Abstract
Aims:
This study was undertaken to establish correlation between intracholedochal cystic pressure (ICCP) with biochemical changes in bile, liver histology, cyst wall histology, length of common channel, and cyst volume.
Materials and Methods:
In this cross-sectional study, ICCP was measured after surgical access before any mobilization by direct cyst cannulation. Bile was then aspirated for biochemical estimation (bilirubin, amylase, lipase, pH, and electrolytes). Common channel length and cyst volume were determined by preoperative magnetic resonance cholangiopancreatography (MRCP). Liver histology was assessed under parenchymal, bile duct, and portal parameters. Cyst wall was examined for ulceration, inflammation, fibrosis, and metaplasia.
Results:
ICCP was recorded in 31 patients; mean and median ICCP were 15.64 and 14 mmHg, respectively (range = 6-30 mmHg). Cases with median ICCP < 14 had median cyst volume of 48 cc (range = 36-115) and amylase 2052 IU/L (range = 190-5052) whereas those with ICCP ≥ 15 had volume of 20 cc (range = 10-100) (P = 0.004) and amylase 36 IU/L (range = 0-2806) (P = 0.0004) suggesting inverse correlation. No significant correlation was found with bilirubin and electrolytes. ICCP directly correlated with parenchymal changes like hepatocellular damage (P = 0.002) and cholestasis (P = 0.001). It also correlated with bile duct changes. ICCP inversely correlated with cyst wall changes (P = 0.003, 0.0001, 0.023, 0.0013, respectively). High pressure cysts had normal pancreaticobiliary junction.
Conclusion:
High-pressure cysts tend to be smaller but have more severe backpressure changes in liver parenchyma. Low-pressure cysts have high volume and higher levels of amylase and lipase and therefore have more severe cyst wall changes.
KEY WORDS: Choledochal cyst, cyst wall histology, intra choledochal cystic pressure, liver histology, long common channel
INTRODUCTION
The diagnosis and management of choledochal cyst has standard procedures and strategies. However, various aspects of etiology and pathophysiology are not clear particularly with reference to the liver histology, bile composition, the pancreatobiliary junction, and the intracystic pressure.
Dr. Nitin Sharma (main author) received
Dr. U C Chakraborty award
Liver histology has not been given due importance during the course of treatment of choledochal cyst. A few studies have reported extensive pathological changes in the liver in patients with choledochal cyst.[1,2,3] These changes correlate with not only clinical symptoms at presentation but also with response to surgery.[1]
It is conjectured that a cyst, which is tense and has high pressure will have backpressure changes, which in turn will affect liver pathology. Further, the length of the common pancreatobiliary channel should make a difference in the volume and pressure of the cyst and possibly the composition of the bile in the cyst. There are very few studies, which have tried to address this issue. However, no study has attempted simultaneously to correlate the intracystic pressure with detailed biochemical composition of the bile, histopathological changes in the liver, cyst wall histology, length of the common channel and the volume of the cyst. This study attempts to explore these aspects.
MATERIALS AND METHODS
The study was conducted in the Department of Pediatric Surgery, All India Institute of Medical Sciences, New Delhi over a period of 2 years (January 2011 to November 2012). It was a cross- sectional observational study. All patients operated upon for choledochal cyst were included. Patient and parents who refused participation in the study and cases presenting with ruptured or decompressed choledochal cyst were excluded from the study. Ethical clearance for the study was obtained from the Institute Ethics Committee. All enrolled patients were evaluated clinically, biochemically, and radiologically at presentation. All cases underwent preoperative magnetic resonance cholangiopancreatography (MRCP) to confirm the diagnosis, classify the cyst into one of the subtypes, to calculate cyst volume [Figure 1a], delineate the common bile duct [Figure 1b], pancreatic duct [Figure 1b] and to diagnose an abnormal pancreatobiliary junction (APBJ) and a long common channel [Figure 1b], if present. A long common channel was defined as a common channel exceeding 10 mm distal to junction of common bile duct and main pancreatic duct.[4] Cyst volume was calculated using standard formula (0.5 × length × width × anteroposterior dimension/depth at the site of maximum width, length was calculated by multiplying the slice thickness with the number of slices in which cyst was visible).
