Abstract
Magnetic resonance imaging (MRI) in rectal cancer was first investigated in 1999 and has become almost mandatory in planning rectal cancer treatment. MRI has a high accuracy in predicting circumferential resection margin involvement and is used to plan neoadjuvant therapy. The accuracy of MRI in assessing mesorectal lymph nodes remains moderate, as there are no reliable criteria to assess nodal involvement. MRI seems to be good in assessing peritoneal involvement in upper rectal cancer; this however has been assessed in only a few studies and needs further research. For low rectal cancers, mesorectum is thin at the level of levator ani especially in relation to prostate; so predicting circumferential resection margin involvement is not easy. However high spatial resolution coronal imaging shows levator muscles, sphincter complex and intersphincteric plane accurately. This is used to stage low rectal tumors and plan plane of surgery (standard surgery, intersphincteric resection, Extralevator abdominoperineal resection). While most centres perform MRI post chemoradiotherapy, its role in accurate staging post neoadjuvant therapy remains debatable. THe role of Diffusion weighted MRI post neoadjuvant therapy is being evaluated in research settings.
Keywords: Magnetic resonance imaging, Rectal cancer, Surgeon
Core tip: Magnetic resonance imaging in rectal cancer is mandatory for a surgeon to plan neoadjuvant therapy. It also helps in planning surgical approach especially in low rectal cancer.
INTRODUCTION
Over the last two decades outcomes of rectal cancer surgery has improved. The principle of sharp dissection in the total mesorectal excision (TME) plane as advocated by Bill Heald and implementation of national training programmes have improved outcomes of rectal cancer surgery[1,2]. The German Rectal Cancer Study Group trial showed that preoperative long course chemoradiotherapy (LCRT) improves 5-year locoregional recurrence rates compared with postoperative LCRT in stage T3, T4, or node-positive patients and with less toxicity[3].
The success of pre-operative therapy over post-operative treatments meant that a technique identifying prognostic factors pre-operatively is of potential benefit in modifying the intensity of pre-operative therapy according to risk of local or distant failure. Careful staging of rectal tumors results in selective pre-operative treatment strategies aimed at reducing local failure and distant failure in high risk patients[4].
In rectal cancer staging, magnetic resonance imaging (MRI) has played a crucial role. In this review, we discuss in brief the history and relevance of rectal MRI through a surgeon’s perspective.
RESEARCH
A systematic search of PubMed, MEDLINE and the Cochrane Library databases was performed from January 1995 to March 2013 using the terms: “MRI and rectal cancer” to identify studies investigating role of MRI in rectal cancer surgery. Using the criteria listed above 1231 articles were identified. After records were screened by abstract, 137 articles were eligible for full text evaluation and 72 were included in the reference list. This review included brief history of MRI in rectal cancer with its role in staging, selecting patients for neoadjuvant therapy, classification rectal cancers and other relevant topics.
History
The first MRI of human body was performed in 1977. In 1980 GE built the first high-field whole body MRI scanner. Blomqvist et al[5] in 1999, performed MRI on rectal cancer specimens concluded that presence of tumor free lateral resection margin could be predicted by MRI of resected specimen when this exceeds 1 mm[5]. However it is Brown et al[6] who used thin section MRI imaging to identify mesorectal fascia in all patients and accurately stage tumors especially T3 tumors. The same group performed MRI in cadaveric sections and in patients before they underwent total mesorectal excision surgery to establish criteria for visualization of the structures relevant to anterior resection of the rectum[7]. The MERCURY (Magnetic Resonance Imaging and Rectal Cancer European Equivalence) Study Group is a multicenter multidisciplinary collaboration formed in 2001. This group evaluated association between MRI and histopathology in measuring depth of tumour invasion beyond the bowel and involvement of the circumferential resection margin (CRM) in rectal cancer specimens[8,9]. Low Rectal Cancer study group (LOREC) is undertaking a study with the primary aim to reduce rate of incomplete excision in these patients from 30% to less than 10%[10].
Principles of MRI scan
Clinical MRI uses the magnetic properties of hydrogen and its interaction with both a large magnetic field and radio waves to produce highly detailed image of human body. By changing parameters on scanner a contrast between tissues can be obtained. T1 images-water and fluid containing tissues dark and fat brighter, basic scan; T2 images-water and fluid containing tissues bright, fat dark suited to show edema; FLAIR sequence-water dark but edema bright.
Special MRI: MR imaging of the rectum may be performed with either an endorectal coil or a phased-array surface coil. While endorectal coil gets better resolution of lesion, it is uncomfortable and cannot be used for stenosing lesion and rectosigmoid tumors. Hence standard MRI includes images with phased-array body coil only.
Diffusion MRI: Diffusion-weighted MRI (DW-MRI) is a functional imaging technique that displays information about the extent and direction of random water motion in tissues. Preclinical and clinical data indicate a number of potential roles of DW-MRI in the characterization of malignancy, including determination of lesion aggressiveness and monitoring response to therapy[11-13].
MRI with super paramagnetic iron oxide: In structures such as lymph nodes, insufficient contrast between normal and diseased tissues requires development of contrast agents. Super paramagnetic iron oxide (SPIO) structure is composed of ferric iron and ferrous iron (coated with a layer of dextran or other polysaccharide). SPIO particles are taken up by phagocytic cells such as monocytes, macrophages, and oligodendroglial cells but not by tumor cells. This SPIO enhanced MRI to enhance nodal resolution is under investigation and has shown promising results in rectal cancer[14,15]. Use of this agent in patients who have complete response after LCRT can be potentially used to identify patients (no lymph node involvement) who may be candidates for local excision yPT0/T2[16]. This agent is not FDA approved for rectal MRI.
Guidelines to perform MRI rectum
The technique for MRI in rectal cancer has been described by Taylor et al[17] (MERCURY study). The clinician provides location of tumor on rigid sigmoidoscopy. There is no need for bowel preparation or intravenous contrast. We use 1.5-T system with phased array coil with the coil positioned from sacral promontory to 10 cm below pubic symphysis. Rectal distention with water may improve the depiction of a primary rectal tumor and the assessment accuracy of a perirectal tumor extension, but it does not improve the accuracy for determining the presence of regional lymph node involvement[18]. This however is not used routinely except selected centres: (1) the first series-sagittal, T2-weighted, fast spin echo from one pelvic sidewall to other, which locates tumor and relation to peritoneal reflection; (2) the second series- large field of view axial sections whole pelvis; (3) the third series-T2 weighted thin slice (3 mm) axial images through rectal cancer perpendicular to long axis rectum; and (4) for low rectal cancers, high spatial resolution coronal imaging to show levator muscles, sphincter complex and intersphincteric plane.
There is no need for post contrast MRI. Only T2 weighted non-fat suppressed sequences in all three orthogonal planes to tumor axial, coronal and sagittal should be used (Figure 1). The findings on scan are recorded on set proforma, which shows MRI based classification of rectal tumors, classification for low rectal tumors, tumor regression grades after LCRT on MRI[19].
Figure 1.
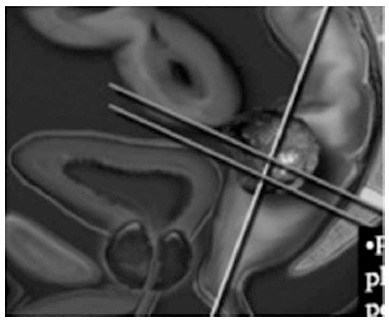
Magnetic resonance imaging technique. T2 weighted non-fat suppressed sequence in all three orthogonal planes to tumor axial, coronal, sagittal should be used.
Normal MRI findings: Anatomy, T2-weighted MR imaging sequences are the most suitable for depicting the rectal wall anatomy. The rectal wall consists of three different layers that can be recognized at MR imaging. Inner hyper-intense layer, which represents the mucosa and submucosa (no differentiation is possible between these two components); an intermediate hypointense layer, which represents the muscularis propria; and an outer hyperintense layer, which represents the perirectal fat tissue. The mesorectal fascia appears as a thin, hypointense line surrounding the hyperintense perirectal fat (Figure 2). At the level of levator ani/prostate mesorectum is thin anteriorly and mesorectal fascia is close to muscularis propria, so accuracy is low[20]. At the level of anal canal, even if the spatial resolution is low compared with endoanal coil imaging, all of the major anatomic structures (levator ani muscle, puborectal muscle, internal and external anal sphincters, anal canal) can easily be evaluated. CRM is considered as closest distance from tumor to MRF (mesorectal fascia and around the levator, tumor invading the intersphincteric plane or extends to within 1 mm of the levator muscle is considered to potentially involve the CRM.
