Abstract
Background
The aim of this study was to assess national practice patterns regarding use of perioperative antibiotics by surgeons performing breast operations requiring drainage tubes.
Methods
The members of the American Society of Breast Surgeons (ASBrS) were surveyed regarding use of perioperative antibiotics for breast operations requiring drains, with or without immediate tissue expander or implant reconstruction.
Results
Of 2857 ASBrS members contacted, 917 (32%) responded and all self-identified as surgeons. Of 905 evaluable respondents, most described themselves as general surgeons (46%) or breast surgeons (46%). For cases in which drains are anticipated, most respondents (86%) reported routine use of preoperative prophylactic antibiotics, 99% selecting cephalosporins. Use of antibiotic >24 hours postoperatively varied by whether or not reconstruction was performed. In non-reconstruction cases, the majority (76%) reported “never/almost never” prescribing antibiotics beyond the 24 hour postoperative period, but 16% reported “always/almost always”. In reconstruction cases, the majority (58%) reported routine antibiotic use beyond 24 hours and the primary driver of the decision to use antibiotics was reported to be the plastic surgeon (83%). Among those reporting use >24 hours, the duration recommended for non-reconstruction cases was “up to one week” in 38% and “until drains removed” in 39%, and this was similar for reconstruction cases.
Conclusions
Cephalosporins are utilized uniformly as preoperative antibiotic prophylaxis in breast operations requiring drains. However, use of postoperative antibiotic prophylaxis is strongly dependent on the presence of immediate breast reconstruction. Consensus is lacking on the role of postoperative antibiotic prophylaxis in breast operations utilizing drains.
Introduction
Surgical site infections (SSI) after breast and axillary procedures are more common than expected for “clean” cases, with reported incidence of 1–26%.[1–6] Reasons for this are likely multifactorial, but both surgical drains and implant-based breast reconstruction are demonstrated risk factors.[7–9]
A recent study by Felippe et al. demonstrated that bacterial colonization of surgical drains used in breast and axillary procedures is a significant risk factor for the development of SSI; also, the microorganism(s) causing SSIs were the same as those colonizing the drainage tube in 83% of cases.[10] Drainage tubes are similarly implicated with SSI in the context of tissue expander or implant breast reconstruction, with a recent retrospective analysis by Lanier et al. showing an association between longer drain duration and increased incidence of SSI.[11]
In immediate tissue expander/implant reconstruction cases, infection can result in implant removal and failed reconstruction. Therefore, some surgeons prescribe postoperative prophylactic antibiotics in an attempt to reduce the risk of SSI despite 1) lack of evidence of efficacy of this approach and 2) the presence of national guidelines that call for discontinuation of antibiotics 24 hours after operation.[12] Currently, there is little published data regarding adherence to these national guidelines. The purpose of this study was to evaluate practice patterns of breast surgeons regarding the use of extended (>24 hours) postoperative prophylactic antibiotics after breast operations utilizing drainage tubes for cases with and without immediate reconstruction.
Methods
Approval from the Mayo Clinic Institutional Review Board was obtained. Survey content and distribution methods were approved by the American Society of Breast Surgeons’ (ASBrS) Research Committee and Board of Directors. Members of the ASBrS were initially contacted by the Mayo Clinic Survey Research Center (SRC) in July 2011 via email addresses obtained from the ASBrS 2011 directory. To encourage responses, the questionnaire was accompanied by a short letter of appeal. A reminder email was sent after one month, and the survey was closed two months after initial contact. Study data were collected by the Survey Research Center via SurveyTracker, deidentified, and exported for statistical analysis.