Figure 1.
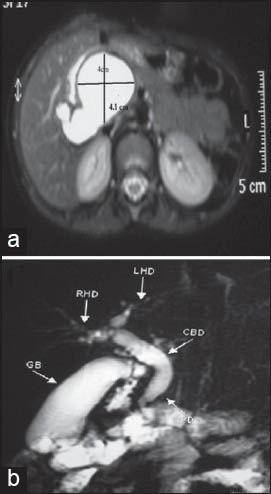
(a) Volume estimation in MRCP, (b) MRCP showing common channel and pancreatic duct
After written and informed consent, all cases underwent exploration. Pressure measurements were made immediately after surgical access and before any mobilization of liver and biliary tree. The system used for pressure measurement was “Datex Ohmeda S/5™ monitor” (range of measurement = −40 to 320 mm Hg, accuracy = ±5% or ±2 mm Hg, sensitivity 5 μV/V/mm Hg), which was attached to the “truwave disposable pressure transducer (Edward life sciences) with continuous 3 ml/hr flush device and stop cock,” which was mounted at the mid cyst level carefully to avoid the error due to height (10 mm Hg for every 13.6 cm difference).[5] A 22-G cannula, attached to saline filled pressure tubing was inserted directly into the choledochal cyst [Figure 2], intracystic pressure was measured using the set up after proper zeroing for 3 times and the average of 3 measurements was taken as intra cystic pressure of the choledochal cyst. Bile was then collected for amylase and other biochemical estimation. Liver histology was assessed by intraoperative liver biopsy.
Figure 2.
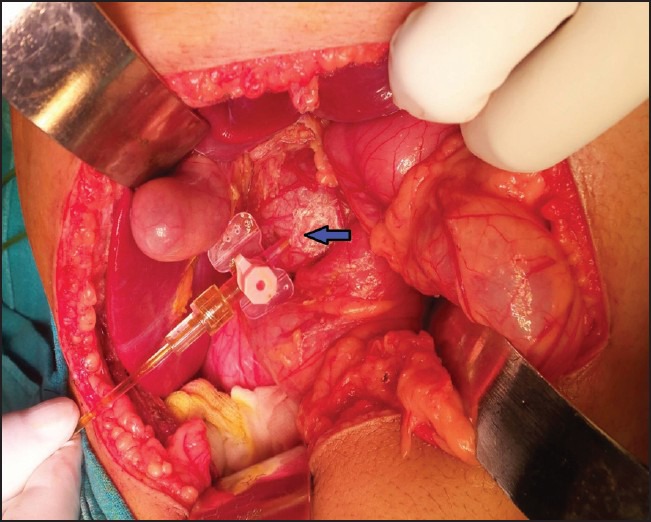
Cannulating choledochal cyst for pressure measurement
Bile analysis consisted of bilirubin, amylase, lipase, pH, sodium, potassium, calcium, chloride, bicarbonate. Amylase, total bilirubin, and lipase estimation were done based on the principle CNP-G (2-chloro 4- nitrophenyl maltotrioside as substrate), DCA (dichloroaniline) and kinetic colorimetry, respectively, on Hitachi 902 analyzer. Bicarbonate estimation was done on Roche-Cobas 221 blood gas analyzer, whole pH, sodium, potassium, chloride and calcium estimates were done on Carelyte electrolyte analysis (from Care Well Biotech Pvt. Limited) using ion-elective electrode method.
All the liver biopsy sample slides (4-μm thick paraffin embedded sections were stained with hematoxylin and eosin) were analyzed by a single senior pathologist who was blinded for the tests. The histopathological changes were graded [Figure 3a–g] using established criteria[1] [Tables 1 and 2]. Cyst wall histology [Figure 3h–j] was graded as given in Table 3.
