Abstract
Subject matter experts systematically reviewed evidence on the effectiveness of housing interventions that affect health outcomes, primarily asthma, associated with exposure to moisture, mold, and allergens. Three of the 11 interventions reviewed had sufficient evidence for implementation: multifaceted, in-home, tailored interventions for reducing asthma morbidity; integrated pest management to reduce cockroach allergen; and combined elimination of moisture intrusion and leaks and removal of moldy items to reduce mold and respiratory symptoms. Four interventions needed more field evaluation, one needed formative research, and three either had no evidence of effectiveness or were ineffective. The three interventions with sufficient evidence all applied multiple, integrated strategies. This evidence review shows that selected interventions that improve housing conditions will reduce morbidity from asthma and respiratory allergies.
Keywords: asthma, moisture, allergens, dust, mites, cockroaches, rats, mice, prevention, housing
Introduction
Asthma is of great concern because its prevalence and morbidity have increased dramatically in the past 2 decades.1 Recent basic research suggests that asthma develops as a result of interactions between genes and environments.2 The contribution of environmental factors to the observed increase in asthma has been the focus of many investigations.3–7 Biologic agents figure prominently among environmental factors implicated in asthma morbidity, including allergens from cockroaches, rodents, dust mites, and fungi, in addition to respiratory irritants such as fungal cell wall components.4
Housing conditions are associated with exposure to these biologic agents. Excess moisture in a home supports the growth of mold and provides an environment favorable to dust mites, cockroaches, and rodents. Common sources of water and moisture in homes include structural membrane leaks, condensation, damp foundations and crawl spaces, inadequate ventilation, activities such as bathing and cooking, and unattended plumbing problems.7 Structural and plumbing deficiencies in a home provide entry points for pests, which are attracted by hidden food spills and garbage.8 Poorly maintained heating and ventilation can disburse allergen-containing dust throughout the home.
House Dust Mites
Dust mite allergens are the only class of inhalant allergens for which the National Academy of Sciences found sufficient evidence for a causal association between exposure and the development of asthma.4 Exposure to dust mite allergen is also associated with asthma exacerbations. A body of clinical and epidemiologic evidence suggests that exposure to der p or der f antigens at levels greater than 2 ug/mg is associated with sensitization and above 10 ug/mg with exacerbation of established asthma in mite-sensitized persons (Custovic et al. 1998; Huss et al. 2001).These cut-points are often used to assess exposure risk in field studies. A recent survey found that more than 80% of homes in the United States have detectable levels of house dust mite allergen in the bedroom, 46% have levels above 2 ug/mg, and 24% have levels above 10 ug/mg.11
Cockroaches
Cockroach allergens are an important cause of asthma exacerbations, particularly in deteriorated homes where cockroach infestation is most common.12,13, 14 Heavy infestations in homes may create reservoirs of allergen in carpets, rugs, beds, and in areas that are difficult to reach behind appliances and furniture.15 A detectable level of cockroach allergen is found in 63% of dwellings in the United States,16 and 10.2% of all dwellings have cockroach allergen levels above the asthma morbidity cut-point.17
Fungi (Mold) and Excessive Moisture
Epidemiologic and laboratory evidence links the presence of mold and moisture to poor health outcomes, such as upper respiratory tract symptoms, cough, wheeze, and other asthma symptoms.18 Although mold is associated with exacerbation of allergic rhinitis and allergic asthma in those people who are sensitized to mold, some components of mold can also elicit inflammation via non-allergic mechanisms.4,18,19 Fungal growth can result from excessive indoor moisture.17
Rodents
The contribution of exposure to rodents to allergic conditions was first described in studies of laboratory animal workers caring for mice and rats.20,21 More recent research has shown that allergens from these rodents are present in homes and are associated with asthma morbidity.22 Detectable levels of mouse allergen are found in 82% of dwellings in the United States.24 The National Cooperative Inner-City Asthma Study (NCICAS) found that 95% of all homes assessed had detectable mouse allergen in at least one room, suggesting that mouse allergens are widely distributed in inner-city homes.25 Chew et al. observed that mouse allergen was common in low-income, inner-city apartments, even when sightings were not reported.26
Interventions Reviewed
The literature search and review methods are described in more detail in a companion paper in this series by Jacobs et.al.27 In brief, the panel sought to identify interventions that are effective in improving asthma outcomes by reducing exposure to indoor biologic asthma triggers. The panel searched the literature for publications describing interventions to reduce exposure to biologic agents related to asthma morbidity as well as the web for guidelines. Titles and abstracts of all retrieved articles were read and relevant articles were reviewed and abstracted into standard study summary templates by 2 panel members and scored as to degree of impact and study quality. Panel members as a group reviewed the scoring and agreed upon classification of each intervention as having sufficient evidence effectiveness and ready for implementation, needing more field testing but promising, promising but needing formative research, and ineffective. An effective intervention results in improvements in health or leads to changes in behaviors or other factors that have been previously shown to result in better health. 28 The definition of “sufficient evidence” of effectiveness is based on the CDC Community Guide, which bases its ratings on intervention studies.28 In addition, we deemed an intervention to have sufficient evidence if the combination of intervention studies (on their own insufficient for meeting the Guide criteria), other expert panel recommendations, and strong epidemiologic evidence of association between exposure and health outcomes was convincing. We did not limit the studies reviewed to randomized controlled trials, because the likelihood of harm from the types of interventions under consideration is low, suggesting that the level of evidence need not be as rigorous, and because this is an emerging and rapidly developing field. In short, the recommendations are based on existing evidence, not the best possible evidence.
For this topic, a panel of subject matter experts reviewed the following 11 interventions:
multifaceted, tailored asthma interventions;
integrated pest management (IPM) to reduce pest exposure;
elimination of moisture intrusion and leaks and removal of moldy items;
improved insulation;
HEPA air filtration;
carpet cleaning and vacuuming;
ventilation and dehumidification;
one-time professional cleaning;
bedding encasement and/or sheet and/or upholstery cleaning alone;
acaricides as a single intervention; and
air cleaners releasing ozone
Results
Of the 11 interventions reviewed, three have sufficient evidence of effectiveness and are ready for implementation, four need more field testing but are promising, one is promising but needs formative research, and three are ineffective.