The survey consisted of 14 multiple choice questions with space for free-text comments where appropriate. The questions were designed to inquire about practice and surgeon demographics, preoperative antibiotic use, and postoperative antibiotic use with and without immediate reconstruction. Professional role, years in practice, practice volume, volume of breast cases, and practice setting were collected. Respondents were also asked about the use of surgical drains in breast procedures and to characterize this frequency in their practice. Patterns of preoperative antibiotic use were characterized by frequency and type of antibiotic. Patterns of postoperative antibiotic use were characterized by frequency and duration in procedures with and without immediate reconstruction. Answers regarding frequency of use were represented on surveys as percentages accompanied by nominal descriptors as follows: “never/almost never” (0% to 10% of cases), “sometimes” (11% to 50%), “most of the time” (51% to 90%), or “always/almost always” (91% to 100% of cases). In the setting of immediate reconstruction, respondents were queried as to the primary driver of the decision to prescribe postoperative antibiotics, either breast/general surgeon, plastic surgeon, or both.
Descriptive statistics were reported as proportions of respondents. Comparisons were evaluated using Kruskall-Wallis and Wilcoxon signed-rank tests. A p-value < 0.05 was considered statistically significant, except for multiple comparisons in which a Bonferroni correction was used. All analyses were performed using PROC FREQ in SAS (Version 9, SAS Institute Inc., Cary, NC).
Results
Survey response
Surveys were initially sent to 2881 ASBrS members. A total of 2857 survey requests were delivered electronically, of which 917 completed surveys were returned, representing a response rate of 32%. Twelve respondents not in active clinical practice were excluded from further analysis.
Demographics
All 905 evaluable respondents described themselves as surgeons in active clinical practice in which they place drains in patients undergoing breast and axillary procedures. Most respondents (96%) reported placing drains in up to 4 patients in a typical week (Table 1). Most respondents described themselves as general surgeons (46%) or breast surgeons (46%). As expected in this sample of the ASBrS, a majority of respondents (56%) reported that breast operations comprised >60% of their surgical cases. Three (0.3%) self-described plastic surgeons completed the survey. A majority (67%) of respondents reported being in private practice, while 23% described their practice as academic or university-affiliated. Reported number of years in practice was 6–15 years for 34% and >15 years for 50% of respondents (Table 1).
Table 1.
Demographics
| Category | n | % |
|---|---|---|
| % breast practice | ||
| 1%–20% | 96 / 905 | 10.6 |
| 21%–40% | 174 / 905 | 19.2 |
| 41%–60% | 128 / 905 | 14.1 |
| 61%–80% | 84 / 905 | 9.3 |
| 81%–100% | 423 / 905 | 46.7 |
| Approximate # pts in whom drains are placed (per week) | ||
| 0–1 | 506 / 904 | 56.0 |
| 2–4 | 365 / 904 | 40.4 |
| 5–10 | 29 / 904 | 3.2 |
| >10 | 4 / 904 | 0.4 |
| Professional role | ||
| General Surgeon | 414 / 900 | 46.0 |
| Breast Surgeon | 412 / 900 | 45.8 |
| Surgical Oncologist | 66 / 900 | 7.3 |
| Fellow | 4 / 900 | 0.4 |
| Plastic Surgeon | 3 / 900 | 0.3 |
| Resident | 1 / 900 | 0.1 |
| Practice description | ||
| Community/Private | 516 / 904 | 57.1 |
| Academic/University-affiliated | 207 / 904 | 22.9 |
| Urban/Private | 92 / 904 | 10.2 |
| Group Practice | 43 / 904 | 4.8 |
| VA/Government/Military | 2 / 904 | 0.2 |
| Other | 44 / 904 | 4.9 |
| Years in practice | ||
| <1 | 11 / 904 | 1.2 |
| 1–2 | 36 / 904 | 4.0 |
| 3–5 | 99 / 904 | 11.0 |
| 6–10 | 156 / 904 | 17.3 |
| 11–15 | 150 / 904 | 16.6 |
| >15 | 452 / 904 | 50.0 |
Preoperative antibiotic prophylaxis
In procedures in which drain placement was anticipated, 86% of respondents reported that they “always/almost always” administer antibiotic prophylaxis prior to skin incision whereas 9% responded “never/almost never”. Ninety-nine percent of surgeons reported cephalosporins as their standard preoperative antibiotic.