Figure 3.
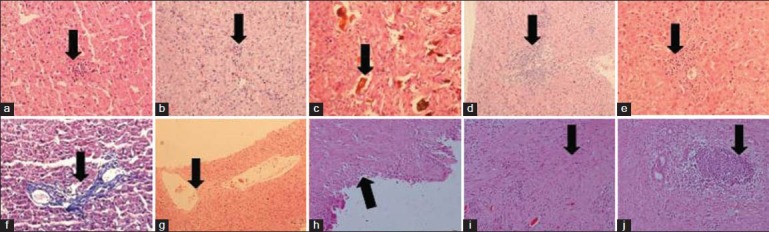
(a) Hepatocellular damage, (b) Parenchymal inflammation, (c) Cholestasis [bile lakes], (d) bile duct inflammation, (e) Bile duct proliferation, (f) Portal fibrosis, (g) Central venous distention, (h) Cyst wall ulceration, (i) Cyst wall fibrosis, (j) Cyst wall inflammation
Table 1.
Grades of hepatocellular damage
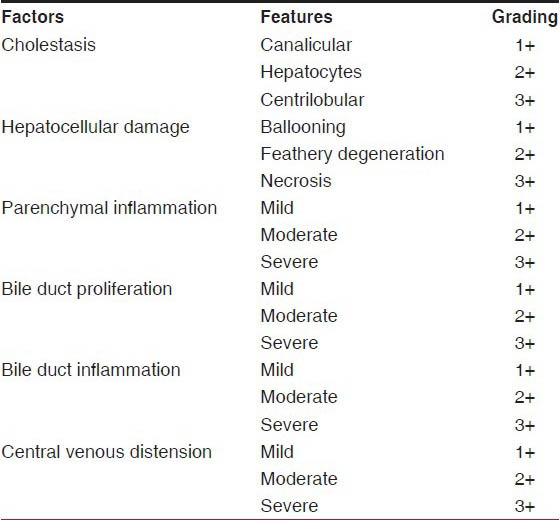
Table 2.
Ohkuma's classification for portal fibrosis
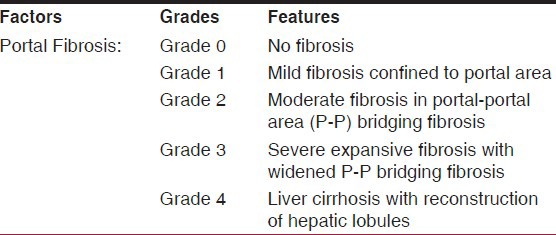
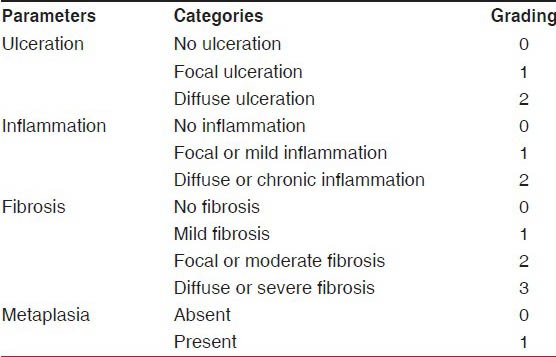
Table 3.
Choledochal cyst wall assessment
Pressure was correlated with different parameters using STATA software version 11 [Stata Corp LP Texas USA]. The statistical tests of significance included chi square test and wilcoxon signed rank test wherever applicable. P value was calculated using Fisher's exact test and a value of <0.05 was considered statistically significant. Due to statistical consideration including a high standard deviation of 6.02 and variation in the values, the median choledochal cystic pressure was used for correlation studies.
