Abstract
A 31-year-old white male with a known history of colon carcinoma was referred to the Interventional Pulmonary service for right lower lobe infiltrates and mucous plugging on computed tomography with concern for pneumonia. Bronchoscopy was performed revealing a broad based mass completely obstructing the bronchus intermedius. It was possible to pass a probe into the right lower lobe, and subsequent photoablation and mechanical debulking revealed that the mass was arising near the origin of the superior basal segment of the right lower lobe (RB6) and could be resected. Pathology confirmed this was consistent with the patient's known primary colon carcinoma. The potential for endobronchial metastasis in patients with colorectal carcinoma should be investigated in those patients with new or worsening pulmonary symptoms and signs.
Key words: Pulmonary infiltrates, Colon carcinoma, Endoluminal metastasis, Endobronchial colon cancer, Bronchoscopy, Interventional pulmonology
Case Report
A 31-year-old white male with a known history of colon carcinoma was referred to the Interventional Pulmonary service for right lower lobe infiltrates and mucous plugging on computed tomography (CT) with concern for pneumonia (fig. 1). Bronchoscopy was performed revealing a broad based mass completely obstructing the bronchus intermedius (fig. 2). It was possible to pass a probe into the right lower lobe, and subsequent photoablation and mechanical debulking revealed that the mass was arising near the origin of the superior basal segment of the right lower lobe (RB6) and could be resected (fig. 3). Pathology confirmed that this was consistent with the patient's known primary colon carcinoma.
Fig. 1.
CT scan of the chest with density in bronchus intermedius.
Fig. 2.
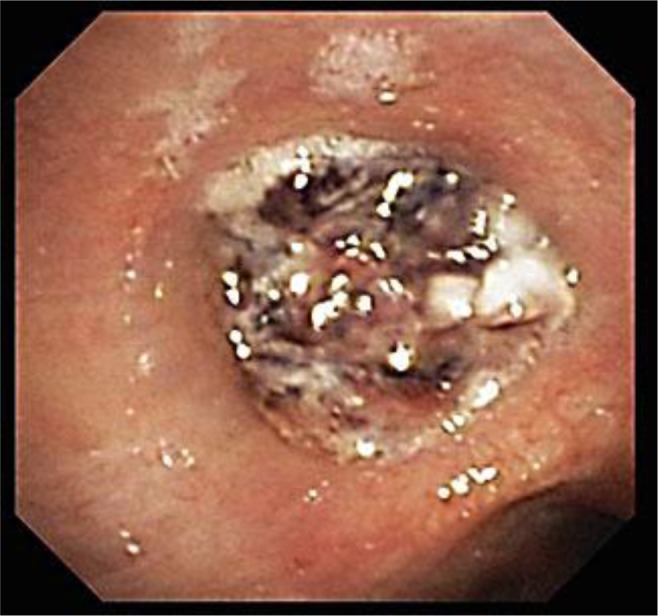
Bronchus intermedius mass.
Fig. 3.

Bronchus intermedius after endobronchial debulking.
Discussion
The incidence of endobronchial metastasis is reported to be about 2–28%, with the actual prevalence most likely much higher, as bronchoscopic inspection is not often routinely performed without symptoms or radiographic findings such as in our case [1, 2, 3, 4]. Endobronchial metastases are most frequently observed in patients with breast, colorectal, and renal cell carcinoma, with colorectal cancer thought responsible for 12–26% [1, 2, 3, 4, 5, 6]. According to a classification scheme described by Kiryu et al. [7], the development of endoluminal metastasis has been described to originate from different modes of progression. They proposed four developmental schemas characterized as type I, which is represented by direct metastasis to the bronchus; type II, with bronchial invasion by a parenchymal lesion; type III, which is described as bronchial invasion by mediastinal or hilar lymph node metastasis, and finally, type IV, where peripheral lesions extend along the proximal bronchus. Our patient most likely represented involvement classified as type I.
