| Mild intermittent | Reference | |
| Annual income per household person | ||
| <$15 000 | 1.39 | 0.94 to 2.05 |
| ≥1$15 000 | Reference | |
| Caregiver educational attainment | ||
| High school or less | 1.21 | 0.92 to 1.60 |
| More than high school | Reference | |
| Looking for work, unable to find | ||
| Yes | 1.35 | 1.03 to 1.77 |
| No | Reference | |
| Unable to borrow money in time of need | ||
| Yes | 1.26 | 0.96 to 1.65 |
| No | Reference | |
| Owns home | ||
| No | 1.59 | 1.10 to 2.29 |
| Yes | Reference | |
| Owns car | ||
| No | 1.57 | 1.19 to 2.08 |
| Yes | Reference | |
| Marital status | ||
| Single, never married | 1.69 | 1.20 to 2.38 |
| Married | Reference |
Outcome was time to hospital readmission with hazard ratios obtained by using unadjusted Cox proportional hazards.
Table 3 shows the analytic approach to identifying the degree to which SES and hardship explained observed racial disparities. After adjustment for asthma severity, model 1 shows that African Americans still had double the hazard of readmission (hazard ratio: 1.98; 95% CI: 1.42 to 2.77). In model 2, the parameter estimate for race was unchanged after inclusion of the SES variables. In model 3, however, financial and social hardship variables were found to explain 41% of racial differences. When both SES and hardship were included with race in model 4, nearly 49% (95% CI: −2.2% to 111.0%) of race’s association with readmission was explained. This reduction nearly met statistical significance, and the adjusted hazard for readmission for African Americans decreased from 1.98 to 1.44.
TABLE 3.
Association of African American Race With Readmission Accounting for Socioeconomic and Hardship Covariates Using IPW for Patients Enrolled in the GCARS Between August 2010 and October 2011 and Followed Through October 2012
| Race Parameter Estimate | Hazard Ratio (95% CI) | Percentage Reduction in Race Parameter Estimate (95% CI)a | |
|---|---|---|---|
| Model 1: no SES or strain covariatesb | 0.68 | 1.98 (1.42 to 2.77) | — |
| Model 2: SES covariatesc | 0.69 | 1.99 (1.45 to 2.74) | −0.2 (−23.7 to 24.0) |
| Model 3: strain covariatesd | 0.42 | 1.52 (1.13 to 2.04) | 40.6 (−5.5 to 94.4) |
| Model 4: SES and strain covariatese | 0.37 | 1.44 (1.07 to 1.96) | 48.5 (−2.2 to 111.0) |
Parameter estimate obtained by using IPW with Cox proportional hazards regression; 95% CIs obtained by using bootstrapping.
Model 1 includes race alone, adjusted for asthma severity classification.
Model 2 includes race and SES variables (reported income and caregiver educational attainment), adjusted for asthma severity classification.
Model 3 includes race and hardship variables (looking for work but unable to find, need to borrow money, home ownership, car ownership, marital status), adjusted for asthma severity classification.
Model 4 includes race, SES, and hardship variables, adjusted for asthma severity classification.
Discussion
Child health continues to be characterized by pervasive and persistent disparities. Among children admitted for asthma or wheezing, African Americans were twice as likely to be readmitted as whites. We quantified that >40% of the observed disparity could be explained by financial and social hardship. Together with traditional measures of SES, hardships explained almost 50%. Readmission rates are a central focus of health care reform in the United States, and reducing disparities in such outcomes will be critical. Our findings suggest that a more intense patient- and population-level focus on the financial and social hardships that underlie racial disparities may provide 1 path for achieving better outcomes.