RESULTS
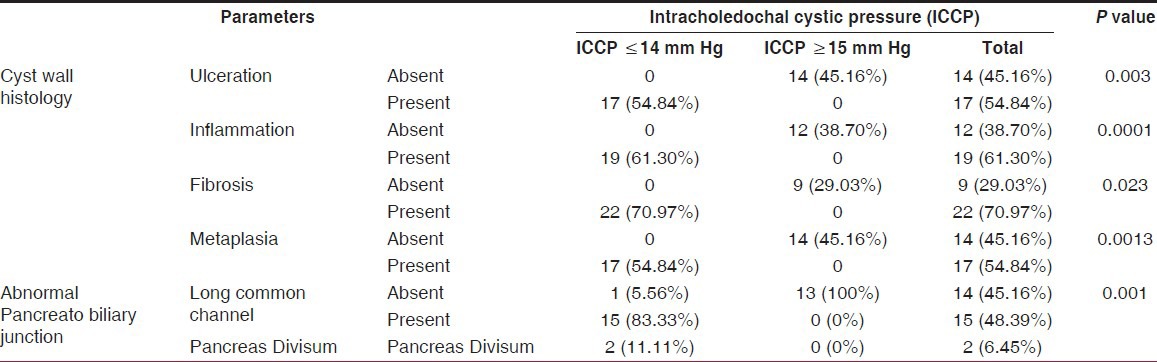
ICCP was measured in 31 patients (all type of choledochal cysts). The male to female ratio was 18:13 = 1.5:1. Mean age at presentation was 63.32 months, median age was 72 months, and the age range was between 4-150 months. Mean ICCP was 15.64 ± 6.02 mm Hg and the median pressure was 14 mm of Hg (range = 6-30 mm Hg). Owing to the standard deviation of 6.02 and variation in the values, median choledochal cystic pressure was used for correlation studies. Considering the median ICCP of 14 (Range = 6-30) mm Hg as a reference point two groups were made one with value less than or equal to the median and another above median. The details of correlation with bile composition are presented in Table 4; ICCP inversely correlated with pH (P = 0.001), amylase (P = 0.004), lipase (P = 0.001). No significant correlation was found with bilirubin (P = 0.54), sodium (P = 0.22), potassium (P = 0.11), calcium (P = 0.18), chloride (P = 0.93) and bicarbonate (P = 0.96). The details of parenchymal changes in the liver are presented in Table 5; ICCP directly correlated with parenchymal changes like hepatocellular damage (P = 0.002) and cholestasis (P = 0.001). It also correlated with bile duct changes. The details of cyst wall changes are presented in Table 6; ICCP directly correlated with cyst wall ulceration (P = 0.003), inflammation (P = 0.0001), fibrosis (P = 0.023) and metaplasia (P = 0.0013). It was found that all cases, with a normal pancreatobiliary junction had an intracholedochal cystic pressure above the median while those with abnormal pancreatobiliary junction including two cases of pancreas divisum had an ICCP below the median value. This observation was also strongly significant (P = 0.001) [Table 6]. Median ICCP ≤ 14 mm Hg was associated with median cyst volume of 48 cc (range = 36-115 cc) (mean = 58.03 ± 24.62). Median ICCP ≥ 15 mm Hg was associated with median cyst volume of 20 cc (range = 10-100 cc) (mean = 30.78 ± 25.84 cc) suggesting a strong inverse correlation (P = 0.0004).
Table 4.
Correlation of ICCP with bile composition
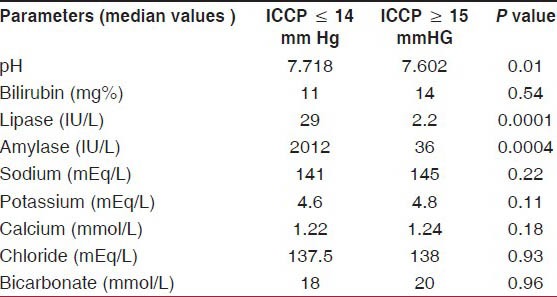
Table 5.