Figure 2.
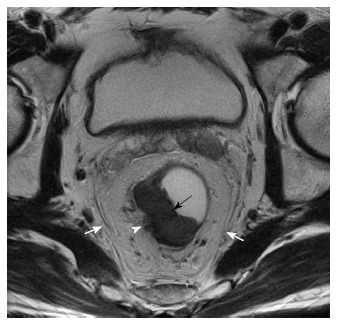
T3 tumor, circumferential resection margin not threatened. T2W axial magnetic resonance imaging image shows a mildly hyperintense proliferative tumor along the right lateral and posterior wall (black arrow). Arrow head shows the tumor reaching upto the muscularis with spiculation in the adjacent perirectal fat. The white arrows show the mesorectal fascia which is not involved/threatened.
Besides normal anatomy, MRI pelvimetry can be used to anticipate problems during TME dissection. Kim et al[21] analysed factors related to difficult Laparoscopic TME (pelvic dissection time). In a prospective study enrolling 74 patients, tumor and patient characteristics (including pelvic dimensions) were analysed with respect to pelvic dissection time. Multivariate analysis showed that patients with longer sacral length, narrow intertuberous diameter and shallow sacral angle on MRI had longer pelvic dissection time but were not associated with increased postoperative complications[21]. Also variations in pelvic dimensions did not predict the risk of CRM involvement in rectal cancer[22].
MRI rectal cancer
It is mandatory to have location of tumor on rigid sigmoidoscopy prior to performing a MRI scan. Location of tumor on MRI and rigid sigmoidoscopy have a 10% discrepancy in location, the difference being 3 cm for anterior tumors while it is 1.2 cm for posterior tumors[23]. For upper rectal cancers, relation to peritoneal reflection is looked out for. Mucinous and non--mucinous rectal tumors can be differentiated with MR Imaging. Mucinous tumors are hetrogenous with intermediate and high SI (signal intensity) on T2-weighted FSE (fast spin echo) images reflecting the mucin content[24,25] Figure 3.
Figure 3.

Mucinous adenocarcinoma of rectum. Sagittal T2 weighted MRI image showing a circumferential rectal tumour with high signal intensity (arrows) characteristic of a mucinous tumor. MRI: Magnetic resonance imaging.
Staging: Tumor staging and EMD (extramural depth of tumor) assessment, There is seldom any dispute about Endo anal ultrasonography being more accurate when compared to MRI for T1/T2 lesions[26]. A recent metanalysis of MRI staging of rectal cancer (T1/T2 vs T3/T4) revealed a sensitivity and specificity of T staging to be 87% and 75%[27], Table 1. Previous studies have described staging failures due to overstaging of T2 lesions with difficulty in the distinction of spiculation in the perirectal fat caused by fibrosis alone compared with that caused by fibrosis that contains tumor cells[28]. Peritumoral fibrosis is represented by spiculation while broad based nodular growth is tumor spread.
Table 1.
Metanalysis of magnetic resonance imaging staging of rectal cancer-Al-Sukhni et al[27]
| Sensitivity% (95%CI) | Specificity% (95%CI) | DOR (95%CI) | |
| T stage | 87 (81-92) | 75 (68-80) | 20.4 (11-37) |
| N stage | 77 (69-84) | 71 (59-81) | 8.3 (4.6-14.7) |
| CRM | 77 (57-90) | 94 (88-97) | 56.1 (15-205) |
DOR: Diagnostic odds ratio; CI: Confidence interval; CRM: Circumferential resection margin.
Although tumor staging with use of the T component of the TNM classification is the traditional method of prognostically stratifying patients, this approach has limitations[26]. The main limitation of T staging is that T3 tumors comprise the majority of rectal cancers seen at presentation, and the outcome of patients with these tumors depends on the depth of extramural spread.
The maximal extramural depth (EMD) of tumor spread, defined on histopathologic analysis as the distance from the outer edge of the longitudinal muscularispropria to the outer edge of the tumor is more related to tumor prognosis and preoperative therapy than T stage alone. In one of the largest series published by a University of Erlangen group, T3 tumors with extramural spread of more than 5 mm were associated with a 5-year cancer-specific patient survival rate of only 54%, but T3 tumors with 5 mm or less of extramural spread regardless of whether lymph node involvement was present were associated with a 5-year cancer-specific survival rate of greater than 85%. T3 tumors with 5 mm or less of extramural spread and pT2 patients showed very similar 5-year survival rates (both lymph node positive and negative patient)[29].
In a prospective study of 679 patients with rectal cancer, MERCURY group demonstrated EMD invasion to be equivalent on MRI and histopathology to a mean difference of less than 0.5 mm[9]. Pederson et al[30] evaluated 168 patients with rectal cancer MRI and histopathological examination and felt measurements of extramural tumor spread are more reproducible among different observers than are 5 mm distance measurements to the anticipated CRM. This EM spread is the basis of classification of T3 tumors on MRI (T3a EMD < 1 mm, T3b 1-5 mm, T3c 5-15 mm, T4 > 15 mm).
NCCN guidelines recommend neoadjuvant LCRT for all T3/T4 tumors irrespective of CRM involvement. However in the United Kingdom, LCRT would be reserved for only T3 tumors with threatened CRM. However it can be suggested, that for T3 tumors with EMD invasion > 5 mm (bad T3) but with clear CRM can undergo preoperative short course radiotherapy rather than surgery alone.
Nodes: Size is not a criteria for lymph node involvement[27]. In fact, one study found that 15% of lymph nodes less than or equal to 5 mm on MRI were involved with metastatic disease[31,32]. A suspicious nodebased on an irregular border or mixed signal intensity had a superior accuracy with a sensitivity of 85% and a specificity of 97%[31] (Figure 4). However, these can be subjective with inter observer variability. Distance of involved node to CRM is important. If suspicious nodes are present, one to three nodes is stage N1 and four or more is stage N2.
Figure 4.
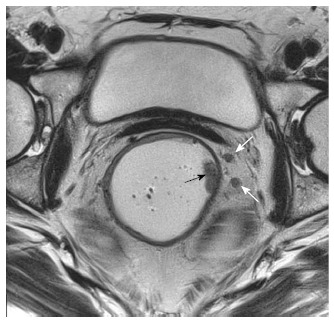
T1 N+ tumor. T2W axial magnetic resonance image shows two small nodes in the mesorectal fat on the left (white arrows) with irregular borders and signal intensity similar to primary tumor along left lateral wall (black arrow).
A metanalysis of MRI staging of rectal cancer revealed a sensitivity and specificity of N staging to be 77% and 71%[27]. This indicates limitation of MRI in assessing mesorectal lymph nodes, which is exacerbated by the lack of agreement on optimal criteria to assess lymph nodes.
However, high-resolution pelvic MRI was more accurate than PET/CT for the prediction of regional nodal status. Magnetic resonance imaging had a high sensitivity and PET/CT had a high specificity for N staging in rectal cancer[33].
Mesorectal fascia and CRM: Although the tumour stage on MRI is an important prognostic factor, it alone may not alter preoperative or operative management. Prediction of the CRM, by contrast, could be clinically useful to select patients for preoperative radiotherapy. MRI prediction of CRM mesorectal fascia (MRF) with final histology was performed by Beets-Tan et al[28]. They concluded that tumour-free margin of at least 1.0 mm could be predicted when the measured distance on MRI was at least 5.0 mm, and a margin of at least 2.0 mm when the MRI distance was at least 6.0 mm. Inter observer agreement was better for CRM than for T stage. However nodes threatening CRM can were difficult to evaluate.