Postoperative antibiotic prophylaxis
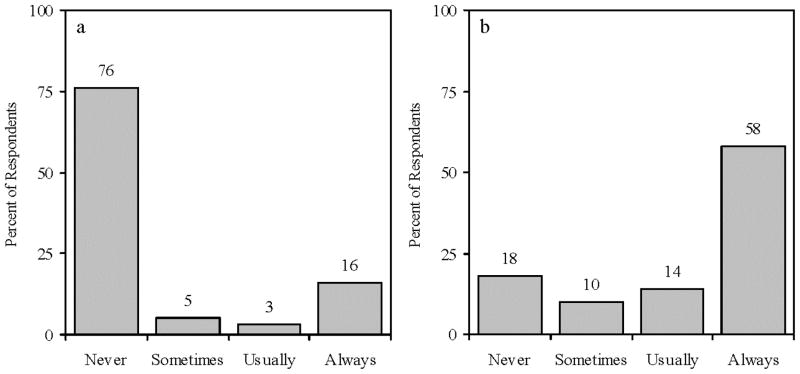
The data demonstrate a polarization of responses with regard to the use of postoperative antibiotic prophylaxis in both reconstruction and non-reconstruction cases. Overall, 92% of respondents reported adopting a routine practice of either using or not using antibiotics beyond 24 hours. In the absence of reconstruction, 76% of respondents reported that they “never/almost never” prescribe prophylactic antibiotics beyond the 24 hour postoperative period, and 16% responded that they prescribe antibiotics “always/almost always”. The intermediate responses of “sometimes” and “most of the time” were infrequently selected, 5% and 3% respectively. In reconstruction cases, responses were similarly polarized but in the opposite direction, with 18% of respondents indicating they “never/almost never” use prolonged antibiotic prophylaxis and 58% responding “always/almost always” (Figure 1).
Figure 1.
Responses regarding frequency of postoperative antibiotic prophylaxis beyond 24 h without (a) and with (b) reconstruction, expressed as percentage of respondents.
Some inconsistency was observed for postoperative antibiotic prophylaxis with and without reconstruction among subgroups of respondents. Of the 128 respondents (16%) who reported “always/almost always” using postoperative prophylactic antibiotics in non-reconstruction cases, only 80% reported “always/almost always” using them in reconstruction cases. Of the 614 respondents (76%) who reported “never/almost never” using antibiotic prophylaxis in non-reconstruction cases, the majority (53%) reported use “always/almost always” in reconstruction, with 22% “never/almost never”, 11% “sometimes”, and 14% “most of the time”.
This variability in postoperative antibiotic drain prophylaxis between reconstruction and non-reconstruction cases is corroborated by responses regarding the impact of the plastic surgeon in the decision for postoperative antibiotic prophylaxis, with 83% of respondents indicating that the primary driver of the decision to prescribe antibiotic prophylaxis is the plastic surgeon. Three percent responded that the breast/general surgeon is the primary driver, while 14% indicated that both teams equally support postoperative antibiotics.
Duration of postoperative antibiotic prophylaxis
Among respondents who reported postoperative prophylactic antibiotic use in either non-reconstruction or reconstruction cases, the duration of treatment was similar. In cases without reconstruction, respondents continued antibiotic prophylaxis for 2 to 7 days or until all drains were removed (38% and 39% respectively). In reconstruction cases, a similar distribution was observed, with 33% continuing prophylaxis for 2 to 7 days, and 33% until all drains were removed. However, 22% of respondents reported that the duration of prophylaxis in reconstruction cases varied according to the practice of the plastic surgeon.
