Abstract
Objective: Patient self-management support may be augmented by using home-based technologies that generate data points that providers can potentially use to make more timely changes in the patients' care. The purpose of this study was to evaluate the effectiveness of short-term targeted use of remote data transmission on treatment outcomes in patients with diabetes who had either out-of-range hemoglobin A1c (A1c) and/or blood pressure (BP) measurements. Materials and Methods: A single-center randomized controlled clinical trial design compared in-home monitoring (n=55) and usual care (n=53) in patients with type 2 diabetes and hypertension being treated in primary care clinics. Primary outcomes were A1c and systolic BP after a 12-week intervention. Results: There were no significant differences between the intervention and control groups on either A1c or systolic BP following the intervention. Conclusions: The addition of technology alone is unlikely to lead to improvements in outcomes. Practices need to be selective in their use of telemonitoring with patients, limiting it to patients who have motivation or a significant change in care, such as starting insulin. Attention to the need for effective and responsive clinic processes to optimize the use of the additional data is also important when implementing these types of technology.
Key words: : telemedicine, diabetes, hypertension, care management
Introduction
Diabetes mellitus and hypertension are prevalent illnesses that co-occur in many patients. Simultaneous control of blood glucose (BG) and blood pressure (BP) is complex1 and difficult to achieve.2 Self-management support can improve outcomes3,4 and may be augmented by using home-based technologies that enable providers to monitor patients more frequently than is possible through face-to-face office visits. In-home monitoring can increase the number of non–clinic visit-generated data points that providers can potentially use to make changes in the patients' care. In-home monitoring and transmission provide more timely information that could potentially change the care plan, as opposed to waiting for 3 months for the next scheduled visit or for an emergency to occur, before getting updated clinical values. Use of these technologies can also shift some responsibility for review of data and/or patient management from the primary care physician to other clinicians (e.g., nurses or pharmacists), which has been shown to be effective in managing hypertension.5
The purpose of this study was to evaluate the effectiveness of short-term targeted use of data transmission from in-home devices (BG meter and BP machine) to the clinic on treatment outcomes in patients with diabetes who had either out-of-range hemoglobin A1c (A1c) or systolic BP (SBP) measurements.
Materials and Methods
Participants
The study was approved by the University of Missouri Institutional Review Board. The study took place at six University of Missouri Family Medicine (FM) and General Internal Medicine (GIM) clinics. To identify subjects with established type 2 diabetes who were out of desired range on either A1c (≥8%) or SBP (>130 mm Hg), we queried the electronic medical record every 2 weeks during the study enrollment phase. In addition to A1c and SBP levels, criteria for inclusion were age ≥18 years old, taking either oral diabetes medication or injectable insulin, diagnosis of type 2 diabetes for at least 1 year prior to study enrollment, currently using and/or owning a BG meter compatible with study equipment, having an in-home analog phone line or computer with Internet connection, and receiving primary care at FM or GIM clinics from an attending physician and anticipating receiving primary care for the next 12 months from that clinic. We excluded patients who were diagnosed in the past 12 months or had type 1 diabetes, were legally blind, resided in a long-term care facility (nursing home, assisted living facility, or other residential care), were severely cognitively impaired (more than two errors on a six-item cognitive screen6 administered by telephone), or had someone else from their immediate household enrolled in the study.
For potential subjects identified from the electronic medical record query, we asked their primary care physicians to sign a letter along with the study's Principal Investigator (D.R.M.) that described the study and invited participation. Thus, the patient's primary physician could exclude patients from the study. The letter included a copy of the consent form and a stamped postcard for the patient to return indicating if he or she was not willing to be contacted for the study (an opt-out approach). Within 2 weeks of sending the letter, a study research assistant telephoned those patients who had not declined, described the study in more detail, answered questions, obtained verbal consent for participation and to access and review pertinent records in the electronic medical record, scheduled the enrollment visit, and instructed the patient to bring his or her BG meter to the enrollment visit. After patients signed the study consent form, they were randomized to intervention and control groups by the research assistant using sequentially numbered sealed opaque envelopes prepared in advance by the study data manager. Because of the nature of the intervention, neither the patients nor the physicians were blinded to the patient's group assignment.
