Abstract
Background: Adoption of smart devices for hospital use has been increasing with the development of health applications (apps) for patient point-of-care and hospital management. To promote the use of health apps, we describe the lessons learned from developing 12 health apps in the largest tertiary hospital in Korea. Materials and Methods: We reviewed and analyzed 12 routinely used apps in three categories—Smart Clinic, Smart Patient, and Smart Hospital—based on target users and functions. The log data for each app were collected from the date of release up until December 2012. Results: Medical personnel accessed a mobile electronic medical record app classified as Smart Clinic an average of 452 times per day. Smart Hospital apps are actively used to communicate with each other. Patients logged on to a mobile personal health record app categorized as Smart Patient an average of 222 times per day. As the mobile trend, the choice of supporting operating system (OS) is more difficult. By developing these apps, a monitoring system is needed for evaluation. Conclusions: We described the lessons learned regarding OS support, device choice, and developmental strategy. The OS can be chosen according to market share or hospital strategic plan. Smartphones were favored compared with tablets. Alliance with an information technology company can be the best way to develop apps. Health apps designed for smart devices can be used to improve healthcare. However, to develop health apps, hospitals must define their future goals and carefully consider all the aspects.
Key words: : health applications, e-health, telehealth, telecommunications, smartphones
Introduction
Mobile health (m-health) is defined as medical and public health practice supported by mobile devices including phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices by the Global Observatory for eHealth of the World Health Organization.1 Because of the potential benefits, the m-health market has grown rapidly.2,3 The global m-health market was estimated to be worth $1.2 billion in 2011 and is expected to increase to $11.8 billion by 2018.2 Roughly half of the consumers predict that m-health will improve the convenience, cost, and quality of healthcare within the next 3 years.3 Also, many academic articles on m-health have been published recently.4–18 One such study conducted a comprehensive review of 60 previous studies on the use of smartphones in medicine.4 Case studies of m-health use5,18 and systematic reviews of protocols for adopting m-health technology6,13 have also been published. A recent literature review examined how effectively m-health changed patient behavior in developing countries.7 The impact of mobile handheld technology on the work and practices of hospital physicians and on patient care has been summarized in recent reviews.8,13 Several interesting studies have examined how effectively m-health increases physical activity,9 the management of diabetes,10,16 and the self-management of chronic illnesses.11,14 M-health has even been used for randomized controlled trials for weight loss12 and glucose control.17
If we adopt the Global Observatory for eHealth definition, m-health has existed since the early 2000s. However, the rapid growth of m-health for use in business and healthcare coincided with the smartphone “explosion.” In 2012, almost half of U.S. mobile subscribers used smartphones, and two-thirds of those who bought a new phone chose a smartphone.19 In 2012, 81% of physicians in the United States used smartphones and tablets.20 Many physicians already use smartphones for patient care or for disease diagnosis, drug reference, literature searches, clinical communications, and hospital information system client applications; they are even used as medical calculators.21 Also, the health application (app) market has expanded rapidly. The sports and health app market will reach $400 million in revenues by 2016. The number of health app downloads will reach 44 million in 2012, rising to 142 million by 2016.22 There are already 75 Food and Drug Administration–regulated mobile apps.23
However, because this technology is still relatively new, physicians have concerns about patients using health apps. Only 27% of doctors encourage patients to use them to become more active in managing their health, and 13% actually discourage it.3 Here, to ease physicians' worries and to promote the active adoption of apps for patient care, we describe our experience in a smart health service that uses health apps.
Asan Medical Center (AMC) in Seoul was established in 1989 and is the largest hospital in Korea, with about 2,700 inpatient beds and 10,000 outpatient visits per day. Since its establishment, health information technology has been actively adopted and is widely used to improve quality of care and to make clinical workflow more efficient.24 In the early 2000s, AMC began using m-health services (on PDAs) to improve the accessibility, mobility, and efficiency of patient care. Because of the very large number of patients and the active use of health information technology, our experience may be helpful to other hospitals.