Antibiotic prophylaxis by breast surgical case volume
The use of postoperative antibiotic prophylaxis beyond 24 hours in non-reconstruction cases was directly correlated with breast surgical case volume. Respondents with a higher self-reported proportion of practice devoted to breast operations were more likely to report “always/almost always” prescribing postoperative antibiotic prophylaxis in non-reconstruction cases. For example, among respondents with 81–100% of their practice devoted to breast surgery, 21% reported “always/almost always” prescribing postoperative antibiotic prophylaxis in the absence of reconstruction compared to 9% among respondents who devote 1–20% of their practice to breast surgery (p=0.001) (Table 2). However, the majority across all groups did not routinely prescribe postoperative antibiotic prophylaxis for non-reconstruction cases. This effect of breast surgical case volume impacting postoperative antibiotic prophylaxis was also seen in reconstruction cases (p=0.001). However, in the reconstructed cases, the majority of respondents across all breast surgical volumes did use routine postoperative antibiotic prophylaxis as shown in Table 2.
Table 2.
Responses by Practice and Surgeon Demographics
| Without Reconstruction | With Reconstruction | |||
|---|---|---|---|---|
|
| ||||
| Never/almost never (%) | Always/almost always (%) | Never/almost never (%) | Always/almost always (%) | |
| % breast practice | ||||
| 1%–20% | 91.2 | 8.8 | 53.7 | 46.3 |
| 21%–40% | 86.8 | 13.2 | 34.0 | 66.0 |
| 41%–60% | 84.0 | 16.0 | 31.4 | 68.6 |
| 61%–80% | 85.5 | 14.5 | 20.0 | 80.0 |
| 81%–100% | 78.7 | 21.3 | 15.0 | 85.0 |
| Approx. # pts in whom drains are placed (per wk) | ||||
| 0–1 | 85.1 | 15.0 | 31.2 | 68.8 |
| 2–4 | 79.8 | 20.2 | 17.7 | 82.3 |
| >5 | 87.5 | 12.5 | 3.7 | 96.3 |
| Professional role | ||||
| General Surgeon | 80.4 | 13.3 | 22.6 | 46.8 |
| Breast Surgeon | 71.6 | 17.7 | 10.4 | 66.7 |
| Surgical Oncologist | 77.3 | 18.2 | 31.3 | 56.3 |
| Plastic Surgeon | 100.0 | 0.0 | 0.0 | 100.0 |
| Practice description | ||||
| Community/Private | 78.3 | 15.5 | 20.1 | 56.0 |
| Urban/Private | 65.2 | 23.9 | 15.7 | 59.0 |
| Academic/University-affiliated | 74.4 | 12.6 | 16.2 | 60.6 |
| Group Practice | 81.4 | 14.0 | 13.2 | 57.9 |
| Other | 75.0 | 15.9 | 17.7 | 58.8 |
| Years in practice | ||||
| <1 | 77.8 | 22.2 | 10.0 | 90.0 |
| 1–2 | 82.9 | 18.1 | 14.8 | 85.2 |
| 3–5 | 80.7 | 19.3 | 13.1 | 86.9 |
| 6–10 | 81.3 | 18.7 | 20.8 | 79.2 |
| 11–15 | 84.9 | 15.1 | 22.7 | 77.3 |
| >15 | 83.5 | 16.5 | 29.3 | 70.7 |
Antibiotic prophylaxis by professional role and practice setting
The use of postoperative antibiotic prophylaxis correlated with self-described professional role but not with practice setting. In non-reconstruction cases, self-described breast surgeons were significantly more likely than self-described general surgeons to “always/almost always” prescribe postoperative antibiotic prophylaxis, (18% versus 13%, p=0.004). In reconstruction cases, a similar pattern of responses was observed with respect to professional role, with 67% of self-described breast surgeons reporting “always/almost always” prescribing antibiotic prophylaxis compared to 47% of self-described general surgeons (p<0.001). All 3 plastic surgeons reported “never/almost never” using antibiotic prophylaxis in non-reconstruction cases and “always/almost always” in reconstruction cases. Regarding practice setting, self-described academic surgeons and private-practice surgeons reported similar frequencies of postoperative antibiotic use in cases with and without reconstruction (Table 2).