CRM margin 5 mm or 1 mm: While the original study by Beets-tan concluded that MRI prediction of CRM involvement is reliable but suggested the use of a wider threshold on MRI compared to pathology[28]. The MERCURY group based their predicted CRM involvement on MRI to be less than 1 mm. A prospective study by Taylor et al[34] also showed that a cutoff of 1 mm on MRI could be used to predict clear margins with a low positive histologic CRM rate (3.3%)[34].
In the MERCURY group study, the accuracy for predicting the status of CRM by initial imaging or imaging after treatment but before surgery in 408 patients was 88%. Of the 408 patients, 311 underwent primary surgery. The accuracy for prediction of a clear margin was 91% with a negative predictive value of 93%. This compared with an accuracy of 77% and negative predictive value of 98% in patients who had received preoperative chemoradiotherapy or long course radiotherapy[8].
A recent meta analysis to assess accuracy of MRI staging rectal cancer based on 21 studies concluded that MRI specificity was significantly higher for CRM involvement (94%) than for T category (75%) and lymph nodes (71%)[27] Table 2. However MRI can overestimate the CRM involvement in low and anterior tumor with the risk of over treating the patients[35,36].
Table 2.
Classification of low rectal cancers Shihab et al[41]
| Level | Tumor height | Tumor depth | Operative plane |
| 1 | Tumor height between levator origin and puborectalis sling | Confined to muscle | LAR/intersphincteric APE |
| Beyond muscle | LAR/intersphincteric APE | ||
| Tumor < 1 mm MRF/levator | Extralevator APE | ||
| Tumor extending beyond levator | Extralevator APE | ||
| 2 | Tumor at or below puborectalis sling | Submucosal/partial thickness muscle | LAR/intersphincteric APE |
| Full thickness muscle | Extralevator APE | ||
| In to intersphincteric plane | Extralevator APE | ||
| In to external sphincter | Extralevator APE | ||
| Beyond external sphincter into ischiorectal tissue | Pelvic exenteration |
APE: Abdominoperineal excision; LAR: Low anterior; MRF: Mesorectal fascia.
Extramural vascular invasion
Extramural vascular invasion is an important and independent prognostic feature that can be readily identified on MRI. The morphologic features of extramural venous invasion on baseline T2 weighed MRI range from discrete serpiginous or tubular projections of intermediate signal intensity into perirectal fat following the course of a visible vessel to, in more advanced cases, the vessel being expanded by intermediate-signal-intensity tumor and having an irregular contour, Figure 5. The degree of extramural venous invasion system predicts relapse-free survival, with a 3-year relapse-free survival rate of 35% for patients with advanced extramural venous invasion, compared with 74% for those with no or early extramural venous invasion[37].
Figure 5.
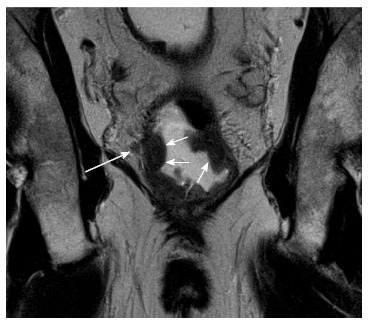
T2 tumor coronol views with extramural venous invasion. Coronal T2W magnetic resonance imaging shows a cicumferential tumor in the rectum (small arrows) reaching the muscularis with extramural venous invasion (long arrow).
Pelvic lymph nodes: While lateral pelvic lymph node dissection (LPLND) is not performed routinely in United Kingdom, this is a good prognostic indicator as evaluated as part of MERCURY study. Patients with rectal cancer and suspicious pelvic side-wall lymph nodes (PSW) on MRI had significantly worse Disease free survival (DFS) that improved with the use of preoperative therapy. Five-year DFS was 42% and 70.7% respectively for patients with, and without suspicious PSW nodes (P < 0.001), but the presence of suspicious nodes had no impact on survival among patients who received preoperative therapy[38]. Based on this, most Mutidisciplinary teams would advocate preoperative LCRT for patients with rectal cancer and suspicious PSW nodes. While most nodes shrink with LCRT, management of persistent PSW nodes after LCRT is not standardized. In South Korea, selective unilateral/bilateral LPLND is performed for persistent PSW after LCRT[39]. From a surgeon’s perspective, localization of these lymph nodes by preoperative MRI is important. At Yonsei university, between 2007 and 2012, of 1686 patients who underwent TME for rectal cancer, 92 (5.4%) patients underwent TME and LPND (unpublished). This however is not evidence based and requires further research.
Peritoneal involvement: Burton et al[40] in a small study showed that tumors of the distal sigmoid, rectosigmoid, and upper rectum can be staged accurately using high spatial resolution MRI and that those with poor prognostic disease including upper rectal cancer (anterior) may benefit from preoperative therapy. However further trials regarding this may be worthwhile.
MRI BASED CLASSIFICATION AND PLANNING THE SURGICAL PROCEDURES FOR LOW RECTAL CANCER
Currently, rectal cancer is classified based on the distance from the anal verge (upper, middle and lower). However, a selection of the optimal surgical procedures by tumor height is not enough. Low rectal tumors especially those treated by abdominoperineal excision (APE), have a high rate of margin involvement when compared with tumors elsewhere in the rectum. Correct surgical management to minimise this rate of margin involvement is reliant on highly accurate imaging, which can be used to plan the planes of excision. Two staging systems for low rectal cancers have been proposed[17,41] (Tables 2 and 3). Shihab et al[42] reported a retrospective analysis of MRI and histopathology data of 33 patients with low rectal cancer. They felt defining plane of surgery preoperatively would be the best way to avoid a positive margin[42].
Table 3.
Classification low rectal cancer (Taylor et al[34] 2008)
| Stage | |
| 1 | Tumor confined to bowel wall, outer muscle intact |
| 2 | Tumor occupies muscle coat but does not enter intersphincteric plane |
| 3 | Tumor enters intersphincteric space or lies within within 1 mm of levator muscle |
| 4 | Invades external anal sphincter or is 1 mm or beyond levator with/without adjacent organ involvement |
Similarly, based on Taylor classification, positive resection margins of patients undergoing APER/Low anterior resections were analysed. Of 101 patients with low rectal cancers (70 APER, 30 ant resection), positive resection margin odds were higher for magnetic resonance Stages 3 to 4 than Stages 1 to 2 by a factor of 17.7 (P < 0.001)[43]. Based on this classification we can plan a tailored procedure as shown below: Stage 1-TME; Stage 2-TME + intersphincteric resection; Stage 3-APER; Stage 4-APER or pelvic exenteration.
MRI for radiotherapy planning
CT scan remains a gold tool for planning radiotherapy for rectal cancer (conformal radiotherapy using 3 dimensional views). Most Radiation oncologists would also have access to MRI views to enable planning i.e., delineation of target volume. Tumour volumes defined on MRI are smaller, shorter and more distal from the anal sphincter than CT-based volumes. For radiotherapy planning, this may result in smaller treatment volumes, which could lead to a reduction in dose to organs at risk and facilitate dose escalation[44,45]. Co-registration of the images where MR images are used for optimal outlining while retaining the CT data for dose calculations is now considered the gold standard in prostate cancer radiotherapy[46]. However for rectal cancer, further research is required regarding this.
MRI as prognostic factors
Following can be used as a prognostic factors on MRI: (1) tumor EMD/T4/CRM; (2) extramural vascular invasion; (3) inflammatory reaction; (4) mucinous tumours; (5) pelvic lymphnodes; and (6) MRI assessment of TRG (tumor regression grade) and CRM are imaging markers that predict survival outcomes for good and poor responders[47]. Practically it translates in to following.
Good tumor no adjuvant therapy: The preoperative identification of good prognosis tumors using MRI allows stratification of patients and targeting of preoperative therapy. MRI can also identify T3 rectal cancer patients who are likely to have a good outcome with primary surgery alone[34].
Poor prognostic tumors may benefit from: (1) preoperative extrastaging: Adverse features found on rectal MRI identify patients at increased risk of synchronous metastatic disease. Hunter et al[48] evaluated the incidence of synchronous metastatic disease on FDG-PET/CT and contrast-enhanced multiple-row detector computed tomography in MRI-stratified high- and low-risk rectal cancers. Incidence of confirmed distant metastases was significantly greater in the MRI high-risk group, with 20.7% vs the low-risk group, with 4.2% (odds ratio 6.0). This group may benefit from additional preoperative investigation for synchronous metastases such as FDG-PET/CT or liver MRI; and (2) trials involving Novel therapies such as Neoadjuvant capecitabine and oxaliplatin followed by synchronous chemoradiation and total mesorectal excision in magnetic resonance imaging-defined poor-risk rectal cancer[49].