Materials and Methods
Categorization
Categories of health apps can be diverse.25 Here, we categorized the apps into three classes based on the target users and hospital function as follows: Smart Clinic (sClinic), Smart Patient (sPatient), and Smart Hospital (sHospital). The sClinic apps support efficient clinical practices by providing patient information and medical information. The sPatient apps provide reliable health information that supports patient self-monitoring and self-care. The sHospital apps improve communications between hospital staff by allowing them to share medical or clinical information and knowledge. We categorized 12 AMC health apps into the above categories and then analyzed the usage patterns of representative apps from each category to evaluate their usefulness. The mobile electronic medical record (EMR) app, mobile Asan Medical Information System (mAMIS), was selected from the sClinic category; My Chart in My Hand, which is the first mobile personal health record (PHR) app in Korea, was selected from the sPatient category; and AsaniN (information & kNowledge) and Asan Phonebook were selected from the sHospital category. Based on the lessons learned during app development, we reviewed these health apps in terms of the operating system (OS) (Android® [Google, Mountainview, CA]) OS or iOS [Apple, Cupertino, CA]), the development strategy (outsourcing, in-house, or alliance), and the target device (phone or tablet).
Log Data Collection and Analysis
The logs for the selected apps were collected as described below. The mAMIS logs were collected from December 2010 to December 2012, beginning when the app was first released to the clinicians at AMC. mAMIS was upgraded to version 2.0 in March 2012; therefore, separate log analyzes were performed for versions 1.0 and 2.0. The simple statistics of the previous PDA-based mAMIS were also analyzed for comparison. The My Chart in My Hand logs were collected from December 2010 to December 2012, starting from the release of the app by the SK Telecom T store in December 2010 and by Google Play in January 2011. The log data for the AsaniN and Asan Phonebook apps were collected from December 2010 to December 2012 for fair comparison. Other apps were briefly described and reviewed in terms of the number of downloads from the App Store because no log information was available.
Results
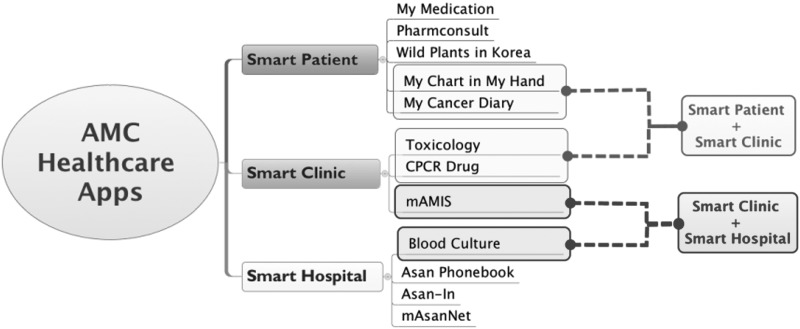
Figure 1 shows the categories for the 12 AMC health apps. There were five sClinic apps, seven sPatient apps, and five sHospital apps. Because an app with diverse functions can be categorized into different classes, six of the apps were included in two categories.
Fig. 1.
Categories of smart health applications (apps) at Asan Medical Center. The app names and their purpose and category are shown. Smart Clinic includes apps for effective clinical practice, Smart Patients includes apps for self-monitoring or self-care, and Smart Hospital includes apps for communication or knowledge sharing between hospital employees. An app can be included in more than one category if it has multiple functions. mAMIS, mobile Asan Medical Information System.
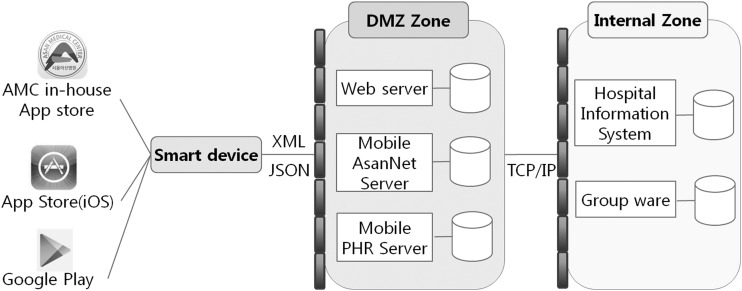
The 12 AMC health apps' deployment of platform and technological architecture are described in Figure 2. All of the sPatient apps and some sClinic apps not linked to the legacy system were released via the App Store or Google Play. sClinic apps linked to the legacy system and all sHospital apps were released via the AMC in-house application store for hospital staffs. When connecting to the legacy hospital information system, mobile servers in the demilitarized zone (DMZ) are used. Smart devices communicate with mobile servers using XML or JSON, and mobile servers are connected to internal system by transmission control protocol/Internet protocol.