The racial disparities in asthma-related readmissions observed in our population-based cohort align with previous accounts nationally.3,9 For example, a retrospective analysis in all children admitted for asthma over a 10-year period in St Louis, Missouri, found that African American children were at a 50% greater risk of having multiple admissions.5 No previous studies, to our knowledge, have analyzed population-based readmission differences by race with the patient-level detail available in this cohort, details that may inform interventions for clinicians and public health officials alike.42
In an attempt to more deeply characterize racial disparities, we focused on socioeconomic determinants of health.13,15,43 To assess the impact of SES, we used caregiver reports of income and educational attainment. Surprisingly, these markers of SES explained none of the observed racial readmission difference. Although some have suggested that such a finding could support the genetic basis for disparities,44 we expect that these measures of SES, taken alone, do not adequately characterize racial differences in socioeconomic adversity experienced day to day and over the life course.20,45
Hardship complements SES and provides a more textured characterization of such day-to-day challenges.1 Each marker of financial and social hardship was chosen given hypothesized relationships with both race and readmission, and the potential for such information to change clinical practice. For example, certain hardships (eg, job-seeking, transportation barriers) may be amenable to intervention, including social services consultation, connections to community resources, or medication home delivery. Other factors (eg, ability to borrow money, marital status, home ownership) may benefit from in-depth screening regarding a family’s support structure, barriers to medication adherence, or lower expectations for asthma control.14
Alone, these hardship markers explained ∼41% of observed racial readmission differences. Jointly, SES and hardship explained nearly half of the observed disparity. This finding supports the notion that hardship identification could prompt partnerships with individuals and agencies poised to add support to lives characterized by disadvantage.42 Recent work with social services, public health officials, and legal aid advocates highlights the impact that such interventions can have for individual patients and populations.36,46–48 Enhanced, scaled partnerships of this sort may be especially relevant as health care reform pushes clinicians to find cost-effective methods for reducing health service utilization.30 Nationally, identifying where social service and public health expenditures can be augmented may also prove impactful.31 The increased focus on clinical quality metrics and payment for health outcomes and disparity reduction, not simply for volume of care, would support a broadened approach to these types of health interventions.49,50
Additional factors are also likely to affect and explain residual disparities. For example, differential access to care has been linked to both increased risk of readmission and race (African Americans use less ambulatory care and more acute care compared with whites).9,51 Similarly, previous work has revealed differential adherence to asthma controllers and lower expectations of asthma control among African Americans.14 Exposures to pollution, tobacco, or substandard housing conditions may also explain persistent differences while presenting opportunities for intervention.
Genes, too, have been postulated to drive racial differences in asthma morbidity.44 The distribution of asthma-related genes, however, varies by and within race, and a gene’s impact often depends on coexistent social and environmental exposures. This fact ought to provoke caution before the personalization of asthma care relies solely on genetic factors or measured biomarkers.22,52,53 Personalized management of asthma may benefit from complementing genetics with a focus on financial or social hardships that could guide hospital- and community-based resources to those with the most to gain.54 Additionally, whenever critically appraising conclusions highlighting genes as a basis for health disparities, the issue of residual confounding, of not accurately measuring the underlying variables that affect racial disparities, should be taken into account.17
There were limitations to this study. First, asthma admission data were only available for children hospitalized at CCHMC facilities; children may have been admitted elsewhere. Local data indicate, however, that CCHMC cares for ∼85% of all childhood asthma admissions in the 8-county service area.32 Additionally, none of the 164 patients reached 1 year after index admission reported being admitted elsewhere. Second, our sample was composed primarily of African American and white children, limiting generalizability. Third, there were significant differences with respect to race and insurance between those enrolled and those not enrolled. Given that enrolled children were likely at “higher risk,” we expect that this fact, if anything, would bias our findings toward the null. Fourth, wide CIs surrounding our estimates of the percentage of racial disparity explained resulted from loss of power upon inclusion of additional covariates in the IPW model. Finally, although SES and hardship explained nearly half of observed racial disparities, we are unable to prove that they caused differences in readmission risk to occur.
Conclusions
In a population-based cohort of children admitted with asthma or bronchodilator-responsive wheezing, African Americans were twice as likely to be readmitted as whites. This disparity was partially explained by financial and social hardship, which added measurably to SES. Highlighting the role of a child’s financial and social environment is especially relevant as targeted approaches to risk identification and mitigation are explored. In the future, we will assess potential explanations for residual racial disparities including differential access to care and expectations of care, alongside exposure to air pollution, tobacco smoke, substandard housing conditions (eg, mold, pest infestation), violent crime, and racial discrimination. We also plan to determine how knowledge of such factors could be efficiently translated into testable interventions aimed at improving outcomes and reducing disparities.
