Abstract
The most important factor affecting esthetics is colour. Whether a definitive prosthesis or a provisional restoration, maintenance of esthetics is of prime concern along with restoration of function. Colour stability of provisional prosthesis is affected by various factors and various studies are documented in the literature on this. The purpose of this study was to evaluate the colour stability of provisional restorative materials exposed to different mouth rinses at varying time intervals. 120 discs, each of self cure tooth moulding material, Protemp 4 and Revotek LC were prepared and immersed in two mouth rinses, hexidine and periogard and evaluated for their colour stability after 1 week, 1 and 3 months. The data obtained was statistically analysed using ANOVA and Tukey’s post hoc analysis. The results indicate that there is a significant difference in the colour variation of various materials in two different mouth rinses at different time intervals. Revotek LC was found to be the most colour stable material and periogard had the least staining potential at varying time intervals.
Keywords: Provisional restoration, Colour stability
Introduction
Provisional restorations are used in fixed prosthodontics for the period between tooth preparation and final prosthesis placement. Provisional restorations in fixed prosthodontic rehabilitation are important treatment procedures, particularly if the restorations are expected to function for extended periods of time or when additional therapy is required before completion of rehabilitation. The prognosis of a fixed restorative procedure is largely dependent upon the quality of the interim treatment restoration [1]. Fixed prosthodontic treatment, whether involving complete or partial coverage, natural tooth or dental implant abutments, commonly relies on indirect fabrication of a definitive prosthesis in the dental laboratory. Fabrication of this definitive prosthesis, on an average takes about 7–10 days during which the prepared tooth need to be protected from the oral environment and also its relationship with the adjacent and opposing tooth need to be maintained. Thus, in order to protect these prepared abutment teeth, provisional restorations are fabricated and the process is called as temporization.
The term “provisional” denotes “serving for the time being”, as a necessary step in providing for the final arrangement. The requirements can be biological, mechanical and esthetic concerns. The provisional crown protects the pulp from thermal and chemical insults after crown preparation and enamel removal. It serves to maintain gingival health and contour while providing for an esthetic and/or functional interim restoration. Provisional crown should also be easy to clean and not impinge on the tissues. Most importantly they maintain the inter-occlusal and intra-arch tooth relationships. Finally they should exhibit a good shade match and have a highly polished surface so that they are esthetically pleasing to the patient [2]. These restorations must not only provide an initial shade match, but also maintain an esthetic appearance over a period of time. Alterations in colour of these restorations compromise the acceptability.
Materials used for fabricating provisional restorations involve autopolymerizing polymethyl methacrylate, polyethylene methacrylate, polyvinyl methacrylate, urethane methacrylate, bis-acryl and even microfilled resin. These materials can be either chemically or light polymerised or both [3].
Colour stability of provisional materials is of prime concern, particularly when the restorations involve esthetic zone and must be worn for extended periods of time. Discoloration of provisional materials may lead to patient dissatisfaction and even additional expense for replacement. Although the use of stabilizers has decreased to a certain extent, the chemically induced colour change, provisional materials absorb liquids thereby producing colour change due to staining [4].
The degree of colour change can be affected by various factors like incomplete polymerization, water sorption, diet of the patient and oral hygiene measures. Water is found to play an important role in chemical degradation process such as oxidation and hydrolysis and thereby subsequent change in the optical property of the provisional restorative material.
The quantitative evaluation of colour difference (∆E) with a spectrophotometer confers advantages such as repeatability, sensitivity, objectivity despite some limitations [5]. If a material is completely colour stable or unstained, no colour difference will be detected after its exposure to the testing apparatus (∆E = 0).
Various studies have been reported on the influence of staining materials like tea, coffee, red wine on the provisional materials [6–8]. Mouth rinses have been routinely used to prevent bacterial colonization and maintenance of oral hygiene. But there is a lack of literature evidence on the effect of these mouth rinses on the colour stability of provisional crowns.
Hence, this study has been designed to evaluate the colour stability of three different commercially available provisional restorative materials when exposed to different mouth rinses at varying time intervals.
Materials and Methods
Three different provisional restorative materials (self cure tooth moulding powder-DPI, Protemp 4—3M ESPE, Revotek LC—GC Corp) and two mouth rinses (hexidine—ICPA and periogard—Colgate) were used. 360 specimens (120 of each material) were prepared in the form of discs of size 10 mm diameter and 2 mm thickness.