Fig. 2.
Deployment of platform and technological architecture in Asan Medical Center (AMC) health applications (apps). OS, operating system; PHR, personal health record; DMZ, demilitarized zone; TCP/IP, transmission control protocol/Internet protocol.
sClinic APP: mAMIS (MOBILE EMR)
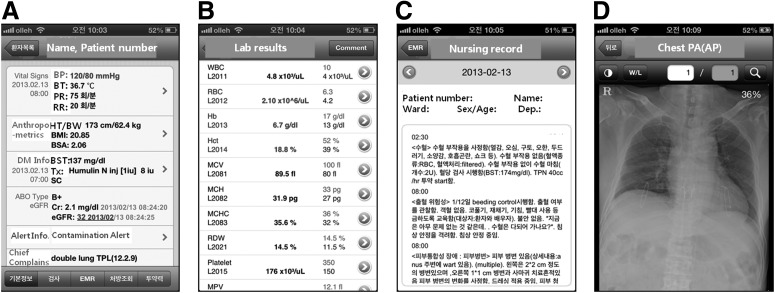
mAMIS is the mobile EMR developed to realize point-of-care treatment. mAMIS can be used to review all necessary medical records, including medications, laboratory results, and picture archiving and communication system images. Screenshots of mAMIS are shown in Figure 3. It was first launched in 2004 for use on PDAs running the Windows mobile OS. However, the PDA-based mobile EMR was not successful because it failed to provide the smart user experience offered by more recent smartphones. mAMIS was rebuilt for iOS and released in December 2010. After 1 year, the app was improved, and version 2.0 was launched in March 2012.
Fig. 3.
Screenshots of the mobile Asan Medical Information System application: (A) basic patient information, (B) lab results, (C) electronic medical record viewer, and (D) picture archiving and communication system image.
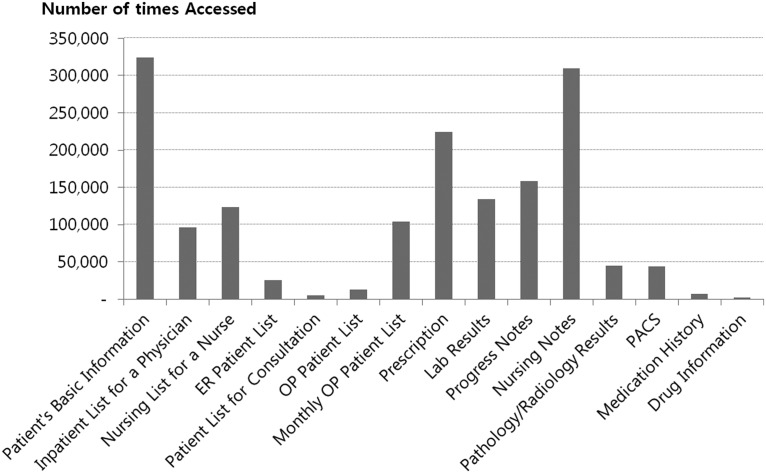
The total number of mAMIS version 2.0 users is now over 1,500. Two hundred users accessed EMRs using mAMIS on a daily basis, and approximately 13,600 transactions occurred every day. Most users were doctors (45%) and nurses (53%), but some were pharmacists (1%). As shown in Figure 4, the most frequently used service (other than checking basic patient information) was access to nursing notes, followed by prescriptions, progress notes, lab results, and nursing lists. As usage by nurses has steadily increased, so has access to nursing-related services such as nursing notes and nursing lists.
Fig. 4.
Popular services in the mobile Asan Medical Information System application. The number of times each menu in the mobile Asan Medical Information System was accessed is shown. The most frequently used service was basic patient information, followed by prescriptions and lab results. ER, emergency room; OP, operating room; PACS, picture archiving and communication system.