MRI variation in countries
While there is good evidence supporting the role of MRI in rectal cancer, resource limitations and lack of National guidelines mean many patients with rectal cancer are still operated upon without preoperative MRI leading to suboptimal results. In United Kingdom in 2005, less than 50% of the units studied were able to offer preoperative MRI to all of their rectal cancer cases[50]. This however has changed to near 84% in 2012[51]. In an international questionnaire regarding use of MRI in rectal cancer, only 35% respondents used MRI routinely[52]. In South Korea, rectal MRI has been used for local staging since 2005, now it is very popular (90%). Furthermore cost of MRI is covered with national insurance system. In our institution, usually MRI and trans rectal USG are performed together for all mid and low rectal cancer patients.
POST LCRT MRI
MRI in rectal cancer is sometimes performed after radiotherapy (MRI 2) to evaluate tumor response and to choose alternative forms of surgery (Figure 6). With regards to MRI 2, there are two schools of thought.
Figure 6.
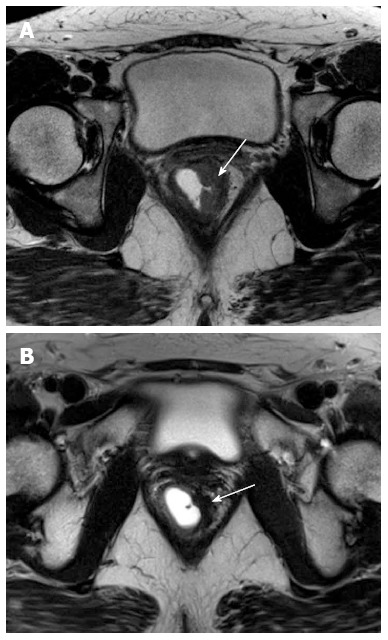
(A) Pre-chemoradiotherapy and (B) postchemoradiotherapy status. Arrows point to tumor along left lateral wall tumor which is mildly hyperintense in A that has become darkly hypointense in B indicating response (fibrosis).
MRI2 mandatory
MERCURY group believe MRI 2 should be mandatory for post treatment staging. This special radiology group felt with appropriate training, radiologists were able to differentiate tumor and fibrosis and even acellular mucin from cellular mucin on MRI scans. On post CRT T2 weighted images areas of fibrosis have very low signal intensity (similar to muscularis propria), whereas areas of residual tumor have intermediate signal intensity (similar to baseline tumor). Careful examination of high-resolution images enables delineation of small foci of intermediate signal intensity tumor in areas of low intensity fibrosis. Low intensity spicules in perirectal fat radiating from residual tumor represent desmoplastic reaction whereas advancing tumor has more nodular intermediate signal intensity. The guidelines for reporting MRI2 have been published by Patel et al[53], Table 4. MRI for restaging has established accuracy of involvement of intersphincteric plane[42,43,47]. Another argument on which MRI was based was that endoluminal USG cannot differentiate tumor and fibrosis[54,55]. In a study by this group, the negative predictive value of CRM for MRI 2 was 98%. In this study both posttreatment MRI T staging and posttreatment MRI assessment of tumor regression grade showed statistical correlation with pathologic T stage, which in turn was strongly associated with overall and disease-free survival as well as local recurrence[56].
Table 4.
Post long course chemoradiotherapy magnetic resonance imaging 2-Parameters are assessed on post treatment magnetic resonance images
| Pre treatment | Post treatment | |
| Height of tumor from anal verge | ||
| Length of tumor | ||
| Tumor stage (sub stage based on extramural spread) | ||
| Nodal spread | ||
| Nodes pelvic sidewall | ||
| Involvement peritoneal reflection | ||
| Distance to potential CRM | ||
| Depth of maximum extramural spread (distance from outer edge of muscularis propria) tumor and fibrosis separately | ||
| Extramural venous invasion |
MRI tumor regression grade, Grade V: No response (same as original tumor); Grade IV: Slight response (litte area of fibrosis/mucin, mostly tumor); Grade III: Moderate response (more than 50% fibrosis, mucin but mostly tumor); Grade II: Good response (dense fibrosis, no obvious residual tumor); Grade I: Radiological complete response (no evidence of ever treated tumor); CRM: Circumferential resection margin.
As a consequence, reassessment of MRI scans after preoperative therapy has implications for surgical planning, the timing of surgery, sphincter preservation[53,56]. Patients with CRM positivity on MRI 2 may require excision of adjacent organs (exenteration). While it has been suggested development of further preoperative treatments for radiologically identified poor responders and deferral of surgery for good responders, this can happen only in context of a trial. Phase II trials are currently evaluating the safety of deferring surgical resection in patients with a good response as shown on MRI[57]. However there are drawbacks, while MRI 2 has an negative predictive value of 98% for CRM, its specificity for CRM was 73% (compared to 92% for MRI 1)[8]. This would mean, excision performed based on MRI2, chances of involved margin would be less, but at the same time, you would be likely to overtreat and excise outside TME plane/exenteration. Sphincter preservation (ISR) would also be less likely.
MRI2 optional/unnecessary
MRI accuracy is poor after LCRT, T stage (43%), N stage (71%), On MRI it is difficult to differentiate tumor cells in scar tissue[58]. In a recent multicentric evaluation of MRI post neoadjuvant chemoradiotherapy (MERRION) found limited use of MRI post therapy[59]. In a small series of 16 patients with locally advanced cancer MRI before and after LCRT (MRI 1 and MRI 2) were compared to final histology. The accuracies of both MRI before and after radiotherapy were moderate, with no additional value of MRI after radiotherapy. They concluded that morphological assessment of pelvic MRI after preoperative radiotherapy does not provide any significant new information about tumor extent in patients with locally advanced rectal cancer[60]. Similarly, in another study, authors felt that accuracy of MRI 2 in distinguishing tumor delineation might be difficult due to fibrosis[61]. Post treatment MRI is a poor predictor of final histology and should not be relied upon to guide the extent of surgical resection. Larsen et al[62] felt that to achieve R0 resection, optimal surgery should be based on pre-treatment MRI. The study has initiated a new approach to histopathological classification of the removed specimen where they introduce a MRI assisted technique for investigating the areas at risk outside the mesorectal fascia in the specimen[62]. Kang et al[63] concluded that the tumor volume reduction ratio was not significantly associated with T and N downstaging. MRI is unable to detect the majority of patients who have a complete histopathological response as MRI appearances of ypT0 tumours are heterogeneous[64].
There is little consensus on the use of MRI after LCRT. Martellucci et al[65] suggested against restaging with MRI and recommended TRUS. They found that regarding the depth of invasion after treatment, TRUS agreed with histopathology in 25/37 patients (67.5%), CT agreed in 22/37 cases (59.5%), and MRI in 12/20 cases (60%). They therefore suggested limiting the use of MRI for restaging to selected cases. There however is uniform consensus on current guidelines, which advocate removing areas of fibrosis on MRI 2, as they could harbor tumor cells.
Even in United Kingdom, ACPGBI guidelines do not enforce MRI 2[8] prior to surgery. Ultimately it would be a joint decision by individual MDT as there seems to be no uniform consensus across the board. In low resource economies MRI 2 may be performed only in selected cases for locally advanced unresectable cases to plan operability, extent of resection or consideration of more non-cross resistant chemotherapy prior to surgery.
Timing of MRI 2: There remains some controversy regarding the optimum time for imaging prior to surgery after the chemoradiotherapy treatment has been completed. As surgery is planned for approximately 6-8 wk after the final chemoradiotherapy treatment, the MRI needs to be performed during this time, too early and the oncologists will argue that the chemoradiotherapy will still be having effects and potentially decrease the tumour size further; therefore the closer to surgery the better. Many centres aim for approximately 1 mo after LCRT to enable the surgery to be planned/organised.