Correlation of various histology parameters correlated with ICCP
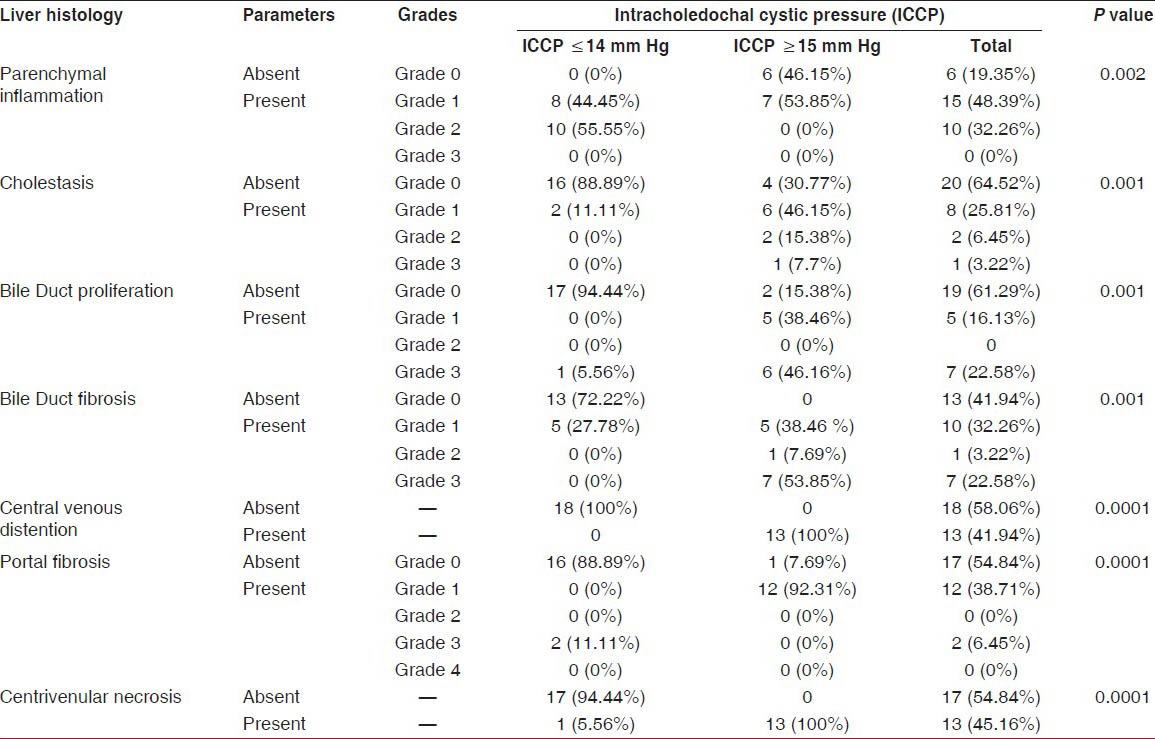
Table 6.
Correlation of Cyst wall histology and abnormal pancreatobiliary junction correlated with ICCP
DISCUSSION
Pressure inside a sphere is related to its volume and surface tension. Pressure and volume are indirectly proportional to each other, thus if we increase the volume then pressure will decrease and vice versa. If the cyst is connected to a system, the backpressure effects are expected at both the ends, if one end is closed or limited, the obvious effect comes to the open end. Same principles are expected to hold true in choledochal cysts, a large cyst is expected to have low pressure and a small volume cyst to have high pressure. The effect of pressure on the ends is also expected but if the distal end is limited by a long common channel then backpressure effects on the liver and cyst wall is expected to be at maximum. A reflux of pancreatic contents into the cyst due to long common channel is likely to worsen the pathology further. Sufficient information on the importance of intracystic pressure, including the normal intracystic pressure values is not available. This study was designed to correlate the intracholedochal cystic pressure with various parameters. In a study by Davenport et al.,[6] the intracystic pressure was correlated with the amylase level of the cyst fluid in a total of 25 patients. The median choledochal pressure (CP) was 13 (interquartile range [IQ] 8.5-17) mm Hg for the study group. The highest pressure recorded was 35 mmHg in a 9-month-old child who was clearly obstructed at the time of laparotomy and they concluded that increased CP was inversely related to the level of bile amylase (and hence the length of the functional common channel). They suggested that obstructive stenosis at the level of the pancreatobiliary junction (but not the ampulla) may be a causal factor in a proportion of choledochal malformations. Li et al.,[7] measured both choledochal pressure and bile amylase levels in Chinese children with choledochal malformation and showed high resting pressures in both fusiform and cystic variants (respective mean pressures 9 and 29 mmHg). In the present study, the mean ICCP was 15.64 mm Hg, the median pressure was 14 mmHg. The range of values was between 6-30 mmHg.