When we first launched the PDA-based mAMIS in 2004, we provided doctors with PDAs to encourage them to use the app. However, PDA-based mAMIS was used only twice a day on average. After mAMIS was upgraded for use on the iPhone® (Apple), it was accessed 452 times per day, even though we did not provide staff with iPhones. We believed that an intuitive user interface (UI) would increase the use of mAMIS, and it appears that it was the iPhone UI that led to a significant increase in usage. The difference between mAMIS version 1.0 and 2.0 (for the iPhone) is small; therefore, it was the iPhone UI that was responsible for the increased use. Now, as “Bring Your Own Device” becomes more popular, users' needs to support other OSs are increased.
sPatient APP: MY CHART IN MY HAND (MOBILE PHR)
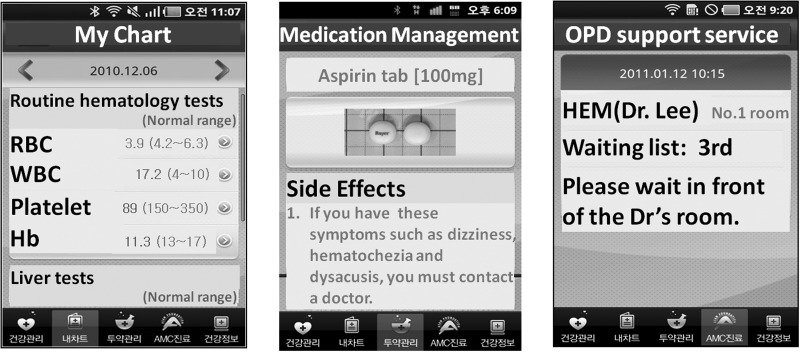
My Chart in My Hand was the first mobile PHR app in Korea. This mobile PHR app was developed with a Korean telecommunication company (SK Telecom Co., Ltd., Seoul) and operates on the Android OS. Screenshots are shown in Figure 5. The app was released on Google Play in January 2011 and has five main features: “My chart,” “Health management,” “Medication management,” “Outpatient service,” and “Health information.” The “My chart” menu shows a patient's medical information, such as lab results, problem lists, and allergies diagnosed or checked-in at AMC. The “Health management” menu shows diaries of body weight, blood sugar levels, blood pressure levels, and medical calculation (e.g., body mass index, 10-year cardiovascular disease risk, and metabolic syndrome risk) depending on the user's input. The “Medication management” menu provides information regarding medication history and reminders and includes a scheduler. “Outpatient service” shows information about outpatient scheduling and the patient waiting time in the doctor's office. The “Health information” menu offers extensive health education materials.
Fig. 5.
Screenshots of My Chart in My Hand: (left) the home screen, (middle) basic lab results, and (right) drug information. It currently supports only the Korean language. My Chart in My Hand can be downloaded at https://play.google.com/store/apps/details?id=com.amc.mphr.mphrui
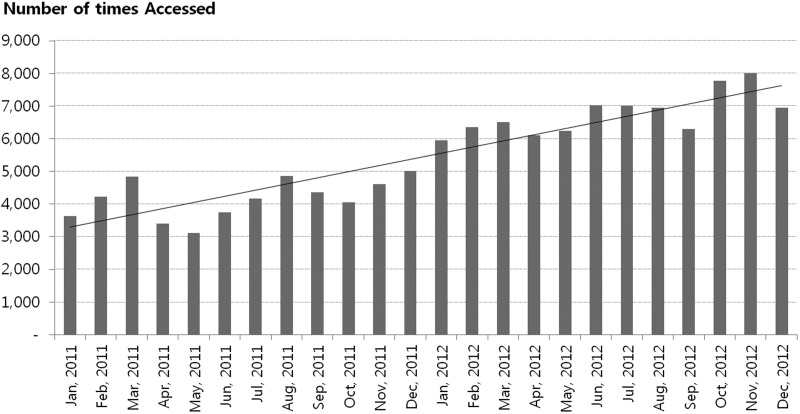
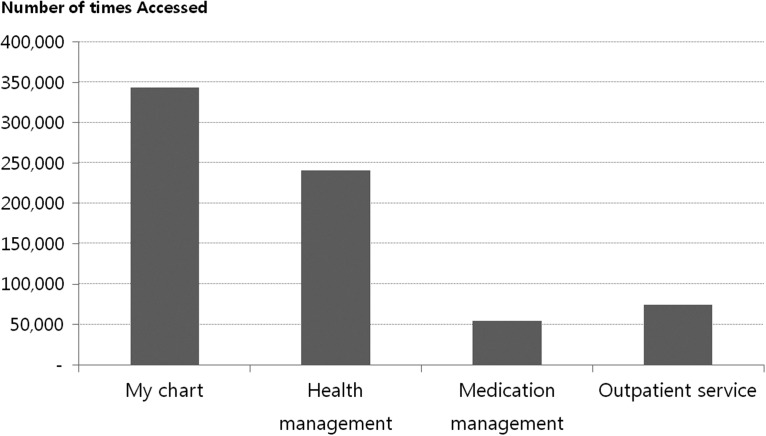
Now, 2 years after the app was launched, there are over 108,000 registered users, and the number of active users who have logged in to the system more than five times after installing the app is about 3,400. The total number of logins is continuously increasing (Fig. 6). The average number of daily logins in 2012 was 222. The most popular service is “My chart.” The next most frequently accessed services are the “Health management” service and “Outpatient scheduling” service (Fig. 7). Laboratory results is the most frequently accessed submenu; almost half of the accesses (44%) are for checking laboratory results.