MRI for surveillance
Surgical treatment offers the best prospect of survival for patients with recurrent colorectal cancer. Unfortunately, most local recurrences are diagnosed at an advanced (unresectable) stage, when traditional follow-up methods are used. The impact of MRI surveillance on the early diagnosis of local recurrences has been evaluated by Titu et al[66] In this unique study, 226 patients who underwent curative surgery for rectal and left-sided colon tumors were included in a program of surveillance using pelvic MRI in addition to standard follow-up protocol. Twenty-six (13%) local recurrences were identified. These were then analyzed based on mode of diagnosis, resectability, and overall survival. Recurrent pelvic cancer was diagnosed by MRI with a 87% sensitivity and 86% specificity. In 19 (63%) cases, CEA was abnormally elevated, and 9 patients (30%) were symptomatic. Surgical resection was possible in only 6 patients (20%). There was no difference between MRI and conventional follow-up tests in their ability to detect cases suitable for surgery. Hence they concluded, pelvic surveillance by MRI is not justified as part of the routine follow-up after a curative resection for colorectal cancer and should be reserved for selectively imaging patients with clinical, colonoscopic, and/or biochemical suspicion of recurrent disease[66].
Functional outcome: MRI pelvis may predict functional outcome in patients undergoing anterior resection. In a small series of patients undergoing anterior resection, How et al[67] evaluated functional outcome and co-related it with preoperative MRI sphincter morphology and anal manometry. They found only puborectalis thickness showed a significant (P = 0.01) relationship with the number of adverse symptoms suffered postoperatively[67].
MRI in recurrent cancers
MRI scans of pelvis are mandatory for selection for exenterative surgeryfor recurrent cancers, as CRM co-relates with survival. In primary cancers, assessing the preservation of fat plane can be used to predict invasion. However this is difficult in post-operative/post-radiotherapy pelvis, where fat planes are often grossly distorted or absent. Pelvic oncology unit in Leeds consider definite invasion in three specific circumstances on MRI: (1) when tumour tissue is clearly seen to invade or destroy adjacent anatomy; (2) when signal change in adjacent tissue is comparable with the signal intensity of the recurrent tumour; or (3) where muscle enlargement is evident. In their experience when patients are assessed between 21 and 48 mo post-primary surgery, muscle enlargement seen on MRI is related to recurrence rather than haematoma/inflammatory changes[68].
MRI directed MDT: MRI directed MDT improves outcome and is mandatory for recognition as a cancer centre. In 2006, Burton et al[69] compared CRM involvement of rectal cancer patients who were operated with/without MDT discussion and found low CRM involvement in patients discussed at MDT. This opinion however is not uniform. Review By Danish MDT team found increased detection of metachronous cancers through MDT but no difference in overall survival. Similar results were shown by Department of Health care policy, Harvard Medical school[70,71].
CLINICAL APPLICATION OF MRI FOR THE SURGEON
T1/T2 cancer. MRI can’t differentiate, hence need endorectal usg to identify T1 cancers. Theses may be candidates for local excision (transanal or TEO) (Figure 4).
T3 minimal (no CRM involvement) can go for surgery either per primum or after shortcourse radiotherapy (Figure 2).
T3/N0, + (Figures 3, 7 and 8) with circumferential margin involvement and T4 tumors (Figure 9) are treated with LCRT and reassesses with MRI 2.
Figure 9.

T4 lesion rectum involving prostate.
All rectal cancer with pelvic side wall nodes needs to undergo LCRT as this leads to improved survival and avoids need for lateral pelvic node dissection (Figure 8).
Figure 8.
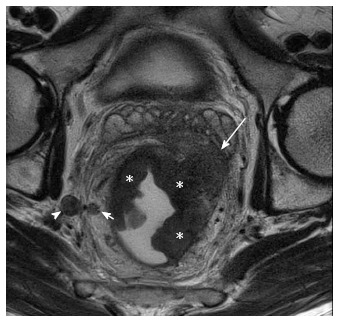
T3 tumor with lateral pelvic nodes. Axial T2W magnetic resonance imaging shows a large right lateral pelvic wall node (arrowhead). Short arrow shows perirectal node. The primary rectal tumor (asterisk) is seen extending into left mesorectal fat upto the mesorectal fascia (long arrow).
All low rectal cancers (5 cm from anal verge) are assesses with coronal images of MRI T2 sequences, to see involvement of intersphincteric plane and extension to levator ani: (1) those tumors free from intersphincteric plane and more than 1 mm from levator plate can be subjected to intersphincteric dissection and sphincter saving procedures (Figure 10A); (2) tumors involving intersphincteric space and external sphincters undergo standard APER (Figure 10B); and (3) tumors involving levators need extralevator APER (Figure 11).
Figure 10.
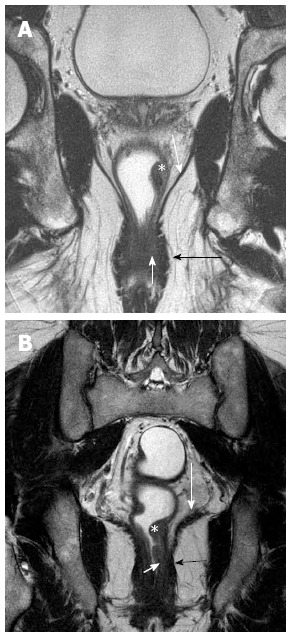
Coronal section T2 weighted magnetic resonance imaging to see level of tumor for planning surgery. A and B show tumor (asterisk) along the left lateral wall, that reaches up to the internal sphincter (short white arrows) in B, but spares it in A. The uninvolved external sphincter (darkly hypointense) is shown by black arrows. The long white arrows in A and B shows the spared levator ani.
Figure 11.
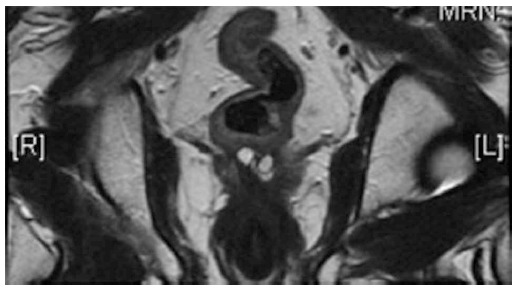
Low rectal cancer involving left levator.
DISCUSSION
One of the most important factors that governs the success of TME surgery is the relationship of tumour to the CRM. Tumour involvement of the CRM in patients undergoing TME surgery is related to poor survival and local recurrence. Tumor relation to CRM on MRI (predicted CRM) helps in planning preoperative LCRT in selected cases. MRI may help plan plane of resection for low rectal tumors and may decreases CRM involvement and ultimate outcome (LOREC project).
While not in line with NCCN (National comprehensive cancer Network) guidelines, it helps avoid radiotherapy for T3 patients where predicted CRM is not threatened. This will mitigate radiotherapy related complications and improve bowel function. In addition, MRI will identify tumours exhibiting other poor prognostic features, namely, extramural spread > 5 mm, extramural venous invasion by tumour, nodal involvement, and peritoneal infiltration who may be candidates for trials regarding intensive chemotherapy/biological therapy along with radiotherapy to improve DFS/OS/LR.
For advanced tumors (Non-resectable) on MRI, targeted preoperative therapy may not only reduce the size of the primary tumour and render potentially unresectable tumour resectable. This would also enable patients at high risk of systemic failure to benefit from intensive combined modality therapy aimed at eliminating micrometastatic disease[72]. The Role of MRI post LCRT is uncertain but is often used in selected centres planning to offer sphincter preservation based on tumor response.
CONCLUSION
MRI should be mandatory in planning radical surgery for rectal cancer. This improve R0 resection rates, decreases local recurrences with improved oncological outcomes. There is uncertainty over the role of MRI post LCRT. While MRI directed MDT has shown improved outcome in most studies, this however is debatable. The role of MRI in early rectal cancer seems to be limited, and needs complimentary endorectal ultrasound.
