Abstract
Background: Germany, like many other countries, will soon have a shortage of qualified doctors. One reason for the dissatisfaction amongst medical residents are the relatively unstructured residency training programs despite increasing importance of outcome-based education. The aim of our study was to identify characteristics and requirements for good teaching during anesthesiology residency training from the resident’s point of view.
Methods: A consensus workshop with residents from all medical universities in Germany was held. Participants were allocated to one of the three topics, chosen based on a 2009 nationwide evaluation of residency. The three topics were (A) characteristics of helpful/good teachers, (B) characteristics of helpful/good conditions and (C) characteristics of helpful/good curricular structure. Each group followed a nominal group technique consensus process to define and rank characteristics for a good residency.
Results: 31 (79.5%) resident representatives were present. The consented results put emphasis on the importance of structured curricula including transparent goals and objectives, in training formative assessments and quality assurance measures for the program. Residents further long for trained trainers with formal teaching qualifications and protected teaching time.
Conclusions: Good residency training requires careful consideration of all stakeholders’ needs. Results reflect and extend previous findings and are at least to some degree easily implemented. These findings are an important step to establish a broader consensus within the discipline.
Keywords: residents, curriculum development, needs assessment, anesthesiology, consensus
Zusammenfassung
Hintergrund: In Deutschland wird es, wie in vielen Ländern, in absehbarer Zukunft einen Mangel an qualifizierten Ärzten geben. Einer der Gründe für Unzufriedenheit unter den Weiterbildungsassistenten sind die relativ unstrukturierten Weiterbildungsprogramme trotz der zunehmenden Wichtigkeit von Ergebnis-orientierter Weiterbildung. Ziel dieser Studie ist es, Charakteristika von und Anforderungen an gute Lehre während der anästhesiologischen Facharztweiterbildung aus Sicht der Weiterzubildenden zu identifizieren.
Methoden: Es wurde eine Konsensus-Konferenz mit Weiterzubildenden von allen 39 anästhesiologischen Universitätskliniken Deutschlands durchgeführt. Die Teilnehmer wurden Gruppen zu einem von drei Themen zugeordnet, die anhand der nationalen Evaluation der Weiterbildung 2009 identifiziert wurden. Diese Themen waren (A) Charakteristika hilfreicher/guter Weiterbildner, (B) Charakteristika hilfreicher/guter Bedingungen und (C) Charakteristika hilfreicher/guter Curriculumsstruktur. Jede Gruppe folgte dem Nominal-Group-Technik-Konsensprozess, um Charakteristika guter Weiterbildung zu definieren und zu priorisieren.
Ergebnisse: 31 (79,5%) Assistentensprecher waren anwesend. Die Ergebnisse betonen die Bedeutung strukturierter Curricula inklusive transparenter Ziele und Inhalte, formativer Zwischenprüfungen und Qualitätssicherungsmaßnahmen der Programme. Weiterbildungsassistenten wünschen sich zudem ausgebildete Weiterbildende mit formaler Lehrqualifikation und geschützte Zeit zum Lehren.
Schlussfolgerung: Gute Facharztweiterbildung setzt eine sorgfältige Berücksichtigung der Bedürfnisse aller Beteiligten voraus. Die Ergebnisse bestätigen und erweitern bisherige Publikationen und können zum Teil einfach umgesetzt werden. Die Ergebnisse sind ein wichtiger Schritt hin zu einem breiteren Konsens innerhalb einer Fachdisziplin.
Introduction
Germany, like many other countries, will soon have a shortage of qualified doctors. Many possible reasons for this shortage are discussed in the literature: The current generation of medical students (generation Y) are unlikely to accept poor training conditions. They may well leave the hospital or indeed the country to get better training [1], [2], [3]. Hospitals currently react to these new challenges with random isolated measures [3].
New planning tools are necessary to cope with the challenges medicine and especially anesthesiology will face in the future. Outcome-based education has become the gold standard in curriculum development for residency training [4], curricula focus on outcomes and their description [5]. Many countries have already developed a structured outcome-based curriculum for various levels of training (e.g., for specialties and subspecialties) in order to assure high quality of future health care [4], [6], [7], [8]. In Germany the German Association for Medical Education (Gesellschaft fuer Medizinische Ausbildung (GMA)) and The Council of Medical Faculties (Medizinischer Fakultaetentag (MFT)) have begun to develop a competency-based catalogue of learning objectives to inform undergraduate medical education [9]. A catalogue for the purpose of residency training is planned by the same Association [10].
