Abstract
Introduction: Secure messages and electronic visits (“e-visits”) through patient portals provide patients with alternatives to face-to-face appointments, telephone contact, letters, and e-mails. Limited information exists on how portal messaging impacts face-to-face visits in primary care. Materials and Methods: We conducted a retrospective cohort study of 2,357 primary care patients who used electronic messaging (both secure messages and e-visits) on a patient portal. Face-to-face appointment frequencies (visits/year) of each patient were calculated before and after the first message in a matched-pairs analysis. We analyzed visit frequencies with and without adjustments for a first message surge in visits, and we examined subgroups of high message utilizers and long-term users. Results: Primary care patients who sent at least one message (secure message or e-visit) had a mean of 2.43 (standard deviation [SD] 2.3) annual face-to-face visits before the first message and 2.47 (SD 2.8) after, a nonsignificant difference (p=0.45). After adjustment for a first message surge in visits, no significant visit frequency differences were observed (mean, 2.35 annual visits per patient both before and after first message; p=0.93). Subgroup analysis also showed no significant change in visit frequency for patients with higher message utilization or for those who had used the messaging feature longer. Conclusions: No significant change in face-to-face visit frequency was observed following implementation of portal messaging. Secure messaging and e-visits through a patient portal may not result in a change of adult primary care face-to-face visits.
Key words: : e-health, information management, primary care, telemedicine
Introduction
The patient portal is a Web service provided by many healthcare providers to allow patients access to their medical records. Patient portal features vary but often include administrative and messaging capabilities in addition to medical record access. For administrative functions, patient portals are used for patient appointment scheduling, updating health-related information prior to a visit, and requesting medication refills. Increasingly, patient portals are used for patients to communicate with their healthcare team.
The Veterans Administration, Partners Health, Kaiser Permanente, the Cleveland Clinic, M.D. Anderson Cancer Center, Vanderbilt, and the Mayo Clinic are examples of U.S. healthcare institutions offering a patient portal.1–7 The portal has been promoted as a way to decrease administrative costs of appointment scheduling and handling of medication refills.8 Patient portal secure messaging is increasingly being viewed as necessary to satisfy patient expectations and to provide a competitive advantage in the move toward accountable care.9
Although patient portal appointment scheduling is expected to reduce administrative costs, the impact of secure messaging on face-to-face visits is not well known. Similarly, providers have expressed reservations about electronic messaging with patients. Forty-six percent of providers expressed concern about using e-mail, and 71% thought that e-mailing to patients would increase workload.10 Fifty-two percent of providers believed that their overall workload would increase because of the patient portal.11 A survey of 43 primary care physicians discovered that none of the providers actually used the patient portal for secure messaging during the first 6 months of implementation.12
Only a few studies have examined the impact of secure messaging on healthcare utilization. A randomized controlled trial of 200 patients and six providers in Norway observed a significant drop in face-to-face visits among patients allowed to interact with providers through secure messaging.13 A larger study at Kaiser Permanente Northwest with over 3,000 patients observed that patient office visits decreased by about 10% after implementation of secure messaging through KP HealthConnect™.14 Another more recent study of a Kaiser Permanente group in Colorado showed a significant increase in patient office visits of 0.7 visits per member per year.15
Our aim was to expand the knowledge base on the potential impact of portal messaging on a primary care practice. We also wanted to examine a subgroup of patients who are high message utilizers to determine whether increased portal communication would be associated with fewer face-to-face visits.
Materials and Methods
Study Overview
We conducted a retrospective cohort study examining the frequency of primary care office visits before and after first use of secure messaging through a patient portal. The cohort comprised all adult primary care patient portal users who also had at least one primary care office visit with a provider within the study time interval. Patients were used as their own control in a matched-pairs analysis. This study was approved by the Mayo Clinic Institutional Review Board.
Practice Setting
The study analyzed data from the Mayo Clinic primary care practice in Rochester, MN, which has 141,000 impaneled patients. Patients are impaneled in one of three primary care practices: Family Medicine (73,000 patients), Primary Care Internal Medicine (46,000), and Community Pediatrics and Adolescent Medicine (22,000). Patient care is provided by 121 staff physicians and 59 midlevel providers.
Patient portal services were available starting April 7, 2010 exclusively to patients impaneled in primary care at Mayo Clinic in Rochester. After August 20, 2011, Mayo patient portal services were available to other Mayo Clinic Rochester patients.