120 samples, each of self cure tooth moulding powder-DPI belonging to group I (Fig. 1), Protemp 4—3M ESPE belonging to group II (Fig. 2) and Revotek LC—GC Corp belonging to group III (Fig. 3) were then divided into four categories (A: untreated specimens, B: synthetic saliva, C: synthetic saliva + hexidine, D :synthetic saliva + periogard). The 120 samples of each group were now separated into these four categories of 30 samples each as I A: self cure untreated specimens, I B: self cure-synthetic saliva, I C: self cure-synthetic saliva + hexidine and I D: self cure-synthetic saliva + periogard and similarly for group II and group III.
Fig. 1.

Self cure tooth moulding material: group I
Fig. 2.
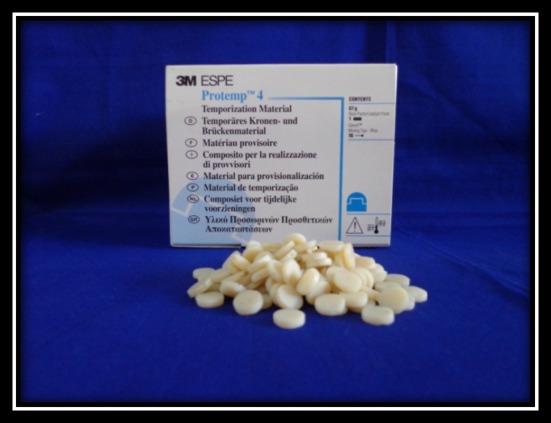
Protemp 4—3M ESPE: group II
Fig. 3.
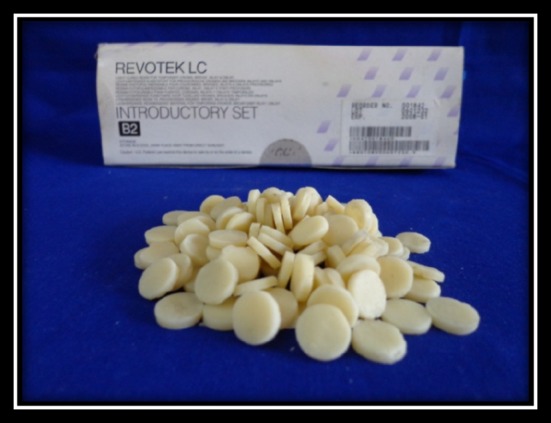
Revotek LC—GC Corp: group III
A brass template was fabricated using precise milling instruments with circular sections of 10 mm diameter and 2 mm depth cut off for the preparation of samples (Fig. 4).
Fig. 4.
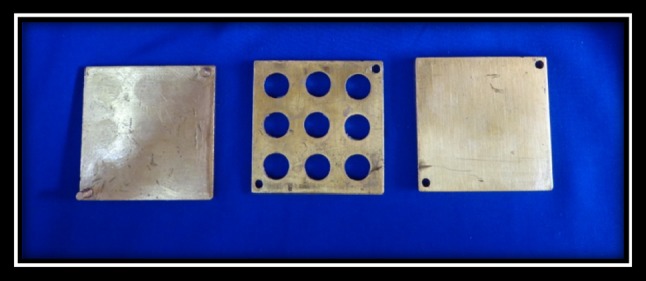
Brass template for fabrication of specimens 10 mm diameter and 2 mm depth
After finishing and polishing, the discs were rinsed with distilled water at room temperature and immersed in staining solutions. Untreated group specimens were used as a control. Colour intensity was evaluated after 1 week, 1 and 3 months using a spectrophotometer. Specimens of the required dimensions which were highly polished with smooth, flat and glossy surface were included in the study and specimens with surface irregularities, visible cracks or porosities were excluded from the study. The staining solutions were prepared in the ratio 3:1 (mouth rinse:synthetic saliva). The samples were then incubated at 37 °C and stored in a dark place to simulate oral conditions (Fig. 5).
Fig. 5.

Specimens in testing solutions
Surface stain was evaluated using a PC based double beam spectrophotometer. After 1 week, 1 and 3 months, 10 discs from each group were evaluated for colour variation. At 1 week, each disc was treated with 99.9 % ethanol to leach out the stain taken by it. This leached out solution was then evaluated for colour intensity. The frequency of the spectrophotometer was set by setting the maximum absorbance at 635 nm. The untreated group specimens were used as control. The same procedure was followed to evaluate the colour intensity of the remaining specimens after 1 and 3 months time interval.
