Abstract
One of the considerable challenges for screw-retained multi-unit implant prosthesis is achieving a passive fit of the prosthesis’ superstructure to the implants. This passive fit is supposed to be one of the most vital requirements for the maintenance of the osseointegration. On the other hand, the misfit of the implant supported superstructure may lead to unfavourable complications, which can be mechanical or biological in nature. The manifestations of these complications may range from fracture of various components in the implant system, pain, marginal bone loss, and even loss of osseointegration. Thus, minimizing the misfit and optimizing the passive fit should be a prerequisite for implant survival and success. The purpose of this article is to present and summarize some aspects of the passive fit achieving and improving methods. The literature review was performed through Science Direct, Pubmed, and Google database. They were searched in English using the following combinations of keywords: passive fit, implant misfit and framework misfit. Articles were selected on the basis of whether they had sufficient information related to framework misfit’s related factors, passive fit and its achievement techniques, marginal bone changes relation with the misfit, implant impression techniques and splinting concept. The related references were selected in order to emphasize the importance of the passive fit achievement and the misfit minimizing. Despite the fact that the literature presents considerable information regarding the framework’s misfit, there was not consistency in literature on a specified number or even a range to be the acceptable level of misfit. On the other hand, a review of the literature revealed that the complete passive fit still remains a tricky goal to be achieved by the prosthodontist.
Keywords: Passive fit, Misfit, Implant, Splinting
Introduction
In implant supported prostheses, reduced stress along the implant and surrounding bone is a desired feature. This could be possible through a passive fit of the prosthesis’ superstructure on the implant abutments [1]. The passive fit of implant supported prostheses to the underlying structures is fundamental for successful and survival of the osseointegrated prosthesis [2, 3]. Any misfit of the framework to the osseointegrated implants, clinically detectable or not, is believed to induce internal stresses in the prosthesis’ framework, the implants, and the bone surrounding the implant [4]. Certain biologic tolerance for the misfit between the prosthesis and the implant does present [5]. However, the quantifiable level of this misfit without adverse biomechanical problems could be difficult to be determined [6].
Generally, implant-supported fixed prostheses comprise screw retained and cement retained superstructures. A passive fit is more complex and difficult to achieve for a screw-retained implant superstructure especially with multi-unit implant supported prostheses [1]. Contributing factors to this problem could be distortion of impression material, dental stone and metal castings. On the other hands, cement retained implant prostheses have the potential for being passive because of the die spacer which can provide around 40 μm cement space [1, 7]. which can compensate for superstructure distortions and provide a more passive fit.
Randy et al. [8] has demonstrated a significant improvement in passive fit of cement retained prostheses compared to screw retained prostheses’ distortions. The lack of fit passivity of screw-retained superstructures may lead to greater stress concentrations around the implants in comparison to cement retained prostheses. It is therefore, essential to optimize the prosthesis fit by optimizing the prosthesis fabrication steps.
Materials and Methods
Electronic searches were performed in November 2010 from Science Direct, PubMed, and Google database with combinations of the key words passive fit, misfit and splinting. The publication year limit option was not used. The key words were typed in different combination with (dental implant). As a result 1,435 and 196 articles were found in Science Direct and PubMed, respectively. The found articles’ abstracts were retrieved and screened autonomously to evaluate their eligibility for selection in this literature review. They were sorted based on the following inclusion and exclusion criteria. To be included the article had to be published in an English peer-reviewed journal and it should contain sufficient information related to; (1) the framework misfit’s related factors 2-passive fit and its achievement techniques, (3) the misfit related marginal bone changes (4) implant impression techniques accuracy. The exclusion criteria were the followings: the reports which simply describing a particular material or technique, and structurally incomplete articles such as abstracts only.
Results
The electronic search in databases (Science Direct, PubMed, and Google databases) provided more than 1,400 titles and abstracts that were relevant to the dental implant superstructure passive fit/misfit. The complete text of 300 articles was retrieved and subjected to close scrutiny. Throughout this procedure, 256 articles were excluded. Eventually, 44 articles were selected, three articles [5, 15, 16] reporting on the misfit related marginal bone changes were selected, 37 articles [2–4, 10, 12–14, 17–24, 26–32, 34–40, 42–49] reporting on the framework misfit’s related factors, passive fit and its achievement techniques and implant impression techniques accuracy. Four articles [6, 11, 25, 33] were reviews.