Portal services allowed patients to send a message through the patient portal to their healthcare team as either a secure message or an electronic visit (“e-visit”). A secure message was an unstructured message with free-text subject and body fields like an e-mail. Patients were instructed to use secure messages for ongoing care issues and to use e-visits for new symptoms. The e-visit led patients through a computer-directed interview, resulting in a structured message to the provider with information pertinent to the new symptom. Providers had the option of responding to e-visits asynchronously by text (secure message) or telephone; there was no synchronous video option. The stated expectation given to patients and providers was that the response time for a secure message or e-visit was no more than 24 h (except on weekends).
For Mayo Clinic employees and dependents no fees were charged for primary care office visits or e-visits. Nonemployee patients were charged $39 for an e-visit and typical outpatient fees for face-to-face visits. Secure messages for all primary care patients were no charge and no number limit. Approximately 80% of patients seen for a face-to-face office visit in primary care during the study period had no out-of-pocket expense.
All Mayo Clinic primary care providers are salaried. Provider compensation is not based on numbers of patient encounters by office visits, e-visits, or secure messages.
Study Population and Office Visit Capture
We examined all primary care patients who generated a secure message or e-visit from April 7, 2010 to August 20, 2011. We excluded those who did not have universal research authorization and those under 18 years of age. We also excluded those acting as surrogates when we could not positively identify the patient by clinic number (surrogates sometimes sent a message about a patient under their own clinic number).
We used the Mayo Clinic appointment scheduling system to obtain all completed primary care visits for the study patients during the time interval from September 1, 2008 through December 31, 2011. From these appointments, we excluded all completed visits that were not face-to-face provider visits. We also excluded patients who did not have at least one face-to-face visit during the study time interval, those who were not registered patients for the complete interval of the study, and those who had moved out of the area by the end of the study. We used billing information to capture overall change in primary care office visit frequency over the course of the study.
Appointment Frequency Analysis
Index dates were created corresponding to the date when each patient first sent a secure message. This created two intervals for each patient: an interval from the start of appointment capture (September 1, 2008) to the date of his or her first message and an interval from the date of the first message to the end of appointment capture (January 1, 2012). We divided each patient's visit counts by the days in each interval and multiplied by 365.25 to get the annual visit frequencies of each patient before and after their first message. Each patient served as his or her own control, so that each patient's yearly appointment frequency before the first portal message could be matched with the same patient's appointment frequency after the message. To ensure sufficient follow-up, we captured visit data for at least 4 months following the message (i.e., last message included was on August 19, 2011, and the last appointment included was December 31, 2011).
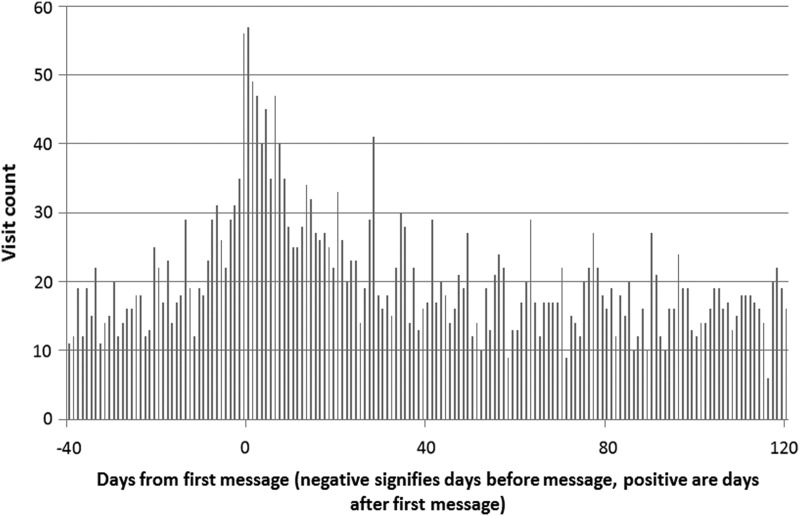
A surge of visits was observed around the time of the first message (Fig. 1). Because the first message could be symptom-related, a visit to evaluate the symptom could be an appropriate response but could also result in more frequent appointments due to a new illness. To adjust for this, we conducted a separate analysis excluding the surge visits (exclusion of visits occurring within 30 days before or after the first message). This adjustment was consistent with those made in previous studies.14,15
Fig. 1.
