Abstract
Objective
Attention for recurrent preterm delivery has primarily focused on spontaneous subtypes with less known about indicated preterm delivery.
Study Design
In a retrospective cohort of consecutive pregnancies among 51,086 women in Utah (2002–2010), binary relative risk regression was performed to examine risk of preterm delivery < 37 weeks (PTD) in the second observed delivery by PTD in the first, adjusting for maternal age, race/ethnicity, prepregnancy body mass index, insurance, smoking, alcohol and/or drug use, and chronic disease. Analyses were also performed stratified by prior preterm delivery subtype: spontaneous, indicated, or no recorded indication.
Results
There were 3,836 (7.6%) women that delivered preterm in the first observed pregnancy, of which 1,160 (30.7%) repeated in the second. Rate of recurrent PTD was 31.6% for prior spontaneous, 23.0% for prior indicated delivery, and 27.4% for prior elective delivery. Prior spontaneous PTD was associated with RR 5.64 (95% CI 5.27–6.05) of subsequent spontaneous and RR 1.61 (95% CI 0.98–2.67) of subsequent indicated PTD. Prior indicated PTD was associated with RR 9.10 (95% CI 4.68–17.71) of subsequent indicated and RR 2.70 (2.00–3.65) of subsequent spontaneous PTD.
Conclusions
Prior indicated PTD was strongly associated with subsequent indicated PTD and with increased risk for subsequent spontaneous PTD. Spontaneous PTD had the highest rate of recurrence. Some common pathways for different etiologies of preterm delivery are likely, and indicated PTD merits additional attention for recurrence risk.
Keywords: recurrent preterm birth, indicated preterm birth, spontaneous preterm birth
INTRODUCTION
Pregnancy complications and adverse pregnancy outcomes often recur in subsequent pregnancies.1 Preterm delivery before 37 weeks of gestation is one common adverse outcome that repeats, where women with a history have a 22% risk of preterm birth in a following pregnancy compared to 9% risk in women without a history of prior preterm delivery.2 Yet even though women with a history of preterm birth have a 2.5-fold increase in spontaneous preterm delivery in the next pregnancy, the vast majority of women will still deliver at term.2 The tendency to recur increases with the number of prior preterm deliveries, earlier gestational age at prior delivery, and the order, with higher risk of subsequent preterm delivery if the immediately preceding birth was preterm.3 Yet our understanding of recurrence risk has primarily focused on spontaneous preterm deliveries or has not taken subtype into consideration.2, 4–9
Indicated preterm birth has been found to confer an increased risk for preterm delivery in subsequent pregnancies in one10 but not all studies.11–13 However, three of these studies relied on birth certificate data or birth registries which are subject to misclassification of preterm birth subtype (e.g. spontaneous versus indicated) and lacked detailed information on important risk factors10, 11, 13. One study from a single institution investigated recurrent preterm birth < 35 weeks of gestation.12 These findings might not be relevant for all preterm births, since most occur between 34 and 37 weeks.14 In addition, while gestational age at birth is known to be inversely related to risk of subsequent preterm delivery, with earlier gestational ages associated with higher risk in the next pregnancy, it is unknown whether we can predict not only if but when a complication would recur, and whether prior preterm birth subtype modifies the relationship. To address these critical data gaps, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) performed a large retrospective cohort study with consecutive pregnancies.
MATERIALS AND METHODS
The NICHD Consecutive Pregnancies Study collected detailed data on 114,679 pregnancies from 51,086 women delivering ≥20 weeks of gestation from 20 hospitals in the state of Utah from 2002 to 2010. Internal review board approval was obtained at all participating institutions. All women contributed at least two deliveries and births were consecutive across pregnancies based on increases in parity. However, 7,712 women (15.1%) had a pregnancy loss prior to 20 weeks of gestation indicated by an increase in gravidity more than parity between pregnancies. Hospitals extracted detailed information from both the antepartum and labor and delivery summary electronic medical records. Patient demographics, past medical history, reproductive and prenatal history, pregnancy, labor and delivery outcomes, postpartum and neonatal information were mapped to predefined categories at the data coordinating center. The type of information available was as would be expected in typical clinical practice although information on who (e.g. nurse versus physician) entered data into the patient chart was not collected. For example prenatal record included past medical history (e.g. chronic hypertension, pregestational diabetes) and pregnancy complications (e.g. gestational hypertension, preeclampsia, eclampsia, premature rupture of the membranes, intrauterine fetal growth restriction, etc.). Labor and delivery records included date and time of admission, cervical exam on admission, repeated cervical exams during labor, labor and delivery characteristics (oxytocin, fetal presentation, etc.) indications for induction (e.g. fetal indication, maternal hypertensive disorder, premature rupture of membranes, postdate, etc.), indications for cesarean (e.g. fetal malpresentation, prior cesarean, non-reassuring fetal heart tones, etc.). Newborn records were linked to the neonatal intensive care unit (NICU) records. International Classification of Diseases-9 (ICD9) codes from maternal and newborn discharge summaries were linked to each delivery.