Discussion
This survey of the American Society of Breast Surgeons demonstrates a lack of consensus in the use of postoperative antibiotic prophylaxis in breast and axillary procedures requiring drains, regardless of immediate breast reconstruction. Our survey was conducted among members of the ASBrS who perform a considerable volume of breast and axillary procedures in which drains are used (96% placing up to 4 drains per week), with respondents describing themselves as breast and general surgeons, most of whom have been in practice for greater than 10 years. The survey findings are relevant to current practice due to increasing national focus on healthcare outcomes such as SSI, with related attention to modifiable contributing factors. The Surgical Care Improvement Project (SCIP) undertaken in August 2005 by the federal government established guidelines for both preoperative and postoperative antibiotic prophylaxis.[13] In breast and axillary procedures, SCIP guidelines require administration of antibiotic (cephalosporins as first choice) prior to incision and antibiotic discontinuation 24 hours after procedure end. The guidelines do not address whether prophylaxis should vary in the context of surgical drains or immediate breast reconstruction.
With regard to SCIP guidelines for preoperative antibiotic prophylaxis, our survey demonstrates excellent surgeon support for both administration and choice of preoperative antibiotic. Conversely, despite SCIP guidelines requiring discontinuation of antibiotic prophylaxis at 24 hours, our survey indicates that routine prolonged antibiotic use is not rare in non-reconstruction cases with drains (16%). Furthermore, in the majority of cases with immediate reconstruction, routine prolonged antibiotic use is common (58%). We found that responses were polarized, with respondents infrequently choosing intermediate responses (“sometimes” or “most of the time”). This suggests that in the absence of clear evidence regarding postoperative antibiotic prophylaxis, most surgeons make a decision about best practice and follow that routine. However, inconsistencies remain. Although routine postoperative antibiotic use was reported by the majority for reconstruction cases and was significantly more frequent compared to non-reconstruction cases, this approach was reported by only 58%, clearly not a uniform national practice pattern.
This survey specifically focused on antibiotic use in breast and axillary procedures requiring drains because surgical drains have recently been linked to SSIs. [10, 14] Felippe et al. conducted a prospective cohort study of 354 women discharged with drains after breast cancer surgery. Sixty SSIs were documented and microbiology of drain colonization and SSIs were evaluated. Colonization rate was 81% by postoperative day 14, and 83% of culture positive SSIs grew the same microorganisms demonstrated in the colonized drain.[10] Retrospective analysis suggests that postoperative antibiotic prophylaxis does not appear to be the solution, although it is often employed.[14, 15] Throckmorton et al. retrospectively evaluated 277 patients in whom drains were placed after breast and axillary procedures, of which 158 received preoperative antibiotics only and 119 received both preoperative and postoperative antibiotic prophylaxis. The frequency of SSI was statistically similar between these two groups (9.5% versus 8.4%, p = 0.76), suggesting that prolonged postoperative antibiotics do not reduce SSI.[15]
Our survey results show much higher rates of prolonged antibiotic use in reconstruction cases. We speculate that this is related to the possibility of failed reconstruction in the event of infection. Indeed, published literature supports a higher incidence of SSI in tissue expander or implant reconstruction cases. The two year results of the Michigan Breast Reconstruction Outcome Study demonstrate that the incidence of infection among expander/implant reconstruction patients was greater than among patients who underwent TRAM flap reconstruction, 35.4% versus 11.7% or 17.9% respectively.[7] In another retrospective case-control study evaluating risk factors for SSI in patients undergoing breast surgery, Olsen et al. demonstrated that insertion of a tissue expander or implant was significantly associated with an increased frequency of SSI, with an odds ratio of 5.1.[9] Thus, it is likely that the increased infection rates associated with tissue expander or implant reconstruction and the possible consequence of failed reconstruction are the factors driving the increased use of postoperative prophylactic antibiotics, despite lack of proven efficacy.