Fig. 6.
Trends in the number of logins. The graph shows the number of logins to My Chart in My Hand from its launch in January 2011 up until December 2012. The trend line shows that the number of logins is steadily increasing.
Fig. 7.
The number of times each service of My Chart in My Hand was accessed. The number of accesses for each service within My Chart in My Hand from its launch up until December 2012 is displayed. Because there are no log data for the “Health information” menu, the graph does not show how many times it was accessed.
Our usage statistics may be comparable to the PHR portal of Kaiser Permanente.26 Even though My Chart in My Hand as a mobile app supports only the Android OS, about 108,000 users agreed to use this app in the AMC homepage, and almost 4,000 users downloaded the app. Among downloaded users, 88% users (3,430 users) are actively using this app. In the case of Kaiser Permanente,26 29.7 million lab results have been viewed online by 4 million users. As a result, a single user checks the lab results five times on average. In our case, a user reviews the lab results 80 times averagely (311,413 views by 3,995 users). Our patients more actively access their medical records. Or, alternatively, the PHR app can be more convenient than the PHR portal for smartphone users.
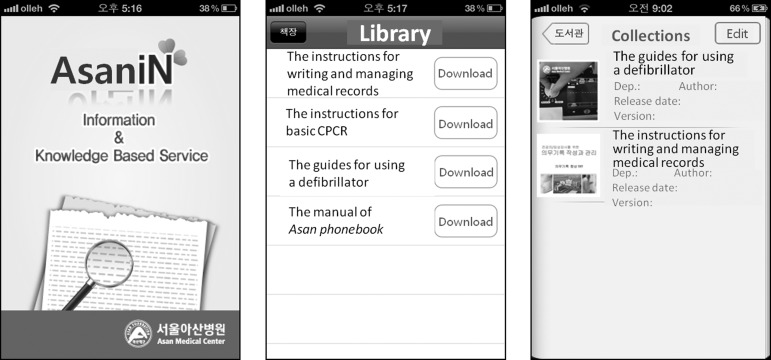
sHospital APP: AsaniN AND ASAN PHONEBOOK
AsaniN provides educational materials and useful reports in various formats, including PDF, PowerPoint® (Microsoft®, Redmond, WA), Word, Excel, and video files, for use by hospital employees. Thus, it is used mainly for knowledge sharing within the hospital. It now contains diverse educational materials, including guidelines on privacy and security, instructions for writing and managing medical records, instructions for basic cardiopulmonary resuscitation, a guide to using a defibrillator, and the Asan Phonebook manual. The user can even upload his or her own materials to AsaniN. Figure 8 shows a screenshot of AsaniN. Unfortunately, we could not generate detailed log data for AsaniN; we have only simple access logs. AsaniN had 1,242 total users and 6 daily users. Each user logged in to AsaniN 13 times per day as of December 2012. We suspect that users do not actively access AsaniN because the information contained within the app is not regularly updated. Therefore, to promote the use of AsaniN, new content should be added continuously and old content updated regularly.
Fig. 8.
Screenshots of AsaniN: (left) home screen, (middle) a list of manuals or useful reports, and (right) the manuals downloaded from the list.