Intervention
The study used a telemonitoring system from Numera (formerly IMetrikus, Mountain View, CA). All participants were provided with an electronic BP monitor and used their personal BG meter to track their BP and BG. Once the patient completed a measurement, he or she pressed the button on the Numera Net Connectivity Hub®, a small portable, one-button device that transfers data directly over either an analog phone line or a personal computer with Internet access (patients chose which upload method to use). The Connectivity Hub securely connects to personal health monitoring devices via a cable or infrared link and thus is able to accommodate a wide range of BG meters. Patient data were securely transferred to a password-protected secure Web site using the company's Food and Drug Administration–cleared gateway. Patients could choose to send data daily or, because data were stored on the glucose meter and BP machine, could upload several measurements at a time. Participants with access to the Internet were able to track and monitor their progress on the patient section of the Web site.
Intervention patients were trained by the study research assistant on the equipment setup at the enrollment visit, including connecting the equipment to their computer or phone line and performing uploads. Training was hands-on, and patients were asked to demonstrate setting up the equipment and connecting their meter and the compatible BP cuff. Patients were given instruction on how to take their BP with the equipment-compatible BP cuff according to American Heart Association measurement guidelines.7 Intervention patients were asked to test their BP and BG a minimum of at least once daily for the 3-month study duration, but their provider could request more frequent readings. We requested that patients upload their readings daily if possible and at least every other day.
Transmitted data were reviewed by the clinic nurse at least two times per week and, if issues were identified, then printed out for provider review, verbally reported, or electronically communicated to the provider, depending on his or her preference. Advanced practice nurses in the FM clinic could make changes in patient treatment based on their currently established privileges (e.g., medication adjustments); other nurses in the GIM or FM clinics reviewed the data with providers who would change treatment plans. All treatment changes were individualized according to patient need. No standardized BG or BP management protocol was used. Communication of changes in therapy to the patient was accomplished per usual clinic protocol (e.g., usually by a telephone call to the patient, with documentation of a telephone note in the medical record).
Control group patients (those who did not receive the device) were asked to test their BP and BG at least once daily (in the same fashion as the intervention group). Those control group patients who did not own a BP cuff were given a study cuff to use and instructed on how to take a measurement. They were instructed to record both readings and bring their records to their clinic visits. After 3 months, all subjects returned to the clinic for follow-up A1c and BP measurement and for poststudy surveys. At that time, all participants received a $20 gift card for their participation.
Nurses were trained on the study protocol by study investigators and use of the equipment by a Numera staff member prior to the enrollment phase. Providers received an overview of the study in scheduled staff meetings. During these meetings, providers were also shown possible data views (daily, summarized, graphed) so that they could choose their preferred data display options when communicating with the clinic nurses.
Measures
Baseline data were collected from the patient, including demographic data (age, gender, race, and years of formal education), payor status (private pay, insurance, Medicaid), and the level of in-home assistance the patient was receiving with his or her BG or BP management. If the most recent A1c was greater than 10 weeks old, an A1c was obtained at study enrollment. In order to assess for baseline differences in patient activation, the 13-item short form Patient Activation Measure (PAM)8 was administered at enrollment. The PAM assesses the patient's beliefs, confidence, and knowledge in self-management and the likelihood of taking action to improve one's health. One of the ways that increased communication about self-monitoring data may work is to draw parallels to lifestyle and self-management choices, which may work through increased activation to motivate behavior change and improved clinical outcomes. PAM items were scored on a 5-point scale, where 1=strongly agree through 4=strongly disagree and 5=no opinion. The primary outcomes were improvement in BG (A1c measure at the end of the 3-month intervention) and SBP. If enrolled subjects had an A1c measurement in the record at the end of 6 months, we collected these data to assess longer-term effects of the intervention. At the conclusion of participation in the study, intervention patients completed a 17-item investigator-developed questionnaire used in prior studies of home monitoring interventions9,10 to assess their perceptions of the program.