ICCP with bile composition
Davenport et al.,[6] found a significant negative correlation between bile amylase and ICCP and concluded that high pressure cysts are associated with low amylase content. In our study, we observed that in patients where the ICCP was below the median (14 mm Hg) amylase was 2052 IU/L (range = 190-5052 IU/L), for those with ICCP above the median value (14 mm Hg) amylase was 36 IU/L (range = 0-2806 IU/L). Thus, low pressure cysts had high amylase content and high pressure cysts had low amylase content. This difference was found to be statistically significant (P = 0.004) suggesting that reflux of pancreatic amylase in cyst is high if pressure within the cyst is low. High pressure within the cyst prevents this reflux and protects the cyst wall. There is no available study to correlate the pressure with other components of the bile. In our study, we found that in patients where the ICCP was below the median value (14 mmHg) the median pH was 7.718 (range = 7.40-7.98), median bilirubin was 11 mg% (range = 2.1-33 mg%), median lipase was 29 IU/L (range = 10-73 IU/L), median sodium, potassium, calcium and chloride were 141 mEq/L, 4.6 mEq/L, 1.22 mmol/L and 137.5 mEq/L, respectively, whereas in those with ICCP above the median value the median pH was 7.602 (range = 7.38-7.80), median bilirubin was 14 mg% (range = 2.1-20 mg%), cyst lipase was 2.2 IU/L (range = 0-28 IU/L), sodium, potassium, calcium and chloride were 145 mEq/L, 4.8 mEq/L, 1.24 mmol/L and 138 mEq/L respectively, this difference was significant for pH (P = 0.001) and lipase (P = 0.001) but insignificant for bilirubin (P = 0.54), and electrolytes (P = 0.22, 0.11, 0.18, and 0.93, respectively). This observation suggests that a cyst with low pressure has more alkaline bile with more of amylase and lipase contents, and thus a greater pancreatic reflux into the cyst is observed.
ICCP with liver histology
There are very few studies to document liver changes in choledochal cyst per se. Nambirajan et al.,[1] conducted a pilot study to document the condition of the liver in choledochal cyst and hepatocellular damage, parenchymal inflammation, cholestasis, bile duct inflammation, proliferation and fibrosis were the most frequent pathological parameters observed. Another case report by Yeong et al.,[8] reported fibrosis, bile duct proliferation, bile duct inflammation, bile lakes (severe form of cholestasis) and hepatocellular damage in a case of choledochal cyst. Other studies contend that congenital hepatic fibrosis, characteristic dysmorphic bile ducts, acute inflammation and ductal epithelial damage can commonly be found. In addition, ranges of alterations ranging from nonspecific portal inflammation to features of acute or chronic biliary obstruction with bile duct proliferation, neutrophil infiltration, acute cholangitis and periductal or portal fibrosis have been reported.[9] Considering all these above findings, in addition to the fact that a choledochal cyst is an obstructive cholangiopathy, the currently used pathological grading was devised which took into account all the parameters as well as their severity. Although no study has reported the correlation between the pressures within the cyst and histopathological changes in the liver, we attempted to correlate the ICCP with backpressure changes in the liver and found that hepatocellular damage was present in all, and the parenchymal inflammation was more in cyst with low pressure (P = 0.002), so was cholestasis (P = 0.001). It is also directly correlated with bile duct changes like bile duct proliferation (P = 0.001), fibrosis (P = 0.001), central venous distension (P = 0.0001), necrosis (P = 0.0001) and portal fibrosis (P = 0.0001). Bile duct inflammation and portal edema were present in all the cases. This observation suggests that pressure measurement can be used as a simple and straight forward predictor of the associated liver histopathological changes. This could also imply that increased pancreatic reflux, as seen in low pressure cysts, may be responsible for pathological changes like inflammation and cholestasis, whereas, obstruction as evidenced by high pressure may be responsible for bile duct proliferation, central venous distension, necrosis and fibrosis.