Asan Phonebook, which shows the telephone numbers of AMC employees, was also frequently accessed. It had 1,164 total users and 58 daily users and was used on average 122 times each day. This implies that even simple apps can improve communication between hospital staff and help to improve patient care.
Other AMC Health APPS
Table 1 shows the number of times that the health apps released by AMC were downloaded from the public App Store. The My Medication app, which provides detailed AMC drug information, was downloaded over 70,000 times in a single year. PharmConsult provides information about medications for specific diseases (such as Parkinson's disease and asthma) and about patient medication counseling via e-mail. Representative examples of the counseling available on PharmConsult include adverse drug events or contraindications, indications or usual dosages, drug interactions with other medications, potential toxicity related to pregnancy or lactation, and information about the purchase, storage, and shelf-life of drugs. The Wild Plants in Korea app provides information on poisonous plants, including pictures, identification characteristics, and related emergency actions. The Toxicology app offers professional information for medical students and physicians regarding symptoms and the treatment of patients exposed to toxic agents. The CPCR Drugs app provides a guide to prescription medications for the cardiopulmonary cerebral resuscitation situation. The My Cancer Diary app helps cancer patients by providing educational material, information about the disease and anticancer drugs, and the planned administration dates for anticancer drugs. The Blood Culture app verifies a correct blood specimen by barcode scanning and collects information on blood sampling to check the quality.
Table 1.
Other Smart Health Applications Released by Asan Medical Center
| APPLICATION | RELEASE DATE | TOTAL NUMBER OF DOWNLOADS AS OF DECEMBER 2012 |
|---|---|---|
| My Medicationa | September 2010 (version 1.0) February 2011 (version 2.0) |
67,381 |
| PharmConsultb | January 2011 | 17,200 |
| Wild Plants in Koreac | January 2011 (version 1.0) June 2011 (version 2.0) |
17,062 |
| Toxicologyd | February 2010 | 9,068 |
| CPCR Drugse | May 2010 | 3,310 |
| My Cancer Diary | ||
| App Storef | October 2012 (phone) November 2012 (tablet) |
166 (phone, 71; tablet, 95) |
| T storeg | November 2012 | 71 |
These six apps have been released on external app stores. My Cancer Diary was released by both the iTunes App Store and the SK Telecom T store.
Discussion
During the development of these apps, we faced many choices regarding OSs, devices, and development strategies. Our experiences are summarized in Table 2.
Table 2.
Asan Medical Center Experience in Choosing the Best Way to Develop Health Applications: Summary of Asan Medical Center Health Applications According to Supporting Operating System, Device, and Development Method
| OS | DEVELOPMENT STRATEGY | DEVICE | |||||
|---|---|---|---|---|---|---|---|
| IOS | ANDROID OS | OUTSOURCING | IN-HOUSE | ALLIANCEa | PHONE | TABLET | |
| Number of apps | 11 | 7 | 3 | 8 | 1 | 12 | 1 |
| My Medication | * | * | * | ||||
| PharmConsult | * | * | * | ||||
| My Chart in My Hand | * | * | * | ||||
| Wild Plants in Korea | * | * | * | ||||
| Asan Phonebook | * | * | * | ||||
| AsaniN | * | * | * | ||||
| mAMIS | * | * | * | * | |||
| mobile AsanNet | * | * | * | * | |||
| Toxicology | * | * | * | ||||
| CPCR Drugs | * | * | * | ||||
| Blood Culture | * | b | * | * | |||
| My Cancer Diary | * | * | * | * | * | ||
Asterisk indicates the app is included in the given category.
This app was developed with a private company.
Under development.
mAMIS, mobile Asan Medical Information System; OS, operating system.
Choice of Operating System
We developed 11 apps for iOS and 4 apps for Android OS. AMC decided to use the iPhone for m-health in 2009. Therefore, all apps except My Chart in My Hand support iOS, which supports the Android OS because of an alliance with the partner company, SK Telecom. As the Android OS market share was over 90% in 2012,27 the company chose that as the target OS. This implies that the supporting OS is chosen according to market share or the hospital strategic plan. However, as “Bring Your Own Device” becomes more popular, the choice may become more difficult. Because of this trend, AMC has developed groupware (mobile AsanNet) for both the iOS and the Android OS. However, limited funding may force us to choose one of the two major OSs. Therefore, we are piloting alternatives to support diverse OSs (i.e., Mobile Enterprise Application Platform28 or HTML5).