Statistical Methods
SAS for Windows version 9.2 software (SAS Institute, Cary, NC) was used for all analyses. Demographic data, patient perception, and PAM data were analyzed using descriptive statistics.
For the BG and BP outcomes, linear mixed models (hierarchical linear models) were fit to the data with both fixed and random effects along with some fixed effect interaction terms and key covariates (sex, baseline measurement of outcome, age at enrollment, and PAM score). Main fixed effects included time in the study (days since enrollment), group (intervention or control), and group-by-time interaction. Random effects included a subject-specific random intercept to account for the heterogeneity among patients with respect to baseline outcome measures. A random effect due to the primary care provider was also included to account for the hierarchical nature of patients being treated by the same primary care provider and the dependency among patients that could induce. We primarily used PROC MIXED in SAS to fit models. Model fit was assessed using graphical model diagnostics to explore both the fixed and random effects via raw and Studentized residuals and conditional Pearson residuals. In conjunction with these graphical approaches, the corrected Akaike Information Criterion11 was used for model selection and to prevent overfitting.
Results
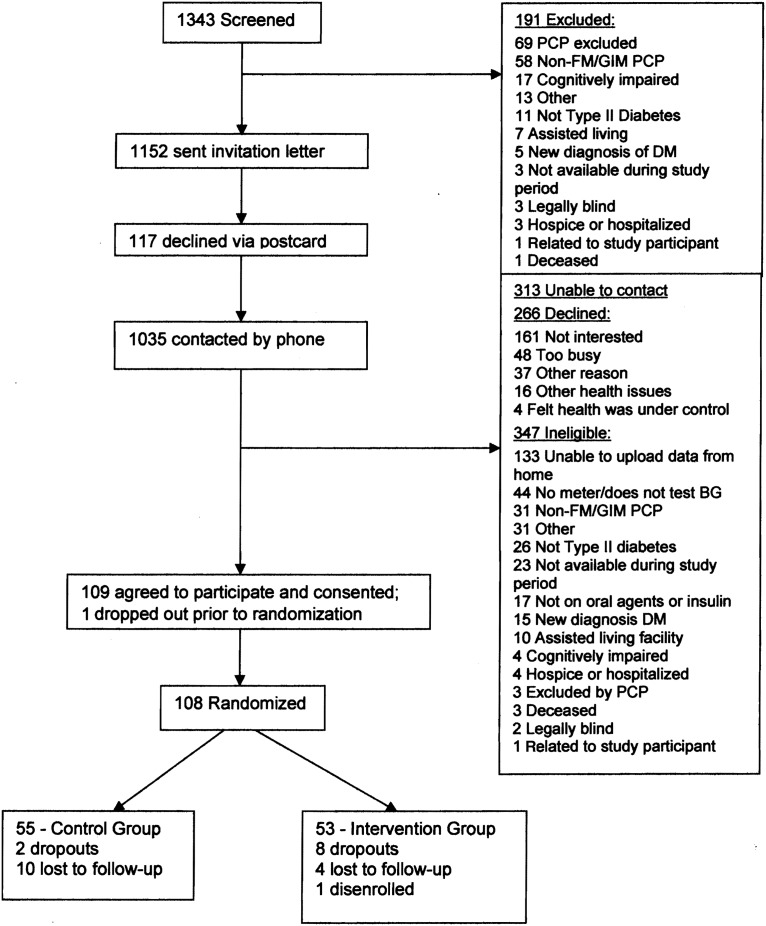
Recruitment occurred from May of 2009 through August 2010. Figure 1 shows participant flow throughout the study. From an initial subject pool of 1,343 potential participants, 191 (14%) were excluded by their primary care physician. The remaining 1,152 received an invitation letter. Of those, 117 (10%) returned the postcard declining participation. Of the 1,035 contacted by telephone, 266 declined, 347 were ineligible, and we were unable to contact 313. Of the 108 who agreed to participate, 53 were randomized to the intervention and 55 to the control group. Most subjects were enrolled based on out-of-control BP (n=52 controls and n=48 intervention). The overall dropout/lost to follow-up rate was 23% (2 controls and 8 intervention patients dropped out; 10 control and 4 intervention patients were lost to follow-up). Thus, complete data were obtained for 94 subjects. There were no adverse events in the study population.