The data obtained was then statistically analysed using ANOVA and Tukey’s post hoc analysis.
Results
The results of the present study indicate that for self cure tooth moulding material, there is a significant difference between the staining variables at 1 and 3 months with as values are less than 0.05(0.016) but not significant at 1 week and this is because of variations between the untreated specimens and samples immersed in synthetic saliva + periogard at 1 month and at 3 months the significance is because of variations between the untreated specimens and samples in synthetic saliva + periogard (Table 1). For Protemp 4, there is a statistically significant difference between the 1 week and 3 month groups with value of 0.001 (Table 2). The difference in variation at 1 month is between the untreated specimens and synthetic saliva, synthetic saliva + hexidine and after 3 months the difference is between untreated specimens and synthetic saliva + hexidine, synthetic saliva + periogard but after 1 month the difference between the groups is not significant. For Revotek LC, there is a significant difference in the colour stability only after 3 months. Results indicate that at 3 months the variation is between untreated specimens and synthetic saliva + hexidine and synthetic saliva + periogard (Table 3).
Table 1.
Comparison of colour variation of self cure tooth moulding material at three separate time intervals
| Time | Material | N | Mean | Std. deviation | Mean square | F | Sig. | Post hoc |
|---|---|---|---|---|---|---|---|---|
| 1 week | Untreated specimen | 10 | 0.014 | 0.011284 | 0.000 | 1.894 | 0.148 | 0.295 |
| Synthetic saliva | 10 | 0.023 | 0.017016 | 0.130 | ||||
| Syn + hexidine | 10 | 0.0253 | 0.008655 | 0.442 | ||||
| Syn + periogard | 10 | 0.0216 | 0.003748 | 0.968 | ||||
| Total | 40 | 0.020975 | 0.011626 | 0.992 | ||||
| 1 month | Untreated specimen | 10 | 0.0169 | 0.010105 | 0.000 | 3.942 | 0.016 | 0.882 |
| Synthetic saliva | 10 | 0.0243 | 0.004644 | 0.058 | ||||
| Syn + hexidine | 10 | 0.0244 | 0.004006 | 0.054 | ||||
| Syn + periogard | 10 | 0.0255 | 0.004353 | 0.021 | ||||
| Total | 40 | 0.022775 | 0.006974 | 1.000 | ||||
| 3 months | Untreated specimen | 10 | 0.1722 | 0.017574 | 0.014 | 3.929 | 0.016 | 0.974 |
| Synthetic saliva | 10 | 0.1953 | 0.075789 | 0.979 | ||||
| Syn + hexidine | 10 | 0.2603 | 0.083812 | 0.823 | ||||
| Syn + periogard | 10 | 0.2026 | 0.034645 | 0.011 | ||||
| Total | 40 | 0.2076 | 0.066132 | 0.669 |
Table 2.
Comparison of colour variation of Protemp 4 at three separate time intervals
| Time | Material | N | Mean | Std. deviation | Mean square | F | Sig. | Post hoc |
|---|---|---|---|---|---|---|---|---|
| 1 week | Untreated specimen | 10 | 0.0082 | 0.00286 | 0.001 | 6.629 | 0.001 | 0.016 |
| Synthetic saliva | 10 | 0.0252 | 0.015433 | 0.006 | ||||
| Syn + hexidine | 10 | 0.027 | 0.00811 | 0.002 | ||||
| Syn + periogard | 10 | 0.0298 | 0.016178 | 0.987 | ||||
| Total | 40 | 0.02255 | 0.014338 | 0.826 | ||||
| 1 month | Untreated specimen | 10 | 0.0239 | 0.006262 | 0.000 | 2.370 | 0.087 | 0.953 |
| Synthetic saliva | 10 | 0.0318 | 0.008817 | 0.328 | ||||
| Syn + hexidine | 10 | 0.0352 | 0.015894 | 0.084 | ||||
| Syn + periogard | 10 | 0.0335 | 0.0072 | 0.175 | ||||
| Total | 40 | 0.0311 | 0.010791 | 0.880 | ||||
| 3 months | Untreated specimen | 10 | 0.1395 | 0.010865 | 0.085 | 32.997 | <0.001 | 0.982 |
| Synthetic saliva | 10 | 0.3124 | 0.070921 | 0.982 | ||||
| Syn + hexidine | 10 | 0.3373 | 0.052362 | <0.001 | ||||
| Syn + periogard | 10 | 0.3195 | 0.049552 | <0.001 | ||||
| Total | 40 | 0.277175 | 0.094614 | <0.001 |
Table 3.