Visit count by days from first message (n=2,357 patients).
Subgroup Capture
Specific subgroups of interest were those in the highest decile of message use (seven or more messages sent) and those whose visits we could capture for at least 1 year after the first message. A 1-year follow-up group was used to examine whether longer patient exposure to secure messages and e-visits would result in lower face-to-face visits. We hypothesized that a longer exposure time to this new mode of access might be needed for patients to get comfortable substituting messages and e-visits for face-to-face visits. We also examined specific demographic subgroups, and we used the Charlson index (Deyo derivation) to examine appointment frequency change associated with patients having comorbidities.16,17
Statistical Analysis
We used JMP version 9.01 software (SAS Institute, Cary, NC) for all statistical tests. For comparison of demographic variables we used the two-sample test for proportions; we used the matched-pair t test to test the significance of differences in appointment frequency before and after the first message. The Cochran Armitage trend test was used to examine the overall trend in visits per impaneled patient for 2009, 2010, and 2011.
Results
After exclusions (154 patients without study authorization and 202 pediatric/surrogate), we had 2,668 adult patients who sent at least one portal message; 2,543 (94%) had at least one face-to-face visit with a provider from September 2008 through December 2011. After further exclusion of patients coming in and leaving the practice, we had a final study population of 2,357 who accounted for 18,997 visits and 7,229 portal messages (6,317 secure messages and 912 e-visits).
The mean yearly visit frequency for all included patients over the entire study interval was 2.42 (standard deviation [SD] 2.09; range, 0.3–35) with a median of 1.8. There was a median of 2 portal messages per patient with a mean of 3.07 messages per patient (SD 4.4; range, 1–86).
A majority of the patients sending messages were female, were white, lived locally, and were employed by the Mayo Clinic (Table 1). The message-sending population was different in several demographic characteristics from our adult primary care practice, which is 54% female (74% in the study population), 50% Mayo Clinic employees or dependents (75% for the study population), and 19% 65 years of age or over (8.7% for the study population). There were some instances of very high message use, with 103 patients (4.4%) who sent 10 or more messages and 23 (1%) who sent 20 or more messages; 16% of the patients sent 5 or more messages (Table 1). The long-term users (those with follow-up intervals over 1 year) were not significantly different from the whole group except for use of the e-visit and total messages sent (Table 1).
Table 1.
Demographics for All Patient Portal Message Users (Follow-Up Available for More Than 4 Months) Compared with the Subgroup of Long-Term Users (Follow-Up Available for Over 1 Year)
| PERCENTAGE (COUNT) | |||
|---|---|---|---|
| PATIENT PORTAL MESSAGE USER GROUP | ALL PATIENTS, FOLLOW-UP GREATER THAN 4 MONTHS (N=2,357) | LONG-TERM USER SUBGROUP, FOLLOW-UP GREATER THAN 1 YEAR (N=1,219) | P VALUEa |
| Age (years) | |||
| 18–34 | 24.8 (585) | 24.9 (303) | 0.99 |
| 35–45 | 21.6 (510) | 22.9 (279) | 0.40 |
| 46–64 | 44.8 (1,057) | 44.4 (541) | 0.80 |
| 65 and over | 8.7 (205) | 7.9 (96) | 0.41 |
| Female | 74.3 (1,752) | 75.0 (914) | 0.69 |
| White | 95.3 (2,246) | 95 (1,158) | 0.68 |
| Mayo employee | 75 (1,768) | 78.1 (952) | 0.04 |
| Resident local county | 83.8 (1,974) | 83.2 (1,014) | 0.67 |
| e-Visit used | 25.2 (594) | 30.1 (367) | 0.002 |
| Message count 5 or more | 17.1 (402) | 23.7 (289) | <0.0001 |
| Charlson index 1 or more | 41.5 (977) | 40.9 (498) | 0.75 |
Two-sample test for proportions.
e-visit, electronic visit.
Our primary care patient population was relatively stable over the course of the study. Total impaneled primary care patients for 2009, 2010, and 2011 were 135,502, 136,685, and 141,543, respectively, with total visits for the same years of 267,645, 256,505, and 264,294. There was an overall slightly decreasing trend in annual visits per patient, going from 1.97 visits/year in 2009 to 1.87 visits/year in 2011 (p<0.0001).