Choice of Device
The choice of device is another important issue. There are many different tablets that run different OSs and are of different sizes. Up until now, we have developed only three apps for the iPad® (Apple). My Cancer Diary was the first iPad app because it is used for patient education, which requires a bigger screen. Following requests by patients or guardians, we have also developed a phone version of this app. When choosing between a phone or a tablet as the target device, the purpose of the app should be carefully reviewed to determine the optimum screen size. The phone app is often the first choice, as it can also be designed for use on tablets if required.
Choice of Development Strategy
When we initially developed these apps, we did not have a dedicated app programmer. Therefore, we could not develop apps with complicated features. Thus, the initial apps such as Toxicology and CPCR Drugs serve simple functions.
Outsourcing or alliances with another company are an alternative. My Chart in My Hand was developed through an alliance, and mAMIS and two other apps were developed through outsourcing. In our experience, an alliance is the best choice because it takes advantage of both in-house and outsourcing expertise. The partner company invests the necessary resources and provides prompt feedback throughout the development stages. The hospital defines the requisite health-related features of the target app. The drawback of this approach is that both sides must share a common interest. Outsourcing means that we can implement the necessary apps easily; however, it requires a larger investment during the initial development and for maintenance. In addition, upgrading and fixing bugs are more difficult.
Other Lessons Learned
First, there should be a monitoring system to analyze the use and effectiveness of the apps. To improve the apps, necessary data such as the usage patterns of menus and the number of users are required. Even if the apps are distributed by external app stores, a monitoring program should be developed. For example, because My Chart in My Hand has a monitoring system, we could easily analyze the log data and decide the future direction of app development. However, we can only check the number of downloads for the other apps in the App Store. This information gives an indication of how popular the apps are but does not provide the detailed background data needed to improve the apps.
Second, these health apps should both be connected to each other and integrated. Based on our experience, even though all apps within a category have their own purpose, they share many common features. To reduce the development and maintenance costs and to improve convenience, we chose My Chart in My Hand as a core app and then connected the other apps to this mobile PHR app. To accelerate this progress, we have a plan to improve My Chart in My Hand so that it is supported on any device, connected to social health networks, and can adopt emerging technologies.
Third, we should mention that since AMC established the ubiquitous Health (u-Health) Center in 2009, which develops m-health resources, the time required to develop diverse apps for various purposes has decreased. A hospital without such a center may experience difficulties in coordinating internal needs and developing apps with a vision for the future.
Conclusions
Eric Topol has argued that mobile technology will revolutionize healthcare.29 The m-health system needed a gateway device for connectivity and to provide the computing power. By adopting smart devices, the problems of connectivity and computing power were solved. In addition, smart devices may also be used as a sensing device. AMC has developed many apps to create a mobile hospital environment. By developing these apps, we learned lessons regarding the OS, improved our development strategies, and developed better connectivity and integration among apps. Based on these lessons, AMC continues to develop and improve the different apps within each category.
Disclosure Statement
No competing financial interests exist.