In 2009 the German Medical Council (Bundesaerztekammer) conducted the first nationwide evaluation of residency training in all medical subspecialties including residency trainers and residents. The evaluation was conducted analogous to German school marks (1 = excellent, 6 = poor). Global rating of residency training was fairly good with 2.54. There were eight question domains (global rating, medical expert teaching, learning culture, leadership, culture of error prevention, culture of decision making, workplace culture, application of evidence-based medicine). Compared to all specialties, anaesthesiology performed below average in seven of the eight question domains. Only “management of medical errors” received higher-than-average ratings. The nationwide evaluation identified different fields where need for change was deemed necessary:
Trainers: need to develop a tutor system for residency, train the trainer programs for clinical teachers.
Conditions: need to develop family friendly hourly working schedule, optimization of pathways in hospitals and within a specialty department.
Curriculum: need to develop well-structured residency training curricula, publication of best practice models, reform of residency training regulations, possibility of residency training programs or rotations to different sites as part of a network [11], [12].
The follow-up survey in 2011 showed only slightly better results with the same pattern [13].
Given this situation there is a need for more structured approaches to curriculum development in Germany including development of appropriate learning goals, implementation and assessment as well as quality assurance of graduate medical education on a national level [10]. According to Kern different stakeholders have to be involved in this task. Societal and patient needs should be taken into account as well as the needs of clinical teachers, residents and employers [14]. While the needs of teachers, medical societies and employers at least partly manifest through council regulations of residency training programs, patient as well as residents needs are generally less frequently sought. We approached one of these groups to contribute to the necessary discussion.
The aim of our study was to identify characteristics and requirements of good teaching in anaesthesiology residency training from the resident’s point of view. We conducted a focused general needs assessment in the specialty of anaesthesiology as defined by Kerns six-step approach to curriculum development [14].
Methods
In order to generate a generic list of characteristics and requirements for all three main topics of the above mentioned nationwide evaluation we conducted a consensus workshop for residents. It took place during one of the main conferences of the German Association of Anesthesiologists (Deutsche Gesellschaft fuer Anaesthesiologie und Intensivmedizin) in Berlin in September 2011 (13. Hauptstadtkongresses der Deutschen Gesellschaft fuer Anaesthesiologie und Intensivmedizin).
Sample (participants)
To maximize legitimacy we invited one elected resident representative (Assistentensprecher) from all 39 German departments of anesthesiology at university hospitals [15]. The invitation was carried out in three steps: All anesthesiology departments at university hospitals were asked by e-mail to send one of their resident representatives to the workshop. In a second step all institutions that hadn’t replied were reminded by a second e-mail and asked to send one of their resident representatives or a substitute. In a third step all resident representatives of non-responding institutions were contacted personally by WB by e-mail or phone and asked to attend or send a substitute. All workshop participants gave their written consent to publish the data gained in the consensus process as well as aggregated participant information. Ethical approval was deemed unnecessary for this workshop in our institution.
Workshop preparation and topics
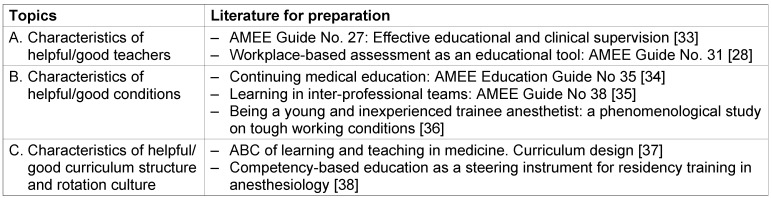
Participants were informed two weeks prior to the workshop about the three topics of the workshop (see Table 1 (Tab. 1)), were asked to subscribe to one of the three workshop groups and to provide a preference list of the given main topics in case the preferred group could not be allocated to everyone. Workshop places were allocated on a first come first served basis, everyone was allocated to the group of their first choice (see Table 1 (Tab. 1)). To familiarize participants with concepts and current debates in their topic all participants received two to three articles to prepare for the workshop five days before the workshop took place (see Table 1 (Tab. 1)). Selected articles were reviews and related to the group topics as well as articles focused on residency training in anesthesiology related to group topics.
Table 1. Topics and literature for preparation.