Figure 1 demonstrates a surge in visits right before and after the first message. Visually, Figure 1 suggests there may be increased visits beyond the 30-day adjustment that we used. However, by the time the follow-up reached at least 4 months (the whole study group) there was no significant difference in the 30-day adjusted visit frequency (2.35 visits/year before and 2.35 after portal messaging, p=0.93). For the subgroup with at least 1 year of follow-up there was an adjusted nonsignificant decrease of 0.1 visits/year (2.44 visits/year before the first message and 2.34 after, p=0.14). For the entire 2,357 patient cohort, the unadjusted mean appointment frequency was 2.43 before the first portal message and 2.47 after (p=0.45). The unadjusted median appointment frequency was 1.81 before and 1.76 after the first portal message.
An increase in visits was observed for those with follow-up for less than 1 year (p=0.03) and younger patients (p=0.02). The differences with p values<0.05 only occurred when not adjusted for the first message visit surge. When adjusted for the first message visit surge there were no groups showing a difference with a p value<0.05. Using a conservative Bonferroni adjustment for multiple subgroup analysis (p<0.005), no subgroups attained statistically significance differences in visit frequencies whether adjusted for first message surge or not.
Discussion
Patients who used portal messages (either secure messages or e-visits) did not significantly change their frequency of face-to-face visits. Important patient subgroups also showed no significant change in office visit frequency. Patients sending the most messages had higher numbers of face-to-face visits both before and after implementation of messaging, but the frequency of their visits did not change. Patients who had at least one e-visit also had no change in visit frequency. Although patients with comorbid conditions (Charlson index 1 or more) might seem a likely group to decrease visits through portal messaging, they also did not change their face-to-face visit frequency. Longer time of portal message familiarity and use was also not associated with a significant change in appointment frequency.
In summary, users with increased message use, longer use, or more comorbidity did not have a significant change in visit frequency after use of portal messages. To our knowledge this is the first study to examine visit frequency in high message users, those with e-visits, and those with longer messaging experience.
Our study does not confirm the overall decrease in appointment frequency observed by Zhou et al.14 in the Kaiser Permanente Northwest study or the increase in visits noted in the Kaiser Permanente Colorado study.15 Even after adjustment for the first message surge in visits we did not see a decline or increase in face-to-face visits either overall or in separate subgroups.
We know that office visits are sensitive to several other healthcare system variables, including type of access and copayments, so a direct comparison with either Kaiser Permanente study may not be possible.18,19 However, an advantage of our study is that we had few confounding variables. For example, Mayo Clinic Primary Care had no major changes to benefits or patient access during the course of the study. We also have a practice panel that does not tend to move from state to state, and we excluded those who did. In so doing, we limited the potential distortion of appointment frequencies from patient migration during the 40-month study interval. Another advantage of our study is that Mayo Clinic provider compensation is neutral to office visits. Salaries do not include extra compensation for more face-to-face visits, and there is no incentive to convert e-visits or secure messages to office visits. Similarly, there are no financial or other rewards for responding to messages or for referring or not referring patients to specialists. Employee patients in Mayo Primary Care also have no office visit copayments and no major access barriers to appointments.
A possible explanation for the different outcomes in previous studies is that secure messages and e-visits are not isolated interventions. Secure messaging and e-visits take place in the context of a patient portal, and other features of the portal may impact patient appointments. Portals have varying degrees of administrative functions that could act as major confounders for changes in visit frequencies. For example, portals can greatly decrease the appointment barrier. Portals often come with appointment request features allowing patients anytime anywhere ability to request appointments.8 Portals can also be linked electronically with provider schedules to give patients a way to directly schedule their own appointments or the ability to view their provider appointment openings. With such patient empowerment to appointment access and scheduling, it is not hard to imagine how portals could increase appointment demand. Portals may also assist patients to self-treatment of acute and chronic diseases. We know that many patients search for symptom information on the Internet, and the information they obtain has varying degrees of pertinent and usable information.20 Portals that connect to well-designed and updated sources of information may drive down office visits by giving patients sufficient online information for self-care. We also know that telephone treatment protocols can decrease office visits.21 Portal implementations that can appropriately direct patients to a treatment protocol may also decrease appointment demand. Some portals are programmed to actively encourage patient appointments. The Mayo Clinic is now using its patient portal to automatically send patient reminders for preventive services such as Pap tests and mammograms. Pap tests require an office visit, and mammograms may generate demand for further follow-up care. Although this portal reminder process did not occur during our study period, it demonstrates the growing complexity of portal influences on office visits. Portal features are rapidly evolving and expanding in scope and numbers. It will be increasingly difficult to identify individual portal features such as secure messages and e-visits as isolated drivers of utilization.
