Abstract
Different kinds of epidemiologic data provide varying views of the relationships among the main osteoporotic fractures. Descriptive incidence data indicate that distal forearm fractures typically occur earlier than vertebral fractures that, in turn, precede hip fractures late in life. In addition, relative risk estimates document the fact that one osteoporotic fracture increases the risk of subsequent ones. These two observations support the notion of a ‘fracture cascade' and justify the recent emphasis on secondary prevention, that is, more aggressive treatment of patients presenting with a fracture in order to prevent recurrences. However, the absolute risk of a subsequent fracture given an initial one is modest, and the degree to which the second fracture can be attributed to the first one is unclear. Moreover, the osteoporotic fractures encountered in the majority of patients are the first one experienced, and even these initial fractures lead to substantial morbidity and cost. These latter points reemphasize the importance of primary prevention, that is, the management of bone loss and other risk factors to prevent the first fracture. Continued efforts are needed to refine risk assessment algorithms so that candidates for such fracture prophylaxis can be identified more accurately and efficiently.
The term, ‘fracture cascade,' has most often been applied in the context of sequential vertebral fractures.1 This is a well-recognized phenomenon relating to an underlying predisposition (compromised bone structure and strength in the thoracic and lumbar vertebrae) combined with regular exposure to the excessive spinal loads that can result from everyday activities.2 However, biomechanical alterations that result from each new fracture are also thought to have a role.3 This may account for the clustering of fractures in neighboring vertebrae that is often observed4 and could be an explanation for the increased risk of fracture in adjacent vertebrae sometimes seen following vertebroplasty/kyphoplasty.5 Although there is little question about the heightened risk of serial vertebral fractures, attention has recently been called to the need for a more aggressive focus on treating all osteoporotic fractures in order to prevent subsequent ones,6 that is, secondary prevention. Consequently, it becomes important to determine the extent to which there also is a more general fracture cascade, or cycle, from one specific type of osteoporotic fracture to another. Different types of epidemiologic data provide varying perspectives on this question.
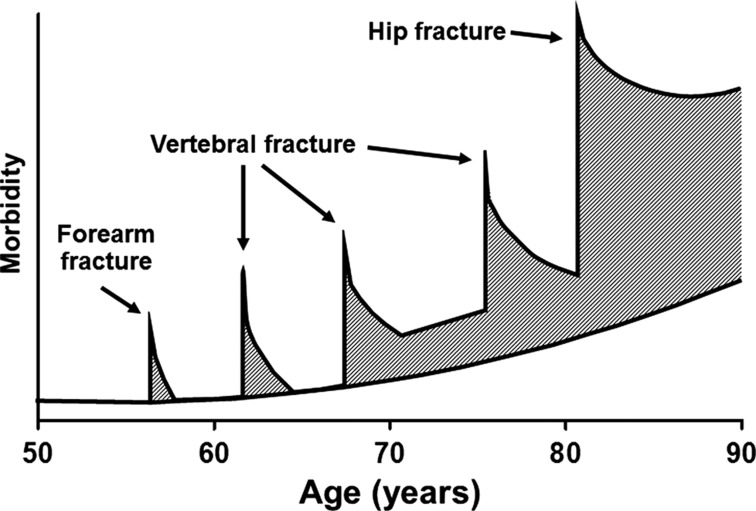
It is generally understood in this regard that forearm fractures typically occur earlier in life among women, especially around the time of menopause, followed by vertebral fractures in mid-life and hip fractures among the oldest old. This notion is captured beautifully in the classic figure by John Kanis and the late Olof Johnell (Figure 1), although that figure pertains specifically to the accumulation of fracture-related morbidity over life rather than to the occurrence of fractures per se. Thus, the idea of a characteristic cascade from forearm to spine to hip fractures is based on descriptive epidemiologic data on fracture incidence. Among adult women in our community, for example, the mean age at hip fracture (82.0 years)7 is indeed greater than the average age (74.1 years) at the time of a spine fracture,8 which in turn is greater than the mean age (65.5 years) at the first distal forearm fracture.9 The situation is less clear in men. Even though hip fractures are seen in the oldest men at a mean age of 77.7 years,7 forearm fractures occur at younger ages in men (mean, 53.8 years) than in women and are infrequent in men in any event.9 Vertebral fractures also occur about a decade earlier on average in men (66.4 years) compared with women, but unlike forearm fractures, they are relatively more common among younger men than younger women;8 this may result from different sex-specific trauma patterns and/or excessive vertebral loading due to occupational activities in men rather than osteoporosis.10
Figure 1.