Comparison of colour variation of Revotek LC at three separate time intervals
| Time | Material | N | Mean | Std. deviation | Mean square | F | Sig. | Post hoc |
|---|---|---|---|---|---|---|---|---|
| 1 week | Untreated specimen | 10 | 0.0249 | 0.004818 | 0.000 | 1.623 | 0.201 | 0.416 |
| Synthetic saliva | 10 | 0.0301 | 0.009927 | 0.240 | ||||
| Syn + hexidine | 10 | 0.0313 | 0.007304 | 0.266 | ||||
| Syn + periogard | 10 | 0.0311 | 0.006967 | 0.984 | ||||
| Total | 40 | 0.02935 | 0.007655 | 0.991 | ||||
| 1 month | Untreated specimen | 10 | 0.0309 | 0.017867 | 0.000 | 0.120 | 0.948 | 1.000 |
| Synthetic saliva | 10 | 0.0324 | 0.015841 | 0.998 | ||||
| Syn + hexidine | 10 | 0.0361 | 0.029983 | 0.938 | ||||
| Syn + periogard | 10 | 0.0337 | 0.012401 | 0.989 | ||||
| Total | 40 | 0.033275 | 0.019449 | 0.976 | ||||
| 3 months | Untreated specimen | 10 | 0.2121 | 0.065212 | 0.021 | 5.314 | 0.004 | 0.999 |
| Synthetic saliva | 10 | 0.3003 | 0.046992 | 0.993 | ||||
| Syn + hexidine | 10 | 0.3124 | 0.044672 | 0.018 | ||||