Footnotes
P- Reviewers: Carboni F, Razek A, Roldan-Valadez E S- Editor: Cui XM L- Editor: A E- Editor: Zhang DN
References
- 1.Kapiteijn E, Putter H, van de Velde CJ. Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg. 2002;89:1142–1149. doi: 10.1046/j.1365-2168.2002.02196.x. [DOI] [PubMed] [Google Scholar]
- 2.Martling A, Holm T, Rutqvist LE, Johansson H, Moran BJ, Heald RJ, Cedermark B. Impact of a surgical training programme on rectal cancer outcomes in Stockholm. Br J Surg. 2005;92:225–229. doi: 10.1002/bjs.4834. [DOI] [PubMed] [Google Scholar]
- 3.Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:1731–1740. doi: 10.1056/NEJMoa040694. [DOI] [PubMed] [Google Scholar]
- 4.Brown G. Staging rectal cancer: endoscopic ultrasound and pelvic MRI. Cancer Imaging. 2008;8 Spec No A:S43–S45. doi: 10.1102/1470-7330.2008.9008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blomqvist L, Rubio C, Holm T, Machado M, Hindmarsh T. Rectal adenocarcinoma: assessment of tumour involvement of the lateral resection margin by MRI of resected specimen. Br J Radiol. 1999;72:18–23. doi: 10.1259/bjr.72.853.10341684. [DOI] [PubMed] [Google Scholar]
- 6.Brown G, Richards CJ, Newcombe RG, Dallimore NS, Radcliffe AG, Carey DP, Bourne MW, Williams GT. Rectal carcinoma: thin-section MR imaging for staging in 28 patients. Radiology. 1999;211:215–222. doi: 10.1148/radiology.211.1.r99ap35215. [DOI] [PubMed] [Google Scholar]
- 7.Brown G, Kirkham A, Williams GT, Bourne M, Radcliffe AG, Sayman J, Newell R, Sinnatamby C, Heald RJ. High-resolution MRI of the anatomy important in total mesorectal excision of the rectum. AJR Am J Roentgenol. 2004;182:431–439. doi: 10.2214/ajr.182.2.1820431. [DOI] [PubMed] [Google Scholar]
- 8.MERCURY Study Group. Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ. 2006;333:779. doi: 10.1136/bmj.38937.646400.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MERCURY Study Group. Extramural depth of tumor invasion at thin-section MR in patients with rectal cancer: results of the MERCURY study. Radiology. 2007;243:132–139. doi: 10.1148/radiol.2431051825. [DOI] [PubMed] [Google Scholar]
- 10. Available from: http://www.lorec.nhs.uk/system/content.
- 11.Lim JS, Kim D, Baek SE, Myoung S, Choi J, Shin SJ, Kim MJ, Kim NK, Suh J, Kim KW, et al. Perfusion MRI for the prediction of treatment response after preoperative chemoradiotherapy in locally advanced rectal cancer. Eur Radiol. 2012;22:1693–1700. doi: 10.1007/s00330-012-2416-3. [DOI] [PubMed] [Google Scholar]
- 12.Lambrecht M, Vandecaveye V, De Keyzer F, Roels S, Penninckx F, Van Cutsem E, Filip C, Haustermans K. Value of diffusion-weighted magnetic resonance imaging for prediction and early assessment of response to neoadjuvant radiochemotherapy in rectal cancer: preliminary results. Int J Radiat Oncol Biol Phys. 2012;82:863–870. doi: 10.1016/j.ijrobp.2010.12.063. [DOI] [PubMed] [Google Scholar]
- 13.Song I, Kim SH, Lee SJ, Choi JY, Kim MJ, Rhim H. Value of diffusion-weighted imaging in the detection of viable tumour after neoadjuvant chemoradiation therapy in patients with locally advanced rectal cancer: comparison with T2 weighted and PET/CT imaging. Br J Radiol. 2012;85:577–586. doi: 10.1259/bjr/68424021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koh DM, Brown G, Temple L, Raja A, Toomey P, Bett N, Norman AR, Husband JE. Rectal cancer: mesorectal lymph nodes at MR imaging with USPIO versus histopathologic findings--initial observations. Radiology. 2004;231:91–99. doi: 10.1148/radiol.2311030142. [DOI] [PubMed] [Google Scholar]
- 15.Koh DM, George C, Temple L, Collins DJ, Toomey P, Raja A, Bett N, Farhat S, Husband JE, Brown G. Diagnostic accuracy of nodal enhancement pattern of rectal cancer at MRI enhanced with ultrasmall superparamagnetic iron oxide: findings in pathologically matched mesorectal lymph nodes. AJR Am J Roentgenol. 2010;194:W505–W513. doi: 10.2214/AJR.08.1819. [DOI] [PubMed] [Google Scholar]
- 16.Engelen SM, Beets-Tan RG, Lahaye MJ, Lammering G, Jansen RL, van Dam RM, Konsten J, Leijtens JW, van de Velde CJ, Beets GL. MRI after chemoradiotherapy of rectal cancer: a useful tool to select patients for local excision. Dis Colon Rectum. 2010;53:979–986. doi: 10.1007/DCR.0b013e3181dc64dc. [DOI] [PubMed] [Google Scholar]
- 17.Taylor FG, Swift RI, Blomqvist L, Brown G. A systematic approach to the interpretation of preoperative staging MRI for rectal cancer. AJR Am J Roentgenol. 2008;191:1827–1835. doi: 10.2214/AJR.08.1004. [DOI] [PubMed] [Google Scholar]
- 18.Kim MJ, Lim JS, Oh YT, Kim JH, Chung JJ, Joo SH, Kim NK, Lee KY, Kim WH, Kim KW. Preoperative MRI of rectal cancer with and without rectal water filling: an intraindividual comparison. AJR Am J Roentgenol. 2004;182:1469–1476. doi: 10.2214/ajr.182.6.1821469. [DOI] [PubMed] [Google Scholar]
- 19.Taylor F, Mangat N, Swift IR, Brown G. Proforma-based reporting in rectal cancer. Cancer Imaging. 2010;10 Spec no A:S142–S150. doi: 10.1102/1470-7330.2010.9092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown G, Daniels IR, Richardson C, Revell P, Peppercorn D, Bourne M. Techniques and trouble-shooting in high spatial resolution thin slice MRI for rectal cancer. Br J Radiol. 2005;78:245–251. doi: 10.1259/bjr/33540239. [DOI] [PubMed] [Google Scholar]
- 21.Kim JY, Kim YW, Kim NK, Hur H, Lee K, Min BS, Cho HJ. Pelvic anatomy as a factor in laparoscopic rectal surgery: a prospective study. Surg Laparosc Endosc Percutan Tech. 2011;21:334–339. doi: 10.1097/SLE.0b013e31822b0dcb. [DOI] [PubMed] [Google Scholar]
- 22.Salerno G, Daniels IR, Brown G, Norman AR, Moran BJ, Heald RJ. Variations in pelvic dimensions do not predict the risk of circumferential resection margin (CRM) involvement in rectal cancer. World J Surg. 2007;31:1313–1320. doi: 10.1007/s00268-007-9007-5. [DOI] [PubMed] [Google Scholar]
- 23.Baatrup G, Bolstad M, Mortensen JH. Rigid sigmoidoscopy and MRI are not interchangeable in determining the position of rectal cancers. Eur J Surg Oncol. 2009;35:1169–1173. doi: 10.1016/j.ejso.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 24.Hussain SM, Outwater EK, Siegelman ES. Mucinous versus nonmucinous rectal carcinomas: differentiation with MR imaging. Radiology. 1999;213:79–85. doi: 10.1148/radiology.213.1.r99se3879. [DOI] [PubMed] [Google Scholar]
- 25.Allen SD, Padhani AR, Dzik-Jurasz AS, Glynne-Jones R. Rectal carcinoma: MRI with histologic correlation before and after chemoradiation therapy. AJR Am J Roentgenol. 2007;188:442–451. doi: 10.2214/AJR.05.1967. [DOI] [PubMed] [Google Scholar]
- 26.Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J. Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging--a meta-analysis. Radiology. 2004;232:773–783. doi: 10.1148/radiol.2323031368. [DOI] [PubMed] [Google Scholar]
- 27.Al-Sukhni E, Milot L, Fruitman M, Beyene J, Victor JC, Schmocker S, Brown G, McLeod R, Kennedy E. Diagnostic accuracy of MRI for assessment of T category, lymph node metastases, and circumferential resection margin involvement in patients with rectal cancer: a systematic review and meta-analysis. Ann Surg Oncol. 2012;19:2212–2223. doi: 10.1245/s10434-011-2210-5. [DOI] [PubMed] [Google Scholar]