ICCP with the cyst wall lining
The normal bile duct consists of vascularized, innervated fibrous tissue with occasional elastic fibers, lined by a mucosa in which a lamina propria bears a single layer of tall columnar epithelium, with scattered mucus-producing goblet cells distally. The characteristic sequence in choledochal cyst appears to be initial generalized reactive hyperplasia succeeded by islands of abnormal mucosa within a denuded, chronically inflamed, fibrotic wall.[10,11,12,13] Necrosis and squamous metaplasia, with sub epithelial inflammatory infiltration and fibrosis appear later, leading to dysplasia and ultimately invasive malignancy (admittedly confined largely to adults). Turowski C et al.,[14] tried to classify the histopathological changes in the cyst wall based on the criteria they mentioned as ELMS (epithelial lining mural score). This scoring system consisted of hyperplasia, inflammation, fibrosis and epithelial lining. They found that, although normal cuboidal and columnar epithelium persisted in every specimen examined, for the most part, changes did occur. Choledochal pressure was significantly higher in the histological groups with higher ELMS values (P = 0.057); conversely, higher ELMS values were significantly associated with lower levels of bile amylase (P = 0.002). We attempted to look at the cyst wall lining with comparatively simpler parameters like ulceration, inflammation, fibrosis and metaplasia because we believed that cyst wall changes can be either due to acute or chronic insult. Ulceration and inflammation were taken to represent acute insult whereas fibrosis and metaplasia were taken to represent chronic sequelae in the cyst wall. When correlated with the intracystic pressure we observed that pressure is inversely correlated with these parameters. It appears that refluxing amylase and lipase may cause these changes in the cyst wall and these effects are both acute and chronic especially in a low pressure cyst.
ICCP with abnormal pancreatobiliary junction
A correlation between the ICCP with abnormal pancreatobiliary junction has not been reported before. Davenport et al.,[6] used bile amylase as an indirect indicator of the presence of a long common channel and showed that those cases where pressure was high the cyst amylase levels were low. In the present study it was found that pressure inversely correlated with the long common channel (P = 0.001). Abnormal or long pancreatobiliary channel was present in 17 (54.84%) cases. Thus those cysts where the ICCP was low, a long common channel was present and similarly a cyst with high pressure had a normal pancreatobiliary junction. This finding could be explained by the fact that those cysts which are low pressure systems have more of associated reflux of pancreatic juice leading to changes in the cyst wall thereby increasing the size of the cyst and further decreasing the pressure within the cyst. Pressure would also be dissipated by the free communication between the common bile duct and the main pancreatic duct.
ICCP with volume
The relationship between intracystic pressure and the volume of the cyst has not been reported before. Davenport et al.,[6] used choledochal dimension index obtained by dividing the maximum diameter of choledochal cyst in mm with the age in years and found that the median choledochal diameter was 15 mm (range = 5-150 mm), the median age-corrected choledochal dimensional index (the maximum diameter [in millimeters] of the common bile duct at preoperative ultrasonography divided by age [in years]) was 6.9 (range = 0.5-71). Dimensional index significantly correlated with the ICCP. As volume of the cyst seemed to be a better parameter rather than taking the diameter at a particular point, which had definite limitations (operator dependence and non-reproducibility) volume calculated by preoperative MRCP using standard formula was considered in this study. We observed a strong negative correlation (P = 0.0004). Thus it could be referred that large volume cyst have lower pressure than those with smaller volumes.