Fig. 1.
Participant flow. BG, blood glucose; DM, diabetes mellitus; FM, family medicine; GIM, general internal medicine; PCP, primary care provider.
The mean age of the sample was 60 years and was significantly different between the two groups (control group, mean=62.5 years, SD=10.9, range=32–92; intervention group, mean=57.7 years, SD=10.8, range=29–82; p=0.02). There were no significant differences in the remaining demographic variables. Most participants had public or private insurance, and most paid for less than 25% of their health costs out of pocket (Table 1). At enrollment, 20% of participants indicated they received help at home with managing diabetes or BP, and this was most often provided by their spouse.
Table 1.
Demographic Participant Characteristics by Randomized Group Assignment
| VARIABLE | CONTROL (N=55) | INTERVENTION (N=53) |
|---|---|---|
| Male gender | 23 (41) | 25 (47) |
| Race | ||
| White non-Hispanic | 48 (87) | 46 (87) |
| Black/African American | 7 (13) | 5 (9) |
| Asian | 0 | 1 (2) |
| Not reported | 0 | 1 (2) |
| Education | ||
| 8–12 years (no high school diploma) | 2 (4) | 1 (2) |
| High school graduate/GED | 13 (24) | 10 (19) |
| Some college | 12 (22) | 19 (36) |
| College graduate | 28 (51) | 23 (43) |
| Marital status | ||
| Married | 30 (55) | 38 (72) |
| Separated/divorced | 9 (16) | 6 (11) |
| Widowed | 6 (11) | 2 (4) |
| Single | 10 (18) | 7 (13) |
| Payor status (could have more than one) | ||
| Medicaid | 7 (13) | 3 (6) |
| Medicare | 31 (56) | 16 (30) |
| Private insurance | 42 (76) | 48 (91) |
| Other | 2 (4) | 0 |
| About what percentage would you say you pay out of your own pocket for your diabetes care not including any hospital care? | ||
| 0–25% | 45 (82) | 39 (74) |
| 26–50% | 8 (15) | 13 (25) |
| 51–75% | 2 (4) | 0 |
| 76–100% | 0 | 0 |
Data are number (%).
Twenty-eight physicians had patients enrolled in the study (23 FM and 5 GIM). Most study patients were in FM (n=85; 79%). Five registered nurses (four in FM and one in GIM) and one licensed practical nurse (in GIM) were responsible for reviewing patient data. The registered nurses included two clinical nurse specialists and one family nurse practitioner. Two of the registered nurses were certified diabetes educators. Years in nursing practice ranged from 25 to 45, with a mean of 32 years. Years in their current position in the clinic ranged from 3 to 12 years (mean, 5.6 years).
There were no baseline differences for mean A1c or SBP, although SBP differed by gender. Likewise, at the end of 3 months, there were no statistically significant differences in A1c or SBP between the intervention and control participants (Table 2). Thus, we concluded that the remote monitoring program did not improve patients' diabetes or BP control. This is summarized in Tables 3 and 4, which contain covariate-adjusted estimates and 95% confidence intervals of differences between groups and time periods for A1c (Table 3) and SBP (Table 4).
Table 2.
Hemoglobin A1c and Systolic Blood Pressure Outcomes (Adjusted Means)
| VARIABLE | BASELINE | 3 MONTHS | 6 MONTHS |
|---|---|---|---|
| Hemoglobin A1c (%)a | |||
| Intervention (n=41) | 7.2 (0.21) | 7.2 (0.20) | 7.3 (0.20) |
| Control (n=53) | 7.4 (0.18) | 7.4 (0.18) | 7.4 (0.17) |
| Systolic blood pressure (mm Hg)a | |||
| Intervention (n=41) | |||
| Male | 142 (3.4) | 140 (3.5) | — |
| Female | 142 (3.3) | 141 (3.5) | — |
| Control (n=53) | |||
| Male | 148 (3.4) | 144 (3.6) | — |
| Female | 141 (2.9) | 137 (3.0) | — |
Data are mean (standard error of the mean) values. Six-month blood pressure was not available because the study data collection ended at 3 months.
n=52 controls and n=48 intervention subjects were enrolled based on out-of-control blood pressure.