Schematic representation of the accumulation of fracture-specific morbidity over life (reprinted from Kanis and Johnell33).
The clinical utility of this fracture-specific age distribution relates, of course, to the potential for one fracture to predict another, and in particular, for a less important fracture to predict a more serious one. Indeed, it was recognized almost 40 years ago that distal forearm fractures are associated with later hip fractures and might, therefore, serve as a sentinel event to initiate evaluation and treatment for osteoporosis.11 This is the basis for secondary prevention, mentioned above, and relies mainly on estimates of relative risk. Among postmenopausal women, analytic epidemiologic data document a 1.4- to 4.4-fold increased risk of a subsequent osteoporotic fracture following an initial one.12 A very large cohort study in the United Kingdom found that distal forearm fractures were associated with a 2.0-fold greater risk of a later hip fracture but only a 1.5-fold increase in subsequent vertebral fractures, although vertebral fractures themselves led to a 2.9-fold increase in hip fracture risk.13 Such discrepancies relate to the fact that precipitating events for fracture can differ, even if bone loss represents a common predisposing factor among older adults.14 For example, forearm fractures are said to occur typically among relatively healthy individuals who trip and fall forward onto an outstretched arm, although the actual distribution of trauma is much more complex.15 By contrast, hip fractures are more likely to result when frail individuals fall backwards or to the side, landing on the hip; in that situation, the traumatic forces involved may be a stronger determinant of fracture risk than is bone loss.16 Both forearm fractures and hip fractures, then, are subject to the stochastic phenomenon of falling. By contrast, spine fractures more often result from excessive skeletal loads experienced during activities of daily living, as noted previously, though about one-seventh of them are also caused by falls.17
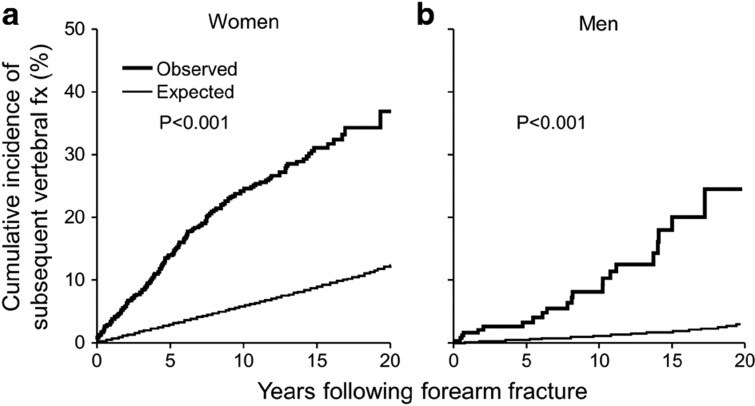
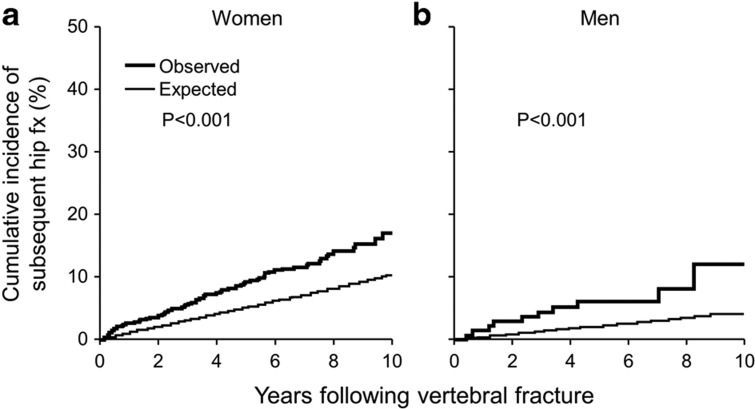
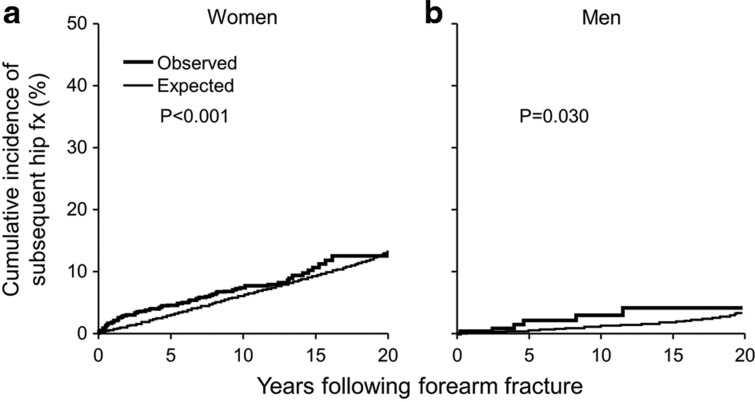
However, making treatment decisions on the basis of relative risk information has long been criticized on the grounds that such estimates may exaggerate the actual likelihood of experiencing either good or bad outcomes.18 In the well-known Women's Health Initiative Trial, for example, there was a relative 26% increase in breast cancer risk but a relative 34% reduction in hip fracture risk associated with combined estrogen/progestin therapy.19 Stated in different terms, the absolute annual increase in breast cancer among treated women was 0.38% compared with 0.30% in controls, whereas the reduction in hip fractures was only from 0.15% to 0.10% per year. What is needed then are epidemiologic data on the absolute risk of one fracture given another. Relevant data from Rochester women and men age 35 years and older are shown in Figures 2, 3, 4. Thus, the cumulative incidence of a vertebral fracture 10 years following a first distal forearm fracture was 24% in women (Figure 2a) and only 8% among men (Figure 2b) but, in both sexes, was substantially more than expected after adjusting for the competing risk of death, which is an important consideration in the osteoporotic population.20 The 10-year cumulative incidence of a hip fracture following a vertebral fracture was 17% in women (Figure 3a) and 12% in men (Figure 3b), again greater than expected. By contrast, even 20 years after a distal forearm fracture, the cumulative incidence of a hip fracture was only 12% in women (Figure 4a) and just 4% in men (Figure 4b). Even though relatively small numbers of subjects were under observation after 10 or 20 years of follow-up, and the study populations included adults as young as age 35 years, these results are consistent with those of Haentjens et al.,21 who found a modest lifetime risk of hip fracture following a distal forearm fracture at age 65 years (17% among women and 10% in men), and a similar lifetime hip fracture risk following vertebral fracture (18% in women and 7% in men).