Sufficient Evidence
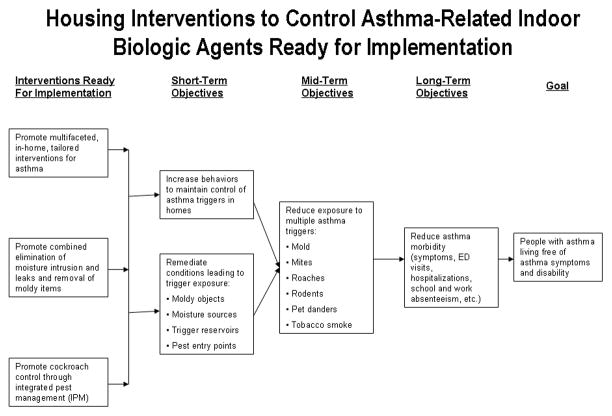
Three interventions were supported by sufficient evidence to warrant widespread implementation. Figure 1 depicts the relationships between these interventions and health outcomes.
Figure 1.
Housing Interventions to Control Indoor Biologic Agents: Interventions Ready for Implementation
1. Multifaceted, in-home, tailored interventions for asthma
Home-based interventions that use a multifaceted approach to help residents decrease exposure to multiple asthma triggers are effective in reducing exposure to triggers, decreasing asthma symptoms and acute health-care use, and improving quality of life. These interventions tailor activities to triggers found in an individual’s home and/or to which the individual is sensitized. Interventions include home environmental assessment, education, use of mattress and pillow covers, use of HEPA (or equivalent) vacuums and HEPA air filters, smoking cessation and reduced environmental tobacco smoke exposure, cockroach and rodent management, minor repairs, and intensified household cleaning. The panel found that evaluations of this approach were well-designed, had many subjects from appropriate populations, and identified statistically significant improvements.
The strongest evidence comes from studies examining the impact of interventions on control of existing asthma.5,29–31 The Inner City Asthma Study (ICAS) was a large, multisite randomized trial that targeted interventions to reduce exposure to asthma triggers to which a child was sensitized. It showed a large and clinically significant reduction in asthma symptoms days and a modest and significant reduction in emergency department and urgent clinic use.29 Eggleston et al. found that their in-home intervention reduced concentrations of airborne particulate matter and dustborne cockroach allergen and decreased daytime asthma symptoms but not other measures of morbidity.30 Krieger et al. showed that home visits by community health workers to support families in decreasing exposure to asthma triggers led to significantly reduced use of urgent health services and to improved quality of life for caretakers.5 Carter and colleagues found that home visits also decreased acute visits for asthma among children with dust mite allergy.29
Other studies with important methodological limitations (such as large attrition rates and small sample size) did not find significant benefits from home interventions.32,33 Additional studies of the benefit of such interventions for reducing incidence of asthma among infants at high risk for it have yielded mixed but generally modest positive results.34–36
The panel conclusion that multifaceted, in-home interventions are effective is consistent with a recent high-quality systematic review of the evidence completed for the Centers for Disease Control and Prevention Task Force on Community Preventive Services. Based on strong evidence of effectiveness for these interventions, the task force now recommends home-based, multi-component, multi-trigger interventions with an environmental focus for children with asthma.37 The conclusion is also supported by recent studies that were not available when this study’s panel convened.38,39
2. Cockroach control through integrated pest management
Integrated pest management is effective in reducing cockroach allergen and pesticides.30, 40 IPM includes carefully assessing the presence and location of roaches, removing food sources through proper food storage and cleaning (in some cases, professional cleaning), educating residents, repairing structural defects that allow roaches to gain access, applying low-toxicity gel-bait pesticides as needed, and monitoring and continuing intervention until roaches are eliminated.
Four randomized, controlled studies have demonstrated the effectiveness of IPM in reducing exposure to cockroaches.30, 41–43 Arbes conducted a 6-month controlled study and found that roach allergen levels were significantly reduced in beds and kitchens. The levels in the beds dropped below the thresholds for both sensitization and exacerbation. Wang and Bennett showed a significantly greater decrease in roach counts with IPM compared with gel bait alone. Miller and Meek found in a randomized study that IPM was initially more costly but also much more effective in reducing cockroaches compared with traditional pesticide treatment. These three studies did not report on health outcomes. A study by Eggleston et al. showed a modest benefit on clinical outcomes but was a multifaceted intervention that addressed other allergens besides cockroaches.
Additional research, using less rigorous methods, has also found IPM to be effective. For example, Levy and colleagues showed reduced cockroach allergen and improved clinical outcomes in a single-group pre-post study.32 McConnell and colleagues44 conducted a randomized trial of IPM methods that showed decreased cockroach counts and dust allergen levels in the IPM group relative to the control group. This trial also showed that intensive cleaning can significantly reduce allergen levels in homes with initially high levels. Clinical outcomes were not reported. Other studies45,46 have also demonstrated improvements, but their conclusions were weakened by small sample sizes, inclusion of multiple interventions in addition to IPM, lack of control groups, use of nonstandard self-reported measures of cockroach exposure, or interventions that would be difficult to replicate.
Evidence of the effectiveness of IPM for reducing exposure to rodent allergens is less well developed. A small study showed no significant improvement in asthma symptoms or forced expiratory volume (FEV) but did show a significant decline in mouse allergen levels.47 In conclusion, the evidence that IPM is effective in reducing exposure to cockroach allergens is quite strong, but further evaluation of its role in reducing exposure to other pests is needed.
3. Combined elimination of moisture intrusion and leaks and removal of moldy items
The panel believes there is enough evidence to begin implementation of interventions that combine elimination of moisture intrusion and leaks and removal of moldy items to reduce mold exposure and respiratory symptoms. The panel took into consideration the IOM Report,18 local (NYC)48 and international guidelines (WHO,49 Finland,50 Canada19), and the studies evaluated below. The recent WHO report that states “Although few intervention studies were available, their results show that remediation of dampness can reduce adverse health outcomes”.49 It is important to recognize that these interventions may not produce improvements in health in all individuals who are exposed to dampness and mold.