Potential clinical predictors of preterm birth were identified as summarized in the Institute of Medicine of the National Academies 2007 report from the Committee on Understanding Premature Birth and Assuring Healthy Outcomes.15 Three models with different sets of predictors were performed with the first including maternal characteristics of age, race/ethnicity, prepregnancy body mass index (BMI), insurance; smoking, alcohol or drug use during pregnancy as recorded in the prenatal record (yes/no), and chronic diseases including diabetes, chronic hypertension, heart disease, renal disease, depression, seizure disorder, thyroid disease, and asthma. Chronic medical conditions were as recorded in the medical record and supplemented with discharge summary data using ICD9 codes. The second model included the above maternal characteristics as well as prior reproductive history including history of pregnancy loss (including miscarriage and terminations) calculated as gravidity minus parity > 1, history of stillbirth calculated as parity minus history of live birth, interpregnancy interval based on the number of days between the delivery and the last menstrual period of a subsequent pregnancy, and history of small for gestational age [birth weight < 10th percentile]. A final model included all of the above maternal characteristics and prior reproductive history as well as pregnancy complications including genitourinary bacterial infection during pregnancy (sexual transmitted disease or urinary tract infection), vaginal bleeding, placenta previa or accreta, and uterine anomaly as identified by ICD-9 codes [752.2, Doubling of uterus (didelphic uterus) or 752.3, Other anomalies of uterus (Bicornuate, unicornis, uterus with only one functioning horn)].
Categories of preterm birth subtypes were created using the following algorithm previously published by our group16: Induction or prelabor cesarean delivery recorded in the medical record was used to identify the non-spontaneous precursors for delivery. A woman was considered to have presented in spontaneous labor if she did not have an induction or prelabor cesarean delivery. Women with spontaneous labor and other pregnancy complications (e.g. preeclampsia) were included only in the spontaneous preterm delivery category. Women with premature rupture of the membranes and not in labor were included as preterm premature rupture of membranes (PPROM). If a women presented with both PPROM and in spontaneous labor she was counted only once in the spontaneous labor category. The results for analyses of spontaneous labor and PPROM were similar, so we elected to combine these categories due to the small numbers in certain analyses. If a woman did not present in spontaneous labor or with PPROM, we then identified all potential maternal, fetal or obstetrical complications of pregnancy, and included these in the indicated category. The rationale for including all complications was if a woman had an induction or prelabor cesarean without an indication listed, and the pregnancy had a complication (e.g. preeclampsia), we wanted to be conservative and assume that the most likely reason for delivery was preeclampsia rather than classify as a medically unnecessary delivery. The final category included labor inductions or cesarean deliveries recorded as “elective” by the site with no other obstetrical, fetal or maternal conditions, as well those deliveries with no recorded indication.
The analysis was restricted to singleton pregnancies. Maternal characteristics upon entry to the cohort and pregnancy characteristics by delivery were summarized. The remaining analyses were limited to the first two or three pregnancies in the dataset. A scatterplot was created of gestational age for the first delivery versus gestational age for the second delivery with a loess smooth curve overlaid. Binary relative risk regression (binary regression with a log-link function) was performed to calculate relative risk (RR) and 95% confidence intervals (CI) of preterm birth in the second observed delivery for category of gestational age for the first observed delivery. Since all women in the dataset had at least two pregnancies by design, risk for women with more or fewer pregnancies could have been different to the extent that their measured and unmeasured characteristics varied. Therefore, a sensitivity analysis was performed limiting the analysis to women who contributed at least three pregnancies to the dataset. Relative risk regression was performed to examine the risk of preterm birth in the third delivery by preterm birth in the first and second deliveries. We also fit models with an interaction term to examine the interaction of preterm birth in the first and second delivery on the occurrence of preterm in the third delivery. The models with interaction terms were adjusted for the same covariates as mentioned above for the additive model. Cumulative incidence curves were estimated by prior delivery timing (20 to <24, 24 to <28, 28 to <34, 34 to <37, and >=37 weeks of gestation) using Kaplan-Meier estimation. The incidence curves were presented for the gestational age in the second delivery by categories of gestational age in the first delivery.