Instruments: Workshop and Nominal Group Technique
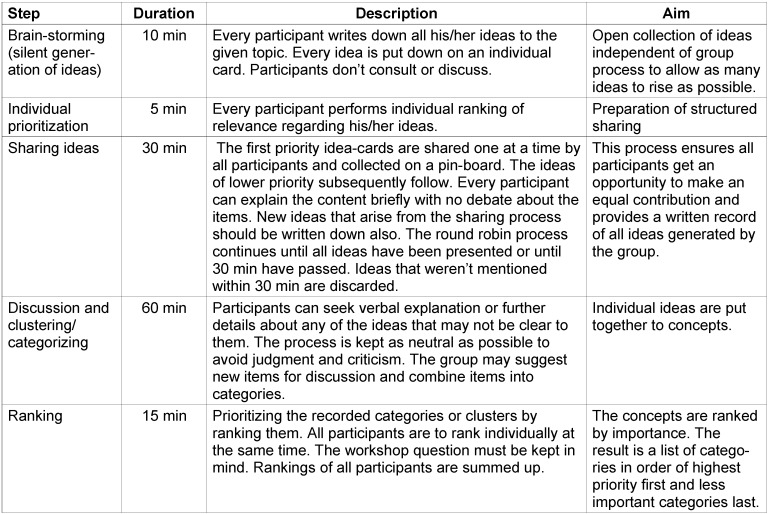
The workshop was divided into three parts from noon to 5.30 pm. After a brief welcome and introduction we stated the workshop goal: to identify characteristics and requirements for good residency training in anaesthesiology from the resident’s point of view. We split the group into the three working groups covering the topics (A) characteristics of helpful/good teachers, (B) characteristics of helpful/good conditions and (C) characteristics of helpful/good curricular structure and rotation culture. Each group was facilitated by at least one anesthesiologist and a second facilitator. At least one of the facilitators per group was familiar with the Nominal Group Technique (NGT) method and had applied it previously in other workshops. Groups were obliged to use the NGT to steer the workshop as recommended for clinical guideline development [16], [17], [18], [19]. The NGT consists of five steps: (1) brainstorming, (2) prioritizing, (3) collection of ideas, (4) discussion and clustering, (5) ranking (see Table 2 (Tab. 2)). The result of the NGT is a prioritized list of idea-clusters and concepts. At the top of the list is the idea-cluster with the highest ranking priority followed by all idea-clusters in decreasing priority. In part three of the workshop, group results were presented to all participants and discussed in a plenary session. Group results could only be changed from the plenary if there was consensus that there is strong concern of misunderstanding within the group results. All participants consented to the results.
Table 2. The five stages of nominal group technique used during the workshop [16], [17], [19], duration and aim in the described consensus process.
Statistics
Data were collected by photography and manually transcribed. Descriptive statistics were carried out using SPSS version 20.
Results
Sample (participants)
31 (79.5%) resident representatives (or their substitute) out of 39 invited participants were present during the consensus process. 14 (45.2%) participants were female and 17 (54.8%) were male. Five (16.1%) of the participants had already passed the anesthesiology specialty examination.
Mean time of residency duration (excluding the candidates that had already passed their specialty examinations) was 3.16 years (median 4, minimum 2, maximum 7) out of a 5-year program. Only one participant had children.
Consensus process
During the plenary presentation of the group results and the consensus discussion, the topic “patient safety” was heavily debated. Some groups had listed “patient safety” amongst their results. The plenary group discussed whether it was suitable to allocate “patient safety” to a prioritizing list even if this was not listed as the first priority. Patient safety was stressed as an overarching theme of residency training which was not explicitly matching any other specific category and therefore removed from the prioritizing lists to avoid misunderstanding. This was the only topic on which the plenary made a change to the results of the groups.