Discussion
The Passive Fit
Although there is no actual definition to highlight the meaning of passive fit clinically, the superstructure of the screw retained implant-supported prosthesis can be considered passive if it does not generate static loads and strains within the prosthesis or in the surrounding bone matrix [9–12]. Jemt [4] defined the passive fit as a level of fit which will not produce or cause any long-term clinical problem.
Why Should the Clinician Achieve the Passive Fit
Unlike the natural teeth which can move in their sockets about 100 microns, the implant has limited range of movement around 10 microns [2]. Thus, the misfit in case of implant-supported prosthesis will be more destructive in contrast to the teeth-supported prosthesis (Fig. 1). And therefore, the passive fit achievement is a prerequisite for the survival and the successful long-term osseointegration [6].
Fig. 1.
Misfit of the implant supported prosthesis
Generally, the framework misfit may lead to mechanical and biological complications. Mechanical problems can be manifested as loosening of the prosthetic retaining screws, locking or fracturing of the abutment’s screw and fracture of various components in the system, which can be referred to a delayed component failure. On the other hand, biological complications may range from pain, tenderness, marginal bone loss, and even loss of osseointegration [6]. Flow diagram in Fig. 2 correlates the misfit of implant superstructure framework to the biologic and mechanical implant complications.
Fig. 2.
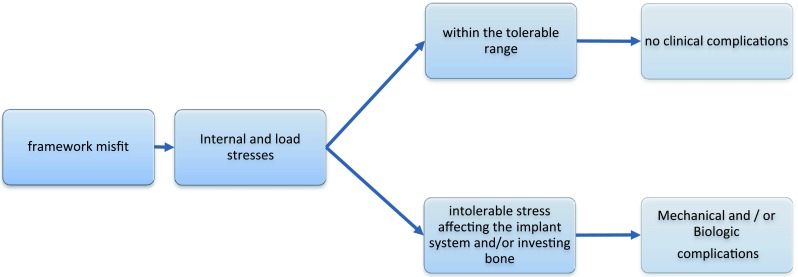
Flow diagram correlates the misfit to the biologic and mechanical implant complications
The Mechanical and Biological Tolerance
Mechanical or machining tolerance is defined as the difference in rest positions (horizontal shift) between the components when these components are held in place by their respective fastening screws. This can be considered as a source of misfit, which can range from 22 to 100 microns [13].
Kim et al. [14] studied the machining tolerance of the implant components, and found a machining tolerance of 31.1 ± 15.5 μm between the abutment and the impression coping and the value of 30.4 ± 15.6 μm between the impression coping and the abutment replica. These two values combined will give more than 61 microns of machining tolerance for single abutment.
Some authors suggested that the machining tolerance could help minimize the final distortion. At the delivery stage, the machining tolerance between the final framework and the intraoral abutments can make the passive fit achievable. Passive fit can occur if the machining tolerance was more than or equal to the final distortion [13].
The biological tolerance is the capability of the bone surrounding the implants to withstand and tolerate the stresses distributed along the implant-bone interface, without any further clinical complications. Roberts et al. [15] showed that remodelling of bone around the implants does occur. Michaels et al. [16] used a white rabbit tibia model to assess the implant-supported framework’s misfit. They found that despite the remodelling of the bone around the implant was obvious, there was no significant clinical, histomorphometric, or radiographic proof of implant-osseointegration failure. Another study by Jemt and Book [5] studied the prosthesis’ misfit and tried to correlate it to the marginal bone loss in edentulous implant, and they found three-dimensional distortions ranged between 91 and 111 μm. However, they could not correlate between this misfit and the observed marginal bone loss around the implant. Therefore, the results of these studies indicate that there is a biological tolerance to the misfit of the prosthesis.
Acceptable Levels of Misfit at the Implant–Abutment Interface
Several studies attempted to define the misfit numerically, but there was no definite agreement to quantify the acceptable level of the misfit [6]. The first person to quantify the passive fit of implant framework was Branemark [9] who stated that the misfit should be not more than 10 microns. While Klinberg and Murray [17] stated that 30 μm gap at the implant–abutment interface will be acceptable if it is not including more than 10 % of the circumference. More recently, Jemt [4] stated that a misfit around 150 microns will be acceptable, and he introduced the screw resistance test. Jemt stated that the passive fit can be achieved by screwing extra one half turn. Actually, this technique is applicable only in the implant systems where the thread pitch of the abutment screw is 300 μm, such as Nobel Biocare prosthetic screw. Therefore, by turning the screw an extra one and a half turn the clinician can gain other 150 microns. However, this might not be true for all implant systems as prosthetic screws are not designed similarly [6].