RESULTS
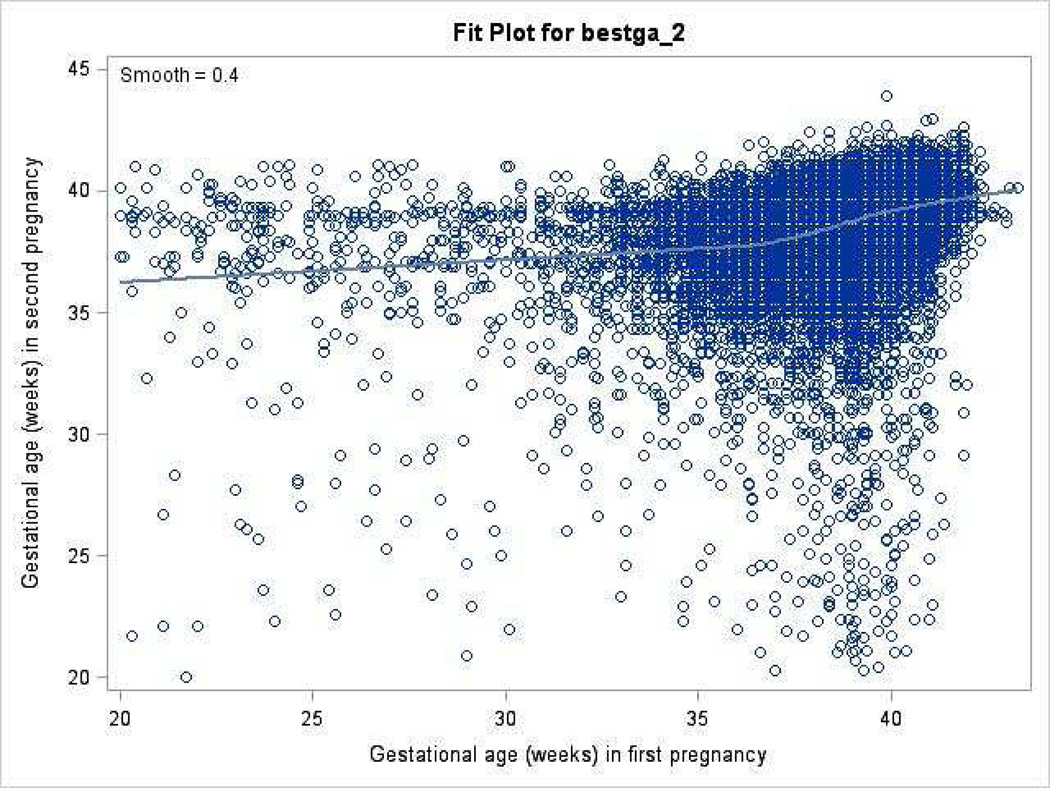
There were 51,066 women with a total of 114,639 singleton pregnancies. Maternal characteristics upon entry to the cohort study and pregnancy characteristics by delivery are presented in Table 1. The majority of women (39,954, 78.2%) contributed only two pregnancies, an additional 9,792 (19.2%) contributed three pregnancies, and 1,320 women contributed 4 or more pregnancies (2.6%). There were 3,836 (7.6%) women that delivered preterm in the first pregnancy, of which 1,160 (30.7%) repeated in the second. The timing of delivery in the first delivery was correlated with timing of delivery in the subsequent pregnancy; however, there was substantial variation (Figure 1).
Table 1.
Maternal characteristics upon entry to cohort study and pregnancy characteristics by delivery.
| Characteristic | No. (%) of Womena N=51066 |
|---|---|
| Age, mean (SD), y | 25.6 (4.5) |
| < 18, y | 1093 (2.1) |
| 18 – 34, y | 48099 (94.2) |
| ≥ 35, y | 1874 (3.7) |
| Body mass index, mean (SD)b | 24.3 (5.3) |
| Race-ethnicity | |
| Non-Hispanic White | 44054 (86.3) |
| Non-Hispanic Black | 223 (0.4) |
| Hispanic | 5431 (10.6) |
| Asian/Pacific Islander | 1088 (2.1) |
| Other/Unknown | 270 (0.5) |
| Marital status | |
| Married | 44032 (86.2) |
| Divorced/widowed | 692 (1.4) |
| Single | 6333 (12.4) |
| Unknown | 9 (0.02) |
| Insurance Status | |
| Private | 37370 (73.8) |
| Public | 13237 (26.2) |
| Gravidity, median (range) | 2 (1–24) |
| Parity, median (range) | 0 (0–14) |
| 0 | 27730 (59.5) |
| 1 | 11704 (25.1) |
| 2+ | 7147 (15.3) |
| Smoker | 1253 (2.5) |
| Alcohol use | 871 (1.7) |
| Illicit drug use | 103 (0.2) |
| Chronic medical disease | 8427 (16.5) |
| Pregestational diabetes | 606 (1.2) |
| Chronic hypertension | 277 (0.5) |
| Uterine anomaly | 116 (0.2) |
| Genitourinary bacterial infection | |
| Sexual transmitted disease | 540 (1.1) |
| Urinary tract infection | 1369 (2.7) |
| Vaginal bleeding | 504 (1.0) |
| Interpregnancy interval, median (range), days | 562 (15, 2410) |
| Prior adverse pregnancy outcomec | |
| Miscarriage or termination | 10817 (21.2) |
| Preterm birth | 2019 (4.0) |
| Number of pregnancies | |
| 2 | 39954 (78.2) |
| 3 | 9792 (19.2) |
| 4 | 1247 (2.4) |
| 5 | 71 (0.1) |
| 6 | 2 (0.0) |
Y, years; SD, standard deviation; GI, gastrointestinal; HIV, human immunodeficiency virus
Unless otherwise indicated
Calculated as weight in kilograms divided by height in meters squared.