Higher rates of prolonged antibiotic use in reconstruction among our respondents are corroborated by a recent survey of plastic surgeons.[16] Phillips et al. surveyed members of the American and Canadian Societies of Plastic Surgeons regarding drain use and perioperative antibiotic prophylaxis in cases of breast reconstruction.[16] Comparable to surgeons in our study, they found that 72% of plastic surgeons prescribed postoperative outpatient antibiotics in reconstruction patients with drains, with 46% continuing antibiotics until drains were removed. The similar findings in these two studies underscore the fact that in current practice, antibiotics are commonly utilized beyond 24 hours in reconstruction cases, despite lack of evidence on this practice.
The primary strength of this study was the ability to access the membership of the ASBrS, who should represent a relevant population of surgeons with a strong interest in and experience with breast and axillary procedures. We acknowledge several limitations to our study. The data reported and conclusions are limited to the questions and response items of our questionnaire. Due to the descriptive, categorical nature of the variables used to assess responses, nuances within the responses may not be reported. Finally, this study is subject to the usual limitations of survey studies, including selection bias and self-reporting.
Despite the fact that breast operations are very common, this study demonstrates that a gap exists in our understanding of optimal use of postoperative antibiotic prophylaxis to reduce surgical site infection in breast procedures requiring drains. This gap is due to a lack of data, resulting in a widely variable practice of postoperative antibiotic prophylaxis. A pilot study is currently underway at our institution to better understand the role of bacterial colonization of drains and its relationship to SSI.[17] Further investigations are needed to determine if there is a benefit to postoperative antibiotic prophylaxis when drains are used. If there is indeed a benefit, appropriate selection criteria need to be developed. Additionally, methods of caring for surgical drains that may prevent SSI should also be investigated as they may decrease the need for antibiotic prophylaxis.
Conclusions
In this survey study, members of the American Society of Breast Surgeons reported infrequent use of prolonged postoperative antibiotic prophylaxis in non-reconstruction cases with drains, in contrast to common use of prolonged antibiotics in immediate tissue expander or implant reconstruction cases. This demonstrates a gap between guidelines and practice and illustrates the need to consider clinical trials regarding the utility of postoperative antibiotic prophylaxis in breast surgery.
Synopsis.
National practice guidelines require antibiotic discontinuation 24 hours after operation. A survey of the American Society of Breast Surgeons shows that prolonged antibiotic prophylaxis in breast operations requiring drains is common, especially with reconstruction, despite unproven efficacy.
Acknowledgments
Amy C. Degnim is supported by the CA90628-08 Paul Calabresi Award for Clinical-Translational Research (K12) via the Mayo Clinic Cancer Center. Rushin Brahmbhatt is supported by the Mayo Clinic Clinical Investigator Program. This project was also supported by NIH/NCRR CTSA Grant Number UL1 RR024150. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Sincere appreciation to Marilyn Churchward for assistance with manuscript preparation.
Support: This study was supported by intramural funds.
Footnotes
Financial Disclosures: None relevant
References
- 1.Vilar-Compte D, Jacquemin B, Robles-Vidal C, Volkow P. Surgical site infections in breast surgery: case-control study. World journal of surgery. 2004;28:242–6. doi: 10.1007/s00268-003-7193-3. [DOI] [PubMed] [Google Scholar]
- 2.Ruvalcaba-Limon E, Robles-Vidal C, Poitevin-Chacon A, Chavez-Macgregor M, Gamboa-Vignolle C, Vilar-Compte D. Complications after breast cancer surgery in patients treated with concomitant preoperative chemoradiation: A case-control analysis. Breast cancer research and treatment. 2006;95:147–52. doi: 10.1007/s10549-005-9058-y. [DOI] [PubMed] [Google Scholar]