Figure 2.
Observed versus expected cumulative incidence of a subsequent vertebral fracture (fx) among women (a) and men (b) following a first distal forearm fracture in 1975–94, adjusted for the competing risk of death.
Figure 3.
Observed versus expected cumulative incidence of a subsequent hip fracture (fx) among women (a) and men (b) following a first clinically diagnosed vertebral fracture in 1985–94, adjusted for the competing risk of death.
Figure 4.
Observed versus expected cumulative incidence of a subsequent hip fracture (fx) among women (a) and men (b) following a first distal forearm fracture in 1975–94, adjusted for the competing risk of death.
Absolute risk estimation is the approach taken in the World Health Organization's fracture prediction algorithm, FRAX (http://www.shef.ac.uk/FRAX/tool.jsp), where a prior fracture is one of the strongest determinants of the probability of a subsequent osteoporotic fracture over the next 10 years.22 While absolute risk may be more understandable as a guide for shared decision making between patient and physician,23 even the FRAX score doesn't predict fractures perfectly as not everyone who has a subsequent fracture would have been considered at high risk by that metric.24 The problem extends beyond the usual issues of sensitivity and specificity to concerns about the proportion of future fractures that can be accounted for on the basis of a prior fracture, that is, attributable risk. Although it is not usually the case that one fracture actually causes another, the degree to which a given osteoporotic fracture is preceded by another is of some interest. In Olmsted County, any of the traditional osteoporotic fractures preceded a prevalent vertebral fracture in 55% of postmenopausal women, compared with 21% of controls, but these consisted predominantly of earlier vertebral fractures.8 Excluding them, only 12% of cases and 11% of controls had a prior distal forearm fracture alone, and the risk of a vertebral fracture that could be ‘attributed' to a prior forearm fracture in our data was only 13%. Others, however, have reported a much greater prevalence of prior fractures. Among 509 middle-aged women (of 1518 invited for study) who were recruited from general practitioner practices, for example, 32% of those with a morphometric vertebral deformity had a previous distal forearm fracture compared with 16% of women without a vertebral deformity.25 Similarly, a prior morphometric vertebral deformity was found in 41% of women with a hip fracture compared with only 18% among control women in a nested case–control analysis from the Study of Osteoporotic Fractures,26 although this estimate may be inflated to the extent that some deformities do not represent actual vertebral fractures.27
It is obvious from this discussion that different kinds of epidemiologic data (incidence, relative risk, absolute risk, attributable risk) provide different perspectives on the issue at hand. The incidence data indicate that, at least among women, there is an increase in the mean age from distal forearm fractures to spine fractures to hip fractures, and the relative risk data show that the occurrence of one fracture substantially raises the risk of another. Both observations are consistent with the notion of a cascade across the traditional osteoporotic fracture types. Among those with a specific initial fracture, however, the absolute risk of a particular osteoporotic fracture subsequently is modest (albeit not negligible) over the intermediate term, and the majority of those later fractures will not have been preceded by that specific prior fracture. The latter points undermine any sole focus on interventions directed at interrupting a stereotypical fracture cascade. This is not to deny the fact that many patients with osteoporotic fractures, and those with hip fractures especially, may have a history of previous fractures. However, these usually include a diverse array of fractures that did not occur in any specified order, some of which may have resulted from severe trauma and/or occurred at skeletal sites not normally prompting a consideration for osteoporosis treatment.28