Evaluating the Implant Framework Misfit Clinically
Kan et al. [6] proposed several clinical assessment methods to evaluate implant framework misfit. (1) The alternate finger pressure the clinician should evaluate the rocking of the prosthesis and watch for any saliva bubbling around the misfit gap. (2) Direct vision and tactile sensation where the clinician uses the tip of an explorer to verify the marginal fit. This technique is limited by the size of the explorer tip. A brand new explorer tip is around 60 microns. (3) Radiographs the drawback, it can be overlapped or superimposed and depends on the angulations. (4) The Sheffield test (the one screw test) one screw will be tightened at one end of the framework and then the discrepancies observed at the other terminal screw. (5) Screw resistance test starting with the implant closest to the midline, the screws were tightened one by one until the initial resistance was met at one of the screws, if that screw needed more than extra half a turn to achieve the optimum screw seating, the framework is considered misfit. (6) Disclosing media and others such as the fit checker, pressure indicating paste and disclosing wax. They can be used in the case of supragingival and subgingival margins. (7) 3-Dimensional quantifying systems such as coordinate measuring machine, which can be used only extra-orally, and 3-D photogrammetric that can be used intra-orally. These systems can evaluate discrepancies to the nearest 10 μm. However, Kan et al. [6] concluded that none of these methods was truly reliable on its own, and suggested using them in combinations to achieve objective results.
The Distortion Equation and its Relationship to the Misfit
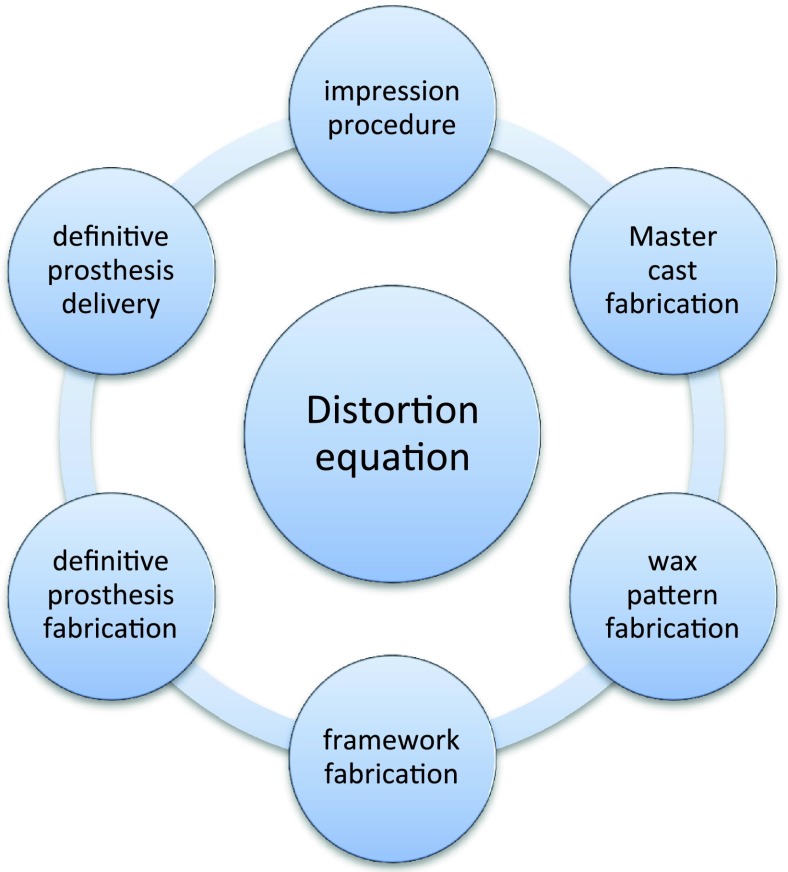
The implant superstructure misfit is a result of accumulative distortions during the whole procedure of final prosthesis fabrication, and this is called distortion equation, theoretically, the passive fit can be achieved if the summation of this distortion equation was zero [11].
The distortion equation includes the following clinical and laboratory procedures and their contributing factors [6, 11]: (1) Impression procedure contributing factors are mandibular flexure, impression technique/material, and machining tolerance of the impression copings. (2) Master cast fabrication contributing factors are machining tolerance of the implant replica, master cast pouring technique, and die materials used. (3) Wax pattern fabrication contributing factors are machining tolerance between the abutment replicas and gold cylinders, and the wax distortion. (4) Framework fabrication contributing factor is the conventional casting distortion. (5) Definitive prosthesis fabrication: contributing factor is Addition of acrylic or porcelain. (6) Definitive prosthesis delivery contributing factors are machining tolerance, fit detection variability between clinicians, and the mandibular flexure (Fig. 3).