| Syn + periogard | 10 | 0.2965 | 0.086374 | 0.006 | ||||
| Total | 40 | 0.280325 | 0.0728 | 0.025 |
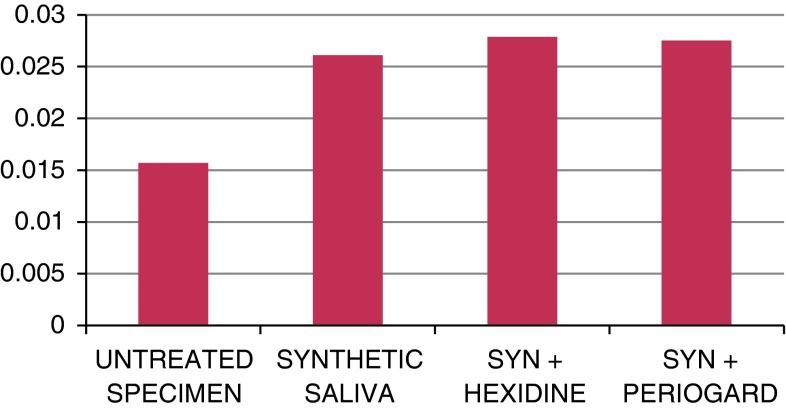
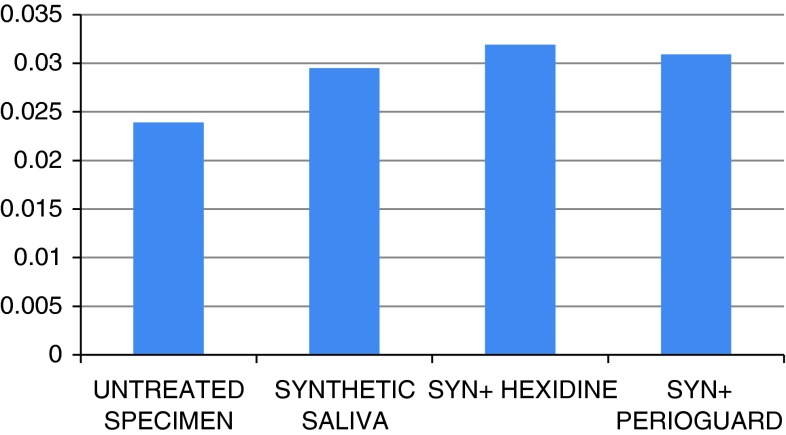
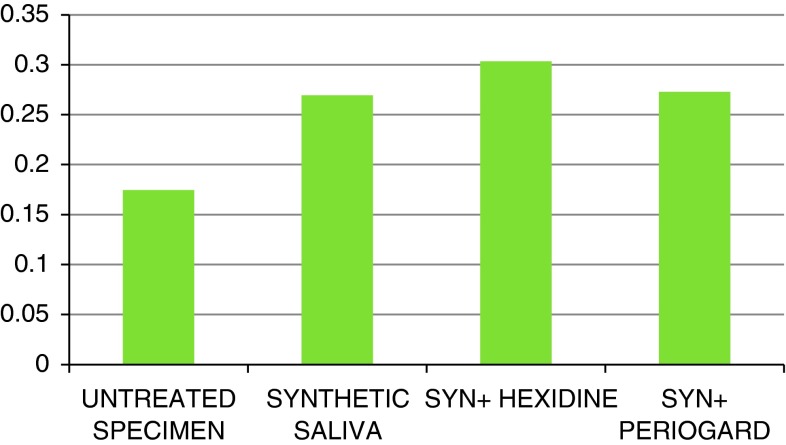
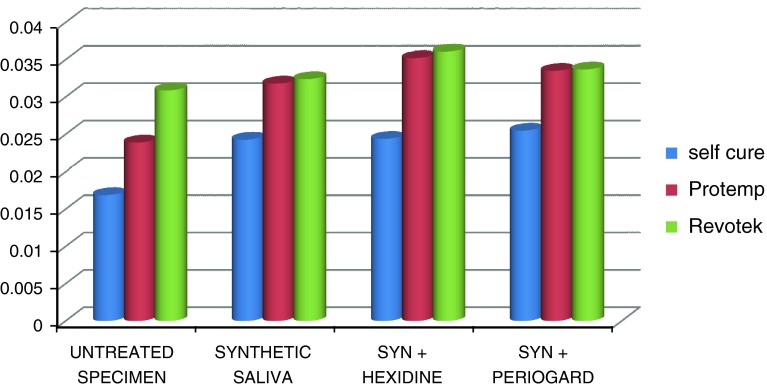
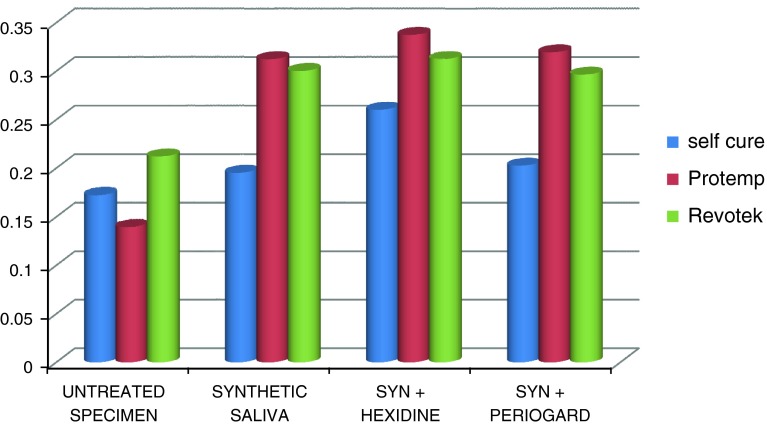
Results of the present study depict that at 1 week, based on the mean spectrophotometric values, synthetic saliva stains the least. But comparing the two mouth rinses, synthetic saliva + periogard has a less potential to stain when compared to synthetic saliva + hexidine (Graph 1). After 1 month, synthetic saliva alone stains the least and when the two mouth rinses are compared, the staining caused by synthetic saliva + periogard is less than synthetic saliva + hexidine (Graph 2). And after 3 months, synthetic saliva stains least. Synthetic saliva + hexidine stains maximum followed by synthetic saliva + periogard (Graph 3).
Graph 1.
Staining caused by various solutions at 1 week
Graph 2.
Staining caused by various solutions at 1 month
Graph 3.