Acknowledgments
We thank Kelly Antony for database management and GCARS clinical research coordinators Emily Greenberg, Angela Howald, Elizabeth Monti, Stacey Rieck, and Heather Strong for their support and dedication.
Glossary
- CCHMC
Cincinnati Children’s Hospital Medical Center
- GCARS
Greater Cincinnati Asthma Risks Study
- IPW
inverse probability weighting
- SES
socioeconomic status
Footnotes
Drs Beck and Simmons participated in the study concept and design, acquisition of data, analysis and interpretation, drafting and critical revision of the manuscript, statistical analysis, and study supervision; Drs Huang, Moncrief, Ryan, and Kahn participated in the study concept and design, analysis and interpretation, drafting and critical revision of the manuscript, statistical analysis, and study supervision; Ms Sauers participated in the study concept and design, acquisition of data, analysis and interpretation, and drafting and critical revision of the manuscript; Dr Chen participated in the study concept and design, analysis and interpretation, statistical analysis, and drafting and critical revision of the manuscript; Dr Newman participated in the study concept and design, analysis and interpretation, and drafting and critical revision of the manuscript; and all authors approved the final manuscript as submitted.
This article is subject to the NIH Public Access Policy (http://publicaccess.nih.gov).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The Greater Cincinnati Asthma Risks Study (GCARS) was funded with support from NIH 1R01AI88116 (principal investigator: Dr Kahn; co-investigators: Drs Beck, Simmons, Moncrief, Ryan, Newman, and Huang). The use of REDCap was supported by the Center for Clinical and Translational Science and Training (NCRR/NIH UL1-RR026314-01). Dr Beck also received funding through the Cincinnati Children’s Hospital Medical Center Procter Scholar Award. The funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Hill TD, Graham LM, Divgi V. Racial disparities in pediatric asthma: a review of the literature. Curr Allergy Asthma Rep. 2011;11(1):85–90 [DOI] [PubMed] [Google Scholar]
- 2.Mehta NK, Lee H, Ylitalo KR. Child health in the United States: recent trends in racial/ethnic disparities. Soc Sci Med. 2013;95:6–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ash M, Brandt S. Disparities in asthma hospitalization in Massachusetts. Am J Public Health. 2006;96(2):358–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chabra A, Chávez GF, Adams EJ, Taylor D. Characteristics of children having multiple Medicaid-paid asthma hospitalizations. Matern Child Health J. 1998;2(4):223–229 [DOI] [PubMed] [Google Scholar]
- 5.Bloomberg GR, Trinkaus KM, Fisher EB, Jr, Musick JR, Strunk RC. Hospital readmissions for childhood asthma: a 10-year metropolitan study. Am J Respir Crit Care Med. 2003;167(8):1068–1076 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention . Asthma hospitalizations and readmissions among children and young adults—Wisconsin, 1991-1995. MMWR Morb Mortal Wkly Rep. 1997;46(31):726–729 [PubMed] [Google Scholar]
- 7.Gupta RS, Carrión-Carire V, Weiss KB. The widening black/white gap in asthma hospitalizations and mortality. J Allergy Clin Immunol. 2006;117(2):351–358 [DOI] [PubMed] [Google Scholar]
- 8.Stewart KA, Higgins PC, McLaughlin CG, Williams TV, Granger E, Croghan TW. Differences in prevalence, treatment, and outcomes of asthma among a diverse population of children with equal access to care: findings from a study in the military health system. Arch Pediatr Adolesc Med. 2010;164(8):720–726 [DOI] [PubMed] [Google Scholar]
- 9.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009;123(suppl 3):S131–S145 [DOI] [PubMed] [Google Scholar]
- 10.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005-2009. Natl Health Stat Rep. 2011(32):1–14 [PubMed]
- 11.Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol. 2009;123(6):1209–1217; quiz 1218–1209 [DOI] [PMC free article] [PubMed]