Fig. 3.
Flow diagram describes the distortion equation and its components
The Impression Procedure as an Affecting Factor
The implant impression accuracy depends on several factors. These include the impression material, impression technique, the implant angulations and the number of implants. The impression technique itself depends on whether it is a direct or indirect method, splinted or non-splinted, and on the design of the impression coping.
The Implant Impression Material Types and Properties
There is an inevitable, inherent discrepancy in the implant impression, which was quoted in the range of 50 μm [18–20]. One of the factors related to this inherent discrepancy is the shrinkage and contraction of the impression material due to the cross-linking and rearrangement of the polymer chains. Further shrinkage can occur due to loss of volatile constituents and by-products. The expansion will also occur if there is water sorption [21].
Several impression materials have been used for multi-unit implant impression; the most commonly described were addition silicone and polyether impression materials. This can be correlated to their improved accuracy [19]. The implant impression material should exhibit an appropriate resiliency not to be deformed by the undercuts, and at the same time, it should be rigid enough to prevent the implant components from movement during the cast pouring procedure [21]. Many researchers found no significant difference in terms of dimensional accuracy between polyether and addition silicon impression materials [12, 22–24].
Sorrentino et al. [12] demonstrated that both polyether and addition silicone impression materials produced similarly accurate casts. However, in the presence of parallel implants, polyether impression material performed better in terms of accuracy. On the other hand, addition silicone impression material produced better accuracy in cases where angled implant situations were simulated. Lee et al. [19] also found that addition silicone was more accurate than the polyether in situations where the implants were placed at deeper sub gingival levels.
The Impression Tray
The customized tray can provide an impression with uniform thickness making it superior and more appropriate than a stock tray particularly in implant cases [25]. Burns et al. [26] compared the accuracy of customized tray to stock tray, and found that the impression taken with the customized tray was significantly more accurate. They postulated that the customized tray was more rigid than the stock tray, and at the same time, the impression material was uniformly distributed within the customized tray unlike the stock tray. However, Shen [27] stated that, with polyether and addition silicone impression materials, the customized tray was not that crucial, as these elastomeric materials were inherently rigid, and they exhibit dimensional stability, that allows the use of the stock tray without much distortion.
The Implant Angulation, Number and Impression Level
Several authors reported that as the angulation of the implant increases the accuracy of the impression decreases [12, 18, 28]. Implant impression accuracy has also been shown to be inversely affected by the number of the implants, and this was thought to be due to increased distortion and deformation on removal of the impression [12, 18]. Conrad et al. [29] reported that the acceptable angulation of the implant that will not have an adverse effect on the impression accuracy was around 15°. They also demonstrated that impression accuracy has as well been shown to be inversely affected by number and angulation of the implants.
The implant impression can be at the abutment or implant level. The implant level impression is preferred in the aesthetic zones and reduces the number of treatment visits. However, Daoudi et al. [22] reported that, in case of implant level impressions, more inaccuracy may be introduced. They postulated that the implant head is comparatively small, with short axial walls, and it lies relatively far away from the occlusal plane, that all could lead to various movements such as rotational movements, axial inclinations, and as a result, seating inaccuracy may occur.
The Impression Coping
The impression copings are mainly supplied in tapered or squared shapes. It has been reported that modification of the coping surface could enhance the accuracy of the impressions [30–32], modifications such as airborne particle abrasion of the copings and coating the copings with the compatible adhesive. It was hypothesized that roughing or adhesive addition to the external surface of the copings could reduce the micro-movement of coping, and therefore, minimizing the discrepancy of the impression.
Sorrentino et al. [12] studied the effect of the impression coping length on the dimensional accuracy of implant impression. They found with polyether impression material, longer coping was more accurate than short coping. On the other hand, with addition silicone impression material short coping was more accurate than the longer coping, particularly in case of non-parallel implants.
The Implant Impression Techniques
Two main implant impression techniques are used for transferring the intra-oral spatial relationship of the implants to the working cast. One impression technique is the direct open tray technique uses an open tray, a custom tray that contains windows exposing the impression copings. The other impression technique is the indirect technique uses closed tray.
Direct technique is also called the pickup impression technique; in this technique, the top of the impression coping screw (commonly square shape) is exposed and accessible. The impression copings are unscrewed to be retrieved along with the impression tray once the impression set [33]. The advantages of this technique is that there will be no concern for repositioning the copings, the angulations of the implants, and the copings do not deform the impression material upon retrieving. However, there could be a high chance of rotational discrepancy when the screws are fastened to connect implant replica to the impression copings [11, 22, 28, 29].