In addition, the panel reviewed several intervention studies, many of which were limited by small sample size, lack of control groups, or implementation in non-residential settings. The largest study (164 homes) was a randomized controlled trial of visible mold eradication (with removal, fungicide application, and ventilation fan installation) among people with asthma. It reduced symptoms and medication use, although not peak flow variability.51 Another randomized trial52 had only 29 participants in the experimental group and 33 in the control group. Despite the small sample size, this housing remediation intervention showed improved asthma clinical outcomes. While it is not clear how much mold was in the homes of these studies before the intervention, both studies listed presence of mold as an inclusion criterion.
Several smaller studies have also suggested that interventions can decrease exposure to mold. One study examined the effect of prompt remediation after water intrusion in a single home and found decreased spore counts and resolution of allergic symptoms.53 A time-series study compared mold exposure and symptoms at a mold-contaminated school before and after remediation with a comparison school. The investigators found that, prior to remediation, the contaminated school had higher mold levels and the children had more allergic and respiratory symptoms than the comparison school. These differences disappeared after intervention.54 A small uncontrolled study of moisture and mold control in three flood-damaged homes showed that mold (e.g., spore and colony counts) and endotoxin increased significantly during renovation work and declined significantly following the removal of moldy items and a multistep cleanup process.55
Promising Interventions That Need More Field Evaluation
The panel identified four interventions—improved insulation, repeated dry-steam cleaning of carpets and upholstered furniture and repeated vacuuming, use of air cleaning devices, and moisture control through dehumidification (including improved general and local exhaust ventilation)—as promising interventions that need more field testing. Each of these interventions has been evaluated, but the evidence of effectiveness is not sufficient to recommend widespread implementation. Further evaluation in real-world settings is needed to determine generalizabilty and feasibility of replication.
1. Improved insulation
The panel found that a large, well-designed, randomized, controlled trial of home insulation in New Zealand showed decreased moisture and mold exposure and improved general and respiratory health status.56 This promising finding should be replicated in different climate zones and settings as the next step toward wider implementation.
2. Repeated dry-steam cleaning and repeated vacuuming
The panel found that several studies of repeated cleaning and/or vacuuming showed these interventions to be promising but in need of more field testing. For example, a small study (11 homes) of intensive vacuuming and steam cleaning of carpeting and furnishings showed sustained reductions in concentration and load of mite allergen in dust relative to vacuuming alone. Both approaches decreased allergen levels, but a control group was not included in the study and clinical outcomes were not reported.57 These findings are consistent with those from a small laboratory study showing benefits from steam cleaning.58 British investigators found that high-efficiency vacuums reduced cat and dog allergen concentrations but not dust mite allergen concentrations. Patients showed improved pulmonary function and decreased beta-agonist use.59 Several studies have demonstrated that repeated vacuuming can decrease mite levels, although these studies were of short duration and did not report clinical outcomes.60,61 A small study that compared five HEPA vacuums with one regular vacuum did not find any difference in exposure to mite allergen during vacuuming.62 Laboratory studies that examined the effect of one-time vacuuming of carpet samples have yielded both positive and negative results.63,64 The vacuuming procedure may not have been intensive enough to show a benefit in the negative study.
3. Use of air cleaning devices
Evaluation of HEPA air filtration has yielded mixed results. A review by Wood concluded that HEPA filters may be effective for removing pet allergens, although studies were mixed and more evidence is needed.65 HEPA filters do not appear to be effective for reducing exposure to mites and mold. When used in uncarpeted rooms or in conjunction with HEPA vacuuming of carpeted rooms, HEPA air filters were effective in decreasing cat and dog allergen.66–68
Evidence for improvements in clinical outcomes is less convincing. For example, a small, randomized, controlled trial examining the reduction of cat allergen by using HEPA air filtration, along with bedding encasements and cat exclusion, did not show a significant clinical effect.69 However, another small (n = 40), randomized trial of HEPA air filters showed a decline in airborne particulates and possible improvement in rhinitis or asthma symptoms and medication use among patients with sensitivity to dust mites.70 Van der Heide found that HEPA filters improved airways hyperesponsiveness but not symptoms among 20 cat- or dog-allergic children.71 Another study showed modest clinical benefits but no reduction in pet allergens.72 A comparison of vacuuming with vacuuming plus air filters found modest clinical benefits from the filters but no improvement in allergen exposure.66 A Cochrane review concluded that the evidence is insufficient to support or refute the effectiveness of air filters among people with pet allergies and exposure to pets.73
4. Moisture control through dehumidification
Ventilation and dehumidification to reduce humidity levels and exposure to mites have yielded mixed but generally positive results. In a national survey, the use of a dehumidifier was an independent predictor of lower levels of some asthma triggers and mold.74 Installation of whole-house mechanical ventilation can decrease humidity, decrease mite numbers, decrease mite allergen levels, and improve clinical outcomes.75–77 Dehumidification in temperate climates with air conditioners and dehumidifiers is effective in reducing mite levels.78 Ventilation and moisture control are typically related. Also, ventilation can decrease indoor contaminants, assuming that the outdoor air has lower levels of contaminants than the indoor air, which is not always the case if housing is located near point sources such as industrial emissions or near high-traffic roadways. In high-humidity climates, whole-house ventilation has been less effective.79–81 Ventilation and air cleaners are considered further by Sandel et al.82 in a companion paper in this series.
Interventions in Need of Formative Research
1. One-time professional cleaning
The panel identified one-time professional cleaning as an intervention needing more formative efficacy research. Professional cleaning included removing clutter, washing hard surfaces and vacuuming porous surfaces. Such cleaning is largely ineffective for lead hazard control purposes and has very short-lived effects.83 However, this cleaning may be more effective for biological contaminants if key elements of the cleaning process can be identified. For example, evidence shows that cleaning reduces cockroach allergen levels.44,84
No Evidence/Ineffective/Harmful Interventions
The panel found that three interventions—air cleaners that generate high levels of ozone, bedding encasement and/or sheet and/or upholstery cleaning alone, and acaricides (chemicals that reduce mite allergen levels) as a single intervention—either had no evidence of effectiveness or were ineffective - and should not be used.