Staining caused by various solutions at 3 months
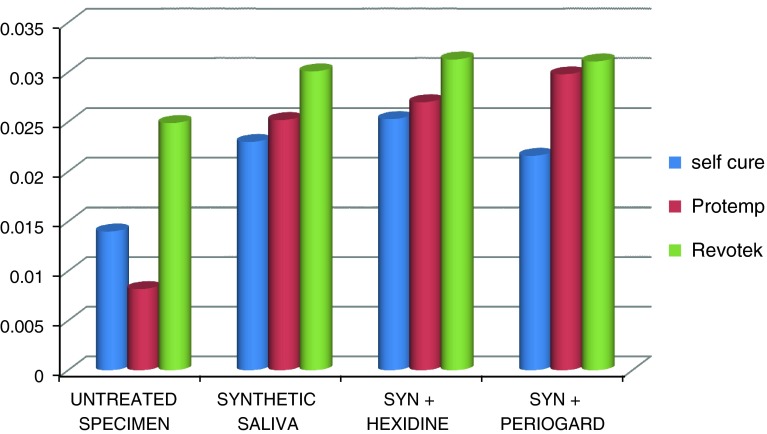
Graphs 4, 5 and 6 show the change in stain taken up by each material in various staining solutions at 1 week, 1 and 3 months respectively and does not depict the comparison of stain taken up by different materials with each other as this depends on the composition and property of the material and hence cannot be compared. Colour taken up by each material is compared with the untreated specimen (control group).
Graph 4.
Stain taken up by each material in different staining solutions after 1 week
Graph 5.
Stain taken up by each material in different staining solutions after 1 month
Graph 6.
Stain taken up by each material in different staining solutions after 3 months
After 1 week, for self cure tooth moulding, synthetic saliva has the least staining potential, followed by synthetic saliva + periogard and synthetic saliva + hexidine. For Protemp 4, after 1 week synthetic saliva stains least and then synthetic saliva + hexidine and highest staining is cause by synthetic saliva + periogard but for Revotek LC, after 1 week, least staining is by synthetic saliva, followed by synthetic saliva + periogard and maximum staining by synthetic saliva + hexidine (Graph 4). After 1 month, for self cure tooth moulding material, synthetic saliva has the least staining potential and this is almost equal to the stain produced by synthetic saliva + hexidine. Significant amount of staining is produced by synthetic saliva + periogard. For Protemp 4, the least staining is caused by synthetic saliva, followed by synthetic saliva + periogard and synthetic saliva + hexidine. The maximum staining for Revotek LC is produced by synthetic saliva + hexidine and least by synthetic saliva with intermediate being synthetic saliva + periogard (Graph 5). After 3 months, for self cure tooth moulding material, synthetic saliva has the least staining potential which is almost similar to the stain produced by synthetic saliva + periogard. The highest stain is produced by synthetic saliva + hexidine. For Protemp 4, the maximum stain is caused by synthetic saliva + hexidine and least stain by synthetic saliva alone with synthetic saliva + periogard causing an intermediate staining. With respect to Revotek LC, the maximum staining potential is shown with synthetic saliva + hexidine and least by synthetic saliva which is almost similar to the discoloration caused by synthetic saliva + periogard (Graph 6).
Discussion
The prime concern of patients during any restorative procedure is esthetics and function. Provisional restorations are intended for the time between tooth preparation and before the fit and insertion of the final prosthesis. Even during the time when provisional restorations are being present in the mouth, esthetics is of importance. Along with restoration of function, colour stability of these provisional restorative materials also becomes an important consideration during prosthodontic rehabilitation when involving an esthetic zone or when intended to be worn for extended periods of time.
The most routinely used group of material in the market is a group of bisacrylate composites. Comparable with composites routinely used for definitive restorations, these materials consist of an organic matrix and inorganic fillers. Monomers such as bisphenol-A-glycidyl methacrylate (bis-GMA), triethylene glycol dimethacrylate or similar monomer systems derived from Bowen resin are also used. Introduction of these bisacrylate systems for temporary restorations lead to improved mechanical properties, lower setting temperature and reduced polymerization shrinkage as well as good polishability.
Provisional crowns are typically fabricated from one of the available methyl or bisacrylate resins, each of them having a slightly different proprietary chemistry and properties. Regardless of their chemistry, dental polymers do undergo a certain amount of adsorption of the liquids from the surrounding environment and hence tend to change colour over time. Discolorations of restorative materials could be due to various factors such as food colorants, drinks, oral habits or even mouth rinses that are commonly prescribed to patients for maintenance of a healthy oral environment.
Various studies have been documented in the literature on the colour stability of different provisional crown materials with numerous colouring agents. This study has been designed to significantly evaluate the colour stability of three commercially available provisional restorative materials in two different mouth rinses and also their difference at varying time intervals.
Discoloration can be evaluated visually and by instrumental techniques (spectrophotometer and colorimeter). The colour perception by visual assessment is subjective, physiologic process that tends to vary from person to person. Variability is a result of factors like illuminant position, object being observed, colour characteristics of the illuminant, fatigue, aging, metamerism, and also the environment state [9, 10]. Use of a standardized instrument would potentially eliminate such errors. A spectrophotometer has been found to be a reliable tool for such measurements [11].