- 12.Kim H, Kieckhefer GM, Greek AA, Joesch JM, Baydar N. Health care utilization by children with asthma. Prev Chronic Dis. 2009;6(1):1–12 [PMC free article] [PubMed] [Google Scholar]
- 13.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(suppl 3):S174–S184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith LA, Bokhour B, Hohman KH, et al. Modifiable risk factors for suboptimal control and controller medication underuse among children with asthma. Pediatrics. 2008;122(4):760–769 [DOI] [PubMed] [Google Scholar]
- 15.Do DP, Frank R, Finch BK. Does SES explain more of the black/white health gap than we thought? Revisiting our approach toward understanding racial disparities in health. Soc Sci Med. 2012;74(9):1385–1393 [DOI] [PubMed] [Google Scholar]
- 16.Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56(4):769–784 [DOI] [PubMed] [Google Scholar]
- 17.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8(6):621–628 [PubMed]
- 18.Tran HN, Siu S, Iribarren C, Udaltsova N, Klatsky AL. Ethnicity and risk of hospitalization for asthma and chronic obstructive pulmonary disease. Ann Epidemiol. 2011;21(8):615–622 [DOI] [PubMed] [Google Scholar]
- 19.Erickson SE, Iribarren C, Tolstykh IV, Blanc PD, Eisner MD. Effect of race on asthma management and outcomes in a large, integrated managed care organization. Arch Intern Med. 2007;167(17):1846–1852 [DOI] [PubMed] [Google Scholar]
- 20.Williams DR. Miles to go before we sleep: racial inequities in health. J Health Soc Behav. 2012;53(3):279–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright RJ. Epidemiology of stress and asthma: from constricting communities and fragile families to epigenetics. Immunol Allergy Clin North Am. 2011;31(1):19–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Drake KA, Galanter JM, Burchard EG. Race, ethnicity and social class and the complex etiologies of asthma. Pharmacogenomics. 2008;9(4):453–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen E, Miller GE, Walker HA, Arevalo JM, Sung CY, Cole SW. Genome-wide transcriptional profiling linked to social class in asthma. Thorax. 2009;64(1):38–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sidora-Arcoleo K, Feldman JM, Serebrisky D, Spray A. A multi-factorial model for examining racial and ethnic disparities in acute asthma visits by children. Ann Behav Med. 2012;43(1):15–28 [DOI] [PMC free article] [PubMed]
- 25.Ouellette T, Burstein N, Long D, Beecroft E. Measures of material hardship: final report, U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. 2004. Available at: http://aspe.hhs.gov/hsp/material-hardship04/index.htm. Accessed May 25, 2013
- 26.Chen E, Bloomberg GR, Fisher EB, Jr., Strunk RC. Predictors of repeat hospitalizations in children with asthma: the role of psychosocial and socioenvironmental factors. Health Psychol. 2003;22(1):12–18 [DOI] [PubMed]
- 27.Bauman K. Direct measures of poverty as indicators of economic need: evidence from the Survey of Income and Program Participation. US Census Bureau; 1998. Population Division Technical Working Paper No. 30. Available at: www.census.gov/population/www/documentation/twps0030/twps0030.html. Accessed May 25, 2013
- 28.Orzechowski S, Sepielli P. Net worth and asset ownership of households: 1998 and 2000. Washington, DC: Housing and Household Economic Statistics Division, US Census Bureau; 2003:70–88. Available at: www.census.gov/prod/2003pubs/p70-88.pdf. Accessed January 19, 2008
- 29.Williams DR. Racial inequalities in health: the social determinants of disease. 2007. Available at: www.wilsoncenter.org/events/docs/Williams.pdf. Accessed February 1, 2008
- 30.Pollack CE, Armstrong K. Accountable care organizations and health care disparities. JAMA. 2011;305(16):1706–1707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bradley EH, Elkins BR, Herrin J, Elbel B. Health and social services expenditures: associations with health outcomes. BMJ Qual Saf. 2011;20(10):826–831 [DOI] [PubMed]