The indirect technique is also called the repositioning technique, in this technique, conical or tapered copings are connected to the implants/abutments before the impression. Closed trays are used. In contrast to the direct technique, the impression copings stay connected to the implant once the impression tray is retrieved, after then these copings will be unscrewed from the mouth and connected to the implant replica. This coping-implant replica assembly will be repositioned into its respective position within the impression [19].
In some situations, the indirect closed tray is preferred to direct open tray techniques, such as in cases of gagging, limited inter-arch space and in cases where access to the posterior region is limited. The advantages of this technique; it is easier as it resembles the conventional impression technique and the replica to copings fastening would be visualized directly. However, the impression material recovering from angled implants will be difficult, and there will be a high chance of impression deformation. Impression copings need to be carefully repositioned and correctly oriented back at their respective sites [28, 29].
Snap-fit (press fit) plastic impression, has been developed and suggested to be used with a close tray technique. The snap-fit procedure is best described as a mix between the two pick-up and closed tray techniques. In this closed tray technique, the direct transfer coping snaps on to the top of the implant/abutment intra-orally. Once the impression has set, the snap-fit coping became fixed in the impression material. On retrieving the set impression from the mouth, the snap-fit coping would be pulled off of the implant/abutment. Akca and Cehreli [34] compared the snap fit (snap on) technique using a stock tray and the two direct and indirect techniques using custom trays, and found that the snap fit technique was similar in terms of accuracy to the direct technique.
The Accuracy of the Direct and the Indirect Techniques
Several authors studied and compared the accuracy of direct and indirect techniques; some found that the direct technique was more accurate than the indirect one [18, 28, 35, 36]. Others demonstrated that the indirect technique was more accurate than the direct ones [37, 38]. While the rest found no statistically significant difference between both techniques [22, 29, 39–41].
A systematic review by Lee et al. [33] concluded that, in situations where there are three implants or fewer, no significant difference between the direct and the indirect techniques were observed, while in case of more than three implants, the direct technique was found to be more accurate.
The Splinting Concept
Branemark [9] was the first one to introduce the splinting of impression copings during impression procedure using rigid material, to stabilize and prevent the rotational, horizontal and vertical movement of the impression coping. Since then, various splinting techniques and materials used to hold rigidly the impression copings have been studied.
Various materials have been used to act as a splinting material. The most common one was the auto-polymerizing acrylic resin. Branemark [9] reported that application of Duralay acrylic resin to an adapted orthodontic wire, steel pin, or a dental floss in between the copings could be used for implant impression. Assif et al. [3] splinted the copings directly to the custom tray with the auto-polymerizing acrylic resin.
The application of auto-polymerizing acrylic resin as a splinting material had been reported in several studies [2, 3, 18, 31, 32, 35–37, 39, 41–44]. However, according to Mojon et al. [45] and Hsu et al. [46] this material has the disadvantage that can interfere with its dimensional stability. The autopolymerizing acrylic resin can shrink up to 7.9 % in the first 24 h, 80 % of this shrinkage appears within the first 17 min of mixing. Furthermore, the greater the mass of the Duralay acrylic resin, the greater the inaccuracy of the resultant impression [46].
Spector et al. [42] reported that the residual stresses within the set auto-polymerizing acrylic resin could be released when the impression is retrieved, leading to inaccuracy of the copings-implant relationship transfer. To overcome these problems, the following suggestions have been made [36, 43, 44]: (1) allow the material to set for 17 min before impression making, to avoid the shrinkage error, (2) minimizing the mass of splinting resin material by making silicone index for its fabrication, (3) sectioning the fabricated acrylic resin splint between the copings with a thin disk, and then rejoining the sectioned pieces together again with the incremental or bead-brushing techniques.
Some authors used the dual cured acrylic resin in an attempt to overcome the problem with splinting material shrinkage [14, 47]. David Assif [47] found that the dual-cured acrylic resin was significantly less accurate than the Duralay auto-polymerizing acrylic resin, and correlated that to incomplete polymerization of the dual-cured acrylic resin, there will be 25–45 % of the chemical bonds stay un-reacted even after 24 h of curing. The intensity and the direction of the light source may also have an adverse effect on the adaptation of the dual-cured acrylic resin to the copings.
The plaster impression was another material used as splinting material. [47, 48] Plaster could also be used for implant impression splinting particularly in edentulous cases but this material is limited to the situations where no anatomical limitations or undercuts [47].