Prior outcome only for deliveries where gravidity > 1. Miscarriage or termination calculated as yes if gravidity-parity>1 (could include neonatal deaths, still births, abortions, and miscarriages).
Figure 1.
Gestational age at delivery in the second delivery by gestational age in the first delivery for all women.
Circles in the scatterplot represent each gestational age (weeks) of delivery with Loess smooth line.
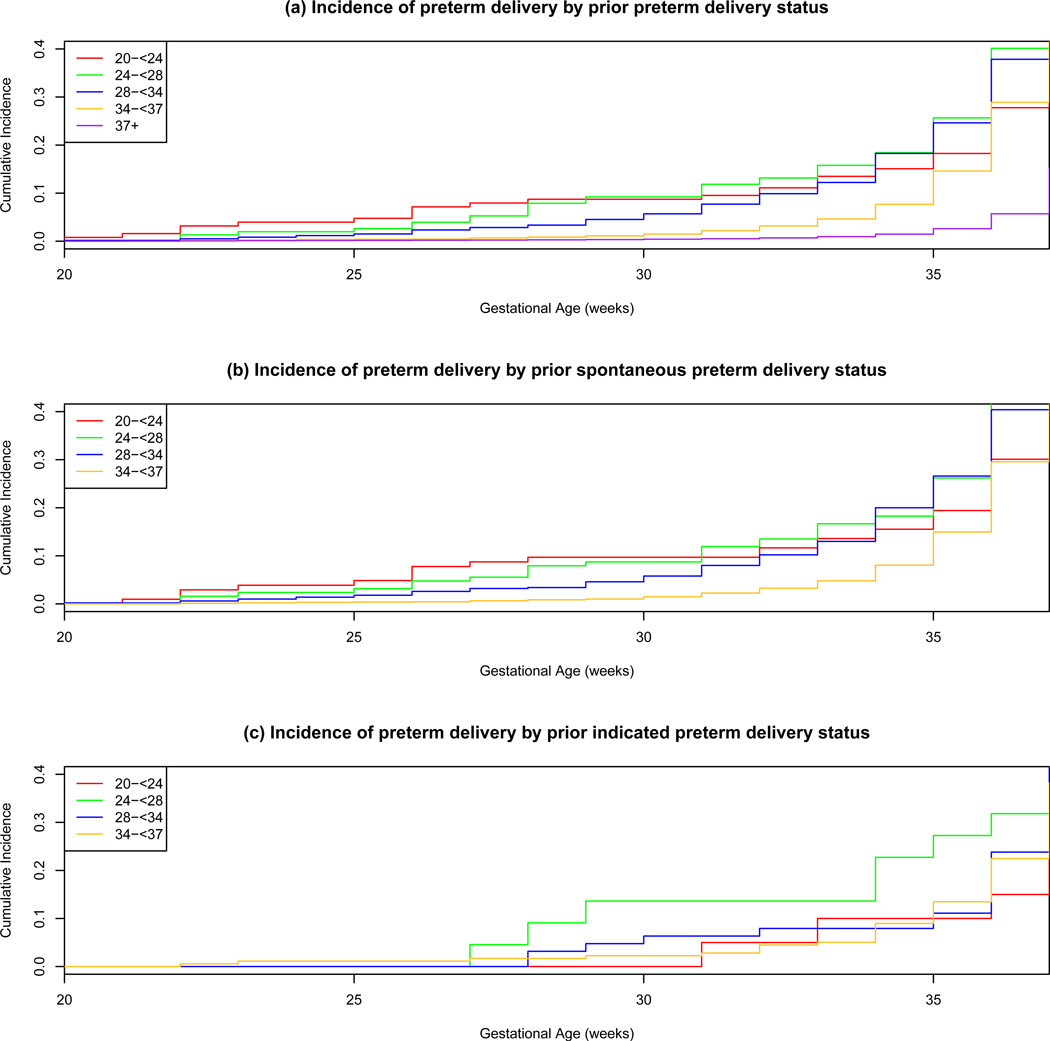
The earlier the gestational age of the first delivery, the higher the risk of preterm birth < 37 weeks of gestation in the subsequent delivery, where the trend for gestational age was highly significant P<.0001 (Table 2). However, while the highest risk for subsequent preterm birth < 37 weeks was with a prior preterm birth at 24 to 27 weeks of gestation (RR, 7.03, 95% CI 5.77–8.57), the RR were overall high for all prior preterm birth gestational age categories and the confidence intervals overlapped. These findings were supported by the second delivery cumulative incidence curves which were ordered by prior delivery gestational age category until around 28 weeks after which the degree of preterm was not as influential as any history of preterm birth (Figure 2a). However, while the degree of preterm birth was highly associated with future risk, history still was not very predictive of either subsequent preterm birth or subsequent preterm gestational age at delivery. For example, if a woman had a prior preterm delivery at 28 weeks, the cumulative incidence of any preterm delivery < 37 weeks was 37.9% but the incidence of delivery ≤ 28 weeks was only 10.4%. Thus, she still had significant risk of preterm delivery throughout the next pregnancy and there was no gestational age cut-off where the risk was no longer increased.