- 28.Beets-Tan RG, Beets GL, Vliegen RF, Kessels AG, Van Boven H, De Bruine A, von Meyenfeldt MF, Baeten CG, van Engelshoven JM. Accuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgery. Lancet. 2001;357:497–504. doi: 10.1016/s0140-6736(00)04040-x. [DOI] [PubMed] [Google Scholar]
- 29.Merkel S, Mansmann U, Siassi M, Papadopoulos T, Hohenberger W, Hermanek P. The prognostic inhomogeneity in pT3 rectal carcinomas. Int J Colorectal Dis. 2001;16:298–304. doi: 10.1007/s003840100309. [DOI] [PubMed] [Google Scholar]
- 30.Pedersen BG, Moran B, Brown G, Blomqvist L, Fenger-Grøn M, Laurberg S. Reproducibility of depth of extramural tumor spread and distance to circumferential resection margin at rectal MRI: enhancement of clinical guidelines for neoadjuvant therapy. AJR Am J Roentgenol. 2011;197:1360–1366. doi: 10.2214/AJR.11.6508. [DOI] [PubMed] [Google Scholar]
- 31.Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG, Dallimore NS, Williams GT. Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology. 2003;227:371–377. doi: 10.1148/radiol.2272011747. [DOI] [PubMed] [Google Scholar]
- 32.Kim JH, Beets GL, Kim MJ, Kessels AG, Beets-Tan RG. High-resolution MR imaging for nodal staging in rectal cancer: are there any criteria in addition to the size. Eur J Radiol. 2004;52:78–83. doi: 10.1016/j.ejrad.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 33.Kim DJ, Kim JH, Ryu YH, Jeon TJ, Yu JS, Chung JJ. Nodal staging of rectal cancer: high-resolution pelvic MRI versus ¹⁸F-FDGPET/CT. J Comput Assist Tomogr. 2011;35:531–534. doi: 10.1097/RCT.0b013e318225720f. [DOI] [PubMed] [Google Scholar]
- 34.Taylor FG, Quirke P, Heald RJ, Moran B, Blomqvist L, Swift I, Sebag-Montefiore DJ, Tekkis P, Brown G; the MERCURY study group. Preoperative High-resolution Magnetic Resonance Imaging Can Identify Good Prognosis Stage I, II, and III Rectal Cancer Best Managed by Surgery Alone: A Prospective, Multicenter, European Study That Recruited Consecutive Patients With Rectal Cancer. Ann Surg. 2011;253:711–719. doi: 10.1097/SLA.0b013e31820b8d52. [DOI] [PubMed] [Google Scholar]
- 35.Kim YW, Cha SW, Pyo J, Kim NK, Min BS, Kim MJ, Kim H. Factors related to preoperative assessment of the circumferential resection margin and the extent of mesorectal invasion by magnetic resonance imaging in rectal cancer: a prospective comparison study. World J Surg. 2009;33:1952–1960. doi: 10.1007/s00268-009-0126-z. [DOI] [PubMed] [Google Scholar]
- 36.Peschaud F, Cuenod CA, Benoist S, Julié C, Beauchet A, Siauve N, Taieb-Kasbi F, Penna C, Nordlinger B. Accuracy of magnetic resonance imaging in rectal cancer depends on location of the tumor. Dis Colon Rectum. 2005;48:1603–1609. doi: 10.1007/s10350-005-0051-7. [DOI] [PubMed] [Google Scholar]
- 37.Smith NJ, Barbachano Y, Norman AR, Swift RI, Abulafi AM, Brown G. Prognostic significance of magnetic resonance imaging-detected extramural vascular invasion in rectal cancer. Br J Surg. 2008;95:229–236. doi: 10.1002/bjs.5917. [DOI] [PubMed] [Google Scholar]
- 38.Shihab OC, Taylor F, Bees N, Blake H, Jeyadevan N, Bleehen R, Blomqvist L, Creagh M, George C, Guthrie A, et al. Relevance of magnetic resonance imaging-detected pelvic sidewall lymph node involvement in rectal cancer. Br J Surg. 2011;98:1798–1804. doi: 10.1002/bjs.7662. [DOI] [PubMed] [Google Scholar]
- 39.Park JA, Choi GS, Park JS, Park SY. Initial clinical experience with robotic lateral pelvic lymph node dissection for advanced rectal cancer. J Korean Soc Coloproctol. 2012;28:265–270. doi: 10.3393/jksc.2012.28.5.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burton S, Brown G, Daniels I, Norman A, Swift I, Abulafi M, Wotherspoon A, Tait D. MRI identified prognostic features of tumors in distal sigmoid, rectosigmoid, and upper rectum: treatment with radiotherapy and chemotherapy. Int J Radiat Oncol Biol Phys. 2006;65:445–451. doi: 10.1016/j.ijrobp.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 41.Shihab OC, Moran BJ, Heald RJ, Quirke P, Brown G. MRI staging of low rectal cancer. Eur Radiol. 2009;19:643–650. doi: 10.1007/s00330-008-1184-6. [DOI] [PubMed] [Google Scholar]
- 42.Shihab OC, How P, West N, George C, Patel U, Quirke P, Heald RJ, Moran BJ, Brown G. Can a novel MRI staging system for low rectal cancer aid surgical planning. Dis Colon Rectum. 2011;54:1260–1264. doi: 10.1097/DCR.0b013e31822abd78. [DOI] [PubMed] [Google Scholar]
- 43.Salerno GV, Daniels IR, Moran BJ, Heald RJ, Thomas K, Brown G. Magnetic resonance imaging prediction of an involved surgical resection margin in low rectal cancer. Dis Colon Rectum. 2009;52:632–639. doi: 10.1007/DCR.0b013e3181a0a37e. [DOI] [PubMed] [Google Scholar]
- 44.O’Neill BD, Salerno G, Thomas K, Tait DM, Brown G. MR vs CT imaging: low rectal cancer tumour delineation for three-dimensional conformal radiotherapy. Br J Radiol. 2009;82:509–513. doi: 10.1259/bjr/60198873. [DOI] [PubMed] [Google Scholar]
- 45.Gwynne S, Mukherjee S, Webster R, Spezi E, Staffurth J, Coles B, Adams R. Imaging for target volume delineation in rectal cancer radiotherapy--a systematic review. Clin Oncol (R Coll Radiol. ) 2012;24:52–63. doi: 10.1016/j.clon.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 46.Chen L, Price RA, Nguyen TB, Wang L, Li JS, Qin L, Ding M, Palacio E, Ma CM, Pollack A. Dosimetric evaluation of MRI-based treatment planning for prostate cancer. Phys Med Biol. 2004;49:5157–5170. doi: 10.1088/0031-9155/49/22/010. [DOI] [PubMed] [Google Scholar]
- 47.Shihab OC, Taylor F, Salerno G, Heald RJ, Quirke P, Moran BJ, Brown G. MRI predictive factors for long-term outcomes of low rectal tumours. Ann Surg Oncol. 2011;18:3278–3284. doi: 10.1245/s10434-011-1776-2. [DOI] [PubMed] [Google Scholar]
- 48.Hunter CJ, Garant A, Vuong T, Artho G, Lisbona R, Tekkis P, Abulafi M, Brown G. Adverse features on rectal MRI identify a high-risk group that may benefit from more intensive preoperative staging and treatment. Ann Surg Oncol. 2012;19:1199–1205. doi: 10.1245/s10434-011-2036-1. [DOI] [PubMed] [Google Scholar]
- 49.Chau I, Brown G, Cunningham D, Tait D, Wotherspoon A, Norman AR, Tebbutt N, Hill M, Ross PJ, Massey A, et al. Neoadjuvant capecitabine and oxaliplatin followed by synchronous chemoradiation and total mesorectal excision in magnetic resonance imaging-defined poor-risk rectal cancer. J Clin Oncol. 2006;24:668–674. doi: 10.1200/JCO.2005.04.4875. [DOI] [PubMed] [Google Scholar]
- 50.Taylor A, Sheridan M, McGee S, Halligan S. Preoperative staging of rectal cancer by MRI; results of a UK survey. Clin Radiol. 2005;60:579–586. doi: 10.1016/j.crad.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 51.Finan P SJ, Greenaway K. National Bowel Cancer Audit - England, Wales, 2012: Report. Available from: http: //catalogue.ic.nhs.uk/publications/clinical/bowel/nati-clin-audi-supp-prog-bowe-canc-2012/nati-clin-audi-supp-prog-bowe-canc-2012-rep.pdfDec 2012.