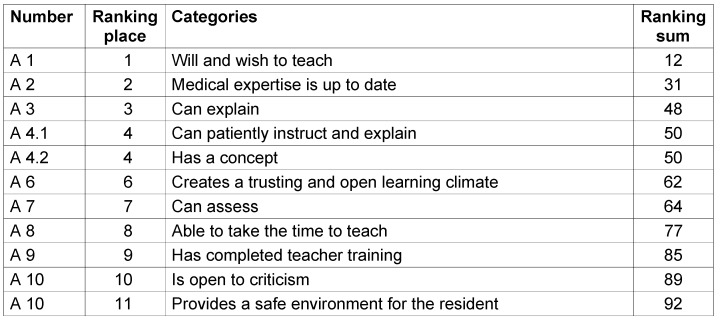
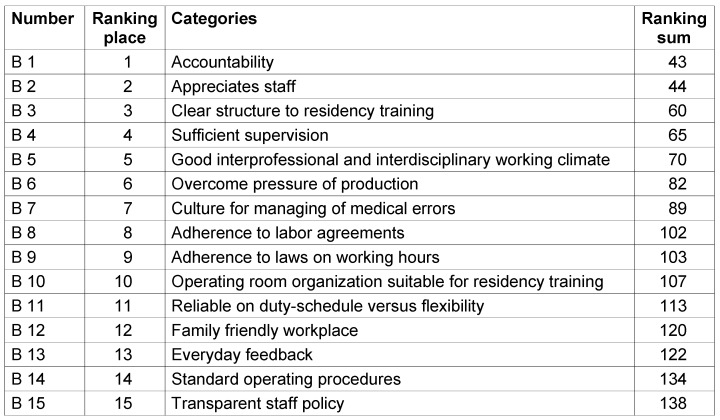
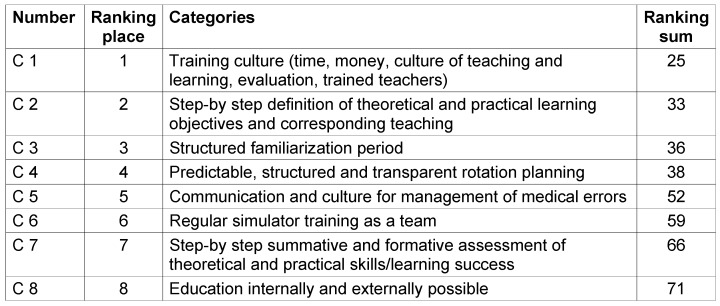
Group A worked on the topic “characteristics of helpful/ good teachers” and developed eleven categories. Fifteen categories were developed by Group B on the topic “characteristics of helpful/good conditions”. Group C worked on the topic “characteristics of helpful/good curricular structure and rotation culture” and developed eight categories. The consented categories of group A, B and C with a ranking sum and in ranking order are summarized in Table 3 (Tab. 3), Table 4 (Tab. 4) and Table 5 (Tab. 5).
Table 3. Results of group A “characteristics of helpful/good teachers”.
Table 4. Results of group B “characteristics of helpful/good conditions”.
Table 5. Results of group C “characteristics of helpful/good curricular structure and rotation culture”.
Discussion
We were able to ensure a broad consensus within the group of workshop participants on the key characteristics for a good residency. The results give a broad overview of possible changes suggested by residents and a lot of the prioritized characteristics for a good residency would require little effort to put into action. Although the ranking orders are not equidistant, they provide an order of more and less importance.
Our results elaborate on the needs and expectations of generation Y. Most of the results from group A on the characteristics of helpful/good teacher like “Can patiently instruct and explain”, “Creates a trusting and open learning climate” as well as the results B2 “Appreciates staff” and B5 “Good interprofessional and interdisciplinary working climate” of group B on the characteristics of helpful/good conditions strengthen the introductory claim, that medical students and junior residents especially from generation Y are not willing to accept poor training conditions.
The reported need for development of appropriate and transparent learning goals and structure [10] is reflected in our findings. Namely in the results A 4.2 “Has a concept”, B3 “Clear structure to residency training” and C1 to C3 “Training culture”, “Step-by step definition of theoretical and practical learning objectives and their teaching”, “Structured familiarization period”. These requirements are not met in all programs as the nationwide surveys by the Bundesaerztekammer demonstrates [11], [12], [13]. The results also confirm and extend previous findings on residency training in the specialty of anesthesiology [20], [21], [22], [23]. One survey of 770 residents at German hospitals revealed that only about one third of residents are able to find a structure in their training program [23]. In the most recent survey, only 42.2% of residents rated their training program as structured [24]. This situation is unsatisfactory, as one would assume that well-structured residency curricula would facilitate a more effective learning environment, followed by enhanced clinical practice and improved patient safety in future generations of physicians [25], [26]. Necessary changes in this domain are relatively easy to achieve and are inexpensive. They might be implemented by political will in single hospitals.
The topic of implementation and assessment of competency-based graduate medical education [10] is reflected in A7 “Can assess” and C7 “Step-by step summative and formative assessment of theoretical and practical skills/learning success”. Changes in assessment methods like performance testing, namely OSCE and portfolio [27], workplace-based assessment e.g. using DOPS or Mini-CEX [28] or even multi source feedback [29], [30] and others need content experts, are labor intensive and therefore need nationwide initiatives and financial support.