Table 2.
Risk of preterm birth < 37 weeks of gestation in subsequent delivery by gestational age at first delivery (n=50,607).a
| Preterm birth < 37 weeks in second delivery |
||||
|---|---|---|---|---|
| Gestational age at first delivery, weeks |
Total n (%) |
n (%) preterm in 2nd birth |
Unadjusted RR | Adjusted RRb |
| ≥ 37 | 46771 (92.4) | 2630 (5.7) | Referent | Referent |
| 34 to < 37 | 2950 (5.8) | 838 (28.9) | 5.07 [4.73, 5.42] | 4.81 [4.48, 5.15] |
| 28 to < 34 | 607 (1.2) | 226 (37.9) | 6.63 [5.95, 7.40] | 5.98 [5.37, 6.66] |
| 24 to < 28 | 152 (0.3) | 61 (40.1) | 7.03 [5.77, 8.57] | 6.42 [5.33, 7.74] |
| 20 to < 24 | 127 (0.3) | 35 (27.8) | 4.87 [3.66, 6.47] | 4.88 [3.66, 6.50] |
Trend for gestational age P<.0001.
Figures in parentheses are 95% confidence intervals except where noted
Models were adjusted for maternal age, race/ethnicity, pre-pregnancy body mass index, insurance, smoker, alcohol, illicit drug use, chronic medical disease.
Figure 2.
Incidences of preterm delivery < 37 weeks in the 2nd pregnancy based on timing of preterm delivery in the 1st pregnancy.
Cumulative incidence curves were estimated by prior delivery timing (20 to <24, 24 to <28, 28 to <34, 34 to <37, and >=37 weeks of gestation) using Kaplan-Meier estimation for the following three panels: a. any prior preterm delivery < 37 weeks; b. prior spontaneous preterm delivery < 37 weeks; c. prior indicated preterm delivery < 37 weeks.
Since the number of pregnancies per woman in the study could have resulted in differences in their measured and unmeasured characteristics, a sensitivity analysis limited to women who contributed at least three pregnancies to the dataset was performed. The results of the analyses on this substantially smaller sub-cohort along and the analyses on the first two pregnancies on the full cohort suggest that the underlying recurrence risk was similar regardless of the number of pregnancies that a woman contributed.
After adjusting for clinical characteristics at baseline in pregnancy, the RR for subsequent preterm birth were slightly attenuated but overall the same (Table 2). Further, models that included these maternal characteristics as well as prior obstetrical history including interpregnancy interval, history of miscarriage or termination, history of small for gestational age < 10th percentile, as well as pregnancy complications including genitourinary bacterial infection during pregnancy, vaginal bleeding, placenta previa or accreta, and uterine anomaly had similar results (data not shown). Therefore, most of the risk of preterm delivery was captured by the unadjusted model signifying that prior history of preterm birth was the single most important predictor of subsequent preterm birth < 37 weeks of gestation. In spite of these high relative risks, 60–72% of women still delivered at term in the subsequent pregnancy.
Three Consecutive Pregnancies
The risk of preterm birth < 37 weeks of gestation in the third delivery was over 10-fold higher for women with two prior preterm deliveries compared to women with two prior term deliveries (Table 3). For women with a history of one prior preterm and one prior term delivery, the risk for subsequent preterm birth in the third pregnancy was higher, 5.5-fold versus 3.5-fold, when the preterm birth occurred in the immediate preceding pregnancy compared to a preterm birth in the first pregnancy.
Table 3.
Risk of preterm birth < 37 weeks of gestation in third delivery by term versus preterm birth in first and second deliveries (n=10,819).a
| Total n (%) |
N (%) preterm in 3rd birth |
Unadjusted RR | Adjusted RRb | |
|---|---|---|---|---|
| Term birth in 1st delivery/Term birth in 2nd delivery | 9441 (87.3) | 468 (5.0) | Referent | Referent |
| Preterm birth in 1st delivery/ Term birth in 2nd delivery | 580 (5.4) | 101 (17.4) | 3.51 [2.88, 4.28] | 3.50 [2.86, 4.28] |
| Term birth in 1st delivery/Preterm birth in 2nd delivery | 555 (5.1) | 155 (27.9) | 5.63 [4.80, 6.61] | 5.50 [4.66, 6.50] |
| Preterm birth in 1st delivery/Preterm birth in 2nd delivery | 243 (2.2) | 142 (58.4) | 11.79 [10.27, 13.53] | 10.57 [9.05, 12.34] |
Figures in parentheses are 95% confidence intervals except where noted
Models were adjusted for maternal age, race/ethnicity, pre-pregnancy body mass index, insurance, smoker, alcohol, illicit drug use, chronic medical disease.