Several studies have been conducted to study and compare between using and non-using splinting technique in implant impressions. Some workers found that splinting techniques were more accurate than the non-splinting ones [2, 18, 31, 41, 49]. While some others found the non-splinting technique was more accurate than the splinting techniques [35, 43, 44]. Other studies showed no significance statistically between both techniques [14, 32, 36, 39, 42, 46]. These different results could be related to the different methodology, materials, and operators’ factors.
Conclusion
The clinical and laboratory procedures in implant prosthodontics are many and demanding. Each stage may lead to a positional distortion and misfit. This misfit sometimes can be tolerated by the surrounding bone without adverse biomechanical complications. However, this tolerability has yet to be quantified and precisely determined. Thus, improving and optimizing the distortion equation components should help in reducing the end misfit of the implant superstructure. Many strategies were introduced to improve the implant superstructure fit; some were targeting the impression procedure, master cast fabrication, and framework construction. Others were targeting the definitive prosthesis delivery. However, a review of the literature revealed that the complete passive fit still remains a difficult goal to be achieved.
Contributor Information
Muaiyed Mahmoud Buzayan, Email: muaiyed_zyan@hotmail.com.
Norsiah Binti Yunus, Email: norsiah@um.edu.ny.
References
- 1.Michalakis KX, Hirayama H. Garefis PDCement-retained versus screw-retained implant restorations: a critical review. Int J Oral Maxillofac Implants. 2003;18:719–728. [PubMed] [Google Scholar]
- 2.Assif D, Marshak B, Schmidt A. Accuracy of implant impression techniques. Int J Oral Maxillofac Implants. 1996;11:216–222. [PubMed] [Google Scholar]
- 3.Assif D, Marshak B, Nissan J. A modified impression technique for implant-supported restoration. J Prosthet Dent. 1994;71:589–591. doi: 10.1016/0022-3913(94)90442-1. [DOI] [PubMed] [Google Scholar]
- 4.Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Branemark implants in edentulous jaws: a study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991;6:270–276. [PubMed] [Google Scholar]
- 5.Jemt T, Book K. Prosthesis misfit and marginal bone loss in edentulous implant patients.”. Int J Oral Maxillofac Implants. 1996;11:620–625. [PubMed] [Google Scholar]
- 6.Kan JY, Rungcharassaeng K, Bohsali K, Goodacre CJ, Lang BR. Clinical methods for evaluating implant framework fit. J Prosthet Dent. 1999;81:7–13. doi: 10.1016/S0022-3913(99)70229-5. [DOI] [PubMed] [Google Scholar]
- 7.Taylor TD, Agar JR, Vogiatzi T. Implant prosthodontics: current perspective and future directions. Int J Oral Maxillofac Implants. 2000;15:66–75. [PubMed] [Google Scholar]
- 8.Randi AP, Hsu AT, Verga A, Kim JJ. Dimensional accuracy and retentive strength of a retrievable cement-retained implant supported prosthesis. Int J Oral Maxillofac Implants. 2001;16:547–556. [PubMed] [Google Scholar]
- 9.Branemark PI, Zarb GA, Albrektsson T. Tissue -integrated prostheses. Chicago: Quintessence; 1985. p. 253. [Google Scholar]
- 10.Jemt T, Rubenstein JE, Carlsson L, Lang BR. Measuring fit at the implant prosthodontic interface. J Prosthet Dent. 1996;75:314–325. doi: 10.1016/S0022-3913(96)90491-6. [DOI] [PubMed] [Google Scholar]
- 11.Wee AG, Aquilino SA, Schneider RL. Strategies to achieve fit in implant prosthodontics: a review of the literature. Int J Prosthodont. 1999;12:167–178. [PubMed] [Google Scholar]
- 12.Sorrentino R, Gherlone EF, Calesini G, Zarone F. Effect of implant angulation, connection length, and impression material on the dimensional accuracy of implant impressions: an in vitro comparative study. Clin Implant Dent Relat Res. 2010;12(Suppl 1):e63–e76. doi: 10.1111/j.1708-8208.2009.00167.x. [DOI] [PubMed] [Google Scholar]