- 3.Prospero E, Cavicchi A, Bacelli S, Barbadoro P, Tantucci L, D'Errico MM. Surveillance for surgical site infection after hospital discharge: a surgical procedure-specific perspective. Infection control and hospital epidemiology : the official journal of the Society of Hospital Epidemiologists of America. 2006;27:1313–7. doi: 10.1086/509838. [DOI] [PubMed] [Google Scholar]
- 4.Neumayer L, Schifftner TL, Henderson WG, Khuri SF, El-Tamer M. Breast cancer surgery in Veterans Affairs and selected university medical centers: results of the patient safety in surgery study. Journal of the American College of Surgeons. 2007;204:1235–41. doi: 10.1016/j.jamcollsurg.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 5.Nahabedian MY, Tsangaris T, Momen B, Manson PN. Infectious complications following breast reconstruction with expanders and implants. Plastic and reconstructive surgery. 2003;112:467–76. doi: 10.1097/01.PRS.0000070727.02992.54. [DOI] [PubMed] [Google Scholar]
- 6.Edwards JR, Peterson KD, Mu Y, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. American journal of infection control. 2009;37:783–805. doi: 10.1016/j.ajic.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plastic and reconstructive surgery. 2002;109:2265–74. doi: 10.1097/00006534-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 8.de Blacam C, Ogunleye AA, Momoh AO, et al. High body mass index and smoking predict morbidity in breast cancer surgery: a multivariate analysis of 26,988 patients from the national surgical quality improvement program database. Ann Surg. 2012;255:551–5. doi: 10.1097/SLA.0b013e318246c294. [DOI] [PubMed] [Google Scholar]
- 9.Olsen MA, Lefta M, Dietz JR, et al. Risk factors for surgical site infection after major breast operation. J Am Coll Surg. 2008;207:326–35. doi: 10.1016/j.jamcollsurg.2008.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felippe WA, Werneck GL, Santoro-Lopes G. Surgical site infection among women discharged with a drain in situ after breast cancer surgery. World journal of surgery. 2007;31:2293–9. doi: 10.1007/s00268-007-9248-3. discussion 300–1. [DOI] [PubMed] [Google Scholar]
- 11.Lanier SW, ED, Phillips BT, Khan SU, Dagum AB, Bui DT. The Association Between Closed Suction Drainage Duration and Complication Rates in Tissue Expander/Implant Breast Reconstruction with Antibiotic Prophylaxis. Plastic and Reconstructive Surgery. 2010;125:67. [Google Scholar]
- 12.ASHP Therapeutic Guidelines on Antimicrobial Prophylaxis in Surgery. American Society of Health-System Pharmacists. Am J Health Syst Pharm. 1999;56:1839–88. doi: 10.1093/ajhp/56.18.1839. [DOI] [PubMed] [Google Scholar]
- 13.Rosenberger LH, Politano AD, Sawyer RG. The surgical care improvement project and prevention of post-operative infection, including surgical site infection. Surg Infect (Larchmt) 2011;12:163–8. doi: 10.1089/sur.2010.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Throckmorton AD, Baddour LM, Hoskin TL, Boughey JC, Degnim AC. Microbiology of surgical site infections complicating breast surgery. Surg Infect (Larchmt) 2010;11:355–9. doi: 10.1089/sur.2009.029. [DOI] [PubMed] [Google Scholar]
- 15.Throckmorton AD, Boughey JC, Boostrom SY, et al. Postoperative prophylactic antibiotics and surgical site infection rates in breast surgery patients. Ann Surg Oncol. 2009;16:2464–9. doi: 10.1245/s10434-009-0542-1. [DOI] [PubMed] [Google Scholar]
- 16.Phillips BT, Wang ED, Mirrer J, et al. Current practice among plastic surgeons of antibiotic prophylaxis and closed-suction drains in breast reconstruction: experience, evidence, and implications for postoperative care. Ann Plast Surg. 2011;66:460–5. doi: 10.1097/SAP.0b013e31820c0593. [DOI] [PubMed] [Google Scholar]
- 17.Scow JS, Hoskin TL, Boughey JC, et al. Randomized Controlled Trial to Reduce Bacterial Colonization of Surgical Drains After Breast and Axillary Operations. Annals of surgical oncology. 2011;18:S180-S. doi: 10.1097/SLA.0b013e31828c0b85. [DOI] [PMC free article] [PubMed] [Google Scholar]