1. Air cleaners generating high levels of ozone
The panel found that air cleaners that generate high levels of ozone should not be used because of the association between ozone and asthma morbidity85 and because of the unknown benefit such devices have on removing indoor airborne particulate matter.6
2. Bedding encasement, sheet or upholstery cleaning alone
Studies that used single interventions—such as bedding encasements, sheet or upholstery cleaning—to control specific asthma triggers without the multifaceted approach described above either did not find benefit or tended to suffer from methodological deficiencies. The use of bedding encasements as isolated interventions to reduce exposure to mite allergen and improve asthma and allergy outcomes has been well studied. Two well-designed, large, randomized studies did not find improvements in clinical measures.86,87 Other earlier, smaller studies of bedding covers also did not find symptom benefits,88,89 although the van den Bemt study observed improvement in morning peak flow. A study that evaluated efficacy of mattress covers, but had limited covariate data, showed no effect on clinical status.90
Studies that have attempted to prevent asthma incidence by reducing exposure to a single allergen (dust mite) have generally not been successful. For example, two studies employed multiple mite control measures among high-risk children. The Child Asthma Prevention Study, a well-designed trial that assessed the impact of bedding encasements and bed linen washing with acaracide solution, did not show reduced asthma, wheeze, or atopy incidence.91,92 Another multi-component study using allergen-impermeable covers for the maternal and child beds, an allergen-impermeable cot/carrycot mattress, a high-filtration vacuum cleaner, vinyl flooring in the child’s bedroom, bed linen that was hot-washed weekly, and a washable, soft toy, showed increased mite sensitization in the intervention group but better lung function (specific airway resistance) at age 3 years.93 A study that employed aggressive and multiple interventions for mites (tannic acid, bedding encasements, and laundry service) showed decreased exposure and improved airways hyper-responsiveness but did not affect FEV1 (a measure of lung function), symptoms, or quality of life.94
3. Acaricides as a single intervention
The panel found that acaricides used as a single intervention do not appear to be effective. A study of treating carpets with chemicals (tannic acid and benzyl benzoate) showed reduced mite allergen concentration, but effects were not seen in all treated carpets and were not long lasting.95 In addition, certain carpet treatments can interfere with immunoassay measurement of allergens, which questions the validity of studies that used this outcome measure.95,96 A meta-analysis of 23 studies that focused on dust mite control with acaricides found no effect.97
Conclusions
The panel concluded that some interventions are effective in reducing exposure to indoor biologic agents that can cause asthma symptoms among people with asthma. In particular, sufficient evidence supports the widespread dissemination of multifaceted, in-home, tailored interventions for asthma; integrated pest management for reducing cockroach allergen; and combined elimination of moisture intrusion and leaks and removal of moldy items to reduce respiratory symptoms. An important limitation of these conclusions is that the effectives of interventions may vary by region (due to variability in climate and predominant types of housing) and tailoring to local conditions may be important. Another caveat is that even the strongest housing interventions will be hampered in their ability to reduce asthma morbidity if those individuals are exposed to other indoor and outdoor pollutants, such as environmental tobacco smoke and ozone.
Acknowledgments
This work was supported by a cooperative grant with the Centers for Disease Control and Prevention, Office of Healthy Homes and Lead Poisoning Prevention, and the National Center for Healthy Housing. In addition funding was provided by NIH P30 ES 009089.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
James Krieger, Chief, Chronic Disease and Injury Prevention Section, Public Health - Seattle and King County, Seattle, Washington.
David E. Jacobs, Director of research, National Center for Healthy Housing, Columbia, Maryland.
Peter J. Ashley, Environmental scientist, Office of Healthy Homes and Lead Hazard Control, U.S. Department of Housing and Urban Development, Washington, DC.
Andrea Baeder, Prevention specialist, Centers for Disease Control and Prevention, Atlanta, Georgia.
Ginger L. Chew, Epidemiologist, Centers for Disease Control and Prevention, Atlanta, Georgia, and also adjunct assistant professor of environmental health sciences, Mailman School of Public Health, Columbia University, New York City, New York.
Dorr Dearborn, Chairman, Department of Environmental Health Sciences, Professor, Case Western Reserve University, Cleveland, Ohio.
H. Patricia Hynes, Professor of environmental health, Boston University, School of Public Health, Boston, Massachusetts.
J. David Miller, Professor of biochemistry, Carleton University, Ottawa, Ontario, Canada.
Rebecca Morley, Executive director, National Center for Healthy Housing, Columbia, Maryland.
Felicia Rabito, Associate professor, Department of Epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, Louisiana.
DC Zeldin, Acting clinical director, National Institutes of Health, National Institute of Environmental Health Sciences, Research Triangle Park, North Carolina.