Table 3.
Covariate-Adjusted Change in Hemoglobin A1c
| COMPARISON OF MEAN A1C | ESTIMATE | STANDARD ERROR | 95% CONFIDENCE INTERVAL |
|---|---|---|---|
| Intervention – control | |||
| Baseline difference | −0.1396 | 0.2596 | (−0.6544, 0.3752) |
| At 90 days | −0.1503 | 0.2511 | (−0.6492, 0.3485) |
| At 180 days | −0.1611 | 0.2462 | (−0.6507, 0.3286) |
| At 180 days – baseline | |||
| Intervention | 0.0301 | 0.0426 | (−0.0539, 0.1140) |
| Control | 0.0515 | 0.0440 | (−0.0352, 0.1382) |
Negative/lower values favor intervention.
A1c, hemoglobin A1c.
Table 4.
Covariate-Adjusted Change in Systolic Blood Pressure
| COMPARISON OF MEAN SBP (INTERVENTION – CONTROL) | ESTIMATE | STANDARD ERROR | 95% CONFIDENCE INTERVAL |
|---|---|---|---|
| Baseline difference | |||
| Males | −6.27 | 4.72 | (−15.65, 3.11) |
| Females | 1.11 | 4.37 | (−7.56, 9.79) |
| Difference at 90 days | |||
| Males | −3.31 | 4.96 | (−13.15, 6.53) |
| Females | 4.08 | 4.61 | (−5.07, 13.23) |
Negative/lower values favor intervention.
SBP, systolic blood pressure.
On average, participants' A1c worsened slightly over time. However, the rate of at which this happened was slower in the intervention group (0.03) than the control group (0.05) after 180 days (Table 3, last two rows). In contrast, SBP improved slightly over time for everyone (data not shown). Patient activation between the two groups at baseline was not significantly different (data not shown). Intervention patients rated the remote monitoring favorably (Table 5).
Table 5.
Patient Device Perceptions Questionnaire
| ITEM | MEAN (SD) |
|---|---|
| 1. I think the IMetrikus device was simple to set up in my home. | 1.6 (0.4) |
| 2. Sending data with the IMetrikus device is easy for me. | 1.8 (1.0) |
| 3. Sending data with the IMetrikus device interferes with my lifestyle. | 3.6 (1.2) |
| 4. Knowing that nurses are monitoring the data I send gives me peace of mind. | 1.8 (0.8) |
| 5. Using the IMetrikus device and Web site could alert me to a health problem I might have otherwise missed. | 1.7 (0.9) |
| 6. Using the IMetrikus device could alert my doctor/nurse to a health problem he or she might have otherwise missed. | 1.5 (0.6) |
| 7. Sending data each day takes too much time. | 3.4 (1.3) |
| 8. It is difficult for me to remember to send my data each day. | 3.4 (1.2) |
| 9. If given the option, I would want to continue sending data every day after the study period ends. | 2.3 (1.1) |
| 10. I would recommend this program (sending daily data) to other patients with the same condition. | 1.6 (0.7) |
| 11. I feel that using the IMetrikus device helped me to manage my diabetes. | 2.0 (0.9) |
| 12. Using the IMetrikus device helped me to manage my blood pressure. | 2.1 (1.2) |
| 13. I am comfortable using a blood glucose machine at home. | 1.3 (0.5) |
| 14. I am comfortable measuring my blood pressure at home. | 1.6 (1.1) |
| 15. I was satisfied with the frequency of communication I received from my doctor or nurse while using the IMetrikus device. | 2.4 (1.3) |
| 16. I was satisfied with the quality of the communication I received from my doctor or nurse about my diabetes while using the health messaging device. | 2.2 (1.3) |
| 17. Overall, I felt I knew more about my diabetes while using the health messaging device than I had without it. | 2.0 (1.1) |
The 5-point scale ranged from strongly agree=1 to strongly disagree=5.