The important aspect of quality assurance of graduate medical education [10] is reflected in the following findings: “Predictable, structured and transparent rotation planning”, B1 “Accountability”, as well as A9 “Has completed teacher training”. Taking into account that hospitals are not reimbursed for residency training in the German medical system, departments can rarely afford staff specifically dedicated to clinical teaching and supervision.
The proposed changes may only be feasible if they are developed and implemented nationally to save costs. Financial support to develop more structured curricula and provide more supervision seems necessary as Ertmer reports a decrease in clinical supervision of anaesthesiology residents in German hospitals [24].
Further research and regular program evaluation is needed to reveal which measures are more educationally and financially effective than others [10].
There are several limitations to the interpretation of the presented data. We invited only one elected resident representative (Assistentensprecher) per anesthesiology department from all German university hospitals. Their point of view may vary from residents trained in smaller hospitals. In the most recent anesthesiology survey 32% of residents were trained in small hospitals (Regelversorgung), 39% at large hospitals with all subspecialties, 29% at university hospitals [24].
In addition, only one of the participants had children, which may explain why family friendliness at the workplace does not seem to be of great importance in our results. Mean time of residency duration in our study population was slightly above three years out of a five-year program. 45.2% of our participants were female. These aspects might play a role in preferences. A Swiss survey reported that career related issues became less important for specialty choice with advancing training status. The same survey reported work- and time-related aspects are more important for women than for men. With an increasing number of female residents, training programs should adapt to this particular aspect [31].
Furthermore, we only asked residents and not teachers, representatives of other health care professions or patients to participate in our workshop. We wanted to give residents the opportunity to exclusively give their point of view without being influenced by others. Other studies have shown that clinical faculty and residents at least in family medicine have a shared view of the ideal clinical teacher. The believed ideal clinical teacher for residents and faculty was stimulating, encouraging, competent and communicative; and not conventional, cautious or controlling, a finding well reflected in the results of our workshop group A. They only differed in the descriptors “Probing” and “Innovative”, both more important for faculty than for residents, thus differences in views might be minimal [32].
The next step to develop quality residency in German anesthesiology could be a nationwide Delphi process involving at least residents and resident teachers to accomplish a broader consensus and in order to involve and motivate people that are involved in everyday teaching in the hospitals. Delphi processes are shown to be effective and recommended in other curriculum development processes [14], [18], [19].
The results of our workshop were presented in a scientific session to senior faculty staff during the congress in which the workshop took place: the reception of results and the following discussion showed a general agreement with the presented findings among the auditorium and conveyed their encouragement to proceed in seeking consensus from a larger group of stakeholders. It would be beneficial to involve other healthcare professionals and patients in such a process if deemed feasible.
Conclusions
Good residency training curricula require careful consideration of all stakeholders’ needs. Characteristics of good residency as defined by residents are at least to some degree easy to implement and reflect previous findings from the literature. These preliminary findings are an important stepping stone in establishing a broader consensus within the discipline.
Notes
Authorship
HO and WEB contributed equally to this article.
Acknowledgements
The authors thank the German Association of Anesthesiologists (Deutsche Gesellschaft fuer Anaesthesiologie und Intensivmedizin) and the organizers of the congress (Hauptstadtkongress für Anaesthesie und Intensivmedizin), especially Dr. Dominik Mittler, for the possibility to conduct the consensus process in the context of the conference. We thank Dr. Eva Kornemann, Dr. Jochen Öltjenbruns and Dr. Andreas Kopf of the Department of Anesthesiology at Charité Berlin for their support during the preparation of the workshop. We thank Dr. Max Skorning, Department of Anesthesiology, University Hospital Aachen for his presentation on the work of the group “young anesthesia” of the German Association of Anesthesiologists.
We especially thank the participants of the consensus process for their dedicated and creative work and their support during the presentation of the workshop results at the congress meeting.
We would further like to thank Stephanie Matthews of the skills lab at Charité Berlin, Ara Tekian, Department of Medical Education, University of Illinois at Chicago and two anonymous reviewers for their constructive critique of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Disclosure of funding
German Association of Anesthesiologists (Deutsche Gesellschaft fuer Anaesthesiologie und Intensivmedizin), Roritzer Straße 27, 90419 Nuremberg funded travel costs and conference fees for participants.