References
- 1.Centers for Disease Control and Prevention. National surveillance for asthma--United States, 1980–2004. MMWR Morb Mortal Wkly Rep. 2007;56(SS–8) [Google Scholar]
- 2.von Mutius E. Gene-environment interactions in asthma. J Allergy Clin Immunol. 2009;123(1):3–11. doi: 10.1016/j.jaci.2008.10.046. [DOI] [PubMed] [Google Scholar]
- 3.Miller RL. Breathing freely: the need for asthma research on gene-environment interactions. Am J Public Health. 1999;89(6):819–822. doi: 10.2105/ajph.89.6.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine. Clearing the Air: Asthma and Indoor Air Exposures. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 5.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–659. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diette GB, McCormack MC, Hansel NN, Breysse PN, Matsui EC. Environmental issues in managing asthma. Respir Care. 2008;53(5):602–615. discussion 616–617. [PMC free article] [PubMed] [Google Scholar]
- 7.Dales R, Liu L, Wheeler AJ, Gilbert NL. Quality of indoor residential air and health. Can Med Assoc J. 2008;179(2):147–152. doi: 10.1503/cmaj.070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogg B, Ferraro D, Ogg O. Cockroach Control Manual. Lincoln, NE: University of Nebraska-Lincoln; 1995. pp. 1–91. [Google Scholar]
- 9.Gravesen S. Identification and prevalence of culturable mesophilic microfungi in house dust from 100 Danish homes; comparison between airborne and dust-bound fungi. Allergy. 1978;33:268–272. doi: 10.1111/j.1398-9995.1978.tb01547.x. [DOI] [PubMed] [Google Scholar]
- 10.Tovey ER, Chapman MD, Platts-Mills TA. Mite faeces are a major source of house dust allergens. Nature. 1981;289(5798):592–593. doi: 10.1038/289592a0. [DOI] [PubMed] [Google Scholar]
- 11.Arbes SJ, Jr, Cohn RD, Yin M, et al. House dust mite allergen in U.S. beds: results from the First National Survey of Lead and Allergens in Housing. J Allergy Clin Immunol. 2003;111(2):408–414. doi: 10.1067/mai.2003.16. [DOI] [PubMed] [Google Scholar]
- 12.Chew G, Perzanowski M, Canfield S, et al. Cockroach allergen levels and associations with cockroach-specific IgE. J Allergy Clin Immunol. 2008;121(1):240–245. doi: 10.1016/j.jaci.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 13.Rauh VA, Chew GL, Garfinkel RS. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ Health Perspect. 2002;110(2):323–327. doi: 10.1289/ehp.02110s2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenstreich DL, Eggleston P, Kattan M, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336(19):1356–1363. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 15.Eggleston PA, Arruda LK. Ecology and elimination of cockroaches and allergens in the home. J Allergy Clin Immunol. 2001;107(3 Suppl):S422–S429. doi: 10.1067/mai.2001.113671. [DOI] [PubMed] [Google Scholar]
- 16.Cohn RD, Arbes SJ, Jr, Jaramillo R, Reid LH, Zeldin DC. National prevalence and exposure risk for cockroach allergen in U.S. households. Environ Health Perspect. 2006;114(4):522–526. doi: 10.1289/ehp.8561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salo PM, Arbes SJ, Crockett PW, et al. Exposure to multiple indoor allergens in U.S. homes and its relationship to asthma. J Allergy Clin Immunol. 2008;121:678–684. doi: 10.1016/j.jaci.2007.12.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Damp Indoor Spaces and Health. Washington, DC: National Academy Press; 2004. [Google Scholar]
- 19.Health Canada. Fungal contamination in public buildings: health effects and investigation methods. Ottawa, Canada: Health Canada; 2004. [Accessed November 4, 2009]. http://www.hc-sc.gc.ca/ewh-semt/alt_formats/hecs-sesc/pdf/pubs/air/fungal-fongique/fungal-fongique-eng.pdf. [Google Scholar]
- 20.Hollander A, Heederik D, Doekes G, Kromhout H. Determinants of airborne rat and mouse urinary allergen exposure. Scand J Work Environ Health. 1998;24(3):228–235. doi: 10.5271/sjweh.303. [DOI] [PubMed] [Google Scholar]
- 21.Lieutier-Colas F, Meyer P, Pons F, et al. Prevalence of symptoms, sensitization to rats, and airborne exposure to major rat allergen (Rat n 1) and to endotoxin in rat-exposed workers: a cross-sectional study. Clin Exp Allergy. 2002;32(10):1424–1429. doi: 10.1046/j.1365-2745.2002.01502.x. [DOI] [PubMed] [Google Scholar]
- 22.Phipatanakul W. Rodent allergens. Curr Allergy Asthma Rep. 2002;2(5):412–416. doi: 10.1007/s11882-002-0075-1. [DOI] [PubMed] [Google Scholar]
- 23.Ohman JL, Hagberg K, MacDonald MR, et al. Distribution of airborne mouse allergen in a major breeding facility. J Allergy Clin Immunol. 1994;94:810–817. doi: 10.1016/0091-6749(94)90147-3. [DOI] [PubMed] [Google Scholar]
- 24.Cohn RD, Arbes SJ, Jr, Yin M, Jaramillo R, Zeldin DC. National prevalence and exposure risk for mouse allergen in U.S. households. J Allergy Clin Immunol. 2004;113(6):1167–1171. doi: 10.1016/j.jaci.2003.12.592. [DOI] [PubMed] [Google Scholar]
- 25.Phipatanakul W, Eggleston PA, Wright EC, Wood RA. Mouse allergen. I. The prevalence of mouse allergen in inner-city homes. The National Cooperative Inner-City Asthma Study. J Allergy Clin Immunol. 2000;106(6):1070–1074. doi: 10.1067/mai.2000.110796. [DOI] [PubMed] [Google Scholar]
- 26.Chew GL, Perzanowski MS, Miller RL, et al. Distribution and determinants of mouse allergen exposure in low-income New York City apartments. Environ Health Perspect. 2003;111(10):1348–1351. doi: 10.1289/ehp.6124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacobs DE, Brown MJ, Baeder A, Scalia Sucosky M, Margolis S, Hershovitz J, Kolb L, Morley R. A Systematic Review of Housing Interventions and Health: Introduction and Methods. J Public Health Manag Pract. 2010;x(x):xxx–xxx. doi: 10.1097/PHH.0b013e3181e31d09. [DOI] [PubMed] [Google Scholar]