The critical importance of secondary prevention, which is a current focus of many organizations (for example, the 2million2many campaign— http://www.nbha.org/), is not debatable as treatment for osteoporosis among those presenting with a fragility fracture of the hip or spine, and assessment for treatment for those with other fragility fractures, is recommended by all relevant clinical practice guidelines. Secondary prevention, though, is not sufficient to fully address the public health problem posed by osteoporosis as the majority of fractures may represent the first such event ever experienced by that patient,29 and they impose adverse consequences and costs.30 Rather, continued efforts are needed to develop more robust predictors of first fractures for use in primary prevention efforts as efficacious therapies are available should suitable patients be identified.31 Given the likelihood that clinical access to dual-energy X-ray absorptiometry assessments will increasingly be limited by reimbursement restrictions, creative alternatives must be sought. One possibility is the potential for using additional comorbid conditions, known to accelerate bone loss (secondary osteoporosis) and increase fracture risk, but not currently included in FRAX, as predictors of future fracture risk.32 To address this possibility, a systematic review of all comorbid conditions is needed in order to identify those clusters of diseases best able to predict the occurrence of specific osteoporotic fractures. This is of growing interest given the potential for exploiting automated data mining techniques on the comorbidity data that, in the future, will be available from linked electronic health records.
Acknowledgments
This work was supported by research grant P01 AG04875 and made possible by the Rochester Epidemiology Project (R01 AG034676) from the National Institute on Aging, U.S. Public Health Service.
Footnotes
The authors declare no conflict of interest.
References
- Lindsay R, Pack S, Li Z. Longitudinal progression of fracture prevalence through a population of postmenopausal women with osteoporosis. Osteoporos Int 2005;16:306–312. [DOI] [PubMed] [Google Scholar]
- Bouxsein ML. Biomechanics of age-related fractures. In: Marcus R, Feldman D, Nelson DA, Rosen CJ (eds)Osteoporosis 3rd edn. Elsevier: Amsterdam, 2008; 601–623. [Google Scholar]
- Briggs AM, Greig AM, Wark JD. The vertebral fracture cascade in osteoporosis: a review of aetiopathogenesis. Osteoporos Int 2007;18:575–584. [DOI] [PubMed] [Google Scholar]
- Lunt M, O'Neill TW, Felsenberg D, Reeve J, Kanis JA, Cooper C et al. Characteristics of a prevalent vertebral deformity predict subsequent vertebral fracture: results from the European Prospective Osteoporosis Study (EPOS). Bone 2003;33:505–513. [DOI] [PubMed] [Google Scholar]
- Trout AT, Kallmes DF. Does vertebroplasty cause incident vertebral fractures? A review of available data. AJNR Am J Neuroradiol 2006;27:1397–1403. [PMC free article] [PubMed] [Google Scholar]
- Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE Jr, McLellan A et al. Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 2012;27:2039–2046. [DOI] [PubMed] [Google Scholar]
- Melton LJ 3rd, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM et al. Secular trends in hip fracture incidence and recurrence. Osteoporos Int 2009;20:687–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melton LJ 3rd, Atkinson EJ, Cooper C, O'Fallon WM, Riggs BL. Vertebral fractures predict subsequent fractures. Osteoporos Int 1999;10:214–221. [DOI] [PubMed] [Google Scholar]
- Melton LJ 3rd, Amadio PC, Crowson CS, O'Fallon WM. Long-term trends in the incidence of distal forearm fractures. Osteoporos Int 1998;8:341–348. [DOI] [PubMed] [Google Scholar]
- Silman AJ, O'Neill TW, Cooper C, Kanis J, Felsenberg D. Influence of physical activity on vertebral deformity in men and women: results from the European Vertebral Osteoporosis Study. J Bone Miner Res 1997;12:813–819. [DOI] [PubMed] [Google Scholar]
- Gay JD. Radial fracture as an indicator of osteoporosis: a 10-year follow-up study. Can Med Assoc J 1974;111:156–157. [PMC free article] [PubMed] [Google Scholar]
- Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 2000;15:721–739. [DOI] [PubMed] [Google Scholar]
- van Staa TP, Leufkens HG, Cooper C. Does a fracture at one site predict later fractures at other sites? A British cohort study. Osteoporos Int 2002;13:624–629. [DOI] [PubMed] [Google Scholar]
- Stone KL, Seeley DG, Lui LY, Cauley JA, Ensrud K, Browner WS et al. BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res 2003;18:1947–1954. [DOI] [PubMed] [Google Scholar]
- Melton LJ 3rd, Christen D, Riggs BL, Achenbach SJ, Muller R, van Lenthe GH et al. Assessing forearm fracture risk in postmenopausal women. Osteoporos Int 2010;21:1161–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Järvinen TLM, Sievänen H, Khan KM, Heinonen A, Kannus P. Shifting the focus in fracture prevention from osteoporosis to falls. BMJ 2008;336:124–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper C, Atkinson EJ, O'Fallon WM, Melton LJ 3rd. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 1992;7:221–227. [DOI] [PubMed] [Google Scholar]
- Malenka DJ, Baron JA, Johansen S, Wahrenberger JW, Ross JM. The framing effect of relative and absolute risk. J Gen Intern Med 1993;8:543–548. [DOI] [PubMed] [Google Scholar]
- Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA 2002;288:321–333. [DOI] [PubMed] [Google Scholar]
- Leslie WD, Lix LM, Wu X. Competing mortality and fracture risk assessment. Osteoporos Int 2013;24:681–688. [DOI] [PubMed] [Google Scholar]
- Haentjens P, Johnell O, Kanis JA, Bouillon R, Cooper C, Lamraski G et al. Evidence from data searches and life-table analyses for gender-related differences in absolute risk of hip fracture after Colles' or spine fracture: Colles' fracture as an early and sensitive marker of skeletal fragility in white men. J Bone Miner Res 2004;19:1933–1944. [DOI] [PubMed] [Google Scholar]
- Identification of risk factors for use in case-finding. In: Kanis JA on behalf of the World Health Organization Scientific Group Assessment of Osteoporosis at the Primary Care Level University of Sheffield: Sheffield, UK, 2007; 86–144. [Google Scholar]
- Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. JAMA 2004;291:2359–2366. [DOI] [PubMed] [Google Scholar]
- Melton LJ 3rd, Atkinson EJ, Achenbach SJ, Kanis JA, Therneau TM, Johansson H et al. Potential extensions of the US FRAX algorithm. J Osteoporos 2012;2012:528790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobias JH, Hutchinson AP, Hunt LP, McCloskey EV, Stone MD, Martin JC et al. Use of clinical risk factors to identify postmenopausal women with vertebral fractures. Osteoporos Int 2007;18:35–43. [DOI] [PubMed] [Google Scholar]
- Wainwright SA, Marshall LM, Ensrud KE, Cauley JA, Black DM, Hillier TA et al. Hip fracture in women without osteoporosis. J Clin Endocrinol Metab 2005;90:2787–2793. [DOI] [PubMed] [Google Scholar]
- Melton LJ 3rd, Riggs BL, Keaveny TM, Achenbach SJ, Kopperdahl DL, Camp JJ et al. Relation of vertebral fractures to bone density, structure and strength. J Bone Miner Res 2010;25:1922–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuermser L-A, Achenbach SJ, Amin S, Khosla S, Melton LJ 3rd. What accounts for rib fractures in older adults? J Osteoporos 2011, article ID 457591: 10.4061/2011/457591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langsetmo L, Goltzman D, Kovacs CS, Adachi JD, Hanley DA, Kreiger N et al. Repeat low-trauma fractures occur frequently among men and women who have osteopenic BMD. J Bone Miner Res 2009;24:1515–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins RB, Tarride JE, Leslie WD, Metge C, Lix LM, Morin S et al. Estimating the excess costs for patients with incident fractures, prevalent fractures, and nonfracture osteoporosis. Osteoporos Int 2013;24:581–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLean C, Newberry S, Maglione M, McMahon M, Ranganath V, Suttorp M et al. Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis.. Ann. Intern. Med. 2008;148:197–213. [DOI] [PubMed] [Google Scholar]
- Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int 2011;22:2395–2411. [DOI] [PubMed] [Google Scholar]
- Kanis JA, Johnell O. The burden of osteoporosis. J Endocrinol Invest 1999;22:583–588. [DOI] [PubMed] [Google Scholar]