References
- 1.Schlitzkus LL, Schenarts KD, Schenarts PJ. Is your residency program ready for Generation Y? J Surg Educ. 2010 Mar-Apr;67(2):108–111. doi: 10.1016/j.jsurg.2010.03.004. Available from: http://dx.doi.org/10.1016/j.jsurg.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Bürkle H. X, Y, … Personalmangel. [X, Y, … lack of personnel?]. Anaesthesist. 2011 Jun;60(6):505–506. doi: 10.1007/s00101-011-1904-1. (Ger). Available from: http://dx.doi.org/10.1007/s00101-011-1904-1. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt GN, Fiege M, Goetz AE. Weiterbildung in der Anästhesiologie. Umsetzung am Universitätsklinikum Hamburg-Eppendorf. [Further education in anesthesiology. Implementation at the University Hospital Hamburg-Eppendorf]. Anaesthesist. 2011 Apr;60(4):366–374. doi: 10.1007/s00101-010-1836-1. (Ger). Available from: http://dx.doi.org/10.1007/s00101-010-1836-1. [DOI] [PubMed] [Google Scholar]
- 4.The Royal College of Physicians and Surgeons in Canada. CanMEDS 2005 Framework. 2005. [cited 2005 Oct 30]. Available from: http://www.royalcollege.ca/portal/page/portal/rc/canmeds/framework. [Google Scholar]
- 5.Leung WC. Competency based medical training: review. BMJ. 2002 Sep;325(7366):693–696. doi: 10.1136/bmj.325.7366.693. Available from: http://dx.doi.org/10.1136/bmj.325.7366.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paterson Davenport LA, Hesketh EA, Macpherson SG, Harden RM. Exit learning outcomes for the PRHO year: an evidence base for informed decisions. Med Educ. 2004 Jan;38(1):67–80. doi: 10.1111/j.1365-2923.2004.01736.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2004.01736.x. [DOI] [PubMed] [Google Scholar]
- 7.Ringsted C, Henriksen AH, Skaarup AM, Van der Vleuten CP. Educational impact of in-training assessment (ITA) in postgraduate medical education: a qualitative study of an ITA programme in actual practice. Med Educ. 2004 Jul;38(7):767–777. doi: 10.1111/j.1365-2929.2004.01841.x. Available from: http://dx.doi.org/10.1111/j.1365-2929.2004.01841.x. [DOI] [PubMed] [Google Scholar]
- 8.Brown AK, Roberts TE, O'connor PJ, Wakefield RJ, Karim Z, Emery P. The development of an evidence-based educational framework to facilitate the training of competent rheumatologist ultrasonographers. Rheumatology (Oxford) 2007 Mar;46(3):391–397. doi: 10.1093/rheumatology/kel415. Available from: http://dx.doi.org/10.1093/rheumatology/kel415. [DOI] [PubMed] [Google Scholar]
- 9.Hahn EG, Fischer MR. Nationaler Kompetenzbasierter Lernzielkatalog Medizin (NKLM) für Deutschland: Zusammenarbeit der Gesellschaft für Medizinische Ausbildung (GMA) und des Medizinischen Fakultätentages (MFT) [National Competence-Based Learning Objectives for Undergraduate Medical Education (NKLM) in Germany: Cooperation of the Association for Medical Education (GMA) and the Association of Medical Faculties in Germany (MFT)]. GMS Z Med Ausbild. 2009;26(3):Doc35. doi: 10.3205/zma000627. (Ger). Available from: http://dx.doi.org/10.3205/zma000627. [DOI] [Google Scholar]
- 10.David DM, Euteneier A, Fischer MR, Hahn EG, Johannink J, Kulike K, Lauch R, Lindhorst E, Noll-Hussong M, Pinilla S, Weih M, Wennekes V. The future of graduate medical education in Germany – position paper of the Committee on Graduate Medical Education of the Society for Medical Education (GMA) GMS Z Med Ausbild. 2013;30(2):Doc26. doi: 10.3205/zma000869. Available from: http://dx.doi.org/10.3205/zma000869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eidgenössische Technische Hochschule Zürich (ETH Zürich) – Institute for Environmental Decisions (IED) Consumer Behavior; Bundesaerztekammer. Ergebnisse der Evaluation der Weiterbildung – 1. Befragungsrunde 2009. Bundesrapport. 2010. [[cited 2010 5 Nov]]. Available from: http://www.bundesaerztekammer.de/downloads/EVA_Bundesrapport_final_16042010.pdf. [Google Scholar]