Risk of Preterm Birth by Subtype
When investigating subtype of preterm delivery risk, the rate of preterm delivery < 37 weeks by the precursor for preterm delivery in the prior pregnancy was 31.6% for spontaneous delivery (adjusted RR 5.12, 95% CI 4.80–5.47), 23.0% for indicated delivery(adjusted RR 3.89, 95% CI 3.15–4.81), and 27.4% for elective delivery or no recorded indication (adjusted RR 4.55, 95% CI 3.87–5.35). Prior spontaneous preterm delivery was associated with a 5.6-fold increased risk of subsequent spontaneous preterm delivery. (Table 4) However, the strongest association was for a prior indicated delivery and subsequent risk of both indicated preterm delivery (adjusted RR 9.10, 95% CI 4.68–17.71) and elective delivery or no recorded indication (adjusted RR 12.57, 95% CI 7.99–19.79). An indicated delivery in a prior pregnancy still had a significant 2.7-fold increased risk for spontaneous preterm birth in the next pregnancy. A history of prior spontaneous delivery was associated with a slightly lower 1.6-fold increased risk for indicated delivery in a subsequent pregnancy, although the significance was attenuated after adjustment and the numbers were small (n=17). Of note, the number of elective deliveries in the second pregnancy decreased over the study period (P = 0.02 for trend) and also significantly varied in both the first (P = 0.003) and second (P = 0.02) delivery by hospital.
Table 4.
Risk of preterm birth < 37 weeks in the second delivery based on precursors for preterm (<37 weeks) deliveries in the first delivery.
| Preterm Precursor for 2nd Delivery | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Delivery ≥ 37 weeksa Frequency %) |
Spontaneous Delivery < 37 weeks |
Indicated Delivery < 37 weeks |
Elective or no recorded indication Delivery < 37 weeks |
|||||||
| Preterm Precursor for 1st Delivery |
Frequency (%) |
Unadjusted RR (95% CI) |
Adjustedb RR (95% CI) |
Frequency (%) |
Unadjusted RR (95% CI) |
Adjustedb RR (95% CI) |
Frequency (%) |
Unadjusted RR (95% CI) |
Adjustedb RR (95% CI) |
|
| Spontaneous delivery | 2154 (68.6) | 921 (29.3) | 6.04 (5.65–6.47) | 5.64 (5.27–6.05) | 17 (0.5) | 1.66 (1.01–2.73) | 1.61 (0.98–2.67) | 47 (1.5) | 3.08 (2.25–4.20) | 2.86 (2.08–3.92) |
| Indicated delivery | 222 (77.4) | 37 (13.1) | 2.67 (1.97–3.62) | 2.70 (2.00–3.65) | 9 (3.2) | 9.71 (5.01–18.83) | 9.10 (4.68–17.71) | 19 (6.7) | 13.75 (8.74–21.64) | 12.57 (7.99–19.79) |
| Elective or no recorded indication delivery | 300 (73.2) | 78 (19.4) | 3.97 (3.24–4.86) | 3.88 (3.17–4.76) | 4 (1.0) | 3.04 (1.13–8.16) | 2.71 (1.01–7.31) | 28 (7.0) | 14.27 (9.76–20.87) | 11.88 (8.08–17.48) |
Reference = term delivery ≥ 37 weeks of gestation
Adjusted for maternal age, race, pre-pregnancy BMI, insurance, smoking, alcohol, illicit drug use, chronic medical disease
The second delivery cumulative incidence curves differed by prior preterm birth subtype (Figure 2b, 2c). For prior spontaneous preterm birth (Figure 2b), in general the curves were ordered by prior delivery gestational age category until around 31 weeks. Ordering was not observed as readily for the incidence of recurrent preterm birth. In contrast to prior spontaneous preterm birth, the incidence of recurrent preterm birth was only marginally increased with prior indicated preterm births until later around 27 weeks of gestation, and was overall low until 37 weeks.