Characteristics of the provider response to messages also need to be examined for their influence on visit utilization. In this study we looked at the impact of long and short message response times. We thought that patients who did not get a provider response in 24 h might be more likely to switch to a face-to-face appointment. We found, however, that only 17% of patients had a median message response time of over 24 h, and they had no significant increase in appointment frequency (Table 2). Those patients with a short median message response time (4 h or less) also did not show a change in appointment frequency. We also observed that some providers had jargon-rich responses, whereas others could be very terse. Certain styles of provider responses probably do not satisfy patients' information needs and could increase office visits. Further study is needed to determine best practices for providers when responding to portal messages.
Table 2.
Face-to-Face Visit Frequencies Before and After Date of First Portal Message With and Without Adjustment for First Message Visit Surge (N=2,357)
| VISIT FREQUENCY (VISITS/YEAR) WITH/WITHOUT ADJUSTMENT FOR FIRST MESSAGE VISIT SURGE | |||||||
|---|---|---|---|---|---|---|---|
| NOT ADJUSTED | ADJUSTED | ||||||
| PATIENT PORTAL MESSAGE USER GROUP | PATIENT [% (n)] | BEFORE | AFTER | P VALUEa | BEFORE | AFTER | P VALUEa |
| All | 100 (2,357) | 2.43 | 2.47 | 0.45 | 2.35 | 2.35 | 0.93 |
| Female | 74.3 (1,752) | 2.54 | 2.58 | 0.48 | 2.46 | 2.48 | 0.71 |
| Male | 25.7 (605) | 2.12 | 2.14 | 0.79 | 2.03 | 1.98 | 0.54 |
| Resides out of county | 16.2 (383) | 2.42 | 2.27 | 0.18 | 2.34 | 2.13 | 0.08 |
| Age under 45 years | 46.5 (1,095) | 2.47 | 2.67 | 0.02 | 2.39 | 2.56 | 0.07 |
| Mayo employee | 75 (1,768) | 2.39 | 2.46 | 0.25 | 2.32 | 2.35 | 0.71 |
| Not Mayo employee | 25 (589) | 2.55 | 2.50 | 0.65 | 2.42 | 2.37 | 0.66 |
| Long-term user (follow up over 1 year) | 51.7 (1,219) | 2.52 | 2.42 | 0.12 | 2.44 | 2.34 | 0.14 |
| Short-term user (follow up less than 1 year | 48.3 (1,138) | 2.33 | 2.53 | 0.03 | 2.25 | 2.36 | 0.20 |
| At least 1 e-visit | 25.2 (594) | 2.67 | 2.87 | 0.12 | 2.66 | 2.69 | 0.81 |
| Secure messages only | 74.8 (1,763) | 2.35 | 2.34 | 0.86 | 2.24 | 2.24 | 0.95 |
| 7 or more messages sent | 8.7 (205) | 3.86 | 3.99 | 0.64 | 3.77 | 3.83 | 0.84 |
| Charlson index 1 or more | 41.5 (977) | 3.07 | 3.02 | 0.59 | 2.98 | 2.91 | 0.50 |
| Message response time to patient was over 24 hb | 16.8 (396) | 2.27 | 2.28 | 0.91 | 2.19 | 2.22 | 0.83 |
| Message response to patient was 4 h or lessb | 47.1 (1,109) | 2.49 | 2.55 | 0.47 | 2.42 | 2.44 | 0.80 |
Matched-pairs t test.
Median of all message responses to that patient.
e-visit, electronic visit.
We did not measure provider burden or the impact of messaging on the whole medical system. For example, we did not measure other workload factors such as a reduction in telephone calls that could counterbalance increased provider workload from answering messages. We also did not measure referrals to the emergency department or to specialists. If messages and subsequent office visits supplanted more costly and inappropriate emergency department visits or specialist referrals, then a secure message or e-visit could have a desirable outcome even without a reduction in face-to-face primary care visits. Further research will be needed to understand how messaging might influence specialist referrals, emergency department visits, and other components of healthcare utilization.