- 28.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services-methods. Am J Prev Med. 2000;18(1S):35–43. doi: 10.1016/s0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 29.Carter MC, Perzanowski MS, Raymond A, Platts-Mills TAE. Home intervention in the treatment of asthma among inner-city children. J Allergy Clin Immunol. 2001;108(5):732–737. doi: 10.1067/mai.2001.119155. [DOI] [PubMed] [Google Scholar]
- 30.Eggleston PA, Butz A, Rand C, et al. Home environmental intervention in inner-city asthma: a randomized controlled clinical trial. Ann Allergy Asthma Immunol. 2005;95(6):518–524. doi: 10.1016/S1081-1206(10)61012-5. [DOI] [PubMed] [Google Scholar]
- 31.Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068–1080. doi: 10.1056/NEJMoa032097. [DOI] [PubMed] [Google Scholar]
- 32.Levy JI, Brugge D, Peters JL, Clougherty JE, Saddler SS. A community-based participatory research study of multifaceted in-home environmental interventions for pediatric asthmatics in public housing. Soc Sci Med. 2006;63(8):2191–2203. doi: 10.1016/j.socscimed.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 33.Williams SG, Brown CM, Falter KH, et al. Does a multifaceted environmental intervention alter the impact of asthma on inner-city children? J Natl Med Assoc. 2006;98(2):249–260. [PMC free article] [PubMed] [Google Scholar]
- 34.Becker A, Watson W, Ferguson A, Dimich-Ward H, Chan-Yeung M. The Canadian asthma primary prevention study: outcomes at 2 years of age. J Allergy Clin Immunol. 2004;113(4):650–656. doi: 10.1016/j.jaci.2004.01.754. [DOI] [PubMed] [Google Scholar]
- 35.Schonberger H, Dompeling E, Knottnerus JA, et al. The PREVASC study: the clinical effect of a multifaceted educational intervention to prevent childhood asthma. Eur Respir J. 2005;25(4):660–670. doi: 10.1183/09031936.05.00067704. [DOI] [PubMed] [Google Scholar]
- 36.Maas T, Kaper J, Sheikh A, et al. Mono and multifaceted inhalant and/or food allergen reduction interventions for preventing asthma in children at high risk of developing asthma. Cochrane Database Syst Rev. 2009;3:CD006480. doi: 10.1002/14651858.CD006480.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Crocker D, Hopkins D, Kinyota S, et al. Home-based interventions to reduce asthma morbidity and mortality. Presentation to the Task Force on Community Preventive Services; Atlanta, GA. 2008. [Google Scholar]
- 38.Parker EA, Israel BA, Robins TG, et al. Evaluation of community action against asthma: a community health worker intervention to improve children’s asthma-related health by reducing household environmental triggers for asthma. Health Educ Behav. 2008;35(3):376–395. doi: 10.1177/1090198106290622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krieger J, Takaro TK, Song L, Beaudet N, Edwards K. The Seattle-King County Healthy Homes II Project: a randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers. Archives Ped Adolesc Med. 2009;163(2):141–149. doi: 10.1001/archpediatrics.2008.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Williams MK, Barr DB, Camann DE, et al. An intervention to reduce residential insecticide exposure during pregnancy among an inner-city cohort. Environ Health Perspect. 2006;114(11):1684–1689. doi: 10.1289/ehp.9168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang CL, Bennett GW. Comparative study of integrated pest management and baiting for German cockroach management in public housing. J Econ Entomol. 2006;99(3):879–885. doi: 10.1603/0022-0493-99.3.879. [DOI] [PubMed] [Google Scholar]
- 42.Miller DM, Meek F. Cost and efficacy comparison of integrated pest management strategies with monthly spray insecticide applications for German cockroach (Dictyoptera: Blattellidae) control in public housing. J Econ Entomol. 2004;97(2):559–569. doi: 10.1093/jee/97.2.559. [DOI] [PubMed] [Google Scholar]
- 43.Arbes SJ, Sever M, Archer J, et al. Abatement of cockroach allergen (Bla g 1) in low-income, urban housing: a randomized controlled trial. J Allergy Clin Immunol. 2003;112(2):339–345. doi: 10.1067/mai.2003.1597. [DOI] [PubMed] [Google Scholar]
- 44.McConnell R, Jones C, Milam J, et al. Cockroach counts and house dust allergen concentrations after professional cockroach control and cleaning. Ann Allergy Asthma Immunol. 2003;91(6):546–552. doi: 10.1016/S1081-1206(10)61532-3. [DOI] [PubMed] [Google Scholar]
- 45.Klitzman S, Caravanos J, Belanoff C, Rothenberg L. A multihazard, multistrategy approach to home remediation: results of a pilot study. Environ Res. 2005;99(3):294–306. doi: 10.1016/j.envres.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 46.Sever ML, Arbes SJ, Gore JC, et al. Cockroach allergen reduction by cockroach control alone in low-income urban homes: a randomized control trial. J Allergy Clin Immunol. 2007;120:849–855. doi: 10.1016/j.jaci.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phipatanakul W, Cronin B, Wood RA, et al. Effect of environmental intervention on mouse allergen levels in homes of inner-city Boston children with asthma. Ann Allergy Asthma Immunol. 2004;92(4):420–425. doi: 10.1016/S1081-1206(10)61777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.New York City Department of Health and Mental Hygiene. [Accessed December 8, 2009];Guidelines on assessment and remediation of fungi in indoor environments. 2008 Nov; http://www.nyc.gov/html/doh/html/epi/moldrpt1.shtml.
- 49.World Health Organization. WHO Guidelines for indoor air quality Dampness and Mould. WHO Regional Office for Europe Copenhagen O; Denmark: 2009. [Accessed December 3, 2009]. http://www.euro.who.int/document/E92645.pdf. [PubMed] [Google Scholar]
- 50.Husman TM. The Health Protection Act, National Guidelines for Indoor Air Quality and Development of the National Indoor Air Programs in Finland. Environ Health Perspect. 1999;107(suppl 3):515–517. doi: 10.1289/ehp.99107s3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Burr ML, Matthews IP, Arthur RA, et al. Effects on patients with asthma of eradicating visible indoor mould: a randomised controlled trial. Thorax. 2007;62(9):766–771. doi: 10.1136/thx.2006.070847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kercsmar CM, Dearborn DG, Schluchter M, et al. Reduction in asthma morbidity in children as a result of home remediation aimed at moisture sources. Environ Health Perspect. 2006;114(10):1574–1580. doi: 10.1289/ehp.8742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rockwell W. Prompt remediation of water intrusion corrects the resultant mold contamination in a home. Allergy Asthma Proc. 2005;26(4):316–318. [PubMed] [Google Scholar]