COMMENT
In this large consecutive pregnancy cohort with detailed maternal and pregnancy information from the patient medical records, recurrence rates were higher for prior spontaneous preterm delivery compared to prior indicated delivery. In addition, the relation between severity of prior preterm birth and subsequent delivery timing as well as risk of recurrent subtype differed by type of prior preterm birth. The degree of prior preterm delivery was more important for prior spontaneous compared to indicated preterm birth, especially for subsequent early preterm delivery prior to 28 weeks of gestation. Prior indicated preterm birth was associated with a relatively later incidence of subsequent preterm birth and was only marginally increased until after 27 weeks of gestation. Both subtypes had the highest risk of recurrence of the same type, with prior spontaneous associated with a 5.6-fold increased risk of subsequent spontaneous delivery and prior indicated associated with a 9.1-fold increased risk of recurrent indicated delivery. Indicated preterm delivery was also associated with subsequent spontaneous preterm birth, and although non-significant, the point estimate for indicated preterm delivery was elevated with prior spontaneous preterm delivery. It is important to note that while the degree of preterm birth was highly associated with future preterm delivery risk and timing, women still remained at risk throughout the preterm period even when they passed the time point of their prior delivery.
Similar to previous studies, prior history of preterm birth was the single most important predictor of subsequent preterm birth < 37 weeks of gestation, with a higher risk for multiple prior preterm births and when the preterm birth occurred in the immediate preceding pregnancy compared to a preterm birth in the first pregnancy.2–7, 11 However, our finding that recurrent preterm birth was higher for prior spontaneous versus indicated preterm delivery differs from prior publications.10, 11 A Danish study11 using birth registry data found the risk of preterm delivery in the second pregnancy to be the same for women regardless of prior spontaneous versus indicated preterm delivery, while a study using Missouri birth certificates10 found a slightly higher risk for prior medically indicated preterm birth although the confidence intervals overlapped (odds ratio for preterm birth < 37 weeks for prior spontaneous preterm birth 2.8, (95% CI 2.7–3.0) and prior medically indicated preterm birth 3.0 (95% CI 2.8–3.3). One explanation for the differences may be that the prior indications for preterm delivery likely had some misclassification since they were derived from administrative data while our study had detailed medical record information. This possibility is supported by the fact that we observed elective preterm deliveries (mostly late preterm), and the study using registries and birth certificates lacked this category resulting in elective preterm deliveries being included in the spontaneous preterm birth category by definition. Our finding that medically indicated delivery had a higher risk of repeating compared to spontaneous was similar to the study by Ananth et al.10 but differed from the findings of the Danish study.11 The reasons for these differences are unclear, but again may be due to the differences in data sources.
In all analyses, adjusting for a number of known risk factors for preterm birth attenuated the risk for recurrent preterm delivery, but prior history of preterm birth regardless of timing, order or subtype, remained the major risk factor. These findings are similar to what has been reported in other studies and suggest that unmeasured factors other than those clinically observed including baseline maternal characteristics, chronic diseases, infections, and bleeding during pregnancy play an important role.7, 11
Our study may be limited by misclassification of some of the deliveries with no recorded indication that were truly medically indicated. However, given the large number of variables on which data were collected, as well as our conservative effort to include all possible conditions, a certain proportion of the deliveries with an unknown precursor were likely elective. This finding is supported by the fact that the percentage of elective deliveries or those with no recorded indication decreased over the study period in parallel with the national focus on decreasing late preterm deliveries without strong indications. In addition, we were unable to determine whether an indication for delivery was truly medically necessary. We also lacked information on some established clinical predictors of preterm delivery, such as cervical length.17 Our study is based on a low risk population of predominantly non-Hispanic white, normal weight, married women, but we still observed the expected pattern of risk factors for subsequent preterm birth. Finally, while our numbers were small for some of the categories, the major strength of our study was the ability to determine recurrent preterm birth risk by subtype given the detailed medical record information.
Prior preterm delivery due to spontaneous versus indicated subtypes both had the highest risk of recurrence for their respective subtype, with prior indicated having the strongest association for recurrent indicated delivery. However, prior indicated was also associated with recurrence of spontaneous preterm delivery, suggesting that there likely are some common pathways for different etiologies for preterm delivery. These findings have potential clinical implications, such as whether progesterone, which has been found to prevent recurrent spontaneous preterm delivery, could also prevent subsequent spontaneous preterm delivery in women with a prior indicated preterm delivery.18 Further strategies are also needed for prevention of recurrent indicated preterm delivery.
Acknowledgments
This research was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, (Contract Numbers HHSN275200800002I, HHSN27500004).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data from the NICHD Consecutive Pregnancies Study were collected in Utah, United States.
Disclosure: The authors report no conflict of interest.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health.
This research was presented as a platform presentation at the Annual Meeting of the Society for Pediatric and Perinatal Epidemiologic Research, Boston, MA, June 17–18, 2013.
Disclaimer: S.K. Laughon, P.S. Albert and P. Mendola are employees of the federal government; please see accompanying cover sheet.