CONCLUSION
Pressure influence a protective effect on the cyst wall but harmful effect on liver histology because ICCP directly correlates with liver parenchymal changes and inversely to cyst wall. High pressure cysts tend to be smaller but have more severe backpressure changes in the liver parenchyma. Low pressure cysts have high volume and higher levels of amylase and lipase in the bile, and possibly as a consequence have more severe changes in the cyst wall.
Although it seems futuristic, preoperative ICCP measurement by endoscopic cannulation of the choledochal cyst may serve as a useful guide for the early intervention in choledochal cyst, especially the asymptomatic and incidentally diagnosed ones. It could also serve as an objective predictor of long-term prognosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Nambirajan L, Taneja P, Singh MK, Mitra DK, Bhatnagar V. The liver in choledochal cyst. Trop Gastroenterol. 2000;21:135–9. [PubMed] [Google Scholar]
- 2.Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL. Choledochal cyst disease. A changing pattern of presentation. Ann Surg. 1994;220:644–52. doi: 10.1097/00000658-199411000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vater A. Qua Scirris viscerum dissert, c.s. ezlerus. Vol. 70. Edinburgh: University Library; 1723. Dissertation in auguralis medica, poes diss; p. 19. [Google Scholar]
- 4.Sugiyama M, Baba M, Atomi Y, Hanaoka H, Mizutani Y, Hachiya J. Diagnosis of anomalous pancreatobiliary junction: Value of magnetic resonance cholangiopancreatography. Surgery. 1998;123:391–7. [PubMed] [Google Scholar]
- 5.S/5TM Datex Ohmeda monitor user manual. 2003 Nov;:2.38–15.6. [Google Scholar]
- 6.Davenport M, Basu R. Under pressure: Choledochal malformation manometry. J Pediatr Surg. 2005;40:331–5. doi: 10.1016/j.jpedsurg.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Li L, Wang D, Chen Y. The changes of morphology and intraluminal pressure in choledochal cyst. Chin J Pediatr Surg. 2000;21:214–6. [Google Scholar]
- 8.Yeong Ml, Nicholson GI, Lee SP. Regression of biliary cirrhosis following choledochal cyst drainage. Gastroenterology. 1982;82:332–5. [PubMed] [Google Scholar]
- 9.Suita S, Shono K, Kinugasa Y, Kubota M, Matsuo S. Influence of age on the presentation and outcome of choledochal cyst. J Pediatr Surg. 1999;34:1765–8. doi: 10.1016/s0022-3468(99)90308-1. [DOI] [PubMed] [Google Scholar]
- 10.Iwai N, Yanagihara J, Tokiwa K, Shimotake T, Nakamura K. Congenital choledochal dilatation with emphasis on pathophysiology of the biliary tract. Ann Surg. 1992;215:27–30. doi: 10.1097/00000658-199201000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lygidakis NJ. Histologic changes and intrahepatic biliary abnormalities in extrahepatic biliary tract obstruction. Surg Gynecol Obstet. 1981;153:532–6. [PubMed] [Google Scholar]
- 12.Davenport M, Stringer MD, Howard ER. Biliary amylase and congenital choledochal dilatation. J Pediatr Surg. 1995;30:474–7. doi: 10.1016/0022-3468(95)90059-4. [DOI] [PubMed] [Google Scholar]
- 13.Dabbas N, Davenport M. Congenital choledochal malformation: Not just a problem for children. Ann R Coll Surg Engl. 2009;91:100–5. doi: 10.1308/003588409X391947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turowski C, Kinsley AS, Davenport M. Role of pressure and pancreatic reflux in the aetiology of choledochal malformation. Br J Surg. 2011;98:1319–26. doi: 10.1002/bjs.7588. [DOI] [PubMed] [Google Scholar]