Discussion
We implemented a remote monitoring program in primary care clinics for patients with diabetes who had either uncontrolled BG or BP. Although patients rated the intervention in a positive light, after 3 months of monitoring, there were no significant differences between the intervention and control groups on either A1c or SBP.
This study differed from previous examinations of telemonitoring because the data were directly transmitted to the patient's primary care nurse/doctor team but without the use of a “study” nurse or other research personnel. As such, it was an attempt to see how such data collection might be integrated into a clinic's normal workflow. It also differs from previous studies in that the response to data was not prescribed but was left to the discretion of the patient's primary care providers. Although the setting for this study was practices associated with academic departments of internal medicine and FM, this study advances the understanding of telemonitoring in more “real-world” primary care practice.
Prior studies have found positive results for remote monitoring for BG and BP. In a study using similar enrollment criteria to our study, Stone et al.12 compared active care management plus home telemonitoring with a monthly telephone call and found significant reductions in A1c at 3 and 6 months with active management and telemonitoring (1.7% vs. 0.7% and 1.7% vs. 0.8%, respectively; n=150). Bosworth et al.13 compared three intervention approaches with usual care hypertension management: nurse-administered behavioral intervention by telephone, home BP monitoring three times per week, and the behavioral intervention plus home monitoring (n=636); only the combined behavioral intervention and home monitoring improved BP control relative to usual care (−0.6 mm Hg and −3.9 mm Hg, respectively). Adding Web-based pharmacist communication14 to Web-only training and BP monitoring significantly improved BP control in patients with hypertension (56% vs. 31% in the control group with controlled BP) (n=778).
Only a few studies have evaluated improving outcomes in patients with multiple morbidities. A study using remote monitoring with an educational component and nurse care management improved A1c over 6 months (0.44% decrease, p=0.0001) and reduced SBP over 6 months (change=−6.05 mm Hg, p=0.01) and 12 months (change=−4.92 mm Hg, p=0.04) in patients who received a more intensive management approach (n=302).10 In a randomized trial in Canada, a pharmacist–nurse team working with a family physician achieved a statistically significant reduction in BP in patients with diabetes mellitus over 24 weeks (reduction in SBP at 6 months of 5.6 [standard deviation 2.1] mm Hg compared with controls) (n=227).15 Others have found a spillover effect where a hypertension management program also improved A1c (0.46% reduction over 2 years; n=216), even though it was not the focus of the intervention.16
There are several possible reasons for our negative findings. First, our study intervention consisted of transmission of BG and BP data to the clinic. No additional teaching, coaching, or other more intensive interventions were implemented. Although the intervention was supported by research funding, we implemented it using existing clinic staff rather than research nurses, which may have muted the effect of the intervention. Enrolled patients were in relatively good control at baseline for both A1c and BP; thus clinicians may have been hesitant to push for tighter control. Another factor that may have led to some physicians to be reluctant to pursue tight glycemic control was the publishing of the results of the ACCORD trial just before our study began.17 Our intervention period was relatively short at 3 months. Although changes in A1c could be manifested in 3 months, it is possible a more intensive intervention over a longer period of time would have resulted in a greater improvement in clinical outcomes.
The primary conclusion from this study may be, as we are learning from other studies,18,19 that the addition of technology alone is unlikely lead to improvements in care. Furthermore, patients may view the technology as an impediment to their existing relationship with providers and feelings of independence and sense of personal control.20 To best make use of these telemonitoring data in primary care, a practice might need to designate additional personnel resources to monitor the data and provide more intensive feedback and education for patients. Technology alone will likely fail to increase patient activation toward their self-management goals. Another factor is that practices may need to be more selective in their use of telemonitoring with patients, limiting it to those who have motivation or a significant change in care, such as starting insulin.