Analysis of variance or ANOVA is the statistical test used along with post hoc analysis. ANOVA is useful in comparing two or more means and finding if the difference is statistically significant. Post Hoc tests are designed for situations in which the researcher has already obtained a significant F test with a factor that consists of three or more means and additional exploration of the differences among the means is needed to provide specific information on which means are significantly different from each other.
Based on the spectrophotometric values obtained in this study, after 1 week, 1 month and also after 3 months, synthetic saliva + hexidine had a greater staining potential when compared to synthetic saliva alone or synthetic saliva + periogard, irrespective of the material being used. Significant difference in the staining was caused at 1 week and 3 months with ANOVA values <0.001.
Considering the clinical implications of this study, the colour stability of various provisional crown materials in mouth rinses was compared with synthetic saliva. The spectrophotometric values showed that after 1 week, self cure tooth moulding material and Revotek LC was stained least by synthetic saliva + periogard but for Protemp 4, synthetic saliva + hexidine stained less.
After 1 month, self cure tooth moulding was stained least by synthetic saliva + hexidine but Protemp 4 and Revotek LC were least stained by synthetic saliva + periogard. The values after 3 months revealed that synthetic saliva + periogard had the least staining potential for self cure tooth moulding material, Protemp 4 and Revotek LC.
According to the results of the present study, Revotek LC was the most colour stable provisional crown material for 1 week and after 1 month time interval and this is in agreement with the results of the study conducted by Gupta and Gupta [12]. Significant colour change was seen when Revotek LC was tested for 3 months. This result of the present study was similar to the conclusion drawn by Guler et al. [3].
At 1 month, self cure tooth moulding material was found to be least colour stable which is similar to the results obtained by Gupta and Gupta [12]. Colour change exhibited by self cure (methyl methacrylates) in comparison to bis-acryl groups may be due to higher water sorption. According to Braden et al. [13], uptake of water by a resin composite is a diffusion controlled process and occurs largely in resin matrix. Diffusion coefficient is usually lower in composites than methyl methacrylate because of higher cross-linked nature of former leading to lower water sorption. The lower colour stability of poly methyl methacrylates could be due to higher resin content and porosities. Self cure tooth moulding (polymethyl methacrylate resins) materials have acceptable mechanical properties but, these materials are subjected to absorption and adsorption of liquids resulting in discoloration. Pigments from food, beverages and drugs get deposited in the interprismatic spaces of the resin leading to compromised esthetics. Moreover, composite is auto-mixed by a dispenser gun instead of hand manipulation. This reduces the amount of air entrapment and porosity leading to higher colour stability.
In the present study, the staining ability of two mouth rinses namely hexidine and periogard were also evaluated. Results of this study indicate that synthetic saliva + hexidine stain more when compared to synthetic saliva + periogard, after 1 week, 1 month and even 3 months. Staining may be the result of the destruction mechanism of alcohol containing mouth rinses.
The present study does not compare the stain taken up by individual materials in various staining solutions with each other but compares the colour stability at different time intervals separately for each material as the colour stability depends on the material composition and properties.
Alcohol has been attributed to softening of polymer matrix that result in partial removal of the surface layer. Removal of the resin matrix result in the degradation of the filler-matrix interface, which contributed to decrease in hardness values [14, 15] and may also contribute to the colour change. But Gurgan et al. [16] showed that irrespective of alcohol concentrations, both alcohol containing and alcohol free mouth rinses affect the hardness of resin-restorative material.
Three commonly used provisional crown materials were used in the present study and evaluated for their colour stability in different mouth rinses at varying time intervals. Based on the results of the present study, Revotek LC was found to be the most colour stable material compared to other two materials and alcohol containing mouth rinse caused maximum discoloration of the provisional restorative materials.
Limitations of the Study
In the present study, to evaluate the colour taken up by each specimen, 99 % ethanol was used to leach out the stain from the specimens and then this solution was used to measure the colour intensity using a spectrophotometer. This procedure being an indirect method has the probability to induce some error in the study as compared to a direct method.
Since exact simulation of the oral environment is difficult in an in vitro study, the present study results would have been affected. In the present study the specimens are in contact with various staining solutions for different time intervals and the result depicts the potentiality of the provisional restorative materials to discolour and the staining characteristics of various mouth rinses. However, along with in vivo considerations for the time span of actual duration of contact during mouth rinsing protocols, further in vivo studies might be required in the same context to evaluate the exact colour change in the oral environment.