References
- 1.Louis GB, Dukic V, Heagerty PJ, Louis TA, Lynch CD, Ryan LM, et al. Analysis of repeated pregnancy outcomes. Stat Methods Med Res. 2006;15:103–126. doi: 10.1191/0962280206sm434oa. [DOI] [PubMed] [Google Scholar]
- 2.Mercer BM, Goldenberg RL, Moawad AH, Meis PJ, Iams JD, Das AF, et al. The preterm prediction study: effect of gestational age and cause of preterm birth on subsequent obstetric outcome. National Institute of Child Health and Human Development Maternal- Fetal Medicine Units Network. Am J Obstet Gynecol. 1999;181:1216–1221. doi: 10.1016/s0002-9378(99)70111-0. [DOI] [PubMed] [Google Scholar]
- 3.McManemy J, Cooke E, Amon E, Leet T. Recurrence risk for preterm delivery. Am J Obstet Gynecol. 2007;196:576 e1–576 e6. doi: 10.1016/j.ajog.2007.01.039. discussion 76 e6-7. [DOI] [PubMed] [Google Scholar]
- 4.Hobel CJ, Hyvarinen MA, Okada DM, Oh W. Prenatal and intrapartum high-risk screening. I. Prediction of the high-rish neonate. Am J Obstet Gynecol. 1973;117:1–9. doi: 10.1016/0002-9378(73)90720-5. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman HJ, Bakketeig LS. Risk factors associated with the occurrence of preterm birth. Clinical obstetrics and gynecology. 1984;27:539–552. doi: 10.1097/00003081-198409000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Carr-Hill RA, Hall MH. The repetition of spontaneous preterm labour. Br J Obstet Gynaecol. 1985;92:921–928. doi: 10.1111/j.1471-0528.1985.tb03071.x. [DOI] [PubMed] [Google Scholar]
- 7.Melve KK, Skjaerven R, Gjessing HK, Oyen N. Recurrence of gestational age in sibships: implications for perinatal mortality. Am J Epidemiol. 1999;150:756–762. doi: 10.1093/oxfordjournals.aje.a010078. [DOI] [PubMed] [Google Scholar]
- 8.Adams MM, Elam-Evans LD, Wilson HG, Gilbertz DA. Rates of and factors associated with recurrence of preterm delivery. JAMA. 2000;283:1591–1596. doi: 10.1001/jama.283.12.1591. [DOI] [PubMed] [Google Scholar]
- 9.Mercer BM, Macpherson CA, Goldenberg RL, Goepfert AR, Hauguel-de Mouzon S, Varner MW, et al. Are women with recurrent spontaneous preterm births different from those without such history? Am J Obstet Gynecol. 2006;194:1176–1184. doi: 10.1016/j.ajog.2006.01.069. discussion 84-5. [DOI] [PubMed] [Google Scholar]
- 10.Ananth CV, Getahun D, Peltier MR, Salihu HM, Vintzileos AM. Recurrence of spontaneous versus medically indicated preterm birth. Am J Obstet Gynecol. 2006;195:643–650. doi: 10.1016/j.ajog.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 11.Kristensen J, Langhoff-Roos J, Kristensen FB. Implications of idiopathic preterm delivery for previous and subsequent pregnancies. Obstet Gynecol. 1995;86:800–804. doi: 10.1016/0029-7844(95)00275-V. [DOI] [PubMed] [Google Scholar]
- 12.Bloom SL, Yost NP, McIntire DD, Leveno KJ. Recurrence of preterm birth in singleton and twin pregnancies. Obstet Gynecol. 2001;98:379–385. doi: 10.1016/s0029-7844(01)01466-1. [DOI] [PubMed] [Google Scholar]
- 13.Simonsen S, Lyon J, Stanford J, Porucznik C, Esplin M, Varner M. Risk factors for recurrent preterm birth in multiparous Utah women: a historical cohort study. BJOG : an international journal of obstetrics and gynaecology. 2013 doi: 10.1111/1471-0528.12182. [DOI] [PubMed] [Google Scholar]
- 14.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Osterman MJ. Births: final data for 2008. Natl Vital Stat Rep. 2010;59:1, 3–71. [PubMed] [Google Scholar]
- 15.Behrman RE. Committee on Understanding Premature Birth and Assuring Healthy Outcomes. In: ASB, editor. Preterm Birth: Causes, Consequences, and Prevention. PDF available from the National Academies Press at: http://www.nap.edu/catalog/11622.html. [PubMed] [Google Scholar]
- 16.Laughon SK, Reddy UM, Sun L, Zhang J. Precursors for late preterm birth in singleton gestations. Obstet Gynecol. 2010;116:1047–1055. doi: 10.1097/AOG.0b013e3181f73f97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334:567–572. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- 18.Meis PJ, Klebanoff M, Thom E, Dombrowski MP, Sibai B, Moawad AH, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348:2379–2385. doi: 10.1056/NEJMoa035140. [DOI] [PubMed] [Google Scholar]