- 32.Bosnjakovic E. INSIGHT Database. Columbus, OH: Ohio Hospital Association; 2009 [Google Scholar]
- 33.Szklo M. Population-based cohort studies. Epidemiol Rev. 1998;20(1):81–90 [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision, Clinical Modification. 2011. Available at: www.cdc.gov/nchs/icd/icd9cm.htm. Accessed May 25, 2013
- 35.National Asthma Education and Prevention Program . Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma—summary report 2007. J Allergy Clin Immunol. 2007;120(5 suppl):S94–S138 [DOI] [PubMed] [Google Scholar]
- 36.Klein MD, Beck AF, Henize AW, Parrish DS, Fink EE, Kahn RS. Doctors and lawyers collaborating to HeLP children—outcomes from a successful partnership between professions. J Health Care Poor Underserved. 2013;24(3):1063–1073 [DOI] [PubMed] [Google Scholar]
- 37.George-Abraham JK, Martin LJ, Kalkwarf HJ, et al. Fractures in children with neurofibromatosis type 1 from two NF clinics. Am J Med Genet A. 2013;161A(5):921–926 [DOI] [PubMed] [Google Scholar]
- 38.Jencks C, Mayer S. Poverty and the distribution of material hardship. J Hum Resour. 1989;24(1):88–114 [Google Scholar]
- 39.Danziger S, Corcoran M, Danziger S, Heflin C. Work, income, and material hardship after welfare reform. J Consum Aff. 2000;34(1):6–30 [Google Scholar]
- 40.Moncrief T, Beck AF, Simmons JM, Huang B, Kahn RS. Single Parent Households and Increased Asthma Morbidity [published online ahead of print December 10, 2013]. J Asthma. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Austin PC. The performance of different propensity score methods for estimating marginal hazard ratios. Stat Med. 2013;32(16):2837–2849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA Intern Med. 2013;173(11):1017–1020 [DOI] [PubMed] [Google Scholar]
- 43.Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51(suppl):S15–S27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kumar R, Tsai HJ, Hong X, et al. African ancestry, early life exposures, and respiratory morbidity in early childhood. Clin Exper Allergy. 2012;42(2):265–274 [DOI] [PMC free article] [PubMed]
- 45.Pollack CE, Cubbin C, Sania A, et al. Do wealth disparities contribute to health disparities within racial/ethnic groups? J Epidemiol Community Health. 2013;67(5):439–445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beck AF, Klein MD, Schaffzin JK, Tallent V, Gillam M, Kahn RS. Identifying and treating a substandard housing cluster using a medical-legal partnership. Pediatrics. 2012;130(5):831–838 [DOI] [PubMed] [Google Scholar]
- 47.Pettignano R, Bliss LR, Caley SB, McLaren S. Can access to a medical-legal partnership benefit patients with asthma who live in an urban community? J Health Care Poor Underserved. 2013;24(2):706–717 [DOI] [PubMed] [Google Scholar]
- 48.Beck AF, Simmons JM, Sauers HS, et al. Connecting at-risk inpatient asthmatics to a community-based program to reduce home environmental risks: care system redesign using quality improvement methods. Hospital Pediatr. 2013;3(4):326–334 [DOI] [PubMed] [Google Scholar]
- 49.Clancy CM. Commentary: reducing hospital readmissions: aligning financial and quality incentives. Am J Med Qual. 2012;27(5):441–443 [DOI] [PubMed]
- 50.Fiscella K. Health care reform and equity: promise, pitfalls, and prescriptions. Ann Fam Med. 2011;9(1):78–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Auger KA, Kahn RS, Davis MM, Beck AF, Simmons JM. Medical home quality and readmission risk for children hospitalized with asthma exacerbations. Pediatrics. 2013;131(1):64–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dougherty D, Conway PH. The “3T’s” road map to transform US health care: the “how” of high-quality care. JAMA. 2008;299(19):2319–2321 [DOI] [PubMed] [Google Scholar]
- 53.Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. 2010;363(4):301–304 [DOI] [PubMed] [Google Scholar]
- 54.Hacker K, Walker DK. Achieving population health in accountable care organizations. Am J Public Health. 2013;103(7):1163–1167 [DOI] [PMC free article] [PubMed] [Google Scholar]