The number of clinical items addressed per visit has increased disproportionally to visit length.21 The increase in the number of clinical items is primarily driven by increases in the number of diagnoses and medications and increased BP monitoring and blood work.21 Thus, approaches such as remote monitoring of some vital signs such as BP or BG may allow more efficient use of time during clinic visits. However, as our data show, monitoring alone may not improve patient outcomes. Thus, patients with out-of-range BP or BG may benefit from more intensive intervention that can be provided by nonphysician staff such as nurses in models such as the patient-centered medical home. However, reimbursement models would need to accommodate this type of care for it to be widely adopted by primary care practices.
Acknowledgments
This work was supported in part by grant number R18HS017035 from the Agency for Healthcare Research and Quality.
Disclosure Statement
No competing financial interests exist.
References
- 1.Grant RW, Pirraglia PA, Meigs JB, Singer DE. Trends in complexity of diabetes care in the United States from 1991 to 2000. Arch Intern Med 2004;164:1134–1139 [DOI] [PubMed] [Google Scholar]
- 2.Jackson GL, Edelman D, Weinberger M. Simultaneous control of intermediate diabetes outcomes among Veterans Affairs primary care patients. J Gen Intern Med 2006;21:1050–1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: Chronic disease self-management programs for older adults. Ann Intern Med 2005;143:427–438 [DOI] [PubMed] [Google Scholar]
- 4.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Med Care 1999;37:5–14 [DOI] [PubMed] [Google Scholar]
- 5.Walsh JME, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: A systematic review. Med Care 2006;44:646–657 [DOI] [PubMed] [Google Scholar]
- 6.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002;40:771–781 [DOI] [PubMed] [Google Scholar]
- 7.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 2005;45:142–161 [DOI] [PubMed] [Google Scholar]
- 8.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res 2005;40:1918–1930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wakefield BJ, Holman JE, Ray A, Scherubel M. Patient perceptions of a remote monitoring intervention for chronic disease management. J Gerontol Nurs 2011;37:16–20 [DOI] [PubMed] [Google Scholar]
- 10.Wakefield BJ, Holman JE, Ray A, et al. Effectiveness of home telehealth in comorbid diabetes and hypertension: A randomized, controlled trial. Telemed J E Health 2011;17:254–261 [DOI] [PubMed] [Google Scholar]
- 11.Cavanaugh JE. Unifying the derivations of the Akaike and corrected Akaike information criteria. Stat Probabil Lett 1997;31:201–208 [Google Scholar]
- 12.Stone RA, Rao RH, Sevick MA, et al. Active care management supported by home telemonitoring in veterans with type 2 diabetes: The DiaTel randomized controlled trial. Diabetes Care 2010;33:478–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bosworth HB, Olsen MK, Grubber JM, et al. Two self-management interventions to improve hypertension control: A randomized trial. Ann Intern Med 2009;151:687–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: A randomized controlled trial. JAMA 2008;299:2857–2867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McLean DL, McAlister FA, Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: Study of Cardiovascular Risk Intervention by Pharmacists–Hypertension (SCRIP-HTN). Arch Intern Med 2008;168:2355–2361 [DOI] [PubMed] [Google Scholar]
- 16.Powers BJ, Olsen MK, Oddone EZ, Bosworth HB. The effect of a hypertension self-management intervention on diabetes and cholesterol control. Am J Med 2009;122:639–646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cartwright M, Hirani SP, Rixon L, Beynon M, Doll H, Bower P, et al. Effect of telehealth on quality of life and psychological outcomes over 12 months (Whole Systems Demonstrator telehealth questionnaire study): Nested study of patient reported outcomes in a pragmatic, cluster randomised controlled trial. BMJ 2013;346:f653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaudhry SI, Mattera JA, Curtis JP, et al. Telemonitoring in patients with heart failure. N Engl J Med 2010;363:2301–2309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanders C, Rogers A, Bowen R, Bower P, Hirani S, Cartwright M, et al. Exploring barriers to participation and adoption of telehealth and telecare within the Whole System Demonstrator trial: A qualitative study. BMC Health Serv Res 2012;12:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abbo ED, Zhang Q, Zelder M, Huang ES. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med 2008;23:2058–2065 [DOI] [PMC free article] [PubMed] [Google Scholar]