- 13.Ma T, Nicholls JI, Rubenstein JE. Tolerance measurements of various implant components. Int J Oral Maxillofac Implants. 1997;12:371–375. [PubMed] [Google Scholar]
- 14.Kim S, Nicholls JI, Han CH, Lee KW. Displacement of implant components from impressions to definitive casts. Int J Oral Maxillofac Implants. 2006;21:747–755. [PubMed] [Google Scholar]
- 15.Roberts WE, Smith RK, Zilberman Y, Mozsary PG, Smith RS. Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod. 1984;86:95–111. doi: 10.1016/0002-9416(84)90301-4. [DOI] [PubMed] [Google Scholar]
- 16.Michaels GC, Carr AB, Larsen PE. Effect of prosthetic superstructure accuracy on the osteointegrated implant bone interface. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:198–205. doi: 10.1016/S1079-2104(97)90006-8. [DOI] [PubMed] [Google Scholar]
- 17.Klinberged IJ, Murray GM. Design of superstructures for osseointegrated fixtures. Swed Dent J. 1985;28:63–69. [PubMed] [Google Scholar]
- 18.Assuncao WG, Filho HG, Zaniquelli O. Evaluation of transfer impressions for osseointegrated implants at various angulations. Implant Dent. 2004;13:358–366. doi: 10.1097/01.id.0000144509.58901.f7. [DOI] [PubMed] [Google Scholar]
- 19.Lee H, Ercoli C, Funkenbusch PD, Feng C. Effect of subgingival depth of implant placement on the dimensional accuracy of the implant impression: an in vitro study. J Prosthet Dent. 2008;99:107–113. doi: 10.1016/S0022-3913(08)60026-8. [DOI] [PubMed] [Google Scholar]
- 20.Rashidan N, Alikhasi M, Samadizadeh S, Beyabanaki E, Kharazifard MJ. Accuracy of implant impressions with different impression coping types and shapes. Clin Implant Dent Relat Res. 2009;14(2):218–225. doi: 10.1111/j.1708-8208.2009.00241.x. [DOI] [PubMed] [Google Scholar]
- 21.Robert G, Craig JMP. Restorative dental materials. St. Louis: Mosby; 2002. [Google Scholar]
- 22.Daoudi MF, Setchell DJ, Searson LJ. A laboratory investigation of the accuracy of two impression techniques for single-tooth implants.”. Int J Prosthodont. 2001;14:152–158. [PubMed] [Google Scholar]
- 23.Wenz HJ, Hertrampf K. Accuracy of impressions and casts using different implant impression techniques in a multi-implant system with an internal hex connection. Int J Oral Maxillofac Implants. 2008;23:39–47. [PubMed] [Google Scholar]
- 24.Aguilar ML, Augusto Elias, Toro Vizcarrondo CE, Psoter WJ. Analysis of three-dimensional distortion of two impression materials in the transfer of dental implants. J Prosthet Dent. 2009;103:202–209. doi: 10.1016/S0022-3913(10)60032-7. [DOI] [PubMed] [Google Scholar]
- 25.Donovan TE, Chee WW. A review of contemporary impression materials and techniques. Dent Clin North Am. 2004;48:445–470. doi: 10.1016/j.cden.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 26.Burns J, Palmer R, Howe L, Wilson R. Accuracy of open tray implant impressions: an in vitro comparison of stock versus custom trays. J Prosthet Dent. 2003;89:250–255. doi: 10.1067/mpr.2003.38. [DOI] [PubMed] [Google Scholar]
- 27.Shen C. Impression material. “K.J. Phillip’s science of dental materials”. Philadelphia: Saunders; 2003. pp. 205–254. [Google Scholar]
- 28.Carr AB. Comparison of impression techniques for a five-implant mandibular model. Int J Oral Maxillofac Implants. 1991;6:448–455. [PubMed] [Google Scholar]
- 29.Conrad HJ, Pesun IJ, DeLong R, Hodges JS. Accuracy of two impression techniques with angulated implants. J Prosthet Dent. 2007;97:349–356. doi: 10.1016/S0022-3913(07)60023-7. [DOI] [PubMed] [Google Scholar]
- 30.Vigolo P, Majzoub Z, Cordioli G. In vitro comparison of master cast accuracy for single-tooth implant replacement. J Prosthet Dent. 2000;83:562–566. doi: 10.1016/S0022-3913(00)70015-1. [DOI] [PubMed] [Google Scholar]
- 31.Vigolo P, Majzoub Z, Cordioli G. Evaluation of the accuracy of three techniques used for multiple implant abutment impressions. J Prosthet Dent. 2003;89:186–192. doi: 10.1067/mpr.2003.15. [DOI] [PubMed] [Google Scholar]