References
- 1.World Health Organization Global Observatory for eHealth Series, Vol. 3: mHealth: New horizons for health through mobile technologies. Geneva: WHO Press, 2011 [Google Scholar]
- 2.Expect rapid growth for telehealth, mHealth markets Available at www.cmio.net/index.php?option=com_articles&view=article&id=34805:expect-rapid-growth-for-telehealth-mhealth-markets (last accessed April22, 2013)
- 3.PricewaterhouseCoopers Emerging mHealth: Paths for growth. Available at www.pwc.com/en_GX/gx/healthcare/mhealth/assets/pwc-emerging-mhealth-full.pdf (last accessed April29, 2013)
- 4.Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: A review of current and potential use among physicians and students. J Med Internet Res 2012;14:e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dobkin BH, Dorsch A. The promise of mHealth: Daily activity monitoring and outcome assessments by wearable sensors. Neurorehabil Neural Repair 2011;25:788–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Free C, Phillips G, Felix L, Galli L, Patel V, Edwards P. The effectiveness of M-health technologies for improving health and health services: A systematic review protocol. BMC Res Notes 2010;3:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gurman TA, Rubin SE, Roess AA. Effectiveness of mHealth behavior change communication interventions in developing countries: A systematic review of the literature. J Health Commun 2012;17:82–104 [DOI] [PubMed] [Google Scholar]
- 8.Prgomet M, Georgiou A, Westbrook JI. The impact of mobile handheld technology on hospital physicians' work practices and patient care: A systematic review. J Am Med Inform Assoc 2009;16:792–801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fanning J, Mullen SP, McAuley E. Increasing physical activity with mobile devices: A meta-analysis. J Med Internet Res 2012;14:e161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baron J, McBain H, Newman S. The impact of mobile monitoring technologies on glycosylated hemoglobin in diabetes: A systematic review. J Diabetes Sci Technol 2012;6:1185–1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 2012;12:CD007459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spring B, Duncan JM, Janke EA, Kozak AT, McFadden HG, DeMott A, Pictor A, Epstein LH, Siddique J, Pellegrini CA, Buscemi J, Hedeker D. Integrating technology into standard weight loss treatment: A randomized controlled trial. Arch Intern Med 2012;173:105–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, Patel V, Haines A. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Med 2013;10:e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nundy S, Dick JJ, Goddu AP, Hogan P, Lu CY, Solomon MC, Bussie A, Chin MH, Peek ME. Using mobile health to support the chronic care model: Developing an institutional initiative. Int J Telemed Appl 2012;2012:871925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim J, Kim S, Kim H, Kim K, Lee CT, Yang S, Kong HJ, Shin Y, Lee K. Acceptability of the consumer-centric u-health services for patients with chronic obstructive pulmonary disease. Telemed J E Health 2012;18:329–338 [DOI] [PubMed] [Google Scholar]
- 16.Burner E, Menchine M, Taylor E, Arora S. Gender differences in diabetes self-management: A mixed-methods analysis of a mobile health intervention for inner-city Latino patients. J Diabetes Sci Technol 2013;7:111–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care 2011;34:1934–1942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blake H. Innovation in practice: Mobile phone technology in patient care. Br J Community Nurs 2008;13:160., 162–165. [DOI] [PubMed] [Google Scholar]
- 19.Nielsen Smartphones account for half of all mobile phones, dominate new phone purchases in the US. Available at http://blog.nielsen.com/nielsenwire/online_mobile/smartphones-account-for-half-of-all-mobile-phones-dominate-new-phone-purchases-in-the-us (last accessed April12, 2013)
- 20.Physician smartphone adoption rate to reach 81% in 2012 Available at http://manhattanresearch.com/News-and-Events/Press-Releases/physician-smartphones-2012 (last accessed April6, 2013)
- 21.Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak 2012;12:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cox A. mHealth users of remote health monitoring to reach 3 million by 2016: Smartphones play leading role [press release]. Available at www.juniperresearch.com/viewpressrelease.php?pr=285 (last accessed May2, 2013)
- 23.75 FDA regulated mobile medical apps Available at http://mobihealthnews.com/19638/analysis-75-fda-cleared-mobile-medical-apps/ (last accessed April30, 2013)
- 24.Ryu HJ, Kim WS, Lee JH, Min SW, Kim SJ, Lee YH, Nam SW, Eo GS, Seo SG, Nam MH. Asan medical information system for healthcare quality improvement. Healthc Inform Res 2010;16:191–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fox S. Mobile Health 2010. Pew Internet & American Life Project Report. 2010. Available at http://pewinternet.org/Reports/2010/Mobile-Health-2010.aspx (last accessed April30, 2013)
- 26.McCann E. Kaiser PHR sees 4 million sign on, most active portal to date. Available at www.healthcareitnews.com/news/kaiser-phr-sees-4-million-sign-most-active-portal-date (last accessed May2, 2013)
- 27.Lyons G. 2012 mobile market share [infographic]. Available at http://connect.icrossing.co.uk/2012-mobile-market-share-infographic_7962 (last accessed May2, 2013)
- 28.Clark W, King MJ. Magic quadrant for Mobile Enterprise Application Platforms: Gartner RAS core research note. ID number G00172728. Stamford, CT: Gartner, 2009 [Google Scholar]
- 29.Topol E. Creative destruction of medicine: How the digital revolution will creative better health care. New York: Basic Books, 2012 [Google Scholar]