- 54.Lignell U, Meklin T, Putus T, et al. Effects of moisture damage and renovation on microbial conditions and pupils’ health in two schools: a longitudinal analysis of five years. J Environ Monit. 2007;9(3):225–233. doi: 10.1039/b615459j. [DOI] [PubMed] [Google Scholar]
- 55.Chew GL, Wilson J, Rabito FA, et al. Mold and endotoxin levels in the aftermath of Hurricane Katrina: a pilot project of homes in New Orleans undergoing renovation. Environ Health Perspect. 2006;114(12):1883–1889. doi: 10.1289/ehp.9258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Howden-Chapman P, Matheson A, Crane J, et al. Effect of insulating existing houses on health inequality: cluster randomised study in the community. BMJ. 2007;334(7591):460–464. doi: 10.1136/bmj.39070.573032.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vojta PJ, Randels SP, Stout J, et al. Effects of physical interventions on house dust mite allergen levels in carpet, bed, and upholstery dust in low-income, urban homes. Environ Health Perspect. 2001;109(8):815–819. doi: 10.1289/ehp.01109815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Colloff MJ, Taylor C, Merrett TG. The use of domestic steam cleaning for the control of house-dust mites. Clin Exp Allergy. 1995;25(11):1061–1066. doi: 10.1111/j.1365-2222.1995.tb03252.x. [DOI] [PubMed] [Google Scholar]
- 59.Popplewell EJ, Innes VA, Lloyd-Hughes S, et al. The effect of high-efficiency and standard vacuum-cleaners on mite, cat and dog allergen levels and clinical progress. Pediatr Allergy Immunol. 2000;11(3):142–148. doi: 10.1034/j.1399-3038.2000.00058.x. [DOI] [PubMed] [Google Scholar]
- 60.Adilah N, Fitzharris P, Crane J, Siebers RW. The effect of frequent vacuum cleaning on the house dust mite allergen, Der p 1 in carpets: a pilot study. N Z Med J. 1997 Nov 28;110(1056):438–439. [PubMed] [Google Scholar]
- 61.Munir AK, Einarsson R, Dreborg SK. Vacuum cleaning decreases the levels of mite allergens in house dust. Pediatr Allergy Immunol. 1993;4(3):136–143. doi: 10.1111/j.1399-3038.1993.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 62.Gore RB, Durrell B, Bishop S, et al. High-efficiency vacuum cleaners increase personal mite allergen exposure, but only slightly. Allergy. 2006;61(1):119–123. doi: 10.1111/j.1398-9995.2005.00946.x. [DOI] [PubMed] [Google Scholar]
- 63.Sercombe JK, Liu-Brennan D, Causer SM, Tovey ER. The vertical distribution of house dust mite allergen in carpet and the effect of dry vacuum cleaning. Int J Hyg Environ Health. 2007;210(1):43–50. doi: 10.1016/j.ijheh.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 64.Roberts JW, Clifford WS, Glass G, Hummer PG. Reducing dust, lead, dust mites, bacteria, and fungi in carpets by vacuuming. Arch Environ Contam Toxicol. 1999;36(4):477–484. doi: 10.1007/pl00022756. [DOI] [PubMed] [Google Scholar]
- 65.Wood RA. Air filtration devices in the control of indoor allergens. Curr Allergy Asthma Rep. 2002;2(5):397–400. doi: 10.1007/s11882-002-0073-3. [DOI] [PubMed] [Google Scholar]
- 66.Green R, Simpson A, Custovic A, et al. The effect of air filtration on airborne dog allergen. Allergy. 1999;54(5):484–488. doi: 10.1034/j.1398-9995.1999.00029.x. [DOI] [PubMed] [Google Scholar]
- 67.de Blay F, Chapman MD, Platts-Mills TA. Airborne cat allergen (Fel d I): environmental control with the cat in situ. Am Rev Respir Dis. 1991;143(6):1334–1339. doi: 10.1164/ajrccm/143.6.1334. [DOI] [PubMed] [Google Scholar]
- 68.Custovic A, Simpson A, Pahdi H, et al. Distribution, aerodynamic characteristics, and removal of the major cat allergen Fel d 1 in British homes. Thorax. 1998;53(1):33–38. doi: 10.1136/thx.53.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wood RA, Johnson EF, Van Natta ML, Chen PH, Eggleston PA. A placebo-controlled trial of a HEPA air cleaner in the treatment of cat allergy. Am J Respir Crit Care Med. 1998;158(1):115–120. doi: 10.1164/ajrccm.158.1.9712110. [DOI] [PubMed] [Google Scholar]
- 70.Reisman RE, Mauriello PM, Davis GB, Georgitis JW, Demasi JM. A double-blind-study of the effectiveness of a high-efficiency particulate air (HEPA) filter in the treatment of patients with perennial allergic rhinitis and asthma. J Allergy Clin Immunol. 1990;85(6):1050–1057. doi: 10.1016/0091-6749(90)90050-e. [DOI] [PubMed] [Google Scholar]
- 71.van der Heide S, van Aalderen WMC, Kauffman HF, Dubois AEJ, de Monchy JGR. Clinical effects of air cleaners in homes of asthmatic children sensitized to pet allergens. J Allergy Clin Immunol. 1999;104(2):447–451. doi: 10.1016/s0091-6749(99)70391-x. [DOI] [PubMed] [Google Scholar]
- 72.Francis H, Fletcher G, Anthony C, et al. Clinical effects of air filters in homes of asthmatic adults sensitized and exposed to pet allergens. Clin Exp Allergy. 2003;33(1):101–105. doi: 10.1046/j.1365-2222.2003.01570.x. [DOI] [PubMed] [Google Scholar]
- 73.Kilburn S, Lasserson TJ, McKean M. Pet allergen control measures for allergic asthma in children and adults. Cochrane Database Syst Rev. 2003;(1):CD002989. doi: 10.1002/14651858.CD002989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Salo PM, Yin M, Arbes SJ, et al. Dustborne Alternaria alternata antigens in U.S. homes: results from the national survey of lead and allergens. J Allergy Clin Immunol. 2005;116(3):623–629. doi: 10.1016/j.jaci.2005.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Warner JA, Frederick JM, Bryant TN, et al. Mechanical ventilation and high-efficiency vacuum cleaning: a combined strategy of mite and mite allergen reduction in the control of mite-sensitive asthma. J Allergy Clin Immunol. 2000;105(1):75–82. doi: 10.1016/s0091-6749(00)90181-7. [DOI] [PubMed] [Google Scholar]