- 12.Hibbeler B, Korzilius H. Evaluation der Weiterbildung: Ein erster Schritt. Dtsch Ärztebl. 2010;107(10):A417–20. [Google Scholar]
- 13.Korzilius H. Evaluation der Weiterbildung: Im Ergebnis eine gute Zwei minus. Dtsch Ärztebl. 2011;108(50):B2250–B2251. [Google Scholar]
- 14.Kern DE, Thomas PA, Hughes MT. Curriculum Development for Medical Education. A Six-Step Approach. 2nd ed. Baltimore: Johns Hopkins University Press; 2009. [Google Scholar]
- 15.Calder J. Survey research methods. Med Educ. 1998 Nov;32(6):638–652. doi: 10.1046/j.1365-2923.1998.00227.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.1998.00227.x. [DOI] [PubMed] [Google Scholar]
- 16.Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften – Ärztliches Zentrum für Qualität in der Medizin. Deutsches Instrument zur methodischen Leitlinien-Bewertung (DELBI) Fassung 2005/2006. 2005. [cited 2006 Jul 11]. Available from: http://www.leitlinien.de/leitlinienqualitaet/leitlinie/delbi/pdf/delbi05.pdf. [Google Scholar]
- 17.Delbecq AL, Van de Ven AH. A Group Process Model for Problem Identification and Program Planning. J Appl Behav Sci. 1975;7(4):466–492. doi: 10.1177/002188637100700404. Available from: http://dx.doi.org/10.1177/002188637100700404. [DOI] [Google Scholar]
- 18.Lloyd-Jones G, Fowell S, Bligh JG. The use of the nominal group technique as an evaluative tool in medical undergraduate education. Med Educ. 1999 Jan;33(1):8–13. doi: 10.1046/j.1365-2923.1999.00288.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.1999.00288.x. [DOI] [PubMed] [Google Scholar]
- 19.Kiessling C, Dieterich A, Fabry G, Hölzer H, Langewitz W, Mühlinghaus I, Pruskil S, Scheffer S, Schubert S Committee Communication and Social Competencies of the Association for Medical Education Gesellschaft für Medizinische Ausbildung; Basel Workshop Participants. Communication and social competencies in medical education in German-speaking countries: the Basel consensus statement. Results of a Delphi survey. Patient Educ Couns. 2010 Nov;81(2):259–266. doi: 10.1016/j.pec.2010.01.017. Available from: http://dx.doi.org/10.1016/j.pec.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 20.Goldmann K, Steinfeldt T, Wulf H. Die Weiterbildung für Anästhesiologie an deutschen Universitätskliniken aus Sicht der Ausbilder – Ergebnisse einer bundesweiten Umfrage. [Anaesthesia education at german university hospitals: the teachers’ perspective – results of a nationwide survey]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2006 Apr;41(4):204–212. doi: 10.1055/s-2006-925367. (Ger). Available from: http://dx.doi.org/10.1055/s-2006-925367. [DOI] [PubMed] [Google Scholar]
- 21.Lehmann KA, Schultz JH. Zur Lage der anästhesiologischen Weiter- und Fortbildung in Deutschland. Ergebnisse einer Repräsentativumfrage. [Anesthesiology education and training in Germany. Results from a representative questionnaire]. Anaesthesist. 2001 Apr;50(4):248–261. doi: 10.1007/s001010170028. (Ger). Available from: http://dx.doi.org/10.1007/s001010170028. [DOI] [PubMed] [Google Scholar]
- 22.Prien T, Siebolds M. Beurteilung der Facharztweiterbildung durch Ärzte in Weiterbildung anhand eines validierten Fragebogens. [Evaluation of medical residency training programmes by residents using a validated questionnaire]. Anaesth Intensivmed. 2004;45(1):25–31. (Ger). [Google Scholar]
- 23.Radtke RM, Hahnenkamp K. Weiterbildung im klinischen Alltag: Bestandsaufnahme und Strategien. [Further education during the daily clinical routine: Stocktaking and strategies]. Anaesth Intensivmed. 2007;48(5):240–250. (Ger). [Google Scholar]
- 24.Hahnenkamp K, Ertmer C, Van Aken H, Skorning M. Praxis der ärztlichen Weiterbildung und Rahmenbedingen im Wandel – Evaluation der Weiterbildung im Fachgebiet Anästhesiologie über einen Zeitraum von fünf Jahren (2006–2011) [Postgraduate education in a changing occupational environment – Evaluation of postgraduate education in anaesthesiology over a period of five years (2006–2011)]. Anaesth Intensivmed. 2012;53(9):452–469. (Ger). [Google Scholar]