Conclusion
Within the limitations of the study, the following conclusions could be drawn:
Among the three provisional restorative materials, Revotek LC was found to be the most colour stable material at varying time intervals.
Evaluation of the staining ability of the mouth rinses revealed that hexidine had more staining potential compared to periogard.
According to the results of the present study, it can be concluded that self cure tooth moulding material showed significant staining and least stain was taken up by Revotek LC.
According to the results of the present study, periogard had the least staining potential.
References
- 1.Crispin BJ, Caputo AA. Color stability of temporary restorative materials. J Prosthet Dent. 1979;42(1):27–33. doi: 10.1016/0022-3913(79)90326-3. [DOI] [PubMed] [Google Scholar]
- 2.Sham AS, Chu FC, Chai J, Chow TW. Color stability of provisional prosthodontic materials. J Prosthet Dent. 2004;91(5):447–452. doi: 10.1016/j.prosdent.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 3.Guler AU, Yilmaz F, Kulunk T, Guler E, Kurt S. Effects of different drinks on stainability of resin composite provisional restorative materials. J Prosthet Dent. 2005;94(2):118–124. doi: 10.1016/j.prosdent.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Caroni C, Yannikakis SA, Zissis AJ, Polyzois GL. Color stability of provisional resin restorative materials. J Prosthet Dent. 1998;80(5):533–539. doi: 10.1016/S0022-3913(98)70028-9. [DOI] [PubMed] [Google Scholar]
- 5.Seghi RR, Gritz MD, Kim J. Colorimetric changes in composites resulting from visible-light-initiated polymerization. Dent Mater. 1990;6(2):133–137. doi: 10.1016/S0109-5641(05)80044-2. [DOI] [PubMed] [Google Scholar]
- 6.Yannikakis SA, Zissis AJ, Polyzois GL, Caroni C. Color stability of provisional resin restorative materials. J Prosthet Dent. 1998;80(5):533–539. doi: 10.1016/S0022-3913(98)70028-9. [DOI] [PubMed] [Google Scholar]
- 7.Luce MS, Campbell CE. Stain potential of four microfilled composites. J Prosthet Dent. 1988;60(2):151–154. doi: 10.1016/0022-3913(88)90305-8. [DOI] [PubMed] [Google Scholar]
- 8.Stober T, Gilde H, Lenz P. Color stability of highly filled composite resin. Dent Mater. 2001;17(1):87–94. doi: 10.1016/S0109-5641(00)00065-8. [DOI] [PubMed] [Google Scholar]
- 9.Wyszecki G, Fielder GH. Color difference matches. J Opt Soc Am A. 1971;61:1501–1513. doi: 10.1364/JOSA.61.001501. [DOI] [PubMed] [Google Scholar]
- 10.Billmeyer FW, Saltzman M. Observer metamerism. Color Res Appl. 1980;5:72. doi: 10.1002/col.5080050203. [DOI] [Google Scholar]
- 11.Brewer DJ, Wee A, Seghi R. Advances in color matching. Dent Clin N Am. 2004;48:341–358. doi: 10.1016/j.cden.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Gupta G, Gupta T. Evaluation of the effect of various beverages and food material on the color stability of provisional materials: an in vitro study. J Conserv Dent. 2011;14(3):287–292. doi: 10.4103/0972-0707.85818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braden M, Causton EE, Clarke RL. Diffusion of water in composite filling material. J Dent Res. 1976;55:730–732. doi: 10.1177/00220345760550050501. [DOI] [PubMed] [Google Scholar]
- 14.Soderholm K. Relationship between compressive yield strength and filler fractions of PMMA composites. Acta Odontol Scand. 1982;40(3):145–150. doi: 10.3109/00016358209012723. [DOI] [PubMed] [Google Scholar]
- 15.Soderholm K, Robert MJ. Influence of water exposure on tensile strength of composites. J Dent Res. 1990;69:1812–1816. doi: 10.1177/00220345900690120501. [DOI] [PubMed] [Google Scholar]
- 16.Gurgan S, Onen A, Koprulu H. In vitro effects of alcohol-containing and alcohol-free mouth rinses on microhardness of some restorative materials. J Oral Rehabil. 1997;24(3):244–246. doi: 10.1111/j.1365-2842.1997.tb00321.x. [DOI] [PubMed] [Google Scholar]