- 76.Harving H, Korsgaard J, Dahl R. Clinical efficacy of reduction in house-dust mite exposure in specially designed, mechanically ventilated “healthy” homes. Allergy. 1994;49(10):866–870. doi: 10.1111/j.1398-9995.1994.tb00789.x. [DOI] [PubMed] [Google Scholar]
- 77.Harving H, Korsgaard J, Dahl R. House-dust mite exposure reduction in specially designed, mechanically ventilated “healthy” homes. Allergy. 1994;49(9):713–718. doi: 10.1111/j.1398-9995.1994.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 78.Arlian L, Neal J, Morgan M, et al. Reducing relative humidity is a practical way to control dust mites and their allergens in homes in temperate climates. J Allergy Clin Immunol. 2001;107(1):99–104. doi: 10.1067/mai.2001.112119. [DOI] [PubMed] [Google Scholar]
- 79.Fletcher AM, Pickering CA, Custovic A, et al. Reduction in humidity as a method of controlling mites and mite allergens: the use of mechanical ventilation in British domestic dwellings. Clin Exp Allergy. 1996;26(9):1051–1056. doi: 10.1111/j.1365-2222.1996.tb00643.x. [DOI] [PubMed] [Google Scholar]
- 80.Niven R, Fletcher AM, Pickering AC, et al. Attempting to control mite allergens with mechanical ventilation and dehumidification in British houses. J Allergy Clin Immunol. 1999;103(5 Pt 1):756–762. doi: 10.1016/s0091-6749(99)70416-1. [DOI] [PubMed] [Google Scholar]
- 81.Crane J, Ellis I, Siebers R, et al. A pilot study of the effect of mechanical ventilation and heat exchange on house-dust mites and Der p 1 in New Zealand homes. Allergy. 1998;53(8):755–762. doi: 10.1111/j.1398-9995.1998.tb03971.x. [DOI] [PubMed] [Google Scholar]
- 82.Sandel M, Baeder A, Bradman A, Hughes J, Mitchell C, Shaughnessy R, Takaro TK, Jacobs DE. Housing Interventions and Control of Health-Related Chemical Agents: A Review of the Evidence. A Review of the Evidence. J Public Health Manag Pract. 2010;x(x):xxx–xxx. doi: 10.1097/PHH.0b013e3181e3cc2a. [DOI] [PubMed] [Google Scholar]
- 83.Tohn ER, Dixon SL, Wilson JW, Galke WA, Clark CS. An evaluation of onetime professional cleaning in homes with lead-based paint hazards. Appl Occup Environ Hyg. 2003;18(2):138–143. doi: 10.1080/10473220301437. [DOI] [PubMed] [Google Scholar]
- 84.Arbes SJ, Jr, Sever M, Mehta J, et al. Abatement of cockroach allergens (Bla g 1 and Bla g 2) in low-income, urban housing: month 12 continuation results. J Allergy Clin Immunol. 2004;113(1):109–114. doi: 10.1016/j.jaci.2003.10.042. [DOI] [PubMed] [Google Scholar]
- 85.Trasande L, Thurston GD. The role of air pollution in asthma and other pediatric morbidities. J Allergy Clin Immunol. 2005;115(4):689–699. doi: 10.1016/j.jaci.2005.01.056. [DOI] [PubMed] [Google Scholar]
- 86.Terreehorst I, Hak E, Oosting AJ, et al. Evaluation of impermeable covers for bedding in patients with allergic rhinitis. N Engl J Med. 2003;349(3):237–246. doi: 10.1056/NEJMoa023171. [DOI] [PubMed] [Google Scholar]
- 87.Woodcock A, Forster L, Matthews E, et al. Control of exposure to mite allergen and allergen-impermeable bed covers for adults with asthma. N Engl J Med. 2003;349(3):225–236. doi: 10.1056/NEJMoa023175. [DOI] [PubMed] [Google Scholar]
- 88.van den Bemt L, van Knapen L, de Vries MP, et al. Clinical effectiveness of a mite allergen-impermeable bed-covering system in asthmatic mite-sensitive patients. J Allergy Clin Immunol. 2004;114(4):858–862. doi: 10.1016/j.jaci.2004.05.069. [DOI] [PubMed] [Google Scholar]
- 89.Luczynska C, Tredwell E, Smeeton N, Burney P. A randomized controlled trial of mite allergen-impermeable bed covers in adult mite-sensitized asthmatics. Clin Exp Allergy. 2003;33(12):1648–1653. doi: 10.1111/j.1365-2222.2003.01729.x. [DOI] [PubMed] [Google Scholar]
- 90.Rijssenbeek-Nouwens LHM, Oosting AJ, de Bruin-Weller MS, et al. Clinical evaluation of the effect of anti-allergic mattress covers in patients with moderate to severe asthma and house dust mite allergy: a randomised double blind placebo controlled study. Thorax. 2002;57(9):784–790. doi: 10.1136/thorax.57.9.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Marks GB, Mihrshahi S, Kemp AS, et al. Prevention of asthma during the first 5 years of life: a randomized controlled trial. J Allergy Clin Immunol. 2006;118(1):53–61. doi: 10.1016/j.jaci.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 92.Mihrshahi S, Marks GB, Criss S, et al. Effectiveness of an intervention to reduce house dust mite allergen levels in children’s beds. Allergy. 2003;58(8):784–789. doi: 10.1034/j.1398-9995.2003.00194.x. [DOI] [PubMed] [Google Scholar]
- 93.Woodcock A, Lowe LA, Murray CS, et al. Early life environmental control: effect on symptoms, sensitization, and lung function at age 3 years. Am J Respir Crit Care Med. 2004;170(4):433–439. doi: 10.1164/rccm.200401-083OC. [DOI] [PubMed] [Google Scholar]
- 94.Shapiro GG, Wighton TG, Chinn T, et al. House dust mite avoidance for children with asthma in homes of low-income families. J Allergy Clin Immunol. 1999;103(6):1069–1074. doi: 10.1016/s0091-6749(99)70181-8. [DOI] [PubMed] [Google Scholar]
- 95.Woodfolk JA, Hayden ML, Couture N, Platts-Mills TAE. Chemical treatment of carpets to reduce allergen: comparison of the effects of tannic-acid and other treatments on proteins derived from dust mites and cats. J Allergy Clin Immunol. 1995;96(3):325–333. doi: 10.1016/s0091-6749(95)70051-x. [DOI] [PubMed] [Google Scholar]
- 96.Chew GL, Higgins KM, Milton DK, Burge HA. The effects of carpet fresheners on the behaviour of indoor allergen assays. Clin Exp Allergy. 1999;29:470–477. doi: 10.1046/j.1365-2222.1999.00490.x. [DOI] [PubMed] [Google Scholar]
- 97.Gotzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317(7166):1105–1110. doi: 10.1136/bmj.317.7166.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]