Compared with face-to-face visits, portal messages are limited in the amount and type of information obtained from the patient. During a face-to-face visit a clinician can reconcile patient histories with physical exam findings and pick up nonverbal clues with sight and sound not available in a secure message or e-visit. In addition, the back-and-forth dialog of a face-to-face visit also allows for assessment of symptoms through an algorithmic approach, which the clinician can expertly guide and is difficult to replicate even in the multibranching logic of a structured e-visit. It may take patients and providers some time to gain sufficient experience and confidence to know when to substitute a portal message or e-visit for an office visit. Our study could not conclusively demonstrate that longer experience with messaging was associated with a change in appointment frequency, but the nonsignificant decrease in visits after 1 year of use deserves further study.
Patients with high message use were of particular interest. Nine percent of the patients sending messages accounted for 36% of the total messages. We postulated this message traffic from high users might fulfill a need, such as reassurance or additional information that would decrease the need for a face-to-face visit. However, patients with the highest message counts still had high appointment frequencies both before and after messaging. More research will need to be done to determine whether high message use is delivering value or contributes little more than noise.
Patients with chronic diseases (Charlson index of 1 or more) might be expected to reduce their utilization of face-to-face visits by the use of secure messages. For example, follow-up visits for blood pressure or diabetes might be handled by a secure message. Patients could transmit self-monitored blood pressure and glucose readings back to the providers by secure messages. In essence, patients and providers could use portal secure messages as a telemonitoring platform. We did find some examples of patients using secure messages for blood pressure telemonitoring. However, this “portal telemonitoring” was not supported by specific templates for transmission of blood pressure or glucose data and had no associated information technology support to enter the patient-generated data into the medical record. Even though our findings did not show a significant reduction in visits for those with chronic disease (Charlson index 1 or over), we think there is a potential for significant reduction in face-to-face visits in the future. Secure messages could incorporate specific templates to encourage portal telemonitoring of patient self-reported measures such as glucose, blood pressure, peak flows, asthma, and mood questionnaires. Follow-up visits for hypertension, diabetes, asthma, and depression could be done virtually through portal secure messages and templates for patient self-reported data. Future research will be needed to determine if portal telemonitoring can decrease face-to-face visits for chronic disease management.
Our study had limitations. Although a randomized controlled trial would have had some advantages, it was not a feasible design in an environment where benefits of the patient portal were being actively promoted to all patients. Lacking a concurrent control, we did calculate our overall patient appointment frequency over the duration of the study. There was a slight but statistically significant decrease in visit frequency for all impaneled patients for the study period 2009–2011. This, however, strengthens our findings because the visit frequencies of patients sending messages do not mirror the overall trend. Our patient population is also not very diverse. The users of portal messaging were mostly white and were predominantly employees of the Mayo Clinic. Being able to use patients as their own controls was an advantage. However, a message may be a marker for new illness or symptom requiring a face-to-face visit. We saw evidence for this in the surge in visits after the first message. A short-term increase in post-message appointment frequency may be inevitable and appropriate medical practice. Although we tried to adjust for this by excluding the visits during the time frame of the post-message visit surge, a persistent illness could have required continued visits beyond the time frame we chose to exclude. Also, like the study by Zhou et al.,14 we had an active recruitment process for portal registration during office visits.7 This could have preferentially given more patients at the beginning of a chronic illness access to the patient portal and may have increased post-message appointment frequency.
The impact of portal messages on face-to-face visits is still not settled. Previous studies have demonstrated both significant decreases as well as increases in face-to-face visits following implementation of portal messaging. We found no change in office visit frequency, even with multiple subgroup analyses. Portal messaging is not an isolated intervention. In practice, it is within a much broader context of healthcare access including telephone calls, e-mails, urgent care visits, emergency department visits, office visits, and specialty referrals. Differences in payment, fees, waiting time, travel time, parking, ease of making appointments, and other portal features may alter which form of access is preferred for a specific person, provider, location, and situation. Portal messaging may also depend on the technology available to the patient when the need arises. It is possible that portal messaging may be used in very different ways depending on the healthcare system and the patient population. We should continue to study the effects of this powerful communication tool on healthcare utilization. In the meantime it should not be assumed that portal messaging will change the number of face-to-face visits.