- 25.Frank JR, Danoff D. The CanMEDS initiative: implementing an outcomes-based framework of physician competencies. Med Teach. 2007 Sep;29(7):642–647. doi: 10.1080/01421590701746983. Available from: http://dx.doi.org/10.1080/01421590701746983. [DOI] [PubMed] [Google Scholar]
- 26.Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach. 2007 Sep;29(7):648–654. doi: 10.1080/01421590701392903. Available from: http://dx.doi.org/10.1080/01421590701392903. [DOI] [PubMed] [Google Scholar]
- 27.Shumway JM, Harden RM Association for Medical Education in Europe. AMEE Guide No. 25: The assessment of learning outcomes for the competent and reflective physician. Med Teach. 2003 Nov;25(6):569–584. doi: 10.1080/0142159032000151907. Available from: http://dx.doi.org/10.1080/0142159032000151907. [DOI] [PubMed] [Google Scholar]
- 28.Norcini J, Burch V. Workplace-based assessment as an educational tool: AMEE Guide No. 31. Med Teach. 2007 Nov;29(9):855–871. doi: 10.1080/01421590701775453. Available from: http://dx.doi.org/10.1080/01421590701775453. [DOI] [PubMed] [Google Scholar]
- 29.Violato C, Lockyer J, Fidler H. Multisource feedback: a method of assessing surgical practice. BMJ. 2003 Mar;326(7388):546–548. doi: 10.1136/bmj.326.7388.546. Available from: http://dx.doi.org/10.1136/bmj.326.7388.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilkinson TJ, Wade WB, Knock LD. A blueprint to assess professionalism: results of a systematic review. Acad Med. 2009 May;84(5):551–558. doi: 10.1097/ACM.0b013e31819fbaa2. Available from: http://dx.doi.org/10.1097/ACM.0b013e31819fbaa2. [DOI] [PubMed] [Google Scholar]
- 31.van der Horst K, Siegrist M, Orlow P, Giger M. Residents’ reasons for specialty choice: influence of gender, time, patient and career. Med Educ. 2010 Jun;44(6):595–602. doi: 10.1111/j.1365-2923.2010.03631.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2010.03631.x. [DOI] [PubMed] [Google Scholar]
- 32.Masunaga H, Hitchcock MA. Residents’ and faculty’s beliefs about the ideal clinical teacher. Fam Med. 2010 Feb;42(2):116–120. [PubMed] [Google Scholar]
- 33.Kilminster S, Cottrell D, Grant J, Jolly B. AMEE Guide No. 27: Effective educational and clinical supervision. Med Teach. 2007 Feb;29(1):2–19. doi: 10.1080/01421590701210907. Available from: http://dx.doi.org/10.1080/01421590701210907. [DOI] [PubMed] [Google Scholar]
- 34.Davis N, Davis D, Bloch R. Continuing medical education: AMEE Education Guide No 35. Med Teach. 2008;30(7):652–666. doi: 10.1080/01421590802108323. Available from: http://dx.doi.org/10.1080/01421590802108323. [DOI] [PubMed] [Google Scholar]
- 35.Hammick M, Olckers L, Campion-Smith C. Learning in interprofessional teams: AMEE Guide no 38. Med Teach. 2009 Jan;31(1):1–12. doi: 10.1080/01421590802585561. Available from: http://dx.doi.org/10.1080/01421590802585561. [DOI] [PubMed] [Google Scholar]
- 36.Larsson J, Rosenqvist U, Holmström I. Being a young and inexperienced trainee anesthetist: a phenomenological study on tough working conditions. Acta Anaesthesiol Scand. 2006 Jul;50(6):653–658. doi: 10.1111/j.1399-6576.2006.01035.x. Available from: http://dx.doi.org/10.1111/j.1399-6576.2006.01035.x. [DOI] [PubMed] [Google Scholar]
- 37.Prideaux D. ABC of learning and teaching in medicine. Curriculum design. BMJ. 2003 Feb;326(7383):268–270. doi: 10.1136/bmj.326.7383.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ortwein H, Dirkmorfeld L, Haase U, Herold KF, Marz S, RehbergKlug B, Scheid A, VargasHein O, Spies C. Zielorientierte Ausbildung als Steuerungsinstrument für die Facharztweiterbildung in der Anästhesiologie. [Competency-based education as a steering instrument for residency training in anaesthesiology]. Anaesth Intensivmed. 2007;48(7):420–429. (Ger). [Google Scholar]