- 32.Vigolo P, Fonzi F, et al. An evaluation of impression techniques for multiple internal connection implant prostheses. J Prosthet Dent. 2004;92:470–476. doi: 10.1016/j.prosdent.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 33.Lee H, So JS, Hochstedler JL, Ercoli C. The accuracy of implant impressions: a systematic review. J Prosthet Dent. 2008;100:285–291. doi: 10.1016/S0022-3913(08)60208-5. [DOI] [PubMed] [Google Scholar]
- 34.Akca K, Cehreli MC. Accuracy of 2 impression techniques for ITI implants. Int J Oral Maxillofac Implants. 2004;19:517–523. [PubMed] [Google Scholar]
- 35.Phillips KM, Nicholls J, Ma T, Rubenstein J. The accuracy of three implant impression techniques: a three-dimensional analysis. Int J Oral Maxillofac Implants. 1994;9:533–540. [Google Scholar]
- 36.Del’Acqua MA, Arioli-Filho JN, Compagnoni MA, Mollo Fde A., Jr Accuracy of impression and pouring techniques for an implant-supported prosthesis. Int J Oral Maxillofac Implants. 2008;23:226–236. [PubMed] [Google Scholar]
- 37.Humphries RM, Yaman P, Bloem TJ. The accuracy of implant master casts constructed from transfer impressions. Int J Oral Maxillofac Implants. 1990;5:331–336. [PubMed] [Google Scholar]
- 38.De La Cruz JE, Funkenbusch PD, Ercoli C, Moss ME, Graser GN, Tallents RH. Verification jig for implant-supported prostheses: a comparison of standard impressions with verification jigs made of different materials. J Prosthet Dent. 2002;88:329–336. doi: 10.1067/mpr.2002.128070. [DOI] [PubMed] [Google Scholar]
- 39.Herbst D, Nel JC, Driessen CH, Becker PJ. Evaluation of impression accuracy for osseointegrated implant supported superstructures. J Prosthet Dent. 2000;83:555–561. doi: 10.1016/S0022-3913(00)70014-X. [DOI] [PubMed] [Google Scholar]
- 40.Daoudi MF, Setchell DJ, Searson LJ. An evaluation of three implant level impression techniques for single tooth implant.”. Eur J Prosthodont Restor Dent. 2004;12:9–14. [PubMed] [Google Scholar]
- 41.Naconecy MM, Teixeira ER, Shinkai RS, Frasca LC, Cervieri A. Evaluation of the accuracy of 3 transfer techniques for implant-supported prostheses with multiple abutments. Int J Oral Maxillofac Implants. 2004;19:192–198. [PubMed] [Google Scholar]
- 42.Spector MR, Donovan TE, Nicholls JI. An evaluation of impression techniques for osseointegrated implants. J Prosthet Dent. 1990;63:444–447. doi: 10.1016/0022-3913(90)90235-5. [DOI] [PubMed] [Google Scholar]
- 43.Inturregui JA, Aquilino SA, Ryther JS, Lund PS. Evaluation of three impression techniques for osseointegrated oral implants. J Prosthet Dent. 1993;69:503–509. doi: 10.1016/0022-3913(93)90160-P. [DOI] [PubMed] [Google Scholar]
- 44.Burawi G, Houston F, Byrne D, Claffey N. A comparison of the dimensional accuracy of the splinted and unsplinted impression techniques for the Bone-Lock implant system. J Prosthet Dent. 1997;77:68–75. doi: 10.1016/S0022-3913(97)70209-9. [DOI] [PubMed] [Google Scholar]
- 45.Mojon P, Oberholzer JP, Oberholzer JP, Meyer JM, Belser UC. Polymerization shrinkage of index and pattern acrylic resins. J Prosthet Dent. 1990;64:684–688. doi: 10.1016/0022-3913(90)90296-O. [DOI] [PubMed] [Google Scholar]
- 46.Hsu CC, Millstein PL, Stein RS. A comparative analysis of the accuracy of implant transfer techniques. J Prosthet Dent. 1993;69:588–593. doi: 10.1016/0022-3913(93)90287-X. [DOI] [PubMed] [Google Scholar]
- 47.Assif D, Nissan J, Varsano I, Singer A. Accuracy of implant impression splinted techniques: effect of splinting material. Int J Oral Maxillofac Implants. 1999;14:885–888. [PubMed] [Google Scholar]
- 48.Eid N. An implant impression technique using a plaster splinting index combined with a silicone impression. J Prosthet Dent. 2004;92:575–577. doi: 10.1016/j.prosdent.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 49.Hariharan R, Shankar C, Rajan M, Baig MR, Azhagarasan NS. Evaluation of accuracy of multiple dental implant impressions using various splinting materials. Int J Oral Maxillofac Implants. 2010;25:38–44. [PubMed] [Google Scholar]