Although frequently asymptomatic (52%), endoluminal metastasis may commonly present with cough, wheezing, dyspnea, and hemoptysis [8]. Endoluminal metastasis may signal slow disease progression and have a median lag time of up to 5 years or more dependent upon the underlying primary malignancy [8, 9, 10]. Patients with colorectal carcinoma have a median age of 60 years (range 36–86), with our patient being one of the youngest patients reported with this complication. Patient survival is reported to be 70 months (range 23–245) with greater than 5-year survival in 54%, however, with a median survival following diagnosis of endobronchial metastasis reported to be 14 months (range 3–40) [4].
Appropriate diagnosis should be performed to exclude the potential of a second primary cancer. Endobronchial biopsies are easily obtained; however, as certain tumors are noted for a propensity toward significant bleeding, such as renal cell carcinoma and melanoma, initial sampling may easily be performed by means of endoluminal needle aspiration described by Wang et al. [11]. Interventional pulmonary techniques are able to benefit up to 93% of these patients, with a low mortality (5/1,000) [4, 12].
The potential for endobronchial metastasis in patients with colorectal carcinoma should be investigated in those patients with new or worsening pulmonary symptoms and signs.
References
- 1.Froudarakis ME, Bouros D, Siafakas NM. Endoluminal metastases of the tracheobronchial tree: is there any way out? Chest. 2001;119:679–681. doi: 10.1378/chest.119.3.679. [DOI] [PubMed] [Google Scholar]
- 2.Jung RC. Pulmonary lesions associated with extrapulmonary malignancies. Semin Respir Med. 1988;9:334–442. [Google Scholar]
- 3.Greelish JP, Friedberg JS. Secondary pulmonary malignancy. Surg Clin North Am. 2000;80:633–657. doi: 10.1016/s0039-6109(05)70204-8. [DOI] [PubMed] [Google Scholar]
- 4.Turner JF, Jr, Samlowski W, Bilodeau LL. Image of the month. Hemoptysis in a patient with melanoma and pulmonary infiltrates. J Thorac Oncol. 2008;3:1466–1467. doi: 10.1097/JTO.0b013e31818e0dee. [DOI] [PubMed] [Google Scholar]
- 5.Fourner C, Bertoletti L, Nguyen B, et al. Endobronchial metastasis from colorectal cancers: natural history and role of interventional bronchoscopy. Respiration. 2009;77:63–69. doi: 10.1159/000158487. [DOI] [PubMed] [Google Scholar]
- 6.Berg HK, Petrelli NJ, Herrera L, et al. Endobronchial metastasis from colorectal carcinoma. Dis Colon Rectum. 1984;27:745–748. doi: 10.1007/BF02554607. [DOI] [PubMed] [Google Scholar]
- 7.Kiryu T, Hoshi H, Matsui E. Endotracheal/endobronchial metastases: clinicopathologic study with special reference to developmental modes. Chest. 2001;119:768–775. doi: 10.1378/chest.119.3.768. [DOI] [PubMed] [Google Scholar]
- 8.Heitmiller RF, Marasco WJ, Hruban RH, et al. Endobronchial metastasis. Thorac Cardiovasc Surg. 1993;106:537–542. [PubMed] [Google Scholar]
- 9.Baumgartner WA, Mark JBD. Metastatic malignancies from distant sites to the tracheobronchial tree. Thorac Cardiovasc Surg. 1980;79:499–503. [PubMed] [Google Scholar]
- 10.Salud A, Porcel JM, Rovirosa A, et al. Endobronchial metastatic disease: analysis of 32 cases. J Surg Oncol. 1996;62:249–252. doi: 10.1002/(SICI)1096-9098(199608)62:4<249::AID-JSO4>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 11.Wang KP, Mehta A, Turner JF. Transbronchial needle aspiration for cytology and histology specimens. In: Wang KP, Mehta A, Turner JF, editors. Flexible Bronchoscopy. ed 2. Cambridge: Blackwell Science; 2012. pp. 147–169. [Google Scholar]
- 12.Cavaliere S, Venuta F, Foccoli P, et al. Endoscopic treatment of malignant airway obstruction in 2,008 patients. Chest. 1996;110:1536–1542. doi: 10.1378/chest.110.6.1536. [DOI] [PubMed] [Google Scholar]