- 52.Augestad KM, Lindsetmo RO, Stulberg J, Reynolds H, Senagore A, Champagne B, Heriot AG, Leblanc F, Delaney CP. International preoperative rectal cancer management: staging, neoadjuvant treatment, and impact of multidisciplinary teams. World J Surg. 2010;34:2689–2700. doi: 10.1007/s00268-010-0738-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Patel UB, Blomqvist LK, Taylor F, George C, Guthrie A, Bees N, Brown G. MRI after treatment of locally advanced rectal cancer: how to report tumor response--the MERCURY experience. AJR Am J Roentgenol. 2012;199:W486–W495. doi: 10.2214/AJR.11.8210. [DOI] [PubMed] [Google Scholar]
- 54.Rau B, Hünerbein M, Barth C, Wust P, Haensch W, Riess H, Felix R, Schlag PM. Accuracy of endorectal ultrasound after preoperative radiochemotherapy in locally advanced rectal cancer. Surg Endosc. 1999;13:980–984. doi: 10.1007/s004649901151. [DOI] [PubMed] [Google Scholar]
- 55.Marone P, de Bellis M, Avallone A, Delrio P, di Nardo G, D’Angelo V, Tatangelo F, Pecori B, Di Girolamo E, Iaffaioli V, et al. Accuracy of endoscopic ultrasound in staging and restaging patients with locally advanced rectal cancer undergoing neoadjuvant chemoradiation. Clin Res Hepatol Gastroenterol. 2011;35:666–670. doi: 10.1016/j.clinre.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 56.Patel UB, Taylor F, Blomqvist L, George C, Evans H, Tekkis P, Quirke P, Sebag-Montefiore D, Moran B, Heald R, et al. Magnetic resonance imaging-detected tumor response for locally advanced rectal cancer predicts survival outcomes: MERCURY experience. J Clin Oncol. 2011;29:3753–3760. doi: 10.1200/JCO.2011.34.9068. [DOI] [PubMed] [Google Scholar]
- 57.SK Yu GB, Heald RJ. Deferral of rectal surgery following a continued response to preoperative chemoradiotherapy (watch and wait) study: a phase II multicenter study in the United Kingdom. J Clin Oncol. 2011;29(suppl 4):Abstract 489. [Google Scholar]
- 58.Suppiah A, Hunter IA, Cowley J, Garimella V, Cast J, Hartley JE, Monson JR. Magnetic resonance imaging accuracy in assessing tumour down-staging following chemoradiation in rectal cancer. Colorectal Dis. 2009;11:249–253. doi: 10.1111/j.1463-1318.2008.01593.x. [DOI] [PubMed] [Google Scholar]
- 59.Hanly AM, Ryan EM, Rogers AC, McNamara DA, Madoff RD, Winter DC; on behalf of the MERRION Study Group. Multicenter Evaluation of Rectal cancer ReImaging pOst Neoadjuvant (MERRION) Therapy. Ann Surg. 2013:Epub ahead of print. doi: 10.1097/SLA.0b013e31828f6c91. [DOI] [PubMed] [Google Scholar]
- 60.Torkzad MR, Suzuki C, Tanaka S, Palmer G, Holm T, Blomqvist L. Morphological assessment of the interface between tumor and neighboring tissues, by magnetic resonance imaging, before and after radiotherapy in patients with locally advanced rectal cancer. Acta Radiol. 2008;49:1099–1103. doi: 10.1080/02841850802477916. [DOI] [PubMed] [Google Scholar]
- 61.Del Vescovo R, Trodella LE, Sansoni I, Cazzato RL, Battisti S, Giurazza F, Ramella S, Cellini F, Grasso RF, Trodella L, et al. MR imaging of rectal cancer before and after chemoradiation therapy. Radiol Med. 2012;117:1125–1138. doi: 10.1007/s11547-012-0804-2. [DOI] [PubMed] [Google Scholar]
- 62.Larsen SG, Wiig JN, Emblemsvaag HL, Grøholt KK, Hole KH, Bentsen A, Dueland S, Vetrhus T, Giercksky KE. Extended total mesorectal excision in locally advanced rectal cancer (T4a) and the clinical role of MRI-evaluated neo-adjuvant downstaging. Colorectal Dis. 2009;11:759–767. doi: 10.1111/j.1463-1318.2008.01649.x. [DOI] [PubMed] [Google Scholar]
- 63.Kang JH, Kim YC, Kim H, Kim YW, Hur H, Kim JS, Min BS, Kim H, Lim JS, Seong J, et al. Tumor volume changes assessed by three-dimensional magnetic resonance volumetry in rectal cancer patients after preoperative chemoradiation: the impact of the volume reduction ratio on the prediction of pathologic complete response. Int J Radiat Oncol Biol Phys. 2010;76:1018–1025. doi: 10.1016/j.ijrobp.2009.03.066. [DOI] [PubMed] [Google Scholar]
- 64.Franklin JM, Anderson EM, Gleeson FV. MRI features of the complete histopathological response of locally advanced rectal cancer to neoadjuvant chemoradiotherapy. Clin Radiol. 2012;67:546–552. doi: 10.1016/j.crad.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 65.Martellucci J, Scheiterle M, Lorenzi B, Roviello F, Cetta F, Pinto E, Tanzini G. Accuracy of transrectal ultrasound after preoperative radiochemotherapy compared to computed tomography and magnetic resonance in locally advanced rectal cancer. Int J Colorectal Dis. 2012;27:967–973. doi: 10.1007/s00384-012-1419-5. [DOI] [PubMed] [Google Scholar]
- 66.Titu LV, Nicholson AA, Hartley JE, Breen DJ, Monson JR. Routine follow-up by magnetic resonance imaging does not improve detection of resectable local recurrences from colorectal cancer. Ann Surg. 2006;243:348–352. doi: 10.1097/01.sla.0000201454.20253.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.How P, Evans J, Moran B, Swift I, Brown G. Preoperative MRI sphincter morphology and anal manometry: can they be markers of functional outcome following anterior resection for rectal cancer. Colorectal Dis. 2012;14:e339–e345. doi: 10.1111/j.1463-1318.2012.02942.x. [DOI] [PubMed] [Google Scholar]
- 68.Messiou C, Chalmers A, Boyle K, Sagar P. Surgery for recurrent rectal carcinoma: The role of preoperative magnetic resonance imaging. Clin Radiol. 2006;61:250–258. doi: 10.1016/j.crad.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 69.Burton S, Brown G, Daniels IR, Norman AR, Mason B, Cunningham D. MRI directed multidisciplinary team preoperative treatment strategy: the way to eliminate positive circumferential margins. Br J Cancer. 2006;94:351–357. doi: 10.1038/sj.bjc.6602947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wille-Jørgensen P, Sparre P, Glenthøj A, Holck S, Nørgaard Petersen L, Harling H, Stub Højen H, Bülow S. Result of the implementation of multidisciplinary teams in rectal cancer. Colorectal Dis. 2013;15:410–413. doi: 10.1111/codi.12013. [DOI] [PubMed] [Google Scholar]
- 71.Keating NL, Landrum MB, Lamont EB, Bozeman SR, Shulman LN, McNeil BJ. Tumor boards and the quality of cancer care. J Natl Cancer Inst. 2013;105:113–121. doi: 10.1093/jnci/djs502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Brown G, Daniels IR. Preoperative staging of rectal cancer: the MERCURY research project. Recent Results Cancer Res. 2005;165:58–74. doi: 10.1007/3-540-27449-9_8. [DOI] [PubMed] [Google Scholar]