Acknowledgments
The authors thank Kristy Thorson, Susan Claxton, Eric Manley, Barbie Mundt, and Chris Rock for their contributions to this manuscript.
Disclosure Statement
No competing financial interests exist.
References
- 1.Osborn CY, Rosenbloom ST, Stenner SP, et al. MyHealthAtVanderbilt: Policies and procedures governing patient portal functionality. J Am Med Inform Assoc 2011;18:i18–i23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nazi KM. Veterans' voices: Use of the American Customer Satisfaction Index (ACSI) Survey to identify My HealtheVet personal health record users' characteristics, needs, and preferences. J Am Med Inform Assoc 2010;17:203–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wald JS. Variations in patient portal adoption in four primary care practices. AMIA Annu Symp Proc 2010;2010:837–841 Available at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3041333/ (last accessed December10, 2013) [PMC free article] [PubMed] [Google Scholar]
- 4.Miller H, Vandenbosch B, Ivanov D, Black P. Determinants of personal health record use: A large population study at Cleveland Clinic. J Healthc Inf Manag 2007;21:44–48 [PubMed] [Google Scholar]
- 5.Merrill M. Patients, referring docs at MD Anderson making good use of Web portal. Available at www.healthcareitnews.com/news/patients-referring-docs-md-anderson-making-good-use-web-portal (last accessed March31, 2013)
- 6.Roblin DW, Houston TK, Allison JJ, et al. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc 2009;16:683–689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.North F, Hanna BK, Crane SJ, et al. Patient portal doldrums: Does an exam room promotional video during an office visit increase patient portal registrations and portal use? J Am Med Inform Assoc 2011;18:i24–i27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gamble KH. Is it registering? Patient portals, part II (see Financial Department for part I). Healthc Inform 2009;26:24, 26, 28 [PubMed] [Google Scholar]
- 9.Degaspari J. Getting the message, securely. Healthc Inform 2012;29:52, 54, 56 passim [PubMed] [Google Scholar]
- 10.Hobbs J, Wald J, Jagannath YS, et al. Opportunities to enhance patient and physician e-mail contact. Int J Med Inform 2003;70:1–9 [DOI] [PubMed] [Google Scholar]
- 11.Siteman E, Businger A, Gandhi T, et al. Clinicians recognize value of patient review of their electronic health record data. AMIA Annu Symp Proc 2006:1101 Available at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1839374/ (last accessed December10, 2013) [PMC free article] [PubMed]
- 12.Kittler AF, Carlson GL, Harris C, et al. Primary care physician attitudes towards using a secure web-based portal designed to facilitate electronic communication with patients. Inform Primary Care 2004;12:129–138 [DOI] [PubMed] [Google Scholar]
- 13.Bergmo TS, Kummervold PE, Gammon D, Dahl LB. Electronic patient–provider communication: Will it offset office visits and telephone consultations in primary care? Int J Med Inform 2005;74:705–710 [DOI] [PubMed] [Google Scholar]
- 14.Zhou YY, Garrido T, Chin HL, et al. Patient access to an electronic health record with secure messaging: Impact on primary care utilization. Am J Manag Care 2007;13:418–424 [PubMed] [Google Scholar]
- 15.Palen TE, Ross C, Powers JD, Xu S. Association of online patient access to clinicians and medical records with use of clinical services. JAMA 2012;308:2012–2019 [DOI] [PubMed] [Google Scholar]
- 16.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40:373–383 [DOI] [PubMed] [Google Scholar]
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613–619 [DOI] [PubMed] [Google Scholar]
- 18.Sen B, Blackburn J, Morrisey MA, et al. Did copayment changes reduce health service utilization among CHIP enrollees? Evidence from Alabama. Health Serv Res 2012;47:1603–1620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Hare CD, Corlett J. The outcomes of open-access scheduling. Fam Pract Manag 2004;11:35–38 [PubMed] [Google Scholar]
- 20.North F, Ward WJ, Varkey P, Tulledge-Scheitel SM. Should you search the Internet for information about your acute symptom? Telemed J E Health 2012;18:213–218 [DOI] [PubMed] [Google Scholar]
- 21.North F, Varkey P, Bartel GA, et al. Can an office practice telephonic response meet the needs of a pandemic? Telemed J E Health 2010;16:1012–1016 [DOI] [PubMed] [Google Scholar]